Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1728
Peer-review started: May 19, 2023
First decision: June 1, 2023
Revised: June 9, 2023
Accepted: July 11, 2023
Article in press: July 11, 2023
Published online: August 27, 2023
Processing time: 98 Days and 3 Hours
Patients undergoing laparoscopic resection of liver metastases of colorectal cancer are prone to negative emotions and decrease of digestive function. Early nursing and psychological intervention are necessary.
To observe the effect of enhanced recovery nursing combined with mental health education on postoperative recovery and mental health of patients undergoing laparoscopic resection of liver metastases of colorectal cancer.
One hundred and twenty patients who underwent laparoscopic resection of liver metastases of colorectal cancer at our hospital between March 2021 and March 2023, were selected as participants. The patients admitted from March 1, 2021 to February 28, 2022 were set as the control group, and they were given routine nursing combined with mental health education intervention. While the patients admitted from March 1, 2022 to March 31, 2023 were set as the observation group, they were given accelerated rehabilitation surgical nursing combined with mental health education intervention. The differences in postoperative recovery-related indices, complications and pain degrees, and mental health-related scores were compared between groups. The T lymphocyte subset levels of the two groups were also compared.
The postoperative exhaust, defecation, eating and drainage time of the observation group were shorter than those of the control group. The pain scores of the observation group were lower than those of the control group at 6, 12, 24, 48, and 72 h after surgery. The cumulative complication rate of the observation group was lower than that of the control group (P < 0.05). The CD4+/CD8+ in the observation group was higher than that in the control group 3 d after surgery (P < 0.05). After intervention, the self-rating depression scale, self-rating anxiety scale, avoidance dimension, and yielding dimension in Medical coping style (MCMQ) scores of the two groups were lower than those prior to intervention, and the scores in the observation group were lower than those in the control group (P < 0.05). The face dimension score in the MCMQ score was higher than that before intervention, and that of the observation group was higher than that of the control group (P < 0.05). After intervention, the total scores of the life function index scale (FLIC) and psychological well-being scores of cancer patients in the two groups, and the physical and social well-being scores in the observation group, were higher than those before intervention. The nursing satisfaction of the observation group was higher than that of the control group (P < 0.05). The physical, psychological, and social well-being, and the total FLIC scores of the observation group were higher than those in the control group after surgery (P < 0.05).
Enhanced recovery nursing combined with mental health education can promote the recovery of gastrointestinal function, improve the mental health and quality of life of patients after laparoscopic resection of colorectal cancer liver metastases, and reduce the incidence of complications.
Core Tip: This study analyzed the effect of accelerated rehabilitation surgical nursing combined with mental health education on postoperative recovery and mental health of patients undergoing laparoscopic resection of colorectal cancer liver metastases. Enhanced recovery after surgical nursing combined with mental health education can promote the recovery of gastrointestinal function, improve the mental health and quality of life of patients after laparoscopic resection of colorectal cancer liver metastases, and reduce the incidence of complications.
- Citation: Li DX, Ye W, Yang YL, Zhang L, Qian XJ, Jiang PH. Enhanced recovery nursing and mental health education on postoperative recovery and mental health of laparoscopic liver resection. World J Gastrointest Surg 2023; 15(8): 1728-1738
- URL: https://www.wjgnet.com/1948-9366/full/v15/i8/1728.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i8.1728
Colorectal cancer is a common gastrointestinal malignant tumor, and the morbidity and mortality of this disease are high. However, the early symptoms are not obvious. When patients gradually develop obvious symptoms such as hematochezia and diarrhea, they are usually in the advanced stage. With the continuous proliferation and differentiation of tumor cells, most patients will have tumor cell metastasis[1]. The liver is the most common organ of distant metastasis in colorectal cancer. Approximately 53% of colon cancer patients will have liver metastasis[2]. Laparoscopic tumor resection is a common surgical treatment method for liver metastasis of colorectal cancer in clinical practice, which reduces the tumor burden of patients by removing liver metastases and has the advantages of a small wound, less bleeding, and quick recovery[3]. However, surgical treatment cannot completely control the disease. Patients will also need to accept chemotherapy and other rehabilitation maintenance, and there is still a risk of postoperative recurrence. Therefore, patients will have negative emotions such as fear and anxiety. The surgical method is in the abdomen of the patient, so it will affect the digestive function after surgery. And therefore, early nursing and psychological intervention are necessary[4,5]. Accelerated rehabilitation surgical nursing is a new nursing concept and rehabilitation model. Based on medical evidence, perioperative intervention is performed to reduce the physiological and psychological traumatic stress of patients and achieve rapid rehabilitation[6,7]. This study analyzed the effect of accelerated rehabilitation surgical nursing combined with mental health education on postoperative recovery and mental health of patients undergoing laparoscopic resection of colorectal cancer liver metastases.
General information: From March 2021 to March 2023, 120 patients who underwent laparoscopic resection of liver metastases from colorectal cancer in our hospital were selected as subjects. Among them, patients admitted from March 1, 2021 to February 28, 2022 were set as the control group, and routine nursing combined with mental health education intervention was given. The group consisted of 30 men and 27 women, aged 31–78 years, with an average age of (62.25 ± 9.74) years. In addition, patients admitted from March 1, 2022 to March 31, 2023 were set as the observation group and given accelerated rehabilitation surgical nursing combined with mental health education intervention. This group included 35 men and 28 women, aged 28–80 years, with an average age of (63.26 ± 10.14) years. The general data of the two groups were similar (P > 0.05). See Table 1.
| General information | Control group (n = 57) | Observation group (n = 63) | χ2/t | P value |
| Gender | 0.063 | 0.802 | ||
| Male | 41 (71.93) | 44 (69.84) | ||
| Female | 16 (28.07) | 19 (30.16) | ||
| Age [ (mean ± SD), age] | 57.79 ± 9.28 | 56.70 ± 11.27 | 0.57 | 0.57 |
| BMI [ (mean ± SD), kg/m2] | 23.43 ± 3.73 | 23.17 ± 3.06 | 0.433 | 0.666 |
| Type of disease | 0.02 | 0.887 | ||
| Rectal cancer | 21 (36.84) | 24 (38.10) | ||
| Colon cancer | 36 (63.16) | 39 (61.90) | ||
| Maximum diameter of metastatic lesion [(mean ± SD), cm] | 3.46 ± 0.94 | 3.39 ± 0.98 | 0.398 | 0.691 |
| Number of liver metastatic lesions | ||||
| 1 | 20 (35.09) | 23 (36.51) | 0.036 | 0.982 |
| 2 | 19 (33.33) | 21 (33.33) | ||
| ≥ 3 | 18 (31.58) | 19 (30.16) | ||
| Surgical program [n (%)] | 0.3 | 0.956 | ||
| Partial hepatectomy | 21 (36.84) | 24 (38.10) | ||
| Segmentectomy | 16 (28.07) | 15 (23.81) | ||
| Lobectomy | 14 (24.56) | 17 (26.98) | ||
| Other | 6 (10.53) | 7 (11.11) |
Inclusion and exclusion criteria: Inclusion criteria: (1) Colorectal cancer in line with the 'colorectal cancer diagnosis and treatment norms'[8] standards and underwent radical surgery; postoperative pathology confirmed; (2) Age 18 ≤ 80 years; (3) Abdominal computed tomography or magnetic resonance imaging confirmed liver metastasis, in line with surgical indications; and (4) Complete clinical data.
Exclusion criteria[9]: (1) Laparotomy or conversion to laparotomy; (2) Palliative excision; (3) With colorectal obstruction or perforation; (4) Combination with other serious diseases; and (5) Have comprehension or hearing impairment.
Mental health education intervention methods: The patients were administered psychological evaluation and intervention according to their existing situation. The goals were to perform mental health education for patients, to encourage patients to express their negative emotions, to take corresponding measures to alleviate them, and to monitor patients' psychological status and emotions in real time.
Routine nursing intervention methods: The patients were given routine preoperative education, routine postoperative treatment according to the doctor's advice, and recommendations of postoperative precautions.
Accelerated rehabilitation surgical nursing methods: (1) Health education and psychological counseling: The nurses were trained on the specific properties of the disease, surgery, and mental health; the patients were then introduced to the disease characteristics and surgical methods in a specific manner, using video, brochures or slides to reduce fear of the disease and surgery. The nurses guided patients in discussions surrounding psychological challenges, encouraged them to vent negative emotions, listened patiently and gave guidance, and established patient confidence in overcoming the disease; (2) Analgesia: Teaching patients to correctly express pain signals to help medical staff to quickly and accurately judge pain symptoms, and inform patients of the rationality of postoperative pain and the importance of reflecting the condition. Nurses guided patients in the use of a self-controlled intravenous analgesia pump, and if necessary, administered oral antipyretic analgesics to enhance the analgesic effect; (3) Diet: After surgery, patients were still not allowed water but if thirsty could dampen their lips with a wet cotton swab. After 6 h, moderate water consumption was allowed, and after 12 h rice soup could be consumed. On the second postoperative day, a number of small semi-liquid meals could be eaten throughout the day. After 3 d of the liquid diet, the principle of consuming numerous small meals throughout the day was continued, while gradually increasing the amount of food, until the patient could return to their normal diet. Patients were advised to eat easily digestible, protein-rich foods that were rich in cellulose, and to avoid spicy foods; (4) Rehabilitation exercise: Nurses informed patients of the necessity of postoperative rehabilitation exercise and strived for the active cooperation of patients and their families. In the early postoperative stage, a semi-reclining position could be assumed, and the patient could be turned onto their back or front every hour. From the third day after surgery, the patients were guided in performing bed exercises such as hip lifting and kicking, which continued daily until they were allowed to get out of bed; and (5) Acupoint massage: Hegu, Zusanli, Weizhong, and other acupoints were massaged to relieve pain, and abdominal massage was performed to promote gastrointestinal motility.
The differences in postoperative recovery-related indices, complications and pain degrees, and mental health-related scores were compared between groups. The T lymphocyte subset levels of the two groups were examined.
Detection method: Fasting fresh blood samples were collected from patients in the morning, using an automatic blood biochemical detector, at a speed of 5500 r/min, centrifugal radius of 10 cm, for a centrifugal processing time of 20 min, allowing separation of serum into the detector, and detection of T lymphocyte subsets.
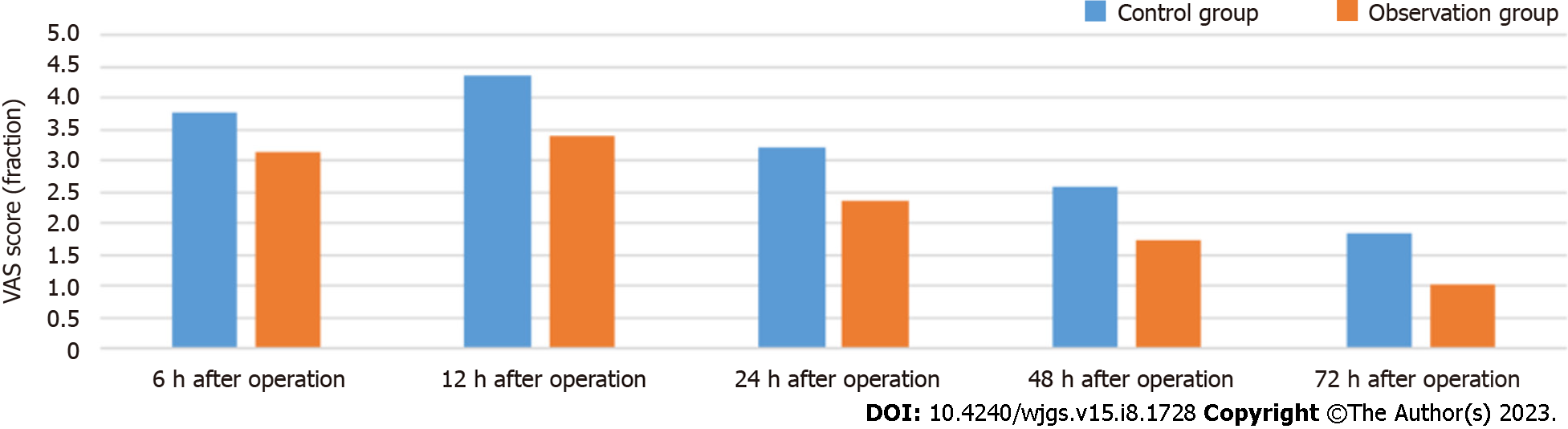
Degrees of pain: The visual analogue scale score was used to evaluate pain at different time points after surgery[10]. Pain was scored out of 10, where 0 was no discomfort, and 10 was the most severe pain; the score was positively correlated with the degree of pain.
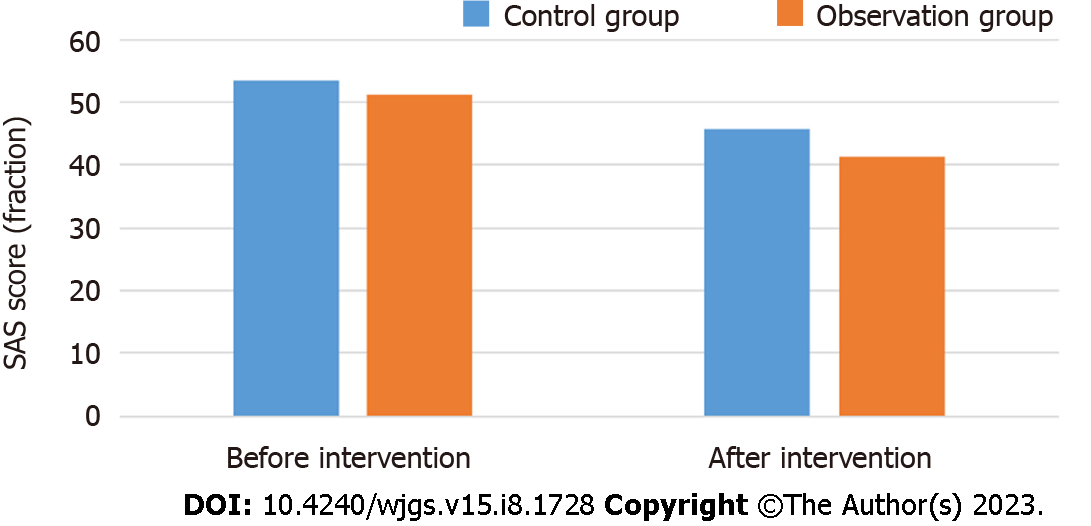
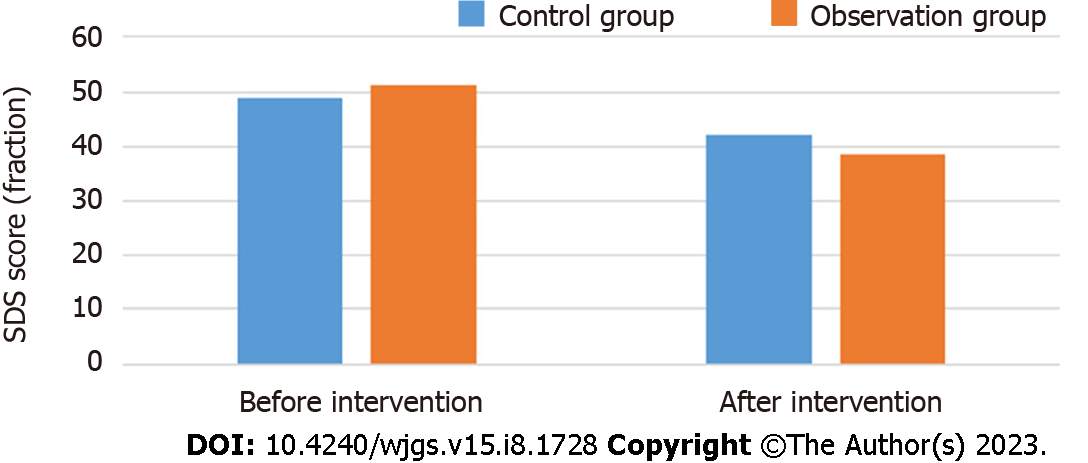
Mental health: The self-rating depression scale (SDS)[11] and self-rating anxiety scale (SAS)[12] that were used to evaluate the mental health of patients included 20 items, and the critical values were 53 and 50 respectively; the higher the score, the worse the mental health of patients.
Medical coping style (MCMQ) score[13]: A total of 20 items, covering the face (8 items), avoidance (7 items), and yield (5 items). For each of these three aspects, a single item was given a score of 1–4 points; the higher the score, the greater the patient was adopting the coping style.
Cancer patients living function index scale (FLIC) score[14]: This consisted of a total of 22 items covering physical condition, psychological state, cancer-related difficulties, social well-being, and nausea. For each of these 5 aspects, a single item was given a score of 1–7 points; the higher the score, the better the quality of life.
Nursing satisfaction: The self-made satisfaction score table of the department was used to evaluate the 0-10 points with the patient when the treatment was completed, 0-4 points were dissatisfied, 5-8 points were satisfied, and 9-10 points were very satisfied.
SPSS 26.0 software was used to process the data. FLIC score, MCMQ score, and other measurement data that conformed to normal or approximate distribution were described by (`c ± s), and a t-test was used for comparison. Countable data such as those for the surgical plan and number of liver metastases were described by the number of patients (%), and a χ2 test was used for comparison.
The postoperative exhaust, drainage, defecation and eating time in the observation group were shorter than those in the control group (P < 0.05). See Table 2.
| Group | n | Exhaust time (hour) | Defecation time (hour) | Eating time (day) | Drainage time (day) | Postoperative hospital stay (day) |
| Control group | 57 | 42.56 ± 10.23 | 66.36 ± 15.23 | 1.96 ± 0.27 | 8.25 ± 1.63 | 14.12 ± 3.13 |
| Observation group | 63 | 31.54 ± 8.67 | 49.93 ± 9.77 | 1.48 ± 0.32 | 6.58 ± 1.44 | 12.03 ± 2.87 |
| t | 6.384 | 7.1 | 8.831 | 5.959 | 3.816 | |
| P value | 0 | 0 | 0 | 0 | 0 |
T lymphocyte subsets were similar between the two groups (P > 0.05). At 3 d after operation, CD4+ in the two groups and CD3+ and CD4+/CD8+ in the control group were lower than before, while CD8+ in the control group was higher than before, and CD3+, CD8+ and CD4+/CD8+ in the observation group were similar with those before operation (P > 0.05). CD4+/CD8+ in the observation group was higher than that in the control group at 3 d after operation, and CD3+, CD4+ and CD8+ were compared with the control group (P > 0.05). See Table 3.
| Group | n | CD3+ (μL) | CD4+ (μL) | CD8+ (μL) | CD4+/CD8+ | ||||
| Preoperative | 3 d after operation | Preoperative | 3 d after operation | Preoperative | 3 d after operation | Preoperative | 3 d after operation | ||
| Control group | 57 | 1214.36 ± 256.36 | 1108.33 ± 241.25a | 859.63 ± 210.36 | 778.52 ± 189.69a | 658.52 ± 187.25 | 736.33 ± 214.05a | 1.36 ± 0.25 | 1.07 ± 0.36a |
| Observation group | 63 | 1197.68 ± 267.33 | 1163.69 ± 287.11 | 867.44 ± 225.59 | 842.52 ± 200.13a | 647.96 ± 193.24 | 665.36 ± 204.78 | 1.34 ± 0.28 | 1.28 ± 0.34a |
| t | 0.348 | 1.137 | 0.196 | 1.793 | 0.303 | 1.856 | 0.411 | 3.286 | |
| P value | 0.728 | 0.258 | 0.845 | 0.076 | 0.762 | 0.066 | 0.682 | 0.001 | |
The pain scores of the observation group were lower than those of the control group at 6 h, 12 h, 24 h, 48 h and 72 h after operation (P < 0.05). See Figure 1.
The mental health related scores of the two groups were similar before intervention (P > 0.05). After intervention, the SAS and SDS scores of the two groups were lower than those before intervention, and the observation group was lower (P < 0.05). See Figures 2 and 3.
MCMQ scores of the two groups were similar before intervention (P > 0.05). After intervention, the face scores of the two groups were higher than those before intervention, and the observation group was higher (P < 0.05). The avoidance and yield scores of the two groups were lower than those before intervention, and the observation group was lower (P < 0.05). See Table 4.
| Group | n | Face | Avoid | Yield | |||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 18.36 ± 3.23 | 21.04 ± 3.34a | 20.36 ± 3.15 | 16.89 ± 2.44a | 14.96 ± 2.77 | 11.25 ± 1.93a |
| Observation group | 63 | 17.78 ± 3.26 | 24.15 ± 2.06a | 21.05 ± 3.34 | 14.12 ± 2.05a | 15.12 ± 2.16 | 10.01 ± 1.27a |
| t | 0.978 | 6.202 | 1.161 | 6.754 | 0.355 | 4.195 | |
| P value | 0.33 | 0 | 0.248 | 0 | 0.724 | 0 | |
The FLIC scores of the two groups were similar before intervention (P > 0.05). After intervention, the total scores of FLIC and good psychology in the two groups and the scores of good body and good society in the observation group were higher than those before intervention. The scores of good body, difficulty due to cancer, good society and nausea in the control group were compared with those before intervention (P > 0.05). The scores of good body, good psychology, good society and the total score of FLIC in the observation group were higher (P < 0.05). See Table 5.
| Group | n | Good body | Psychologically sound | Difficulty due to cancer | |||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 40.58 ± 3.96 | 41.35 ± 4.23 | 24.02 ± 3.36 | 25.26 ± 3.07a | 12.23 ± 2.09 | 12.75 ± 2.26 |
| Observation group | 63 | 41.07 ± 3.75 | 46.96 ± 3.87a | 23.87 ± 3.41 | 26.89 ± 3.31a | 12.14 ± 2.28 | 12.83 ± 2.07 |
| t | 0.696 | 7.587 | 0.242 | 2.788 | 0.225 | 0.202 | |
| P value | 0.488 | 0 | 0.809 | 0.006 | 0.823 | 0.84 | |
| Group | n | Good society | Nausea | Total score of FLIC | |||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | ||
| Control group | 57 | 10.26 ± 1.38 | 10.87 ± 1.47 | 3.05 ± 1.14 | 3.11 ± 1.05 | 81.89 ± 4.56 | 93.34 ± 5.16a |
| Observation group | 63 | 10.19 ± 1.44 | 12.68 ± 1.51a | 2.97 ± 1.21 | 3.23 ± 1.11 | 80.74 ± 4.61 | 102.96 ± 6.44a |
| t | 0.271 | 6.64 | 0.372 | 0.607 | 1.372 | 8.869 | |
| P value | 0.787 | 0 | 0.711 | 0.545 | 0.173 | 0 | |
The cumulative complication rate of the observation group was 3.17% (2/63), which was lower than 14.04% (8/57) of the control group (P < 0.05). See Table 6.
| Group | n | Incision infection | Pleural effusion | Intestinal obstruction | Celiac hemorrhage | Cumulative |
| Control group | 57 | 3 (5.26) | 3 (5.26) | 1 (1.75) | 1 (1.75) | 8 (14.04) |
| Observation group | 63 | 1 (1.59) | 1 (1.59) | 0 (0.00) | 0 (0.00) | 2 (3.17) |
| χ2 | 4.621 | |||||
| P value | 0.032 |
The nursing satisfaction of the observation group was 93.65%, which was higher than that of the control group (80.70%) (P < 0.05). See Table 7.
| Group | n | discontent | satisfied | Very satisfied | Satisfaction rate |
| Control group | 57 | 11 (19.30) | 23 (40.36) | 23 (40.36) | 46 (80.70) |
| Observation group | 63 | 4 (6.35) | 29 (46.03) | 30 (47.62) | 59 (93.65) |
| χ2 | 6.666 | ||||
| P value | 0.01 |
Surgical resection is the best treatment for long-term survival of patients with colorectal cancer and liver metastasis. Simultaneously, one-stage resection of primary and metastatic lesions has become widely accepted[15]. The minimally invasive, safe, and effective characteristics of laparoscopic surgery give it unique advantages in simultaneous resection of colorectal liver metastases[16]. The implementation of targeted nursing and psychological intervention during the perioperative period can further promote the postoperative recovery of patients and help to achieve better therapeutic effects[17]. Accelerated rehabilitation surgical nursing is an innovative treatment revolution, and it is mainly patient centered. Through the cooperation of surgery, anesthesia, nursing, nutrition, and other disciplines, it achieves win-win results for doctors and patients' families[18].
In this study, the postoperative recovery-related indicators of the two groups were compared. The results showed that the postoperative exhaust, defecation, eating, drainage, and hospitalization time of the observation group were shorter than those of the control group, indicating that accelerated rehabilitation surgical nursing combined with mental health education can accelerate the recovery of gastrointestinal function. The reason is that accelerated rehabilitation surgical nursing provides targeted nursing for patients on postoperative diet. According to the recovery guidelines for postoperative gastrointestinal function, a phased diet plan is formulated to avoid spicy and other stimulating foods and reduce the hyperstimulation of gastrointestinal function. At the same time, the patient's abdomen is massaged to promote gastrointestinal peristalsis and accelerate the recovery of postoperative gastrointestinal function[19-21].
In this study, the degrees of pain experienced by the two groups were compared. The pain score of the observation group was lower than that of the control group at 6, 12, 24, 48, and 72 h after surgery, indicating that education can reduce the degree of postoperative pain in patients. The reason is that education promotes the understanding of the importance of surgery and postoperative precautions. The diversification of education methods can enable patients to understand the operation process and treatment principle in different aspects; this may reduce patients' fear of postoperative pain and improve compliance[22]. Simultaneously, accelerated rehabilitation surgical nursing, combined with the use of a self-controlled intravenous analgesia pump, and non-steroidal anti-inflammatory drugs for analgesia treatment, can reduce incision pain[23]. Massage of the Hegu, Zusanli, Weizhong, and other acupoints also helps to reduce the degree of pain and reduce the pain score[24].
This study compared the mental health-related scores of the two groups. The SAS and SDS scores of the two groups were lower than those before the intervention, and the postoperative observation group score was lower than that of the control group. The MCMQ scores of the two groups were compared. The scores of the two groups were higher than those before the intervention, and the observation group score was higher than that of the control group after surgery. The avoidance and yield scores of the two groups were lower than those before the intervention, and the observation group scores were lower than those of the control group after surgery. These results show that accelerated rehabilitation surgical nursing combined with mental health education can more effectively alleviate patients' negative emotions such as anxiety and depression, improve patients' psychological state, and help patients actively face the disease. This is because mental health education through the psychological assessment of patients and use of the full range of psychological interventions, prompting patients to vent their negative emotions, help patients to resolve bad mood and establish a good mentality[25]. Accelerated rehabilitation surgical nursing reduces patients’ fear of disease and surgery, by improving the professional and psychological nursing level of staff, allowing the timely psychological counseling of patients, and conveying knowledge of the disease to patients in an accessible manner, so as to better improve their psychological state [26,27].
After the intervention, the physical, psychological, social well-being, and FLIC in the observation group were higher than those in the control group, and the incidence of complications was lower. The nursing satisfaction of the observation group was better than that of the control group, indicating that accelerated rehabilitation surgical nursing combined with mental health education can help reduce complications and improve the quality of life of patients and nursing satisfaction. As mentioned above, accelerated rehabilitation surgical nursing can promote the recovery of gastrointestinal function and improve the psychological state of patients. Concurrently, through postoperative rehabilitation training, accelerated rehabilitation surgical nursing guides patients to promote physical recovery. The hip lifting and kicking exercises are used to exercise the patients’ lower limbs, thereby promoting their functional recovery, and reducing complications such as intestinal obstruction and incision infection, improving patient activities of daily life and quality of life[28-30]. The prevention of various complications can improve the postoperative comfort of patients, and pay more attention to psychological nursing in the nursing process, timely help patients solve difficulties, and establish a good doctor-patient relationship.
The patients included in this study were from the same center, and the number of patients was also limited. The results of this study need to be confirmed by large cohort study in the future.
In summary, enhanced recovery after surgical nursing combined with mental health education can promote the recovery of gastrointestinal function, improve patients’ mental health and quality of life, and reduce the incidence of complications after laparoscopic resection of liver metastases from colorectal cancer.
Laparoscopic tumor resection is a common surgical treatment method for liver metastasis of colorectal cancer in clinical practice. However, surgical treatment cannot completely control the disease, and patients will also need to accept chemotherapy and other rehabilitation maintenance, and there is still a risk of postoperative recurrence.
These patients will have negative emotions such as fear and anxiety. The surgical method is in the abdomen of the patient, so it will affect the digestive function after surgery. Therefore, early nursing and psychological intervention are necessary.
To analyze the effect of accelerated rehabilitation surgical nursing combined with mental health education on postoperative recovery and mental health of patients undergoing laparoscopic resection of colorectal cancer liver metastases.
One hundred and twenty patients who underwent laparoscopic resection of liver metastases of colorectal cancer were selected and divided into two groups. The control group was given routine nursing combined with mental health education intervention, while the observation group was given accelerated rehabilitation surgical nursing combined with mental health education intervention. The differences in postoperative recovery-related indices, complications and pain degrees, and mental health-related scores were compared between groups. The T lymphocyte subset levels of the two groups were also compared.
The results in the observation group were better in postoperative recovery-related indices, complications, pain degrees, and mental health-related scores than those in the control group. The nursing satisfaction of the observation group was higher than that of the control group. The physical, psychological, and social well-being, and the total FLIC scores of the observation group were higher than those in the control group after surgery.
Enhanced recovery nursing combined with mental health education can promote the recovery of gastrointestinal function, improve the mental health and quality of life of patients after laparoscopic resection of colorectal cancer liver metastases, and reduce the incidence of complications.
The results of this study will be confirmed in large cohort studies performed in multiple centers.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maher CA, United States; Rumpold H, Austria S-Editor: Li L L-Editor: A P-Editor: Wu RR
| 1. | Biller LH, Schrag D. Diagnosis and Treatment of Metastatic Colorectal Cancer: A Review. JAMA. 2021;325:669-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 1425] [Article Influence: 356.3] [Reference Citation Analysis (0)] |
| 2. | Li J, Ma X, Chakravarti D, Shalapour S, DePinho RA. Genetic and biological hallmarks of colorectal cancer. Genes Dev. 2021;35:787-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 303] [Article Influence: 75.8] [Reference Citation Analysis (0)] |
| 3. | Baidoun F, Elshiwy K, Elkeraie Y, Merjaneh Z, Khoudari G, Sarmini MT, Gad M, Al-Husseini M, Saad A. Colorectal Cancer Epidemiology: Recent Trends and Impact on Outcomes. Curr Drug Targets. 2021;22:998-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 154] [Article Influence: 38.5] [Reference Citation Analysis (2)] |
| 4. | Inoue Y, Ishii M, Fujii K, Nihei K, Suzuki Y, Ota M, Kitada K, Kuramoto T, Shima T, Kodama H, Matsuo K, Miyaoka Y, Miyamoto T, Yokohama K, Ohama H, Imai Y, Tanaka R, Sanda M, Osumi W, Tsuchimoto Y, Terazawa T, Ogura T, Masubuchi S, Yamamoto M, Asai A, Shirai Y, Inoue M, Fukunishi S, Nakahata Y, Takii M, Goto M, Kimura F, Higuchi K, Uchiyama K. Safety and Efficacy of Laparoscopic Liver Resection for Colorectal Liver Metastasis With Obesity. Am Surg. 2021;87:919-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (3)] |
| 5. | Mahamid A, Sawaied M, Berger Y, Halim NA, Goldberg N, Abu-Zaydeh O, Bitterman A, Sadot E, Haddad R. Hand-assisted Laparoscopic Surgery for Colorectal Liver Metastasis: Analysis of Short-term and Long-term Results. Surg Laparosc Endosc Percutan Tech. 2021;31:543-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Aoki T, Matsuda K, Mansour DA, Koizumi T, Goto S, Watanabe M, Otsuka K, Murakami M. Narrow-band Imaging Examination of Microvascular Architecture of Subcapsular Hepatic Tumors. J Surg Res. 2021;261:51-57. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Zhu DX, He GD, Mao YH, Wei Y, Ren L, Lin Q, Wang XY, Xu JM. [Efficacy analysis on laparoscopic simultaneous resection of primary colorectal cancer and liver metastases]. Zhonghua Weichang Waike Zazhi. 2020;23:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Tsuji Y, Inoue A, Nishizawa Y, Kagawa Y, Aomatsu M, Takeuchi T, Hirano M, Komatsu H, Miyazaki Y, Tomokuni A, Matsuoka K, Fushimi H, Motoori M, Iwase K, Fujitani K. [A Case of Unresectable Liver Metastasis from Rectal Cancer Treated with Conversion Therapy]. Gan To Kagaku Ryoho. 2021;48:1804-1806. [PubMed] |
| 9. | Machairas N, Dorovinis P, Kykalos S, Stamopoulos P, Schizas D, Zoe G, Terra A, Nikiteas N. Simultaneous robotic-assisted resection of colorectal cancer and synchronous liver metastases: a systematic review. J Robot Surg. 2021;15:841-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Machado MA, Mattos BH, Lobo Filho MM, Makdissi FF. Robotic Right Hepatectomy with Portal Vein Thrombectomy for Colorectal Liver Metastasis (with Video). J Gastrointest Surg. 2021;25:1932-1935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, Newcorn JH, Gignac M, Al Saud NM, Manor I, Rohde LA, Yang L, Cortese S, Almagor D, Stein MA, Albatti TH, Aljoudi HF, Alqahtani MMJ, Asherson P, Atwoli L, Bölte S, Buitelaar JK, Crunelle CL, Daley D, Dalsgaard S, Döpfner M, Espinet S, Fitzgerald M, Franke B, Gerlach M, Haavik J, Hartman CA, Hartung CM, Hinshaw SP, Hoekstra PJ, Hollis C, Kollins SH, Sandra Kooij JJ, Kuntsi J, Larsson H, Li T, Liu J, Merzon E, Mattingly G, Mattos P, McCarthy S, Mikami AY, Molina BSG, Nigg JT, Purper-Ouakil D, Omigbodun OO, Polanczyk GV, Pollak Y, Poulton AS, Rajkumar RP, Reding A, Reif A, Rubia K, Rucklidge J, Romanos M, Ramos-Quiroga JA, Schellekens A, Scheres A, Schoeman R, Schweitzer JB, Shah H, Solanto MV, Sonuga-Barke E, Soutullo C, Steinhausen HC, Swanson JM, Thapar A, Tripp G, van de Glind G, van den Brink W, Van der Oord S, Venter A, Vitiello B, Walitza S, Wang Y. The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 586] [Cited by in RCA: 658] [Article Influence: 164.5] [Reference Citation Analysis (0)] |
| 12. | Liu FH, Liu C, Gong TT, Gao S, Sun H, Jiang YT, Zhang JY, Zhang M, Gao C, Li XY, Zhao YH, Wu QJ. Dietary Inflammatory Index and Health Outcomes: An Umbrella Review of Systematic Review and Meta-Analyses of Observational Studies. Front Nutr. 2021;8:647122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Yan M, Chen J, Liu F, Li H, Huang R, Tang Y, Zhao J, Guo W. Disrupted Regional Homogeneity in Major Depressive Disorder With Gastrointestinal Symptoms at Rest. Front Psychiatry. 2021;12:636820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | D'Abate L, Delvecchio G, Ciappolino V, Ferro A, Brambilla P. Borderline personality disorder, metacognition and psychotherapy. J Affect Disord. 2020;276:1095-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Valkenburg PM, Meier A, Beyens I. Social media use and its impact on adolescent mental health: An umbrella review of the evidence. Curr Opin Psychol. 2022;44:58-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 198] [Article Influence: 66.0] [Reference Citation Analysis (0)] |
| 16. | Sarris J, Marx W, Ashton MM, Ng CH, Galvao-Coelho N, Ayati Z, Zhang ZJ, Kasper S, Ravindran A, Harvey BH, Lopresti A, Mischoulon D, Amsterdam J, Yatham LN, Berk M. Plant-based Medicines (Phytoceuticals) in the Treatment of Psychiatric Disorders: A Meta-review of Meta-analyses of Randomized Controlled Trials: Les médicaments à base de plantes (phytoceutiques) dans le traitement des troubles psychiatriques: une méta-revue des méta-analyses d'essais randomisés contrôlés. Can J Psychiatry. 2021;66:849-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | van Mersbergen M, Vinney LA, Payne AE. Cognitive influences on perceived phonatory exertion using the Borg CR10. Logoped Phoniatr Vocol. 2020;45:123-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Kamp IV, Loon JV, Droomers M, Hollander A. Residential Environment and Health: A Review of Methodological and Conceptual Issues. Rev Environ Health. 2021;19:381-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Weimann A, Braga M, Carli F, Higashiguchi T, Hübner M, Klek S, Laviano A, Ljungqvist O, Lobo DN, Martindale RG, Waitzberg D, Bischoff SC, Singer P. ESPEN practical guideline: Clinical nutrition in surgery. Clin Nutr. 2021;40:4745-4761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 348] [Article Influence: 87.0] [Reference Citation Analysis (0)] |
| 20. | Bogani G, Sarpietro G, Ferrandina G, Gallotta V, DI Donato V, Ditto A, Pinelli C, Casarin J, Ghezzi F, Scambia G, Raspagliesi F. Enhanced recovery after surgery (ERAS) in gynecology oncology. Eur J Surg Oncol. 2021;47:952-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 21. | Bollag L, Lim G, Sultan P, Habib AS, Landau R, Zakowski M, Tiouririne M, Bhambhani S, Carvalho B. Society for Obstetric Anesthesia and Perinatology: Consensus Statement and Recommendations for Enhanced Recovery After Cesarean. Anesth Analg. 2021;132:1362-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 183] [Article Influence: 45.8] [Reference Citation Analysis (0)] |
| 22. | Debono B, Wainwright TW, Wang MY, Sigmundsson FG, Yang MMH, Smid-Nanninga H, Bonnal A, Le Huec JC, Fawcett WJ, Ljungqvist O, Lonjon G, de Boer HD. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J. 2021;21:729-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 217] [Article Influence: 54.3] [Reference Citation Analysis (0)] |
| 23. | Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, Wellge EB, Kunzler F, Besselink MG, Asbun H, Scott MJ, Dejong CHC, Vrochides D, Aloia T, Izbicki JR, Demartines N. Guidelines for Perioperative Care for Pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) Recommendations 2019. World J Surg. 2020;44:2056-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 294] [Article Influence: 58.8] [Reference Citation Analysis (0)] |
| 24. | Stenberg E, Dos Reis Falcão LF, O'Kane M, Liem R, Pournaras DJ, Salminen P, Urman RD, Wadhwa A, Gustafsson UO, Thorell A. Correction to: Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations: A 2021 Update. World J Surg. 2022;46:752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK. Enhanced Recovery After Primary Total Hip and Knee Arthroplasty: A Systematic Review. J Bone Joint Surg Am. 2021;103:1938-1947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 98] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 26. | Zhou J, Du R, Wang L, Wang F, Li D, Tong G, Wang W, Ding X, Wang D. The Application of Enhanced Recovery After Surgery (ERAS) for Patients Undergoing Bariatric Surgery: a Systematic Review and Meta-analysis. Obes Surg. 2021;31:1321-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 27. | Hübner M, Kusamura S, Villeneuve L, Al-Niaimi A, Alyami M, Balonov K, Bell J, Bristow R, Guiral DC, Fagotti A, Falcão LFR, Glehen O, Lambert L, Mack L, Muenster T, Piso P, Pocard M, Rau B, Sgarbura O, Somashekhar SP, Wadhwa A, Altman A, Fawcett W, Veerapong J, Nelson G. Guidelines for Perioperative Care in Cytoreductive Surgery (CRS) with or without hyperthermic IntraPEritoneal chemotherapy (HIPEC): Enhanced Recovery After Surgery (ERAS®) Society Recommendations - Part II: Postoperative management and special considerations. Eur J Surg Oncol. 2020;46:2311-2323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 83] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 28. | de Boer HD, Demartines N. Invited Commentary: "Guidelines for Perioperative Care for Emergency: Laparotomy Enhanced Recovery After Surgery (ERAS) Society Recommendations Part 1-Preoperative: Diagnosis, Rapid Assessment and Optimization". World J Surg. 2021;45:1291-1292. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 29. | Dang JT, Szeto VG, Elnahas A, Ellsmere J, Okrainec A, Neville A, Malik S, Yorke E, Hong D, Biertho L, Jackson T, Karmali S. Canadian consensus statement: enhanced recovery after surgery in bariatric surgery. Surg Endosc. 2020;34:1366-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |