Published online Jul 27, 2023. doi: 10.4240/wjgs.v15.i7.1501
Peer-review started: February 4, 2023
First decision: March 14, 2023
Revised: March 28, 2023
Accepted: May 6, 2023
Article in press: May 6, 2023
Published online: July 27, 2023
Processing time: 167 Days and 6.5 Hours
Minimally invasive pancreatic surgery via the multi-port approach has become a primary surgical method for distal pancreatectomy (DP) due to its advantages of lower wound pain and superior cosmetic results. Some studies have applied reduced-port techniques for DP in an attempt to enhance cosmetic outcomes due to the minimally invasive effects. Numerous recent review studies have compared multi-port laparoscopic DP (LDP) and multi-port robotic DP (RDP); most of these studies concluded multi-port RDP is more beneficial than multi-port LDP for spleen preservation. However, there have been no comprehensive reviews of the value of reduced-port LDP and reduced-port RDP.
To search for and review the studies on spleen preservation and the clinical outcomes of minimally invasive DP that compared reduced-port DP surgery with multi-port DP surgery.
The PubMed medical database was searched for articles published between 2013 and 2022. The search terms were implemented using the following Boolean search algorithm: (“distal pancreatectomy” OR “left pancreatectomy” OR “peripheral pancreatic resection”) AND (“reduced-port” OR “single-site” OR “single-port” OR “dual-incision” OR “single-incision”) AND (“spleen-preserving” OR “spleen preservation” OR “splenic preservation”). A literature review was conducted to identify studies that compared the perioperative outcomes of reduced-port LDP and reduced-port RDP.
Fifteen articles published in the period from 2013 to 2022 were retrieved using three groups of search terms. Two studies were added after manually searching the related papers. Finally, 10 papers were selected after removing case reports (n = 3), non-English language papers (n = 1), technique papers (n = 1), reviews (n = 1), and animal studies (n = 1). The common items were defined as items reported in more than five papers, and data on these common items were extracted from all papers. The ten studies included a total of 337 patients (females/males: 231/106) who underwent DP. In total, 166 patients (females/males, 106/60) received multi-port LDP, 126 (females/males, 90/36) received reduced-port LDP, and 45 (females/males, 35/10) received reduced-port RDP.
Reduced-port RDP leads to a lower intraoperative blood loss, a lower postoperative pancreatic fistula rate, and shorter hospital stay and follow-up duration, but has a lower spleen preservation rate.
Core Tip: In contrast to recent review articles, this mini-review article is the first report to summarize all of the available evidence on spleen-preserving surgery with reduced-port robotic distal pancreatectomy (RDP) and laparoscopic distal pancreatectomy (LDP). Previous review articles only compared multi-port LDP with multi-port RDP. Our results show that conventional multi-port LDP has a shorter operating time than reduced-port LDP and reduced-port RDP. However, the reduced-port techniques result in less intraoperative blood loss; reduced-port RDP has the lowest blood loss. Moreover, reduced-port RDP leads to a lower postoperative pancreatic fistula rate and shorter hospital stay and follow-up duration, but a lower spleen preservation rate.
- Citation: Hsieh CL, Tsai TS, Peng CM, Cheng TC, Liu YJ. Spleen-preserving distal pancreatectomy from multi-port to reduced-port surgery approach. World J Gastrointest Surg 2023; 15(7): 1501-1511
- URL: https://www.wjgnet.com/1948-9366/full/v15/i7/1501.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i7.1501
Distal pancreatic resection is a useful surgical treatment for inflammatory or neoplastic pancreatic disorders in the body and tail of the pancreas[1]. Minimally invasive surgery (MIS) offers the advantages of lower wound pain and superior cosmetic results and has become a trend in diverse fields of surgery over the last two decades. Therefore, minimally invasive distal pancreatectomy (DP) has become popular[2].
The procedure for minimally invasive DP traditionally included splenectomy. However, removal of the spleen frequently results in sequelae such as infections, severe complications, and a higher risk of thromboembolism and post-splenectomy sepsis[3]. This issue prompted the development of minimally-invasive spleen-preserving DP, which has gained popularity as a surgical approach for the treatment of benign or low-grade malignant lesions of the distal pancreas[4,5].
Minimally invasive spleen-preserving DP can be performed through spleen-preserving laparoscopic DP (LDP) and spleen-preserving robotic DP (RDP). The benefits of robotic surgical systems include improved instrument dexterity, ergonomic surgical consoles, and 3D vision support that can greatly aid in complex dissection and surgical reconstruction during long and complex procedures[6]. As the main risk factor for spleen preservation failure is splenic vascular bleeding, LDP is less effective in controlling splenic vascular bleeding than RDP. Therefore, minimally invasive spleen-preserving DP has developed from LDP to RDP.
Compared to MIS with a multi-port surgery system, reduced-port MIS has the disadvantages of the fulcrum effect and a more limited range of motion and limited availability of instruments. However, with the increase in demand for minimally invasive procedures that reduce postoperative morbidity and improve quality of life, MIS approaches have attracted attention as they reduce the number of trocars and size of the ports; thus, the field of MIS has gradually expanded from simple surgery to complex surgery[7]. Recently, some studies employed reduced-port techniques for LDP and RDP with the aim of enhancing cosmetic outcomes through the use of minimally invasive effects[8,9].
Four review articles published in the past three years (2020-2022) have compared the advantages of multi-port LDP and multi-port RDP[10-13]. These studies highlighted the importance of providing readers with important summaries of LDP and RDP. However, there have been no comprehensive reviews of the value of reduced-port LDP and reduced-port RDP. Thus, this review study aimed to evaluate the safety and clinical outcomes of minimally invasive reduced-port LDP and RDP compared to multi-port LDP and RDP.
In order to retrieve eligible studies, the PubMed medical database was searched for articles published between 2013 to 2022. The search terms were implemented using the following Boolean search algorithm: (“distal pancreatectomy” OR “left pancreatectomy” OR “peripheral pancreatic resection”) AND (“reduced-port” OR “single-site” OR “single-port” OR “dual-incision” OR “single-incision”) AND (“spleen-preserving” OR “pleen preservation” OR “splenic preservation”).
A literature review was conducted to identify studies that compared the perioperative outcomes of reduced-port LDP and reduced-port RDP. The inclusion criteria were studies that: (1) Included patients undergoing DP for any disease; (2) Included procedures performed robotically or laparoscopically; (3) Reported data on patients undergoing DP with spleen preservation; and (4) Employed reduced-port or single-port or single-port plus one approaches. The exclusion criteria were case reports, reviews, non-English language papers, technique papers, and animal studies. Two surgeons (Peng CM and Hsieh CL) independently screened the papers by title and abstract to confirm the eligibility of each paper. In addition, the same two surgeons manually searched the references and related papers of the retrieved articles to find other eligible articles. Finally, the full texts of the selected references were reviewed for further analysis and data extraction.
Two surgeons (Peng CM and Hsieh CL) extracted data from each selected paper, including the first author, publication year, period of data collection, surgical procedure(s), number of trocars, number of patients, age, sex, body mass index (BMI), tumor size, conversion rate, blood loss, blood transfusion requirements, operating time, spleen preservation rate, rate of postoperative pancreatic fistula (POPF), complication rate, pain score, length of hospital stay, and length of follow-up. Different surgical approaches were compared using the average of means for factors with mean and standard deviation values, and the average of the standard deviation with unequal sample sizes. In addition, for studies that reported the individual data values, the mean and standard deviation values were computed to compare different types of surgery.
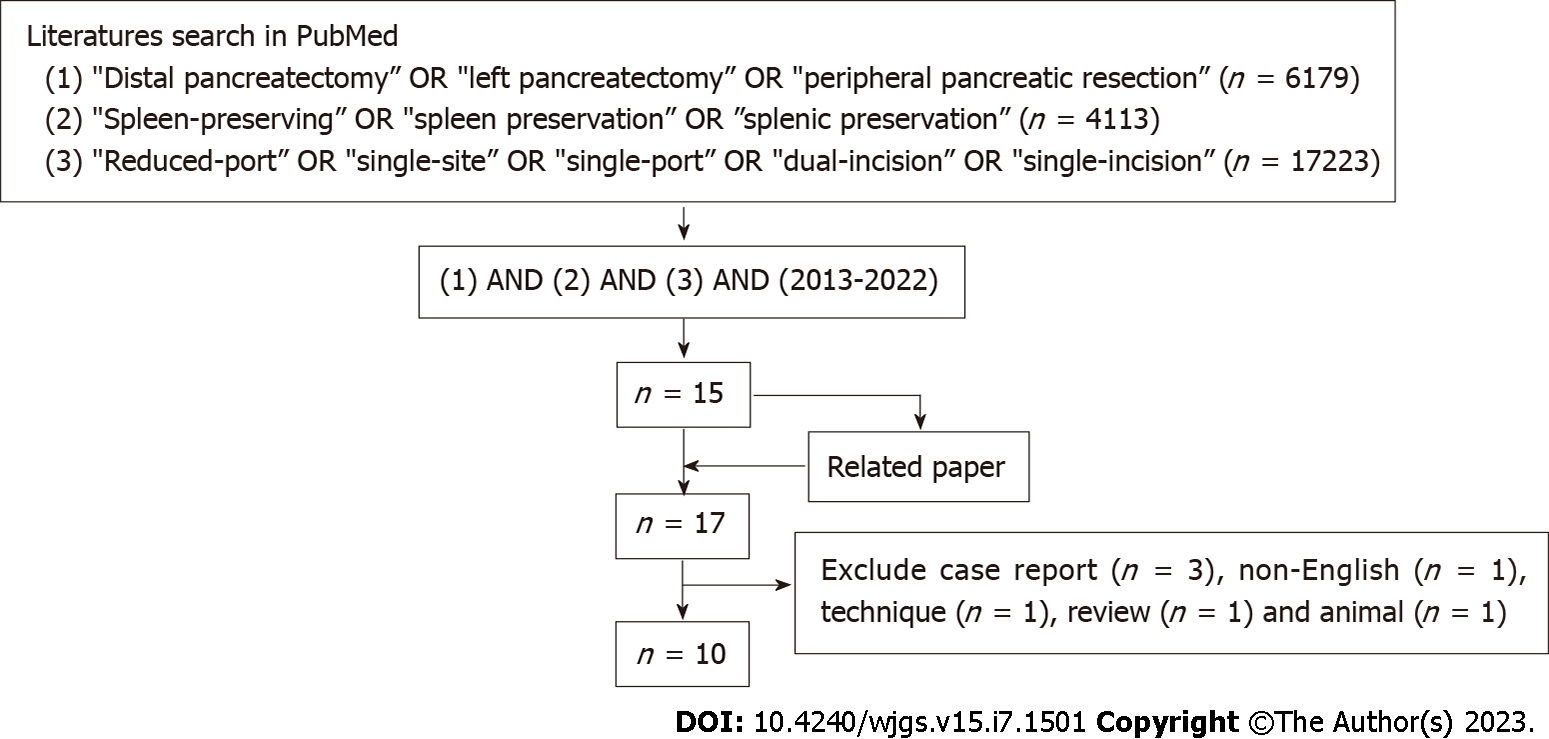
Figure 1 shows the flowchart of the selection of the included studies. A total of 6179 studies were retrieved by the Boolean search algorithm terms (“distal pancreatectomy” OR “left pancreatectomy” OR “peripheral pancreatic resection”); 4113 studies were retrieved using the terms (“spleen-preserving” OR “spleen preservation” OR “splenic preservation”); 17223 studies were retrieved using the terms (“reduced-port” OR “single-site” OR “single-port” OR “dual-incision” OR “single-incision”). A total of 15 articles published in the period from 2013 to 2022 were retrieved using all three groups of search terms. Two studies were added after manually searching the related papers. Finally, 10 papers were selected after removing case reports (n = 3), non-English language papers (n = 1), technique papers (n = 1), reviews (n = 1), and animal studies (n = 1)[14-23].
Ten eligible papers were included in this mini-review article. The common items were defined as items reported in more than five papers, and data on these common items were extracted from all papers. The ten studies included a total of 337 patients (females/males: 231/106) who underwent DP. In total, 166 patients (females/males, 106/60) received multi-port LDP, 126 (females/males, 90/36) received reduced-port LDP, and 45 (females/males, 35/10) received reduced-port RDP.
Table 1 Lists the included papers according to year of publication, along with the study number, year of publication, first author, period of data collection, type of surgery, number of trocars (mean and standard deviation), age (mean and standard deviation), and sex (number of patients). Table 2 Lists the included papers by surgical type. The mean and standard deviation BMI, operating time (min), blood loss (mL), tumor size (cm), length of hospital stay (days), and length of follow-up (months), as well as the spleen preservation rate, POPF rate, and complication rate, are also shown in Table 2. Only five papers reported the postoperative pain score; the mean and standard deviation postoperative pain scores are shown in Table 3.
| Study No. | Ref. | Period | Type of surgery | No. of trocars | M/F | Age |
| 1 | Yao et al[14], 2014 | 2009-2013 | RP_LDP | 1 | 0/11 | 38 ± 14.5 |
| 2 | Han et al [15], 2014 | 2007-2013 | MP_LDP | - | 11/17 | 49.1 ± 15.81 |
| RP_LDP | 1 | 2/10 | 61.3 ± 17.21 | |||
| 3 | Machado et al[16], 2015 | 2012-2014 | RP_LDP | 1 | 8/12 | 44.6 ± 13.4 |
| 4 | Kim et al[17], 2017 | 2015-2016 | RDP_SS+1 | 2 | 2/3 | 37 ± 14.7 |
| 5 | Sumer et al[18], 2017 | 2006-2013 | MP_LDP | 4 | 7/20 | 49.5 ± 14.9 |
| RP_LDP | 1 | 0/3 | 54.3 ± 13.6 | |||
| 6 | Ağcaoğlu et al[19], 2019 | 2007-2014 | MP_LDP | 5 | 3/7 | 48.2 ± 4.0 |
| RP_LDP | 1 | 4/6 | 43.5 ± 2.3 | |||
| 7 | Park et al[20], 2019 | 2012-2017 | MP_LDP | 4.4 ± 0.8 | 31/44 | 55.3 ± 14 |
| MP_LDP (propensity score matched) | 4.3 ± 0.5 | 9/17 | 55.2 ± 15.3 | |||
| RP_LDP | 1 | 9/17 | 60.0 ± 17.4 | |||
| 8 | Kim et al[21], 2019 | 2015-2018 | MP_LDP | 4.9 ± 0.3 | 8/18 | 55.3 ± 15.1 |
| RP_LDP | 2.7 ± 0.7 | 5/17 | 51.5 ± 17 | |||
| 9 | Han et al[22], 2019 | 2012-2018 | RP_LDP | 1.1 ± 0.2 | 8/14 | 58.3 ± 15.01 |
| RDP_SS+1 | 2.0 ± 0.7 | 3/10 | 46.1 ± 14.01 | |||
| 10 | Park et al[23], 2020 | 2015-2018 | RDP_SS+1 | 2 | 5/22 | 47.3 |
| Type | Study No. | BMI | OP time (min) | Blood loss (mL) | Tumor size (cm) | SP rate (%) | Complication rate (%) | Hospital stay (d) | Follow-up duration (mo) | Ref. | |
| POPF | Others | ||||||||||
| MP_LDP | 2 | 23.6 ± 4.0 | 186.9 ± 86.61 | 334 ± 468 | 3.4 ± 2.5 | 60.7 | 21.4 | 25 | 8.3 ± 4.71 | - | [15] |
| 5 | - | 163.3 ± 53.7 | - | - | 48.1 | 22.2 | 14.8 | 9.3 ± 6.6 | 30 ± 22.3 | [18] | |
| 6 | 31.2 ± 2.4 | 116.4 ± 14.11 | 110 (25-250) | 2.8 ± 0.6 | 50 | 30 | 10 | 10 | 56 | [19] | |
| 7 | 25.4 ± 4.3 | 182.6 ± 64.41 | 210 ± 384 | 3.1 ± 1.9 | 53.8 | 20 | 41.9 | 13.2 ± 9.4 | 27.4 ± 22.3 | [20] | |
| 7 (propensity score matched) | 22.9 ± 2.9 | 178.7 ± 66.61 | 114 ± 1811 | 2.7 ± 2.3 | 56 | 11.5 | 36 | 11.6 ± 8.8 | 30.6 ± 24.7 | [20] | |
| 8 | 24.7 ± 2.6 | 190.9 ± 43.71 | 282.7 ± 305.31 | 3.6 ± 2.1 | 65.4 | - | - | 8.0 ± 1.4 | - | [21] | |
| RP_LDP | 1 | 22.67 ± 1.9 | 163.18 ± 63.18 | 159.09 ± 181.02 | 3.85 ± 1.26 | 54.5 | 9.1 | 0 | 7.45 ± 1.44 | 25.8 ± 18.1 | [14] |
| 2 | 23.5 ± 4.6 | 279.8 ± 53.01 | 185 ± 125 | 3.8 ± 1.8 | 33.3 | 25 | 41.6 | 12.2 ± 5.41 | - | [15] | |
| 3 | - | 176.2 ± 59.6 | 77.5 ± 55.0 | 3.2 | 90 | 20 | 0 | 2.1 ± 1.2 | 11 | [16] | |
| 5 | - | 216.7 ± 100.2 | - | - | 0 | 66.6 | 33.3 | 13 ± 14.9 | 13 ± 1.7 | [18] | |
| 6 | 29.4 ± 3.1 | 180.4 ± 34.51 | 142 (30-500) | 2.2 ± 0.2 | 10 | 30 | 20 | 8 | 48 | [19] | |
| 7 | 23.6 ± 3.4 | 278.9 ± 51.81 | 205 ± 1971 | 3.3 ± 2.0 | 46.2 | 23.1 | 42.3 | 15.2 ± 11.4 | 20.8 ± 16.6 | [20] | |
| 8 | 25.2 ± 4.5 | 119.3 ± 50.41 | 96.8 ± 165.31 | 2.7 ± 1.8 | 95.5 | - | - | 7.7 ± 1.3 | - | [21] | |
| 9 | 23.9 ± 3.6 | 281 ± 521 | 163 ± 1971 | 3.0 ± 1.8 | 54.5 | 18.2 | 36.4 | 14.4 ± 12.31 | 23.4 ± 18.61 | [22] | |
| RDP_SS+1 | 4 | - | 203 ± 73.3 | 11 ± 21.9 | - | 40 | 0 | - | 6.8 ± 1.3 | - | [17] |
| 9 | 20.9 ± 4.0 | 192 ± 691 | 12 ± 221 | 2.7 ± 1.2 | 7.7 | 0 | 38.5 | 7.4 ± 1.91 | 7.8 ± 7.11 | [22] | |
| 10 | 22.6 | 173 | 50 | 3 | 34.6 | 23 | 3.8 | 7 | - | [23] | |
| Type | Study No. | Trocar No. | Postoperative pain score | Ref. | ||||
| 6 h | Day 1 | Day 2 | Day 3 | Day 5 | ||||
| MP_LDP | 6 | 5 | 4.5 ± 0.41 | 1.5 ± 0.5 | [19] | |||
| 7 | 4.4 ± 0.8 | 3.4 ± 1.11 | 3.4 ± 1.11 | 3.1 ± 0.91 | [20] | |||
| 7 (propensity score matched) | 4.3 ± 0.5 | 3.5 ± 0.91 | 3.3 ± 0.91 | 3.0 ± 0.91 | [20] | |||
| 8 | 4.9 ± 0.3 | 3.2 ± 1.4 | 3.5 ± 1.8 | 2.6 ± 1.31 | [21] | |||
| RP_LDP | 6 | 1 | 2.5 ± 0.31 | 1 ± 0.2 | [19] | |||
| 7 | 1 | 2.7 ± 0.81 | 2.5 ± 1.31 | 2.4 ± 1.41 | [20] | |||
| 8 | 2.7 ± 0.7 | 3.1 ± 1.1 | 2.8 ± 1.3 | 1.8 ± 0.91 | [21] | |||
| 9 | 1.1 ± 0.2 | 2.6 ± 0.9 | 2.3 ± 1.5 | [22] | ||||
| RDP_SS+1 | 9 | 2.0 ± 0.7 | 2.3 ± 1.2 | 2.5 ± 1.9 | [22] | |||
| 10 | 2 | 3 | 2 | 2 | [23] | |||
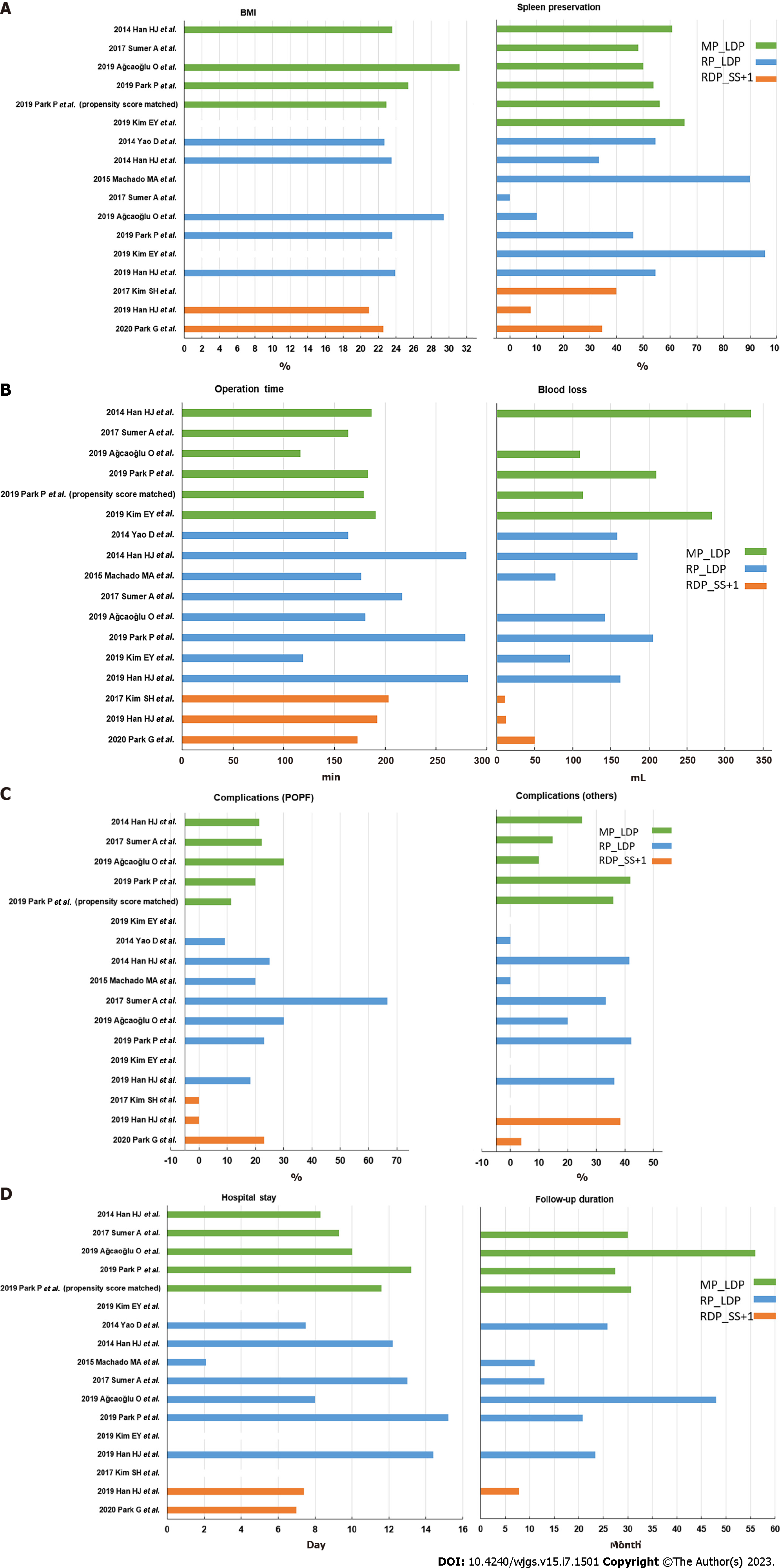
The average BMI and spleen preservation rate, operating time and blood loss, complication rate, and durations of hospital stay and follow-up reported in each paper are visually illustrated in Figure 2, respectively. Table 4 presents the average of the means and average of the standard deviation values of the factors including age, BMI, operating time, blood loss, tumor size, hospital stay, and follow-up duration for multi-port LDP (MP_LDP), reduced-port LDP (RP_LDP), and RDP with single-site plus one-port (RDP_SS+1). In addition, the mean and standard deviation of factors such as the spleen preservation rate and complication rate for MP_LDP, RP_LDP, and RDP_SS+1 are also listed in Table 4.
| Type | MP_LDP | RP_LDP | RDP_SS+1 | |
| Age | 51.5 ± 14.3 | 51.4 ± 15.3 | 43.5 ± 14.2 | |
| BMI | 26.2 ± 3.9 | 24.7 ± 3.7 | 21.8 ± 4 | |
| Operation time (min) | 168 ± 62.7 | 211.9 ± 54.2 | 189.3 ± 70.1 | |
| Blood loss (mL) | 234.2 ± 389.9 | 146.9 ± 165.1 | 24.3 ± 22 | |
| Tumor size (cm) | 3.2 ± 2 | 3.2 ± 1.7 | 2.9 ± 1.2 | |
| Spleen preservation rate (%) | 55.6 ± 7.3 | 48 ± 34 | 27.4 ± 17.3 | |
| Complication rate (%) | POPF | 23.4 ± 4.5 | 27.4 ± 18.4 | 7.7 ± 13.3 |
| Others | 23.0 ± 14.1 | 24.8 ± 18.5 | 21.2 ± 24.5 | |
| Hospital stay (d) | 9.8 ± 7.4 | 10 ± 8.2 | 7.1 ± 1.8 | |
| Follow-up duration (mo) | 37.8 ± 22.3 | 23.7 ± 17.3 | 7.8 ± 7.1 | |
To the best of our knowledge, this is the first review to summarize all of the available data on patients who underwent spleen-preserving DP using reduced-port robotic or reduced-port laparoscopic approaches. All other published review papers have focused on comparing the advantages and disadvantages of multi-port RDP vs multi-port LDP[10-13,24-27]. However, the relative value of reduced-port LDP and reduced-port RDP has not been fully reviewed. This topic is worthy of investigation because the appropriateness of the single-port technique in DP is receiving attention as all minimally invasive procedures are becoming increasingly technically demanding. We compared the patient data and outcomes of minimally invasive DP via the multi-port and reduced-port approaches for benign and malignant disorders of the pancreas. Our results show that conventional multi-port LDP has a shorter operating time than reduced-port LDP and reduced-port RDP; however, reduced-port RDP has a shorter operating time compared to reduced-port LDP. Moreover, reduced-port techniques are associated with lower intraoperative blood loss, with the lowest blood loss observed for reduced-port RDP. Moreover, reduced-port RDP had a lower POPF rate and shorter hospital stay and follow-up durations, but a lower spleen preservation rate.
Spleen removal can result in sequelae such as infections, severe complications, and a higher risk of thromboembolism and post-splenectomy sepsis[3]. Some studies have reported the benefits of spleen preservation including a lower rate of intra-abdominal abscesses[28], and prevention of overwhelming post-splenectomy infection[29] and cardiovascular complications[30]. The “Kimura-first” strategy is feasible and safe for robotic spleen-sparing DP and leads to a high rate of splenic vessel preservation[31]. The "Kimura-first" and "Warshaw-later" strategies are popular as they are time saving and have a lower POPF rate; however, compression of splenic vessels should be excluded before surgery. The “Kimura-first” strategy also requires careful examination to detect possible bleeding after splenic vessel dissection. However, proximal control of the splenic artery with vessel loops, which reduces the risk of bleeding and injury during dissection of the splenic artery and vein, is inefficient. Recently, the new Royal North Shore Technique, which places a vascular clamp on the splenic artery to reduce splenic artery inflow, has allowed for more accurate and injury-free dissection[32]. Thus, it is necessary to further evaluate the benefits of this technique in reduced-port DP.
Although the “Kimura-first and Warshaw-later” spleen-sparing strategy can be applied to both laparoscopic and robotic techniques, recent investigations[10,12,13] concluded the spleen preservation rate was higher for multi-port RDP than multi-port LDP due to the superior vessel manipulation. However, our review showed the spleen preservation rate is lower for reduced-port RDP than reduced-port LDP. This finding may be explained by several factors: firstly, the surgical field in reduced-port RDP is not large enough to allow effective movement during the spleen-preserving process[9]; secondly, only three studies assessed reduced-port RDP, and one of those studies had a spleen preservation rate of only 7.7% as the pancreatic tumors were abutting the splenic hilum in most patients[22]; and thirdly, the numbers of the learning curve in the three reduced-port RDP studies may not be sufficient, because even multi-port LDP and multi-port RDP had 25.3 and 20.7 cases to overcome the learning curve[33]. In addition, the spleen preservation rate is calculated as the ratio of the number of successful spleen preservation to the total number of operations in most studies. According to this definition, the spleen preservation rate is not only affected by the surgical method, but also by the patient’s condition and the preferences of the surgeon. Thus, the objective spleen preservation rate should be calculated based on the ratio of successful spleen preservation to those attempted spleen preservation before surgery[10]. Moreover, bias in patient selection between multi-port DP and reduced-port DP may also influence the complication and spleen preservation rates.
Our study indicates that reduced-port RDP leads to a lower rate of POPF than reduced-port LDP. One possible reason is that transection of the pancreatic tail is more completely performed by endovascular gastrointestinal anastomosis (endo-GIA) or robotic-assisted hand-sewn methods in reduced-port RDP. In previous studies, the suggested risk factors for POPF were BMI, pancreas thickness, and pancreatic texture[34]. A relatively long clamping time (> 2 min) during GIA decreases the water component in the pancreas and makes stapling more stable, and a long clamping time can be easily achieved using robotic assistance. The pancreas texture is easily identified through visual compensation and partly via instrument touch in robotic approaches. The hand-sewn method is more time consuming and labor intensive in the laparoscopic approach, but is easier when using the robotic approach.
The limitations of this study are the restricted inclusion period of 2013 to 2022, the fact that only three studies reported reduced-port RDP[17,22,23], and the absence of studies on multiport RDP. We limited the period of literature screening from 2013 to 2022 to control this review to studies with similar techniques and surgical devices. Even though robotic DP first emerged in 2010, only three studies of reduced-port RDP were identified in this review; many more studies have used multi-port or reduced-port LDP. We believe the current factors, the steep learning curve in reduced-port RDP for surgeons, and the high financial cost of robotic surgery, are the main factors that prevent surgeons from adopting robotic approaches. The small number of publications on reduced-port RDP mean the conclusions of this review should be considered as qualitative observations rather than a quantitative meta-analysis; however, this review provides information to compare multi-port LDP, reduced-port LDP, and reduced-port RDP. Although the lack of multi-port RDP studies in this review is due to the absence of studies that compared the outcomes of multi-port RDP with reduced-port RDP or LDP, data on multi-port RDP is available from systemic review studies to enable a comparison of multi-port LDP and multi-port RDP[10-13].
In conclusion, multi-port LDP, reduced-port LDP, and reduced-port RDP have all been proven to be safe and effective procedures, and the potential of reduced-port DP with spleen preservation has become an option for both benign and malignant pancreatic disorders. Further studies are needed to evaluate the value and efficacy of reduced-port RDP for spleen-preserving DP.
The application of minimally invasive approaches to distal pancreatic surgery has progressively increased over the last two decades.
Many studies have compared laparoscopic distal pancreatectomy (LDP) and robotic distal pancreatectomy (RDP), all of these studies only focused on multi-port LDP and multi-port RDP. However, there have been no comprehensive reviews of the value of reduced-port LDP and reduced-port RDP.
The purpose of this review study was to evaluate the safety and clinical outcomes of minimally invasive reduced-port LDP and RDP compared to multi-port LDP and RDP.
We searched for original manuscripts on minimally invasive reduced-port LDP and RDP, published from 2013 to 2022, in the PubMed database.
10 eligible papers including 337 patients, including 166 patients receiving multi-port LDP, 126 reduced-port LDP, and 45 reduced-port RDP, were considered appropriate for inclusion.
Reduced-port RDP is a safe and effective procedure and appears to offer some advantages over multi-port LDP and reduced-port LDP, but has a lower spleen preservation rate.
The insufficient learning curve may explain the lower spleen preservation rate of reduced-port RDP. Further studies are needed to evaluate the value and efficacy of reduced-port RDP for spleen-preserving distal pancreatectomy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Andrianello S, Italy; Chen N, China S-Editor: Yan JP L-Editor: A P-Editor: Wu RR
| 1. | Fernández-Cruz L. Distal pancreatic resection: technical differences between open and laparoscopic approaches. HPB (Oxford). 2006;8:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Adam MA, Choudhury K, Goffredo P, Reed SD, Blazer D 3rd, Roman SA, Sosa JA. Minimally Invasive Distal Pancreatectomy for Cancer: Short-Term Oncologic Outcomes in 1,733 Patients. World J Surg. 2015;39:2564-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002;137:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 239] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 4. | Yoon YS, Lee KH, Han HS, Cho JY, Ahn KS. Patency of splenic vessels after laparoscopic spleen and splenic vessel-preserving distal pancreatectomy. Br J Surg. 2009;96:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Hwang HK, Chung YE, Kim KA, Kang CM, Lee WJ. Revisiting vascular patency after spleen-preserving laparoscopic distal pancreatectomy with conservation of splenic vessels. Surg Endosc. 2012;26:1765-1771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Palep JH. Robotic assisted minimally invasive surgery. J Minim Access Surg. 2009;5:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 7. | Peng CM, Liu HC, Hsieh CL, Yang YK, Cheng TC, Chou RH, Liu YJ. Application of a commercial single-port device for robotic single-incision distal pancreatectomy: initial experience. Surg Today. 2018;48:680-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Kim EY, You YK, Kim DG, Lee SH, Han JH, Park SK, Na GH, Hong TH. Dual-incision laparoscopic spleen-preserving distal pancreatectomy. Ann Surg Treat Res. 2015;88:174-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Kang CM. Robotic single-site plus ONE-port distal pancreatectomy. Ann Pancreat Cancer. 2018;1. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Li P, Zhang H, Chen L, Liu T, Dai M. Robotic versus laparoscopic distal pancreatectomy on perioperative outcomes: a systematic review and meta-analysis. Updates Surg. 2023;75:7-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 11. | Rompianesi G, Montalti R, Ambrosio L, Troisi RI. Robotic versus Laparoscopic Surgery for Spleen-Preserving Distal Pancreatectomies: Systematic Review and Meta-Analysis. J Pers Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Mavrovounis G, Diamantis A, Perivoliotis K, Symeonidis D, Volakakis G, Tepetes K. Laparoscopic versus Robotic Peripheral Pancreatectomy: A Systematic Review and Meta-analysis. J BUON. 2020;25:2456-2475. [PubMed] |
| 13. | Chen C, Hu J, Yang H, Zhuo X, Ren Q, Feng Q, Wang M. Is robotic distal pancreatectomy better than laparoscopic distal pancreatectomy after the learning curve? A systematic review and meta-analysis. Front Oncol. 2022;12:954227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Yao D, Wu S, Tian Y, Fan Y, Kong J, Li Y. Transumbilical single-incision laparoscopic distal pancreatectomy: primary experience and review of the English literature. World J Surg. 2014;38:1196-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Han HJ, Yoon SY, Song TJ, Choi SB, Kim WB, Choi SY, Park SH. Single-port laparoscopic distal pancreatectomy: initial experience. J Laparoendosc Adv Surg Tech A. 2014;24:858-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Machado MA, Surjan RC, Makdissi FF. Laparoscopic Distal Pancreatectomy Using Single-Port Platform: Technique, Safety, and Feasibility in a Clinical Case Series. J Laparoendosc Adv Surg Tech A. 2015;25:581-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Kim SH, Kang CM, Lee WJ. Robotic single-site plus ONE port distal pancreatectomy. Surg Endosc. 2017;31:4258-4259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Sumer A, Barbaros U, Conde SM, Celik S, Aksakal N, Alamo JM, Alarcon I, Gures N, Karayagiz H, Dinccag A, Seven R, Mercan S, Budak D. Minimally invasive distal pancreatectomy A retrospective review of 30 cases. Ann Ital Chir. 2017;88. [PubMed] |
| 19. | Ağcaoğlu O, Aksakal N, Azamat İF, Doğan S, Mercan S, Barbaros U. Comparison of Clinical Outcomes of Single-Incision Versus Conventional Multiport Laparoscopic Distal Pancreatectomy: A Single Institution Experience. Sisli Etfal Hastan Tip Bul. 2019;53:114-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Park P, Han HJ, Song TJ, Choi SB, Kim WB, Yoo YD, Kim DS, Cha JH. Single-port versus conventional laparoscopic distal pancreatectomy: a propensity score matched analysis and a learning curve of single-port approach. J Hepatobiliary Pancreat Sci. 2019;26:401-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Kim EY, You YK, Kim DG, Hong TH. Dual-Incision Laparoscopic Spleen-Preserving Distal Pancreatectomy: Merits Compared to the Conventional Method. J Gastrointest Surg. 2019;23:1384-1391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Han HJ, Kang CM. Reduced port minimally invasive distal pancreatectomy: single-port laparoscopic versus robotic single-site plus one-port distal pancreatectomy. Surg Endosc. 2019;33:1091-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Park G, Choi SH, Lee JH, Lim JH, Lee H, Kang CM. Safety and Feasibility of Robotic Reduced-Port Distal Pancreatectomy: a Multicenter Experience of a Novel Technique. J Gastrointest Surg. 2020;24:2015-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Masuda H, Kotecha K, Gall T, Gill AJ, Mittal A, Samra JS. Transition from open to robotic distal pancreatectomy in a low volume pancreatic surgery country: a single Australian centre experience. ANZ J Surg. 2023;93:151-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 25. | Zhang X, Chen W, Jiang J, Ye Y, Hu W, Zhai Z, Bai X, Liang T. A comparison of robotic versus laparoscopic distal pancreatectomy: a single surgeon's robotic experience in a high-volume center. Surg Endosc. 2022;36:9186-9193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Chen P, Zhou B, Wang T, Hu X, Ye Y, Guo W. Comparative Efficacy of Robot-Assisted and Laparoscopic Distal Pancreatectomy: A Single-Center Comparative Study. J Healthc Eng. 2022;2022:7302222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 27. | van Ramshorst TME, Giani A, Mazzola M, Dokmak S, Ftériche FS, Esposito A, de Pastena M, Lof S, Edwin B, Sahakyan M, Boggi U, Kauffman EF, Fabre JM, Souche RF, Zerbi A, Butturini G, Molenaar Q, Al-Sarireh B, Marino MV, Keck T, White SA, Casadei R, Burdio F, Björnsson B, Soonawalla Z, Koerkamp BG, Fusai GK, Pessaux P, Jah A, Pietrabissa A, Hackert T, D'Hondt M, Pando E, Besselink MG, Ferrari G, Hilal MA; European Consortium on Minimally Invasive Pancreatic Surgery. Benchmarking of robotic and laparoscopic spleen-preserving distal pancreatectomy by using two different methods. Br J Surg. 2022;110:76-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 28. | Lee W, Hwang DW, Han HS, Han IW, Heo JS, Unno M, Ishida M, Tajima H, Nishizawa N, Nakata K, Seyama Y, Isikawa Y, Hwang HK, Jang JY, Hong T, Park JS, Kim HJ, Jeong CY, Matsumoto I, Yamaue H, Kawai M, Ohtsuka M, Mizuno S, Asakuma M, Soejima Y, Hirashita T, Sho M, Takeda Y, Park JI, Kim YH, Yamamoto M, Endo I, Nakamura M, Yoon YS. Comparison of infectious complications after spleen preservation versus splenectomy during laparoscopic distal pancreatectomy for benign or low-grade malignant pancreatic tumors: A multicenter, propensity score-matched analysis. J Hepatobiliary Pancreat Sci. 2023;30:252-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 29. | Sinwar PD. Overwhelming post splenectomy infection syndrome - review study. Int J Surg. 2014;12:1314-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 30. | Weledji EP. Benefits and risks of splenectomy. Int J Surg. 2014;12:113-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 126] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 31. | Lin X, Lin R, Lu F, Yang Y, Wang C, Fang H, Huang H. "Kimura-first" strategy for robotic spleen-preserving distal pancreatectomy: experiences from 61 consecutive cases in a single institution. Gland Surg. 2021;10:186-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Damodaran Prabha R, Kotecha K, Mittal A, Samra JS. The Robotic Spleen Preserving Distal Pancreatectomy Under Temporary Splenic Artery Occlusion: the Royal North Shore Technique. J Gastrointest Surg. 2021;25:1936-1938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 33. | Chan KS, Wang ZK, Syn N, Goh BKP. Learning curve of laparoscopic and robotic pancreas resections: a systematic review. Surgery. 2021;170:194-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 34. | Kim H, Jang JY, Son D, Lee S, Han Y, Shin YC, Kim JR, Kwon W, Kim SW. Optimal stapler cartridge selection according to the thickness of the pancreas in distal pancreatectomy. Medicine (Baltimore). 2016;95:e4441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |