Published online Jul 27, 2023. doi: 10.4240/wjgs.v15.i7.1277
Peer-review started: December 27, 2022
First decision: February 20, 2023
Revised: March 2, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: July 27, 2023
Processing time: 205 Days and 20.1 Hours
Advancements in technology and surgical training programs have increased the adaptability of minimally invasive surgery (MIS). Gastrointestinal MIS is superior to its open counterparts regarding post-operative morbidity and mortality. MIS has become the first-line surgical intervention for some types of gastrointestinal surgery, such as laparoscopic cholecystectomy and appendicectomy. Carbon dioxide (CO2) is the main gas used for insufflation in MIS. CO2 contributes 9%-26% of the greenhouse effect, resulting in global warming. The rise in global CO2 concentration since 2000 is about 20 ppm per decade, up to 10 times faster than any sustained rise in CO2 during the past 800000 years. Since 1970, there has been a steady yet worrying increase in average global temperature by 1.7 °C per century. A recent systematic review of the carbon footprint in MIS showed a range of 6-814 kg of CO2 emission per surgery, with higher CO2 emission following robotic compared to laparoscopic surgery. However, with superior benefits of MIS over open surgery, this poses an ethical dilemma to surgeons. A recent survey in the United Kingdom of 130 surgeons showed that the majority (94%) were concerned with climate change but felt that the lack of leadership was a barrier to improving environmental sustainability. Given the deleterious environmental effects of MIS, this study aims to summarize the trends of MIS and its carbon footprint, awareness and attitudes towards this issue, and efforts and challenges to ensuring environmental sustainability.
Core Tip: Many minimally-invasive surgeries (MIS) have better post-operative outcomes than their open counterparts. However, MIS requires using carbon dioxide to achieve pneumoperitoneum, sterilization, and production and disposal of equipment. Concerns over the iatrogenic transmission of infectious diseases have led to the preference for disposable equipment; however, disposable equipment has higher carbon footprints than reusable ones. This review summarizes the impact of MIS on carbon footprints, awareness and attitudes of relevant stakeholders towards environmental sustainability, and challenges in reducing carbon footprint in MIS.
- Citation: Chan KS, Lo HY, Shelat VG. Carbon footprints in minimally invasive surgery: Good patient outcomes, but costly for the environment. World J Gastrointest Surg 2023; 15(7): 1277-1285
- URL: https://www.wjgnet.com/1948-9366/full/v15/i7/1277.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i7.1277
The introduction of minimally invasive surgery (MIS) has revolutionized surgical practice. Advancements in technology and the incorporation of MIS techniques into surgical training have changed surgical teaching. General benefits of MIS include lower post-operative morbidity such as wound infection, reduced pain score, better cosmesis, and reduced length of hospitalization stay (LOS)[1]. Minimally invasive gastrointestinal surgery (MIGS) has been shown to have these benefits compared to open surgery in many benign and malignant conditions in upper gastrointestinal, hepatopancreatobiliary, and colorectal disorders[2-4]. This is true even in emergency settings, such as appendicectomy, cholecystectomy, repair of perforated peptic ulcer (PPU) or emergency colorectal surgery[5,6].
Carbon dioxide (CO2) is the main gas used in MIS for insufflation. While direct CO2 emission is the obvious source of greenhouse gases (GHG), MIS also contributes indirectly to carbon footprint through the generation of waste, use of additional medical devices, and consumption of electricity (measured via the proxy of operative duration). Singh et al[7] in proposing a mandatory adoption of a standard set of metrics across the United States Health Care, recommended the classification of such emissions into 3 baskets: (1) Direct emissions; (2) Indirect emissions via purchased electricity; and (3) Indirect emissions via a myriad of other categories, including waste management, medicines, medical devices, etc.
CO2 is a key contributor to global warming, accounting for 9%-26% of the greenhouse effect[8]. Global CO2 emissions increased by 1.6% annually from 1970 to 2003, and accelerated to 3.2% annually from 2003 to 2011 due to rapid industrialization in China[9]. According to the National Centers for Environmental Information’s 2021 Annual Climate Report, there had been an annual increase of 0.18 ºC in global temperature since 1981, with 2021 being the sixth warmest year on record[10]. Additionally, concerns over iatrogenic transmission of infectious diseases have led to the transition from reusable to disposable surgical instruments[11,12].
There is emerging evidence that while patients reap the benefits of MIS, the healthcare industry has become a major contributor to global carbon emissions. A report in 2018 found that a sizeable 9%-10% of carbon emissions arose from healthcare in the United States[13]. Another report demonstrated 4%-5% of the United Kingdom’s carbon emissions occurred from the National Health Service[14]. However, how much of this increase in CO2 emissions is due to MIS? A recent systematic review including eight articles reported a wide variation in CO2 emissions [range 6-814 kg CO2 equivalents (CO2e)] for various surgeries, with higher CO2 emission in robotic surgery compared to laparoscopic surgery[15]. Alongside the increasing trend of MIS in recent years due to increasing availability of technology and growing evidence of its superiority, there is a pressing need to review literature on the carbon footprint in MIS. Operation theatres contribute 3-6 times more towards carbon footprint compared to other areas of a hospital[16]. This is a growing concern and a call for environmental sustainability has been made by various surgical organizations. This narrative review aims to summarize literature on the CO2 emissions of the various types of MIGS and the awareness and attitude of the surgical community towards the environmental sustainability of MIGS. We also aim to review the challenges and efforts put into place to achieve environmental sustainability in MIGS.
While the initial aim of this review was to summarize the existing literature on CO2 emissions in MIGS, there is a paucity of scientific data about carbon footprints in MIGS specifically. Hence, this review will instead summarize evidence in MIS as a whole.
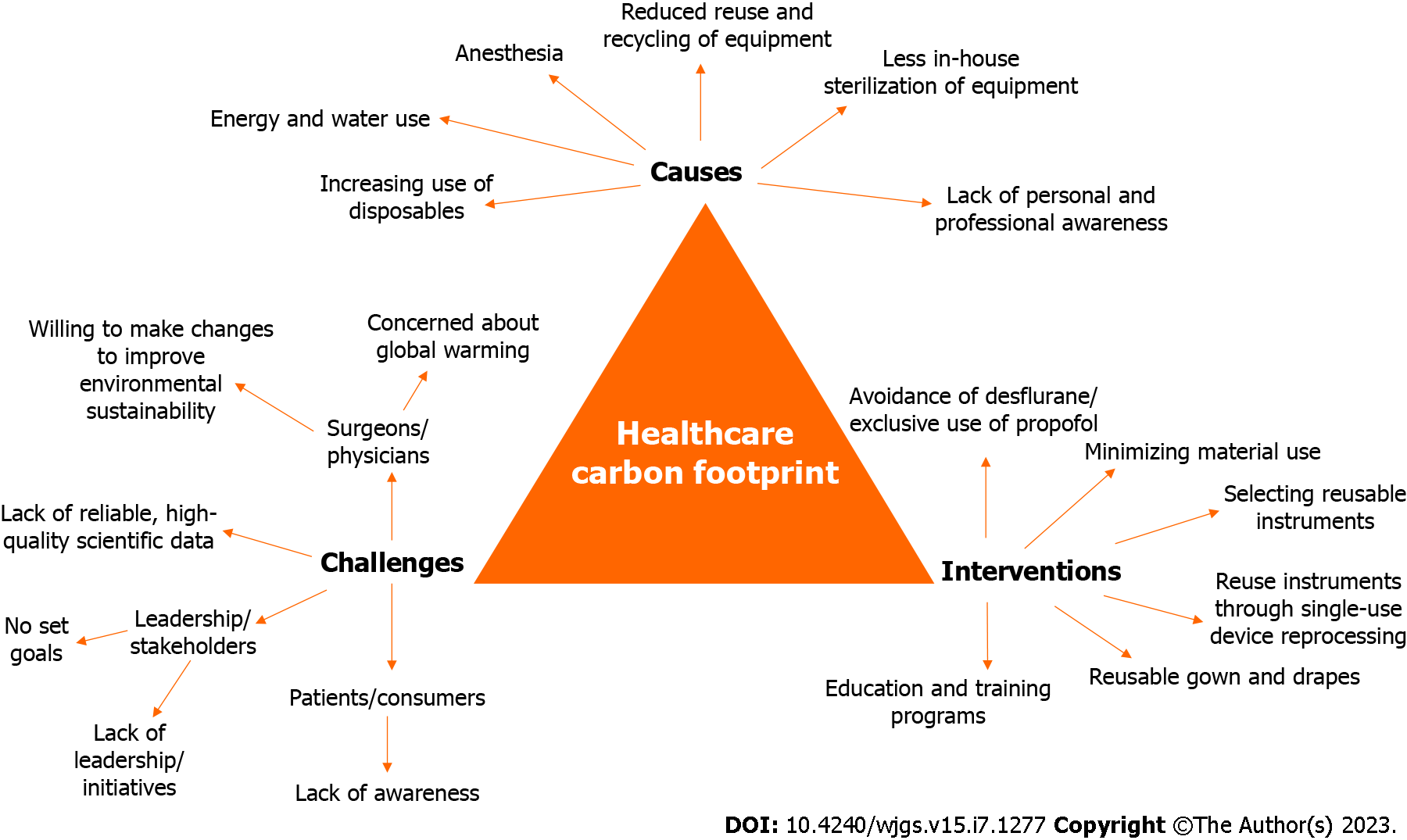
The literature on carbon footprints is summarized by the recent systematic review on laparoscopic and robotic surgery[17]. Out of the six included studies, three studies were on gynaecological procedures[18-20], two were on a variety of procedures (gastrointestinal, gynaecological, urological etc.)[21,22], and one was on minimally invasive phaecoemulsification[23]. Regarding the type of MIS (laparoscopy vs robotic), two studies exclusively reported on laparoscopy[19,22], three studies included a mix of robotic and laparoscopic surgeries[18,20,21], and one study was on phaecoemulsification[23]. The carbon emission from MIS is not limited to only using CO2 for insufflation. In line with the recommended metrics by Singh et al[7], other categories of carbon emissions should also be tracked; sources of carbon emissions are present at all stages of MIS, starting from the production of disposables, energy and water use, anesthesia, to recycling, sterilization and disposal of equipment. Figure 1 summarizes the causes, awareness and challenges, and interventions to help reduce carbon footprint in MIS. Among the six included studies in the review by Papadopoulou et al[17], cataract phaecoemulsification had the least carbon emission of 6 kg CO2e per case[23], while robotic hysterectomy had the highest of 814 kg CO2e per case, which is about 135 times that of phaecoemulsification[18]. To put things into perspective, 150-170 kg CO2e is equivalent to driving 450 miles (724.2 km) with an average petrol car[15]. Hence, a single robotic hysterectomy which produces 814 kg CO2e is equivalent to driving about 2289.4 miles (3684.4 km) using an average petrol car[15,17].
We will discuss a few issues related to the environmental sustainability of MIS. Firstly, it is apparent that data and science related to computing carbon footprint in healthcare are in their infancy and imperfect at best. Secondly, a particular surgery’s carbon footprint is determined by the operation theatre’s processes, procedures and protocols, and preoperative and postoperative care processes that a patient passes through. Regarding a certain surgery, there is no single “one size fits all” number on the CO2e per case as the emissions are determined by operating time, consumables used, disposable items used, and deviations from normal surgical conduct (for example open conversion). About 15 million laparoscopic procedures are performed annually globally, with increasing use of single-use devices[24]. The fear of iatrogenic spread of infectious diseases fuels this transition towards single-use devices; Creutzfeld-Jacob Disease is an incurable and fatal neurodegenerative disease which may be transmitted despite standard sterilization processes[25]. Additionally, the ongoing highly contagious coronavirus disease 2019 (COVID-19) pandemic raises concerns about the use of reusable instruments. The Endoscopic and Laparoscopic Surgeons of Asia expert review recommends the use of disposable instruments where possible due to the risk of iatrogenic transmission[12].
Boberg et al[24] employed the life cycle assessment method to evaluate and compare the environmental impacts of single-use, reusable, and mixed trocar systems used for laparoscopic cholecystectomies at three Swedish hospitals and concluded that reusable instruments reduce both the environmental impact and financial costs for laparoscopic surgery compared to their disposable counterparts. A study by Rizan and Bhutta[26] on laparoscopic instruments used in laparoscopic cholecystectomy showed that the carbon footprint for a laparoscopic hybrid instrument compared to a single-use equivalent was 17% for a clip applier, 33% for scissors, and 27% for four ports. Use of a combination of hybrid laparoscopic clip appliers, scissors and ports for a single laparoscopic cholecystectomy also showed overall better environmental sustainability [reduction of 74% in disability-adjusted life years (DALYs), 76% in loss of local species per year, and 78% in impact on resource depletion][26]. A systematic review by Drew et al[27] similarly demonstrated that disposable equipment was associated with higher environmental impacts than reusable equipment. Conrardy et al[28] demonstrated potential cost savings of an average of 65% by using reusable basins, gowns, back table covers and mayo stand covers instead of single-use ones.
In view of environmental and cost concerns, institutions may have made the transition back from disposable to reusable instruments. Adequate sterilization is however necessary to eliminate the risk of iatrogenic transmission of infectious diseases. Use of steam is the commonest form of surgical sterilization[29]. Both electricity and water are required to power steam sterilizers when on standby, or active. McGain et al[30] reported considerable proportion of electricity (40%) and water (20%) used even when the steam sterilizer was on standby. They also reported that low sterilization load (< 15 kg) was less energy efficient, but was commonly used (about 1 in 3). Institutions need to be cognizant of the above, and factor this when considering the use of reusable instead of disposable equipment. Other methods of sterilization include the use of ethylene oxide (EO) or glutaraldehyde. EO is preferred over steam sterilization for instruments which cannot withstand high temperature and steam. Glutaraldehyde remains a relatively effective and inexpensive method of chemical sterilization, but poses occupational health hazards[31]. However, both methods similarly produce CO2 emissions[31,32]. Additionally, EO may have carcinogenic potential and poses occupational risks, though this risk is minimal with regulations on the safe use of EO[31]. Discussion on occupational health hazards however fall beyond the scope of this review.
CO2, which is a contributor of GHG emissions, is a widely used gas for abdominal insufflation as it is inexpensive, colourless, non-flammable and has higher blood solubility than air (i.e., lower risk of CO2 embolism)[33]. CO2 is absorbed by the peritoneum and delivered to the lungs via blood circulation, and undergo gaseous exchange[34]. However, CO2 is detrimental to both the environment and patient (e.g., hypercapnia, acidosis and cardiac arrhythmia)[35]. Other gases such as helium, argon, nitrogen and nitrous oxide have been introduced as alternatives for achieving pneumoperitoneum. Helium, argon and nitrogen are not GHGs and do not contribute to global warming. However, there is a lack of conclusive evidence on the safety of the use of those gases for abdominal insufflation and still requires further research[36].
Technological advancements have also revolutionized laparoscopic surgery and allowed the use of single-incision laparoscopic surgery (SILS)/single-port laparoscopic surgery (SPLS) in both benign and malignant diseases; SILS/SPLS is associated with better cosmesis, reduced LOS, shorter time to first flatus/diet and lesser post-operative pain[37-39]. While there are no studies reporting the carbon footprint of reusable single-ports, we postulate that this may reduce carbon footprint due to reduced quantity of instrument used. Operating time, complexity of surgery and hospital surgical volume are also important culprits for carbon emissions. Complex surgeries require longer operating time; tertiary specialized centers have higher caseloads and also perform more complex operations due to availability of subspecialty services and technical capabilities. A greater volume of anesthesia gas and CO2 (used for abdominal insufflation) is required. Anesthesia gas has been shown to be the primary source of carbon footprint in some institutions[16].
The introduction of energy devices in MIS has also changed surgical practice; they can be used for dissection, coagulation, and resection of tissues. Some energy devices are favored for coagulation of tissue with minimal injury to surrounding structures (e.g., ultrasonic devices), while other devices are favored for haemostasis (e.g., bipolar electrocautery devices). However, thermal destruction of tissues results in the production of surgical smoke. Beebe et al[40] showed that electrocautery of tissue during laparoscopic cholecystectomy produced a median concentration of 345 ppm of carbon monoxide 5 min after the use of electrocautery. CO2 has also been shown to be present in surgical smoke[41]. Extensive dissection/coagulation of tissue will result in excessive surgical smoke production which may obscure surgeons’ vision and will need to be released externally from the intra-peritoneal cavity; this contributes to GHG and global warming. Use of larger trocars (e.g., 10-mm) and manipulation of trocars during insertion of laparoscopic instruments also result in gas leak[42]. Additionally, surgeons may practice continuous low suction of smoke to improve laparoscopic vision, but this will result in more CO2 use and waste.
Lastly, while both laparoscopic and robotic surgery are MIS, robotic surgery has been shown have superior short-term outcomes (e.g., reduced intra-operative blood loss, shorter LOS)[43]. This may be due to more precise movements (elimination of hand tremors)[44], depth perception, and prior surgical experience (surgeons performing robotic surgery usually have experience in laparoscopic surgery first)[45]. However, this comes with a cost; robotic surgery is also associated with increased carbon footprint. Thiel et al[18] showed that robotic hysterectomy had 43.5% higher GHG emissions compared to laparoscopic hysterectomy, and Woods et al[20] showed that robot-assisted endometrial cancer staging has 38% higher CO2e vs traditional laparoscopy. One contributing factor may be due to increased operating time in robotic surgery[43]. However, Thiel et al[18] showed that the production of disposables (e.g., gowns, bluewrap, drapes and film packaging wrappers) was the main contributor to multiple environmental impacts in robotic hysterectomy. Additionally, another reason for increased carbon footprint in robotic surgery may be due to the limited lifespan of instruments. The most commonly used robotic surgical system is the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, United States of America). However, the robotic instruments are preset for 10 uses regardless of the length of use or the type of task performed[46]. To add on, surgeons may replace instruments prematurely should there be sub-optimal performance. A study by Ludwig et al[47] on robot-assisted laparoscopic radical prostatectomy found that there was premature exchange of monopolar curved scissors in 12.4% of all cases, while the exchange rate for Prograsp forceps, large needle drivers and fenestrated bipolar forceps were less than 2%. This may be due to the nature of the instruments; scissors are required for surgical dissection. Excessive use may result in wear and tear of the scissors, resulting in poor performance and warrant the need for early exchange. To add on, information is limited on the arbitrary number of “10” uses per instrument[48]. With low exchange rates, it is possible that the instruments may be used for more than stipulated “10 cases” without patient risk.
On top of the above information presented on the contributors towards carbon emissions in MIS, it is also important to understand its clinical impact. DALY and quality adjusted life year (QALY) are two common indicators used to measure disease burden in a population. DALY is defined as the sum of years lost due to premature mortality and years lived with disability due to the prevalent cases of the disease or health condition[49]. QALY is defined using a quality of life score estimated using the years of life remaining for a patient following a particular treatment or intervention[50]. One DALY is defined as the loss of equivalent of one year of full health, and one QALY is defined as one year of perfect health.
Using the 2013 United States healthcare sector life cycle emissions, the life cycle GHG emissions associated with United States health care activities was estimated to cause an additional 123000 to 381000 DALYs annually[13]. The main complications of climate change resulting in DALYs were malnutrition (49%-63%), which is of greatest concern in agricultural areas located on floodplains or lack irrigation. Other main contributors to total DALYs were increased incidence of malaria and diarrhoea, due to lengthening of warm seasons and expanding geographic range of disease factors[13]. Looking into procedure-specific DALY, Papadopoulou et al[17] performed a speculative analysis of the DALYs averted in 10 years post-surgery per ton of CO2e or waste produced. Expectedly, DALY averted was the highest in surgeries with low carbon and material footprint, since this would correlate to more surgeries performed per tonne of CO2e or waste produced. Phaecoemulsification had 125 DALYs and 3420 DALYs averted per tonne of CO2 and waste respectively[23]. Robot-assisted hysterectomy, which had the highest CO2e, had the lowest benefit, with 2 DALYs and 72 DALYs averted per tonne of CO2 and waste respectively[18].
Increasing research on environmental sustainability has shown the impact of MIS on carbon footprints and global warming. Environmental sustainability is a global issue which may not be directly felt or perceived by an individual. Stakeholders and surgical staffs should be aware of the environmental impact of MIS. A survey on 130 surgeons and surgical trainees in the United Kingdom and Ireland showed that majority (94%) of respondents were concerned about the threat of climate change[51]. Most of the respondents were also willing to make changes to their clinical practice to improve environmental sustainability[51]. This is in alignment with the ethical principle of precaution, suggesting high moral values of respondents. However, this is confounded by the fear of changing from the “norm” of surgical practice - for instance, disposable equipment is generally preferred to reusable equipment due to the fear of iatrogenic transmission of diseases, especially during the COVID-19 pandemic[12,25]. Industries tap on this fear to manufacture the required products. Individual surgeons do not feel the financial burden from institutional purchase of equipment, since these are covered by their institutions. This leads to a vicious cycle of rising GHG emissions and healthcare costs. Currently, reporting of GHG emissions is voluntary in the United States and there is no standardized set of metrics for monitoring GHG emissions and setting a benchmark on what is deemed “acceptable” for healthcare institutions[7]. Mandatory reporting of carbon footprint will allow tracking and auditing of additional costs incurred[7]; Trinks et al[52] showed that on average, 0.1% higher carbon efficiency is associated with 1.0% higher profitability. This will instead motivate industries to shift towards reducing carbon footprint.
A survey on 166 obstetrics and gynaecology (ObGyn) physicians (attending surgeons, fellows and trainees) in the United States showed that 84% of ObGyn physicians were concerned about global warming. While results shown by the surveys are optimistic, with majority of surgeons feeling the threat of global warming, it is however still concerning that there is a sizable number of respondents who felt that global warming is not of concern (range 4%-16% in the surveys by Harris et al[51] and Thiel et al[53]). Similarly, on top of stakeholders, consumers should also be aware of the environmental impact of MIS. The same survey by Thiel et al[53] compared ObGyn physicians with the general population in United States; they showed that the general population was less likely to believe that global warming is a concern compared to ObGyn physicians (54% vs 84%, P < 0.001).
However, efforts to improve environmental sustainability should not be limited to clinical practice and lies on the responsibility of every individual. It is promising to know that most surgeons and surgical trainees surveyed changed their routines and practices in their personal lives to improve environmental sustainability[51]. In line with this, the Royal College of Surgeons of United Kingdom and Ireland has recently proposed a “Green Theatre Checklist” comprising of four elements - anesthetic care, preparation for surgery, intraoperative practice and postoperative measures - to be conducted at the start of operation[54]. The preoperative checklist items include using reusable textiles, reducing water use for hand scrub, reducing unnecessary procedures (e.g., antibiotic administration or urine catheterization) or ordering unnecessary investigations (e.g., histology or microbiology). The intraoperative checklist items include review and rationalise (surgeon preference lists, instrument sets etc.), reduce (“don’t open it unless you need it”), reuse, and replace (sutures vs clips). The postoperative checklist items include recycle (waste disposal), repair (rather than discard and throw reusable items) and power off (lights, computers, etc.).
The United Nations Educational, Scientific and Cultural Organization Declaration on the Responsibility of the Present Generations Towards Future Generations was adopted in November 1997[55]; article 4 describes the need for preservation of life on Earth, while article 5 describes the need for protection of the environment. For instance, article 5 states that “In order to ensure that future generations benefit from the richness of the Earth’s ecosystems, the present generations should strive for sustainable development and preserve living conditions, particularly the quality and integrity of the environment”. In the context of surgical advancements, developments in MIS have led to improvement in patient outcomes. However, this development needs to be sustainable to ensure that future generations continue to benefit.
While every individual plays a part in ensuring environmental sustainability, changes in practices need to be supported by institutional efforts. The survey by Harris et al[51] showed that a large proportion (70%) of 130 respondents (surgeons and surgical trainees) felt that there was a lack of leadership to help improve environmental sustainability. We described causes of carbon footprints in the above section: From the production of disposables, energy and water use, type of anesthesia, to recycling, sterilization and disposable of equipment. Interventions may be employed at any stage to reduce carbon footprints.
Thiel et al[19] analysed various interventions to reduce the carbon footprint in laparoscopic hysterectomy; they showed that exclusive use of propofol for anesthesia generates a 28% reduction in GHG emissions. Similarly, MacNeill et al[16] showed that avoidance of desflurane as an anesthetic agent resulted in nearly 90% reduction in GHG emissions. Other interventions include minimizing material use and selecting reusable surgical instruments (except for ports and insufflator) (about 50% GHG reduction) and reuse of surgical instruments through single-use device reprocessing (about 10% GHG reduction)[19]. In addition, vaporized hydrogen peroxide (VHP) sterilization has been shown to be effective in a prospective in-vitro animal experiment; Scharf et al[56] inoculated ports, cannulas, and tubing with Staphylococcus pseudintermedius and Escherichia coli to determine the sterilization ability of VHP and found no difference in bacteriological scores between treated ports, cannulas, and insufflation tubing and the negative control port and components; and concluded that in veterinary patients, a single-use single-incision laparoscopic port and its associated components can be effectively sterilized by using VHP.
Reuse of disposable items is common in many middle- and low-income healthcare systems to reduce healthcare costs, so much so that it is an acceptable norm to do so. It is not the purpose of this review to propose a shift in culture of high-income healthcare systems, but to stimulate the rational thinking, if it is worthwhile to dispose an item over the remote risk of fluid-borne disease transmission. If we can ration resources and prioritize care delivery during a pandemic, we can do the same for elective endemic issues too. There is very little scientific data to determine if reusable laparoscopic instruments are safe. Siu et al[57] conducted a systematic review on reusable and disposable laparoscopic equipment and concluded that cost-saving methods, environmental-friendly methods, global operative costs, hidden costs, sterilization methods and quality assurance systems vary greatly between studies; this makes it difficult to compare between single-use and reusable instruments. While there are other causes of carbon footprints, such as the production of disposables and disposable of equipment, these interventions (maximizing recycling, minimizing regulated medical waste and using reusable gown and drapes) have been shown to have minimal reduction (< 5%) in GHG emissions[19]. The reuse of instruments does not result in loss of instrument effectiveness or ease-of-use until a certain threshold limit; reusing equipment in general is also not considered unsafe practice. In laparoscopic bariatric surgery patients, Yung et al[58] reported that reusable ultrasonic shears had cost savings that increased with the number of cases without negatively affecting complication rate and ease-of-use.
The above discussed measures have more apparent and “direct” impact on reducing carbon footprint. However, there are other “indirect” ways of reducing carbon footprints in surgery. Administration of prophylactic antibiotics is recommended about 30 to 60 min prior to skin incision to reduce the risk of post-operative surgical site infections[59]. The use of prophylactic antibiotics for some surgical conditions, however, has not been well-established. For instance, evidence is equivocal on the use of prophylactic antibiotics in sterile severe acute pancreatitis (AP)[60,61]; however compliance to guidelines is poor - there were 53.4% and 83.4% of patients who received prophylactic antibiotics for mild and severe AP respectively[62]. Unnecessary use of antibiotics not only results in undesired adverse drug reactions, drug resistance, but also results in pharmaceutical waste[63]. Tauber et al[64] estimated that potentially 23000 to 105000 million tonnes per year were generated from unused quantities of eye drops, ocular injection and systemic medication pharmaceuticals after cataract surgery. Another example would be the routine intra-operative collection of fungal culture in PPU[65]; Kwan et al[65] showed that while fungal isolates are commonly collected intra-operatively for PPU, the presence of fungal isolates was not an independent predictor of post-operative outcomes. Unnecessary microbiology testing results in waste of consumables (e.g., bottle for collection, petri dish for culture and cardboard used for packaging of consumables[66]), and this can be reduced with ongoing research to identify whether “routine” tests are truly indicated.
The lack of awareness towards environmental sustainability may be attributed to lack of institutional efforts. For instance, the survey by Harris et al[51] showed that only 12% of respondents reported having received education or training in environmental sustainability within their trust. This is contrary to the individuals’ enthusiasm (85% of respondents) in such education or training[51]. Implementation of educational and training programs have shown to be successful. For instance, Wyssusek et al[67] implemented a quality improvement and recycling program for waste management; educational sessions were conducted regularly for operating theatre staff members on appropriate waste segregation. Through the use of the Plan-Do-Study-Act model with a span of 5 years, they reduced the amount of clinical waste produced by the operating theatre by 82%, and total amount of operating theatre waste by more than 50%[67].
This review highlights the sizable impact of MIS on carbon footprint and environmental sustainability. CO2 emissions begin from the production of disposables, energy and water use, anesthesia, to recycling, sterilization and disposable of equipment. While surgical staffs are aware of the issue of global warming, there is a lack of leadership and education in this area. Educational and training programs should be conducted to improve awareness and reduce carbon footprint.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Boscarelli A, Italy; Liu J, China; Navarrete Arellano M, Mexico S-Editor: Wang JJ L-Editor: A P-Editor: Yuan YY
| 1. | Velanovich V. Laparoscopic vs open surgery: a preliminary comparison of quality-of-life outcomes. Surg Endosc. 2000;14:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 121] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Mederos MA, de Virgilio MJ, Shenoy R, Ye L, Toste PA, Mak SS, Booth MS, Begashaw MM, Wilson M, Gunnar W, Shekelle PG, Maggard-Gibbons M, Girgis MD. Comparison of Clinical Outcomes of Robot-Assisted, Video-Assisted, and Open Esophagectomy for Esophageal Cancer: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4:e2129228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 59] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 3. | Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 293] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 4. | Zhuang CL, Huang DD, Chen FF, Zhou CJ, Zheng BS, Chen BC, Shen X, Yu Z. Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2015;29:2091-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Chan KS, Ng STC, Tan CHB, Gerard G, Oo AM. A systematic review and meta-analysis comparing postoperative outcomes of laparoscopic versus open omental patch repair of perforated peptic ulcer. J Trauma Acute Care Surg. 2023;94:e1-e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Warps ALK, Zwanenburg ES, Dekker JWT, Tollenaar RAEM, Bemelman WA, Hompes R, Tanis PJ, de Groof EJ. Laparoscopic Versus Open Colorectal Surgery in the Emergency Setting: A Systematic Review and Meta-analysis. Annals Sur Open. 2021;2:e097. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Singh H, Eckelman M, Berwick DM, Sherman JD. Mandatory Reporting of Emissions to Achieve Net-Zero Health Care. N Engl J Med. 2022;387:2469-2476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Alley R, Berntsen T, Bindoff NL, Chen Z, Chidthaisong A, Friedlingstein P, Gregory J, Hegerl G, Heimann M, Hewitson B, Hoskins B, Joos F, Jouzel J, Kattsov V, Lohmann U, Manning M, Matsuno T, Molina M, Nicholls N, Overpeck J, Qin D, Raga G, Ramaswamy V, Ren J, Rusticucci M, Solomon S, Somerville R, Stocker TF, Stott P, Stouffer RJ, Whetton P, Wood RA, Wratt D, Arblaster J, Brasseur G, Christensen JH, Denman K, Fahey DW, Forster P, Jansen E, Jones PD, Knutti R, Treut HL, Lemke P, Meehl G, Mote P, Randall D, Stone DA, Trenberth KE, Willebrand J, Zwiers F. Climate change 2007: The physical science basis: Summary for policymakers: Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. [cited 10 October 2022]. Available from: https://cimss.ssec.wisc.edu/climatechange/nav/IPCCreport07.pdf. |
| 9. | Olivier JGJ, Peters JAHW. Trends in Global CO2 and Total Greenhouse Gas Emissions. 2019. |
| 10. | National Centers for Environmental Information. Annual 2021 Global Climate Report. [cited 5 October 2022]. Available from: https://www.ncei.noaa.gov/access/monitoring/monthly-report/global/202113. |
| 11. | Thomas JG, Chenoweth CE, Sullivan SE. Iatrogenic Creutzfeldt-Jakob disease via surgical instruments. J Clin Neurosci. 2013;20:1207-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Shabbir A, Menon RK, Somani J, So JBY, Ozman M, Chiu PWY, Lomanto D. ELSA recommendations for minimally invasive surgery during a community spread pandemic: a centered approach in Asia from widespread to recovery phases. Surg Endosc. 2020;34:3292-3297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Eckelman MJ, Sherman JD. Estimated Global Disease Burden From US Health Care Sector Greenhouse Gas Emissions. Am J Public Health. 2018;108:S120-S122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 122] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 14. | British Medical Association. More support needed to help the NHS reach net zero. [cited 15 November 2022]. Available from: https://www.bma.org.uk/what-we-do/population-health/protecting-people-from-threats-to-health/more-support-needed-to-help-the-nhs-reach-net-zero#:~:text=The%20health%20service%20has%20an,of%20the%20public%20sector's%20emissions. |
| 15. | Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann Surg. 2020;272:986-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 201] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 16. | MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e381-e388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 405] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 17. | Papadopoulou A, Kumar NS, Vanhoestenberghe A, Francis NK. Environmental sustainability in robotic and laparoscopic surgery: systematic review. Br J Surg. 2022;109:921-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 18. | Thiel CL, Eckelman M, Guido R, Huddleston M, Landis AE, Sherman J, Shrake SO, Copley-Woods N, Bilec MM. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49:1779-1786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 189] [Cited by in RCA: 228] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 19. | Thiel CL, Woods NC, Bilec MM. Strategies to Reduce Greenhouse Gas Emissions from Laparoscopic Surgery. Am J Public Health. 2018;108:S158-S164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 20. | Woods DL, McAndrew T, Nevadunsky N, Hou JY, Goldberg G, Yi-Shin Kuo D, Isani S. Carbon footprint of robotically-assisted laparoscopy, laparoscopy and laparotomy: a comparison. Int J Med Robot. 2015;11:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 78] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 21. | Power NE, Silberstein JL, Ghoneim TP, Guillonneau B, Touijer KA. Environmental impact of minimally invasive surgery in the United States: an estimate of the carbon dioxide footprint. J Endourol. 2012;26:1639-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Yoshizawa J, Baba Y, Mizutani T, Hiramatsu T, Ohashi S, Tanaka K, Kurobe M, Kuwashima N, Ashizuka S, Mizuno R, Ohki T. Laparoscopic Surgery Contributes to Global Warming. Jikeikai Med J. 2011;58:1-6. |
| 23. | Thiel CL, Schehlein E, Ravilla T, Ravindran RD, Robin AL, Saeedi OJ, Schuman JS, Venkatesh R. Cataract surgery and environmental sustainability: Waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J Cataract Refract Surg. 2017;43:1391-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 147] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 24. | Boberg L, Singh J, Montgomery A, Bentzer P. Environmental impact of single-use, reusable, and mixed trocar systems used for laparoscopic cholecystectomies. PLoS One. 2022;17:e0271601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 25. | Sutton JM, Dickinson J, Walker JT, Raven ND. Methods to minimize the risks of Creutzfeldt-Jakob disease transmission by surgical procedures: where to set the standard? Clin Infect Dis. 2006;43:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Rizan C, Bhutta MF. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg Endosc. 2022;36:4067-4078. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 52] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 27. | Drew J, Christie SD, Tyedmers P, Smith-Forrester J, Rainham D. Operating in a Climate Crisis: A State-of-the-Science Review of Life Cycle Assessment within Surgical and Anesthetic Care. Environ Health Perspect. 2021;129:76001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 96] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 28. | Conrardy J, Hillanbrand M, Myers S, Nussbaum GF. Reducing medical waste. AORN J. 2010;91:711-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Rutala WA, Weber DJ. Disinfection, sterilization, and control of hospital waste. In: Mandell, Douglas, and Bennett’s principles and practice of infectious diseases (Eighth Edition). Holland: Elsevier, 2015; 2: 3294-3309.e4. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | McGain F, Moore G, Black J. Steam sterilisation's energy and water footprint. Aust Health Rev. 2017;41:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 31. | Smith DR, Wang RS. Glutaraldehyde exposure and its occupational impact in the health care environment. Environ Health Prev Med. 2006;11:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Faveere WH, Van Praet S, Vermeeren B, Dumoleijn KNR, Moonen K, Taarning E, Sels BF. Toward Replacing Ethylene Oxide in a Sustainable World: Glycolaldehyde as a Bio-Based C(2) Platform Molecule. Angew Chem Int Ed Engl. 2021;60:12204-12223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 33. | Orhurhu VJ, Gao CC, Ku C. Carbon Dioxide Embolism. 2022 Nov 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 34. | Eaton S, McHoney M, Giacomello L, Pacilli M, Bishay M, De Coppi P, Wood J, Cohen R, Pierro A. Carbon dioxide absorption and elimination in breath during minimally invasive surgery. J Breath Res. 2009;3:047005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 35. | Gurusamy KS, Samraj K, Davidson BR. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2009;CD006930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 36. | Yang X, Cheng Y, Cheng N, Gong J, Bai L, Zhao L, Deng Y. Gases for establishing pneumoperitoneum during laparoscopic abdominal surgery. Cochrane Database Syst Rev. 2022;3:CD009569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 37. | Kim SJ, Ryu GO, Choi BJ, Kim JG, Lee KJ, Lee SC, Oh ST. The short-term outcomes of conventional and single-port laparoscopic surgery for colorectal cancer. Ann Surg. 2011;254:933-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 38. | Ahn SH, Son SY, Jung DH, Park DJ, Kim HH. Pure single-port laparoscopic distal gastrectomy for early gastric cancer: comparative study with multi-port laparoscopic distal gastrectomy. J Am Coll Surg. 2014;219:933-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 39. | Curcillo PG 2nd, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A, Dunham R, Fendley S, Neff M, Copper C, Bessler M, Gumbs AA, Norton M, Iannelli A, Mason R, Moazzez A, Cohen L, Mouhlas A, Poor A. Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc. 2010;24:1854-1860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 149] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 40. | Beebe DS, Swica H, Carlson N, Palahniuk RJ, Goodale RL. High levels of carbon monoxide are produced by electro-cautery of tissue during laparoscopic cholecystectomy. Anesth Analg. 1993;77:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | Hui Y, Yan J. Effect of electrosurgery in the operating room on surgeons' blood indices: a simulation model and experiment on rabbits. J Int Med Res. 2018;46:5245-5256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 42. | Robertson D, Sterke F, van Weteringen W, Arezzo A, Mintz Y, Nickel F; Technology committee of the European Association for Endoscopic Surgery (EAES), Horeman T. Characterisation of trocar associated gas leaks during laparoscopic surgery. Surg Endosc. 2022;36:4542-4551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 43. | Marano A, Choi YY, Hyung WJ, Kim YM, Kim J, Noh SH. Robotic versus Laparoscopic versus Open Gastrectomy: A Meta-Analysis. J Gastric Cancer. 2013;13:136-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 44. | Kilic GS, Walsh TM, Borahay M, Zeybek B, Wen M, Breitkopf D. Effect of residents' previous laparoscopic surgery experience on initial robotic suturing experience. ISRN Obstet Gynecol. 2012;2012:569456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 45. | Chan KS, Wang ZK, Syn N, Goh BKP. Learning curve of laparoscopic and robotic pancreas resections: a systematic review. Surgery. 2021;170:194-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 46. | Intuitive Surgical. Instrument & Accessory Catalog. 2019. [cited 8 October 2022]. Available from: https://www.intuitive.com/en-us/-/Media/ISI/Intuitive/pdf/davinci-x-xi-instrument-accessory-us-catalog-1052082.pdf?la=en&hash=AEBFCF4AE94C8A55C013BC9B3A147EF7. |
| 47. | Ludwig WW, Gorin MA, Ball MW, Schaeffer EM, Han M, Allaf ME. Instrument Life for Robot-assisted Laparoscopic Radical Prostatectomy and Partial Nephrectomy: Are Ten Lives for Most Instruments Justified? Urology. 2015;86:942-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 48. | Hubert J. Editorial Comment. Urology. 2015;86:946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 49. | World Health Organization. WHO methods and data sources for global burden of disease estimates 2000-2019. 2020. [cited 8 October 2022]. Available from: https://cdn.who.int/media/docs/default-source/gho-documents/global-health-estimates/ghe2019_daly-methods.pdf?sfvrsn=31b25009_7. |
| 50. | National Institute for Health and Care Excellence. Glossary. [cited 8 October 2022]. Available from: https://www.nice.org.uk/glossary?letter=q#:~:text=One%20quality%2Dadjusted%20%20Life%20year,%20a%200%20to%201%20scale. |
| 51. | Harris H, Bhutta MF, Rizan C. A survey of UK and Irish surgeons' attitudes, behaviours and barriers to change for environmental sustainability. Ann R Coll Surg Engl. 2021;103:725-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 52. | Trinks A, Mulder M, Scholtens B. An Efficiency Perspective on Carbon Emissions and Financial Performance. Ecol Econ. 2020;175:106632. [DOI] [Full Text] |
| 53. | Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J Health Serv Res Policy. 2017;22:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 54. | The Royal College of Surgeons of Edinburgh, Royal College of Surgeons of England, Royal College of Physicians and Surgeons of Glasgow. Intercollegiate Green Theatre Checklist. 2022. [cited 23 December 2022]. Available from: https://www.rcsed.ac.uk/media/1331734/green-theatre-posters-rcsed-a4-161022.pdf. |
| 55. | United Nations Educational Scientific and Cultural Organization. Declaration on the Responsibilities of the Present Generations Towards Future Generations. 1997. [cited 6 November 2022]. Available from: https://en.unesco.org/about-us/Legal-affairs/declaration-responsibilities-present-generations-towards-future-generations. |
| 56. | Scharf VF, Dent B, Jacob ME, Moore B. Efficacy of vaporized hydrogen peroxide for repeated sterilization of a single-use single-incision laparoscopic surgery port. Vet Surg. 2019;48:O59-O65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Siu J, Hill AG, MacCormick AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. ANZ J Surg. 2017;87:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 58. | Yung E, Gagner M, Pomp A, Dakin G, Milone L, Strain G. Cost comparison of reusable and single-use ultrasonic shears for laparoscopic bariatric surgery. Obes Surg. 2010;20:512-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 59. | Chung WTG, Shafi H, Seah J, Purnima P, Patun T, Kam KQ, Seah VXF, Ong RYL, Lin L, Choo RSM, Lingegowda P, Lim CLL, Chung JS, Chua NGSY, Lee TH, Yap MY, Ng TM, Somani J. National surgical antibiotic prophylaxis guideline in Singapore. Ann Acad Med Singap. 2022;51:695-711. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 60. | Chan KS, Shelat VG. Diagnosis, severity stratification and management of adult acute pancreatitis-current evidence and controversies. World J Gastrointest Surg. 2022;14:1179-1197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (5)] |
| 61. | Leppäniemi A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick AW, Ball CG, Parry N, Sartelli M, Wolbrink D, van Goor H, Baiocchi G, Ansaloni L, Biffl W, Coccolini F, Di Saverio S, Kluger Y, Moore E, Catena F. 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg. 2019;14:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 538] [Cited by in RCA: 431] [Article Influence: 71.8] [Reference Citation Analysis (0)] |
| 62. | Podda M, Pacella D, Pellino G, Coccolini F, Giordano A, Di Saverio S, Pata F, Ielpo B, Virdis F, Damaskos D, De Simone B, Agresta F, Sartelli M, Leppaniemi A, Riboni C, Agnoletti V, Mole D, Kluger Y, Catena F, Pisanu A; MANCTRA-1 Collaborative Group; Principal Investigator; Steering Committee; MANCTRA-1 Coordinating Group; Local Collaborators; Argentina; Australia; Bahrain; Brazil; Bulgaria; China; Colombia; Czech Republic; Egypt; France; Georgia; Greece; Guatemala; India; Italy; Jordan; Malaysia; Mexico; Nigeria; Pakistan; Paraguay; Peru; Philippines; Poland; Portugal; Qatar; Romania; Russia; Serbia; Slovak Republic; South Africa; Spain; Sudan; Switzerland; Syria; Tunisia; Turkey; United Kingdom; Uruguay; Yemen. coMpliAnce with evideNce-based cliniCal guidelines in the managemenT of acute biliaRy pancreAtitis): The MANCTRA-1 international audit. Pancreatology. 2022;22:902-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 63. | Richie C. Environmental sustainability and the carbon emissions of pharmaceuticals. J Med Ethics. 2022;48:334-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 64. | Tauber J, Chinwuba I, Kleyn D, Rothschild M, Kahn J, Thiel CL. Quantification of the Cost and Potential Environmental Effects of Unused Pharmaceutical Products in Cataract Surgery. JAMA Ophthalmol. 2019;137:1156-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 65. | Kwan JR, Lim M, Ng F, Shelat V. Fungal Isolates in Peritoneal Fluid Culture Do Not Impact Peri-Operative Outcomes of Peptic Ulcer Perforation. Surg Infect (Larchmt). 2019;20:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 66. | Yusuf E, Luijendijk A, Roo-Brand G, Friedrich AW. The unintended contribution of clinical microbiology laboratories to climate change and mitigation strategies: a combination of descriptive study, short survey, literature review and opinion. Clin Microbiol Infect. 2022;28:1245-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 67. | Wyssusek KH, Foong WM, Steel C, Gillespie BM. The Gold in Garbage: Implementing a Waste Segregation and Recycling Initiative. AORN J. 2016;103:316.e1-316.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |