Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1240
Peer-review started: February 27, 2023
First decision: March 10, 2023
Revised: March 21, 2023
Accepted: April 17, 2023
Article in press: April 17, 2023
Published online: June 27, 2023
Processing time: 108 Days and 4.2 Hours
Fishbone migration from the esophagus to the neck is relatively uncommon in clinical practice. Several complications secondary to esophageal perforation after ingestion of a fishbone have been described in the literature. Typically, a fishbone is detected and diagnosed by imaging examination and is usually removed by a neck incision.
Herein, we report a case of a 76-year-old patient with a fishbone in the neck that had migrated from the esophagus and that was in close proximity to the common carotid artery, and the patient experienced dysphagia. An endoscopically-guided neck incision was made over the insertion point in the esophagus, but the surgery failed due to having a blurred image at the insertion site during the operation. After injection of normal saline laterally to the fishbone in the neck under ultrasound guidance, the purulent fluid outflowed to the piriform recess along the sinus tract. With endoscopic guidance, the position of the fish bone was precisely located along the direction of liquid outflow, the sinus tract was separated, and the fish bone was removed. To the best of our knowledge, this is the first case report describing bedside ultrasound-guided water injection positioning combined with endoscopy in the treatment of a cervical esophageal perforation with an abscess.
In conclusion, the fishbone could be located by the water injection method under the guidance of ultrasound and could be accurately located along the outflow direction of the purulent fluid of the sinus by the endoscope and was removed by incising the sinus. This method can be a nonoperative treatment option for foreign body-induced esophageal perforation.
Core Tip: Fishbones are very common foreign bodies in upper gastrointestinal tracts in clinical practice. The most common fishbone stuck sites are the oropharynx, oral cavity, and esophagus. However, they are movable under the action of esophageal peristalsis, food swallowing and normal pleural pressure, which may cause severe complications if not treated in time. Under the guidance of ultrasound, the fishbone can be accurately located under the endoscope, and the fishbone can be removed by incising the sinus. This method can be an optimal alternative for treating patients with esophageal perforation and reducing surgical trauma.
- Citation: Wei HX, Lv SY, Xia B, Zhang K, Pan CK. Bedside ultrasound-guided water injection assists endoscopically treatment in esophageal perforation caused by foreign bodies: A case report. World J Gastrointest Surg 2023; 15(6): 1240-1246
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1240.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1240
In clinical practice, fishbones are very common in upper gastrointestinal tracts of patients[1] and are associated with the highest risk of gastrointestinal perforation[2]. In adults, the most common stuck sites of fish bones are the oropharynx, oral cavity, and esophagus[3]. Most patients can be discharged after outpatient treatment[4]. However, some foreign bodies, such as fishbones, can move under the action of esophageal peristalsis, food swallowing, and normal pleural pressure. If not treated in time, these sharp foreign bodies may penetrate the esophageal wall, causing an esophageal perforation, and surrounding organs or main blood vessels, causing severe complications[5]. Esophageal perforation is defined as a foreign body penetrating the outer wall of the esophagus[6]. When the fishbone completely penetrates the esophagus and enters the neck, a cervical sinus will be formed over time. Patients may experience symptoms such as dysphagia, pain, hemoptysis, and fever. Computed tomography (CT) and X-ray examinations can detect foreign bodies such as fishbones in the esophagus. For the treatment of esophageal perforation, different surgical methods are required for different types of fishbones, for different locations of perforation, and for the various complications after perforation. Most migratory fish bones in the neck can be removed by making a lateral incision into the neck[7]. However, this method is usually traumatic to the tissue and can lead to severe bleeding. Therefore, in this case, we chose to use the bedside ultrasound-guided water injection positioning method combined with endoscopy to remove a neck-located fishbone, which had migrated from the esophagus. This method can accurately remove the fishbone with less trauma and bleeding.
A 76-year-old Chinese man was admitted to our hospital due to pain during swallowing for 1 wk that was caused by accidental swallowing of a “fishbone”.
The patient had mistakenly swallowed a “fish bone” 26 d prior. However, no foreign body was found during the laryngoscopy examination, and the pain gradually eased. One week prior, the pain in the right throat was aggravated, and it was accompanied by difficulty swallowing. After removing the “epiglottis abscess” and after a course of anti-infection treatment, the patient still had pain during swallowing and dysphagia and had pain in his right neck and shoulder. After the outpatient CT review of the esophagus, the patient was admitted to the hospital and was diagnosed with “foreign bodies in the throat”.
The patient had no history of hypertension, diabetes, viral hepatitis or tuberculosis. He had no known drug or food allergies. He also denied any history of surgery, trauma, or blood transfusions.
The patient denied any history of smoking or drinking or any abnormal family history.
On physical examination, the vital signs were as follows: Body temperature, 36.4 °C; blood pressure, 126/79 mmHg; heart rate, 69 beats per min; and respiratory rate, 19 breaths per min. He was well developed and moderately nourished. He had an active position. The skin was not jaundiced. There are no special general appearances. The patient had no pitting edema. The patient’s superficial lymph nodes in his neck were not found to be enlarged.
No abnormalities were found in coagulation function, blood biochemical parameters, routine blood, or urine analysis.
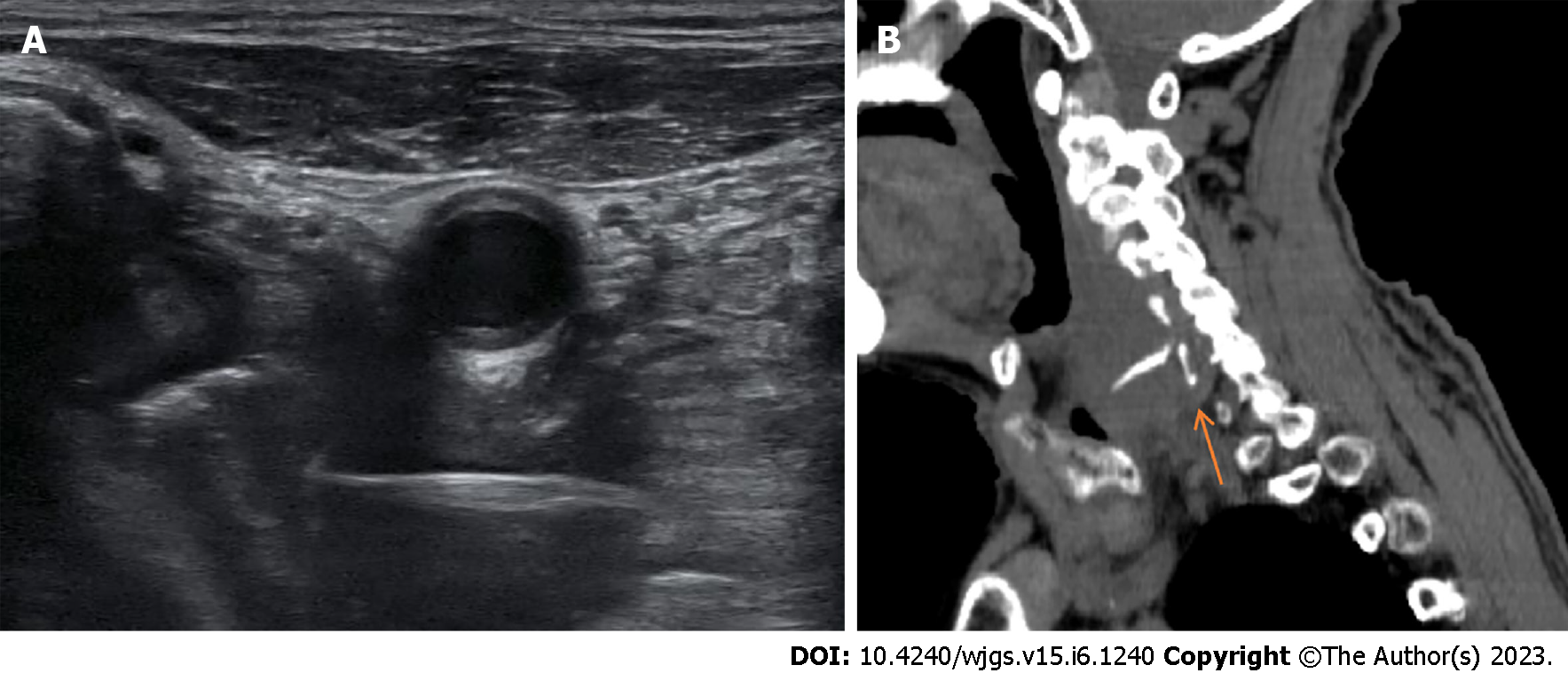
Laryngoscopy examination showed that the pharynx was slightly congested, the bilateral tonsils were not enlarged, and a raised mass of approximately 1.0 cm × 1.0 cm was seen on the right side of the lingual surface of the epiglottis. The surgical site had recovered well with no obvious pus exudation. Both vocal cords were smooth and showed good movement capacity. The right piriform fossa was obviously swollen, and there was no obvious foreign body in the laryngopharynx. Ultrasonography revealed a band of hyperechoic echoes on the right side of the neck (Figure 1A). The sagittal plane of the CT scan showed a high-density strip in the right of the neck (Figure 1B).
The patient was diagnosed clearly, and no further examination was necessary.
Combined with the medical history and examination results, the final diagnosis was “a foreign body in the right paralaryngopharynx and a foreign body with abscess formation”.
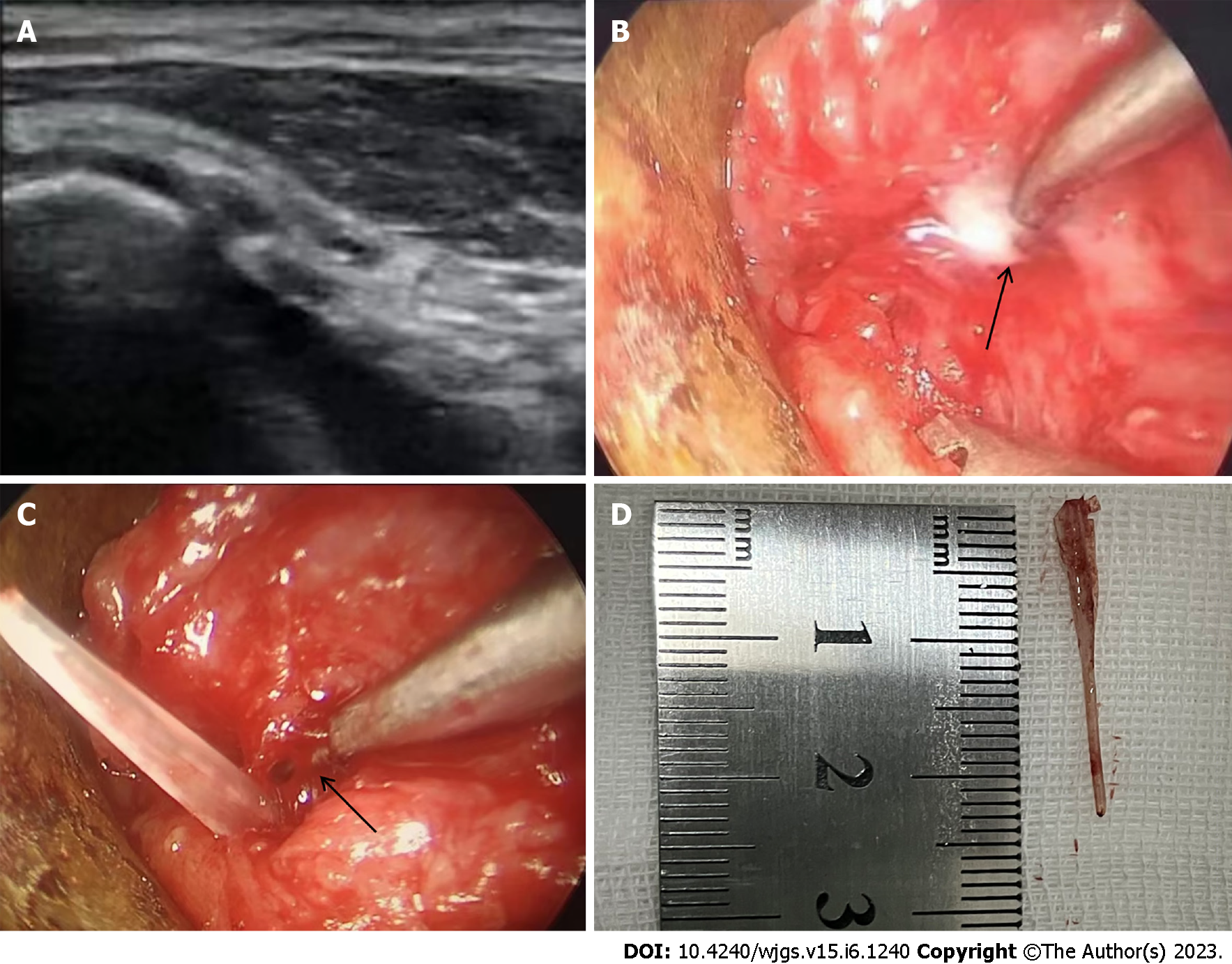
Therefore, surgery was performed on the patient in collaboration with a gastroenterologist and ultrasound physician after the patient signed an informed consent form. During the operation, the mucosa of the lateral wall of the right piriform fossa was obviously swollen, and a mucosal breach was seen. An incision was made at the mucosal breach of the lateral wall of the right piriform fossa. Blunt dissection was performed, but no foreign body was detected. Then, under the guidance of bedside ultrasound positioning, a 23 G/9.0 cm fine needle was found punctured into the cavity where the fishbone was located (Figure 2A). After injection of normal saline, a small amount of purulent fluid overflowing from the dissected lateral wall of the right piriform fossa was observed under video endoscopy and laryngoscopy (Figure 2B). Under endoscopy, the sinus tract was separated until the end of the foreign body was located by ultrasound, and the head of the foreign body (fishbone) was exposed (Figure 2C). Then, a fishbone with a length of 2.5 cm was removed using forceps (Figure 2D). We then withdrew the puncture needle from the neck, adjusted the supporting laryngoscope to expose the epiglottis abscess, and cut the epiglottis abscess with a surgical scimitar. A small amount of pus was seen overflowing. After the pus was completely removed, the swelling on the lingual surface of the epiglottis completely disappeared. After withdrawing the supporting laryngoscope, we completed the operation successfully.
The patient was treated with antibiotics for 3 d after the operation and was discharged from the hospital without symptoms, including neck pain, fever, hematemesis, and melena.
Ingested esophageal foreign bodies are commonly seen in the adult population. Due to the different eating habits of people in China compared to people in Western countries, foreign bodies found in Chinese people are mostly fishbones, jujube shells, and poultry bones[8]. Most ingested foreign bodies pass through the gastrointestinal tract spontaneously without causing complications; however, some foreign bodies may stay in the gastrointestinal tract and cause serious complications. Approximately 20% of patients require nonsurgical intervention; in a few cases, all the standard treatment options are ineffective and may cause the patient to require surgery[9]. Esophageal perforation caused by foreign bodies is still an urgent problem to be solved.
X-ray and endoscopic examinations are the most commonly used methods for detecting fishbones in the upper gastrointestinal tract; however, their accuracy and consistency are lower than those of neck-based CT scans. Magnetic resonance imaging (MRI) has advantages in estimating the extent of soft tissue inflammation caused by foreign bodies and detecting adjacent structures such as cervical blood vessels and nerves, but MRI is not sensitive in diagnosing foreign bodies. Thus, CT is the gold standard for the examination of fishbones in the neck[10].
Endoscopic removal is a safe and effective treatment method for sharp-pointed food impactions[11]. Food that is causing an esophageal obstruction can be gently pushed into the stomach, while foreign bodies that are unsuitable or unable to be pushed into the stomach can be removed by a snare, graspers, a stone extraction mesh basket, a balloon, a holmium laser and other tools after the types and positions are identified endoscopically[12]. However, for patients showing throat and neck discomfort after eating fish without fishbones detected by endoscopy, the possibility of esophageal perforation combined with the fishbone migrating to other locations should be considered[13], as constriction of swallowing muscles and peristalsis of the esophagus can force the fishbone to penetrate the mucosa and move out of the oropharynx[14]. An abscess can be formed 3-4 d after the fishbone moves out of the oropharynx into the neck[15]. In this case, since the fishbone is in the nontraditional position, endoscopic ultrasonography is very promising in accurately locating its position. In this study, the water injection method was adopted, by which normal saline was injected into the abscess formed by the fishbone. Then, purulent normal saline flowed along the sinus tract into the piriform recess. We accurately positioned the fishbone from the piriform crypt in the direction of the outflow. It has been reported that for cases where the insertion point of the fishbone can be seen clearly, the method of injecting normal saline containing methylene blue through the esophagus under ultrasound-guided endoscopy can be used, which can precisely locate the fishbone. By cutting an incision along the stained tract under the endoscope, the fishbone can be removed easily[16]. Therefore, we suggest that for foreign bodies that have been in the neck for a long time, which formed an abscess cavity, normal saline injection positioning can be used to locate the foreign body, and then a neck incision can be performed under the endoscope to remove the foreign body. This surgical protocol yields smaller incisions and less bleeding and avoids perforation and reoperation.
Ultrasound examination, a highly operator-dependent and nonradiation examination technology, has been less commonly used in the detection of neck fishbones in recent years[17]. As ultrasound examination has the advantages of real-time imaging and low cost, the combination of bedside ultrasound and endoscopic techniques may provide a beneficial solution for the diagnosis and treatment of patients with esophageal perforation combined with a migratory fishbone in the neck.
Under the guidance of ultrasound, the fishbone can be located by the water injection method. Then, the foreign body can be accurately located endoscopically and along the outflow direction of the sinus purulent fluid, and the fishbone can be removed by incising the sinus. This method can be an optimal plan for treating patients with esophageal perforation caused by foreign bodies. It can effectively improve the efficiency of endoscopic removal of free foreign bodies in the neck, reducing the surgical incision area and avoiding intraoperative bleeding and extensive tissue damage.
The authors wish to acknowledge the assistance of the people at the Jinyun County People’s Hospital. This report would not have been possible without their efforts in data collection and interprofessional collaboration in treating this patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Calinescu AM, Switzerland; Imatani A, Japan S-Editor: Chen YL L-Editor: A P-Editor: Li X
| 1. | Chee LW, Sethi DS. Diagnostic and therapeutic approach to migrating foreign bodies. Ann Otol Rhinol Laryngol. 1999;108:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Megwalu UC. Migration of an ingested fish bone into the paraglottic space. J Laryngol Otol. 2016;130:973-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Klein A, Ovnat-Tamir S, Marom T, Gluck O, Rabinovics N, Shemesh S. Fish Bone Foreign Body: The Role of Imaging. Int Arch Otorhinolaryngol. 2019;23:110-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Wu TC, Huang PW, Tung CB. Does plain radiography still have a role in cases of fish bone ingestion in emergency rooms? A retrospective analysis. Emerg Radiol. 2021;28:627-631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Tang IP, Singh S, Shoba N, Rahmat O, Shivalingam S, Gopala KG, Khairuzzana B. Migrating foreign body into the common carotid artery and internal jugular vein--a rare case. Auris Nasus Larynx. 2009;36:380-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Liao F, Zhu Z, Pan X, Li B, Zhu Y, Chen Y, Shu X. Safety and Efficacy of Nonoperative Treatment in Esophageal Perforation Caused by Foreign Bodies. Clin Transl Gastroenterol. 2022;13:e00451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Hendricks A, Meir M, Hankir M, Lenschow C, Germer CT, Schneider M, Wiegering A, Schlegel N. Suppurative thyroiditis caused by ingested fish bone in the thyroid gland: a case report on its diagnostics and surgical therapy. BMC Surg. 2022;22:92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 8. | Vitek WS, Pagidas K, Gu G, Pepperell JR, Simpson JL, Tantravahi U, Plante BJ. Xq;autosome translocation in POF: Xq27.2 deletion resulting in haploinsufficiency for SPANX. J Assist Reprod Genet. 2012;29:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Zhong Q, Jiang R, Zheng X, Xu G, Fan X, Xu Y, Liu F, Peng C, Ren W, Wang L. Esophageal foreign body ingestion in adults on weekdays and holidays: A retrospective study of 1058 patients. Medicine (Baltimore). 2017;96:e8409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Guelfguat M, Kaplinskiy V, Reddy SH, DiPoce J. Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol. 2014;203:37-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 11. | Li G, Wu D, Zhou L, You D, Huang X. Delayed Endoscopic Management of Esophageal Sharp-Pointed Food Impaction: An Analysis of 829 Cases in China. Dig Dis Sci. 2022;67:3166-3176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Yang Z, Qin S, Li X. Esophageal foreign body removal under holmium laser-assisted gastroscope: A case report. Front Surg. 2023;10:1094160. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Koh WJ, Lum SG, Al-Yahya SN, Shanmuganathan J. Extraluminal migration of ingested fish bone in the upper aerodigestive tract: A series of three cases with broad clinical spectrum of manifestations and outcomes. Int J Surg Case Rep. 2021;89:106606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Shaariyah MM, Salina H, Dipak B, Majid MN. Migration of foreign body from postcricoid region to the subcutaneous tissue of the neck. Ann Saudi Med. 2010;30:475-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Lam HC, Woo JK, van Hasselt CA. Esophageal perforation and neck abscess from ingested foreign bodies: treatment and outcomes. Ear Nose Throat J. 2003;82:786, 789-794. [PubMed] |
| 16. | Cao L, Chen N, Chen Y, Zhang M, Guo Q, Chen Q, Cheng B. Foreign body embedded in the lower esophageal wall located by endoscopic ultrasonography: A case report. Medicine (Baltimore). 2018;97:e11275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Salmon B, Le Denmat D. Intraoral ultrasonography: development of a specific high-frequency probe and clinical pilot study. Clin Oral Investig. 2012;16:643-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |