Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1232
Peer-review started: January 12, 2023
First decision: January 21, 2023
Revised: January 30, 2023
Accepted: April 19, 2023
Article in press: April 19, 2023
Published online: June 27, 2023
Processing time: 154 Days and 1.1 Hours
The combination of atezolizumab (ATZ) and bevacizumab (BVZ) was approved as first-line systemic therapy for advanced hepatocellular carcinoma (HCC) owing to its superior rates of response and patient survival. However, ATZ + BVZ is associated with increased risk of upper gastrointestinal (GI) bleeding, including arterial bleeding, which is rare and potentially fatal. We present a case of massive upper GI bleeding from a gastric pseudoaneurysm in a patient with advanced HCC who had been treated with ATZ + BVZ.
A 67-year-old man presented with severe upper GI bleeding after atezolizumab (ATZ) + bevacizumab (BVZ) therapy for HCC. Endoscopy failed to detect the bleeding site. Digital subtraction angiography revealed a gastric artery pseudoaneurysm and contrast extravasation from the inferior splenic artery and a branch of the left gastric artery. Successful hemostasis was achieved with embolization.
HCC patients who have been treated with ATZ + BVZ should be followed for 3 to 6 mo to monitor for development of massive GI bleeding. Diagnosis may require angiography. Embolization is an effective treatment.
Core Tip: Atezolizumab (ATZ) + bevacizumab (BVZ) treatment increases the risk of bleeding in hepatocellular carcinoma (HCC) patients. Gastrointestinal (GI) bleeding is most common and usually arises from esophageal varices. We report a patient with advanced HCC who presented with massive upper GI bleeding from a gastric artery pseudoaneurysm after three cycles of ATZ + BVZ. Gastric artery pseudoaneurysm is rare and often asymptomatic. Mortality is high and emergency endovascular embolization is required. Patients receiving ATZ + BVZ treatment should be followed closely for GI bleeding. Arterial bleeding should be considered when massive GI bleeding occurs. Angiography may be required for diagnosis. Embolization has a role in treatment.
- Citation: Pang FW, Chen B, Peng DT, He J, Zhao WC, Chen TT, Xie ZG, Deng HH. Massive bleeding from a gastric artery pseudoaneurysm in hepatocellular carcinoma treated with atezolizumab plus bevacizumab: A case report. World J Gastrointest Surg 2023; 15(6): 1232-1239
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1232.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1232
Primary liver cancer is the fourth leading cause of cancer-related death worldwide[1] and hepatocellular carcinoma (HCC) is the most common type of primary liver cancer[2]. Curative treatment options for early-stage HCC include resection, liver transplantation, and ablation. However, most HCC patients are diagnosed in an advanced stage[2]. In these patients, current guidelines recommend systemic therapy[3].
The multikinase inhibitor sorafenib is an effective first-line systemic agent for treating advanced HCC[4,5]. Lenvatinib, another multikinase inhibitor, is an accepted alternative[6]. Previous studies have shown that both provide modest improvement in survival[6,7]. However, multikinase inhibitors are associated with considerable toxicities which can impair quality of life. The IMbrave 150 trial showed that atezolizumab (ATZ), a programmed cell death ligand 1 antibody and immune checkpoint inhibitor, combined with bevacizumab (BVZ), a vascular endothelial growth factor (VEGF) antibody, achieved a better response rate and rates of progression-free and overall survival than sorafenib in patients with advanced metastatic or unresectable HCC[8]. Based on the trial’s results, ATZ + BVZ was approved as first-line systemic therapy for advanced HCC in May 2020. However, compared with sorafenib, ATZ + BVZ was associated with a higher rate of bleeding overall (25.2% vs 17.3%) and higher rate of upper gastrointestinal (GI) bleeding (7% vs 4.5%). According to previous studies, variceal bleeding accounts for approximately 70% of all upper GI bleeding in HCC patients receiving BVZ or ATZ + BVZ; arterial GI bleeding is rare[9,10]. Here, we report an HCC patient who developed massive GI bleeding from a gastric artery pseudoaneurysm after treatment with ATZ + BVZ.
A 67-year-old man with advanced HCC was admitted to our hospital for massive upper GI bleeding after three cycles of ATZ+BVZ treatment.
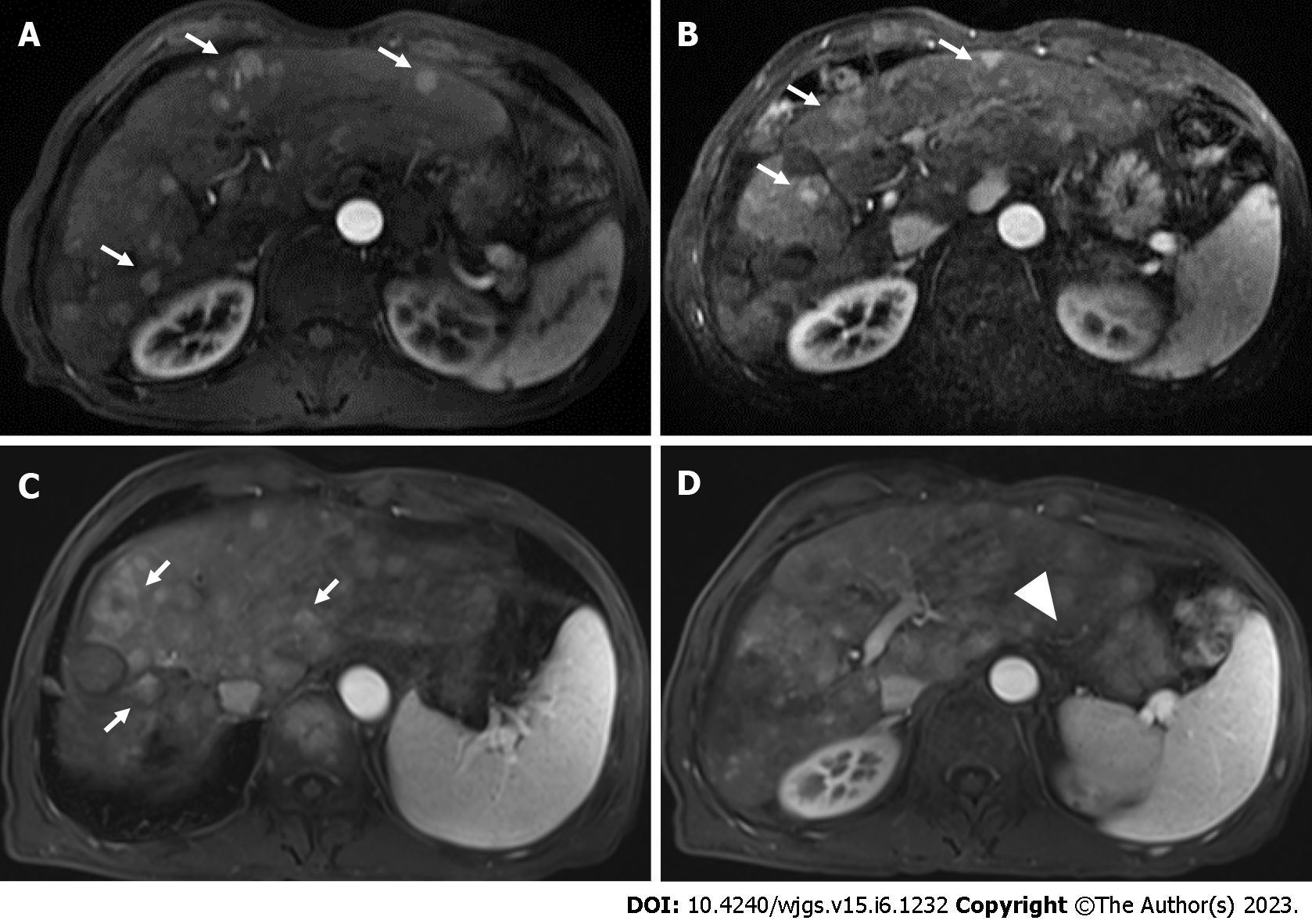
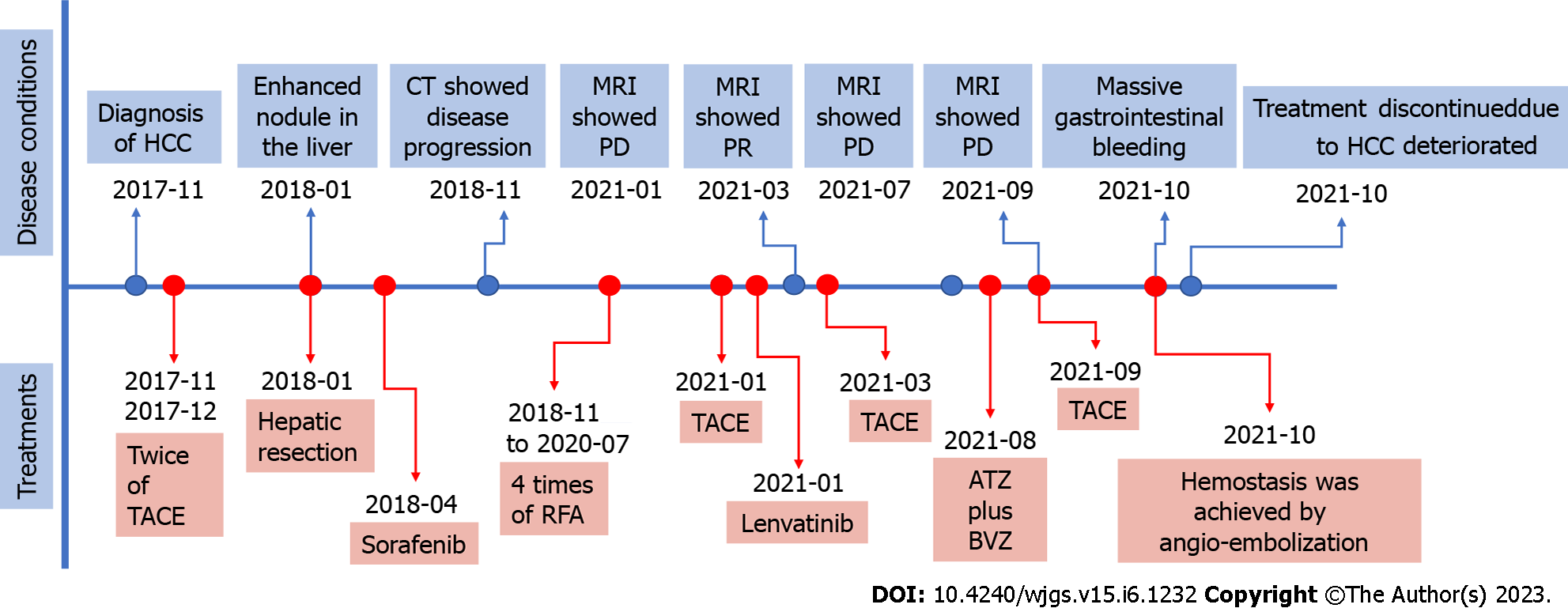
The patient had been treated with transcatheter arterial chemoembolization (TACE) twice and surgical resection. Owing to HCC progression, he had more recently been treated with sorafenib and four radiofrequency ablation procedures. He was referred to our hospital for evaluation of right upper quadrant abdominal pain in January 2021. Contrast-enhanced abdominal magnetic resonance imaging (MRI) showed multiple enhancing nodules in all segments of the liver (Figure 1A). He underwent TACE twice as well as lenvatinib treatment. Nonetheless, his HCC progressed (Figure 1B). Combination of ATZ (1200 mg) and BVZ (15 mg/kg) every 3 wk was therefore initiated. Blood testing revealed a white blood cell count of 2.83 × 109/L, hemoglobin concentration of 127 g/L, and platelet count of 149 × 109/L. Child–Pugh score was 6 (Class A), indicating preserved liver function. Prothrombin time was 2 s longer than normal. Concentrations of the tumor markers des-gamma-carboxyprothrombin and alpha fetoprotein were elevated (29787 mAU/mL and 0.8 ng/mL, respectively). After three cycles, MRI showed continued progression but no remarkable gastroesophageal varices (Figure 1C and D). The patient then underwent another TACE procedure which showed no contrast extravasation in the gastric area (Figure 2). He was discharged without complications. Ten days later, he was admitted to the hospital because of massive hematochezia and melanemesis. The patient’s clinical course is shown in Figure 3.
The patient had a history of hepatitis C, cirrhosis, and HCC diagnosed 3 years ago. He also had a remote history of gastric carcinoma treated with partial gastrectomy 30 years previously.
No specific personal and family history.
On admission, he exhibited signs of hypovolemic shock: Paleness, sweating and low blood pressure (64/38 mmHg).
Hemoglobin concentration and platelet count were 59 g/L and 98 × 109/L, respectively. Prothrombin time was 5 s longer than normal.
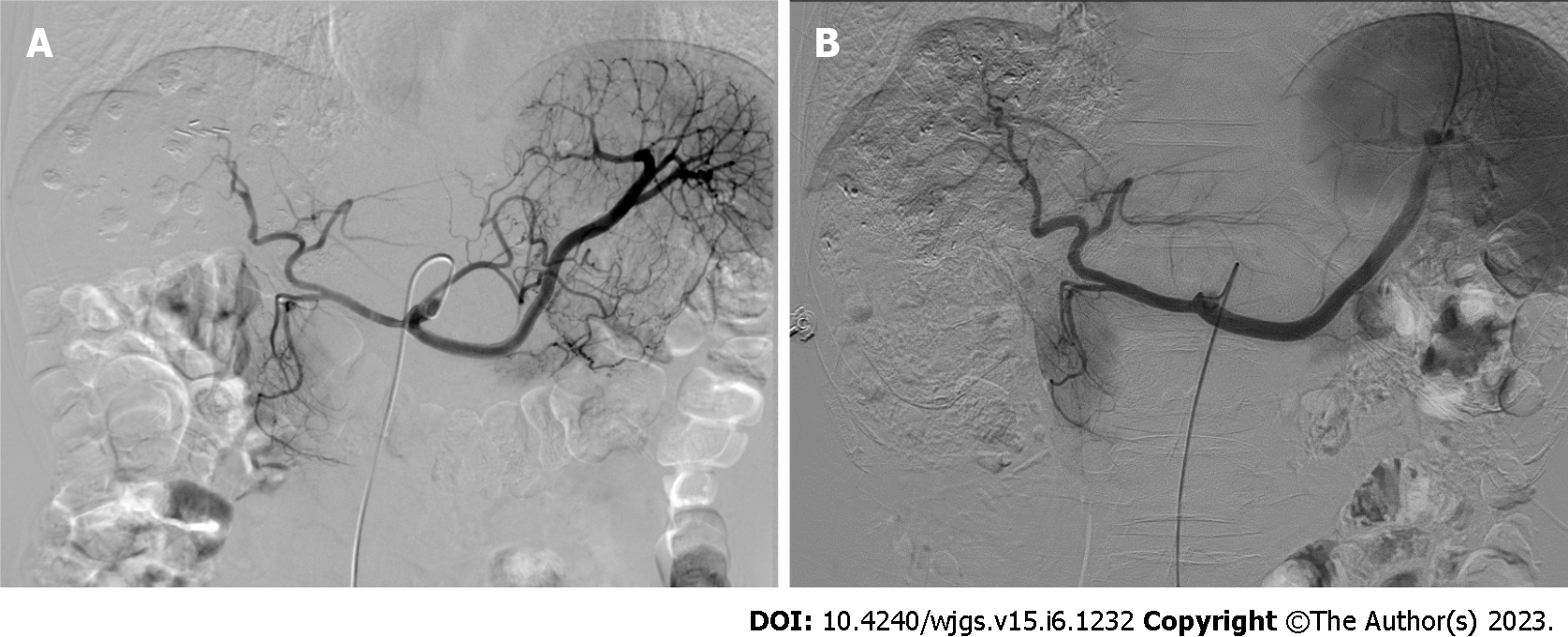
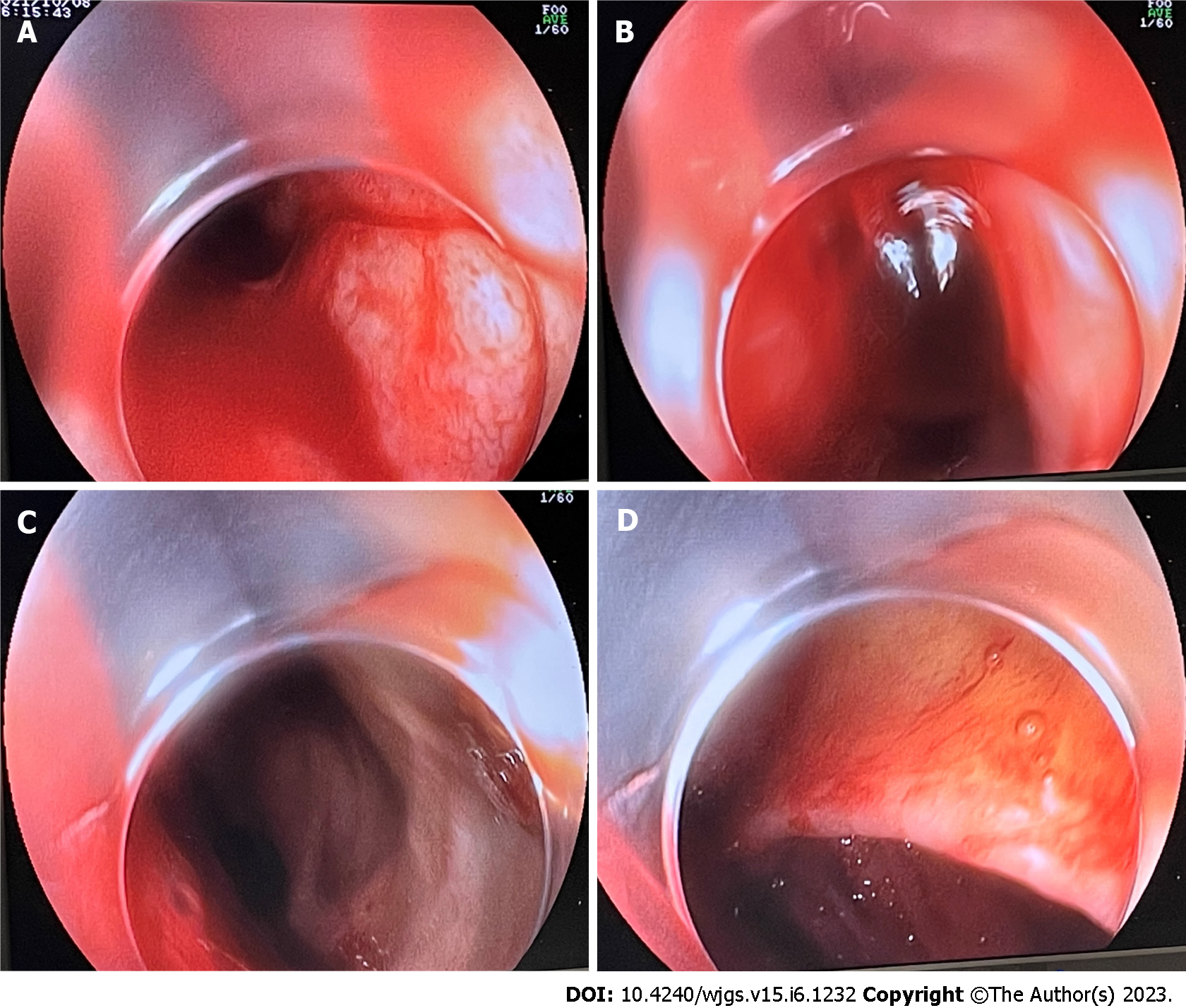
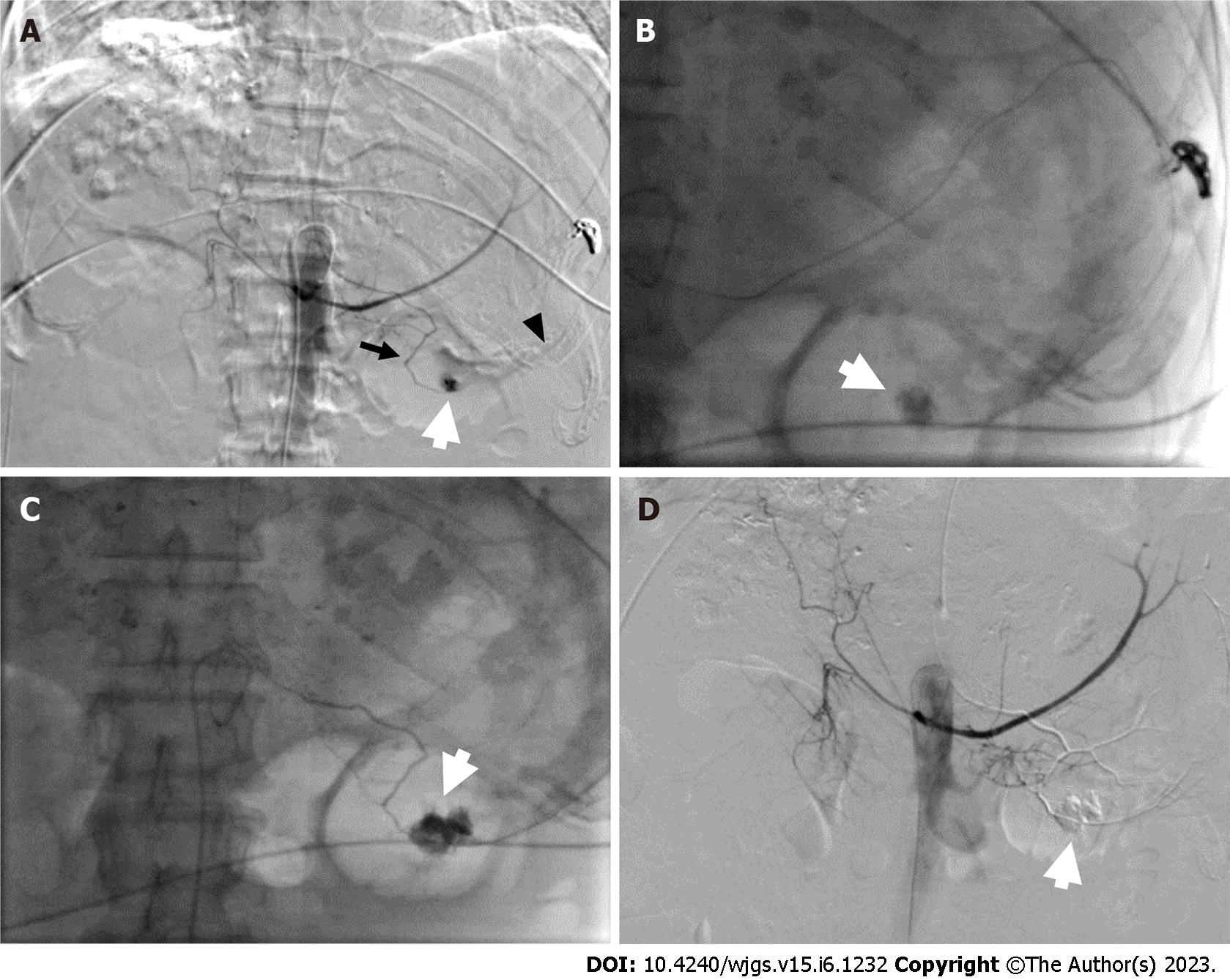
His condition did not improve despite infusion of intravenous fluids and a transfusion of packed red blood cells. Because acute upper GI bleeding was suspected, GI endoscopy was performed, which revealed fresh blood and blood clots within the stomach (Figure 4). The blood could not be removed with repeated washings. Esophageal varices and red wale signs were not observed; however, visualization was limited. Because hemostasis could not be achieved, he underwent emergency digital subtraction angiography (DSA), which showed contrast extravasation from a gastric artery pseudoaneurysm, the inferior splenic artery, and a branch of the left gastric artery (Figure 5A).
The final diagnosis was acute massive upper GI bleeding from a gastric pseudoaneurysm.
The pseudoaneurysm was successfully embolized with a mixture of lipiodol (2 mL) and liquid glue (0.5 mL) (Figure 5B-D).
Although embolization resulted in hemostasis and marked improvement in general condition, the patient later developed liver failure and hepatic encephalopathy. Further treatment was discontinued at the family’s request. Unfortunately, he died because of disease deterioration 6 d later.
We report a patient who presented with massive bleeding after receiving ATZ + BVZ treatment for progressive HCC. Although endoscopy failed to detect a bleeding source, DSA revealed a gastric artery pseudoaneurysm and contrast extravasation from the inferior splenic artery and a branch of the left gastric artery. Hemostasis was achieved after successful embolization.
ATZ is a humanized immunoglobulin G1 monoclonal antibody which selectively targets pro
BVZ is a recombinant humanized monoclonal immunoglobulin G antibody which binds VEGF and blocks its interaction with receptors on endothelial cells to inhibit tumor angiogenesis and growth[14]. VEGF-A is an important growth factor which induces vascular permeability, stimulates extracellular matrix remodeling, and creates new blood vessels[15]. BVZ inhibits normal and pathological angiogenesis via targeting VEGF-A. In the IMbrave150 study[8], GI bleeding (3%), pulmonary hemorr
Because the patient had a remote history of gastric carcinoma and partial gastrectomy and the site of bleeding was in the stomach, recurrence of gastric carcinoma and anastomotic bleeding should be taken into consideration. Unfortunately, we did not perform endoscopy before ATZ + BVZ was administered or before bleeding began. GI endoscopy at the time of bleeding failed to detect the bleeding site because of limited visualization. However, the gastrectomy was performed approximately 30 years prior and the recurrence rate more than 10 years after curative gastrectomy is lower than 0.2%[20]. In addition, DSA performed before the massive bleeding occurred showed no pseudoaneurysm in the gastric area. Therefore, these possibilities are unlikely. In a meta-analysis of the risk of high-grade bleeding in patients with various cancers treated with BVZ, the risk was significantly higher in those who received 5 mg/kg per wk than those who received 2.5 mg/kg per wk[21]. However, none of the studies included in the meta-analysis examined patients with HCC. HCC patients typically receive doses of BVZ (15 mg/kg) and ATZ (1200 mg) on the same day administered every 3 wk[8]. BVZ dosing adjustments have not been established at present. Our patient received the standard recommended BVZ dose; therefore, it is not likely to have been the cause of bleeding.
Acute GI bleeding from varices or nonvariceal lesions can be fatal in patients with cirrhosis or HCC. Careful monitoring and appropriate intervention are important. Visceral artery pseudoaneurysms require immediate treatment because their rupture rate is high[22] and endovascular embolization using coils and/or liquid glue is effective. In our patient, owing to his poor physical condition and the massive degree of bleeding, embolization was successfully performed using a mixture of liquid glue and lipiodol.
In HCC patients undergoing treatment with ATZ + BVZ, we recommend GI endoscopy before and after therapy. Patients with a high risk of bleeding should be followed for 3 to 6 mo[23]. Any pseudoaneurysms identified should be embolized under DSA guidance.
In this study, we report a case of massive GI bleeding from a gastric pseudoaneurysm in patient after ATZ + BVZ treatment for HCC. Awareness of this rare and life-threatening complication allows specific diagnostic evaluation and timely intervention. Angioembolization of the pseudoaneurysm guided by DSA is preferred whenever a pseudoaneurysm becomes apparent.
The authors thank the patient and his family for their involvement.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Huang CF, Taiwan; Tanabe H, Japan S-Editor: Liu JH L-Editor: A P-Editor: Wu RR
| 1. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6038] [Article Influence: 862.6] [Reference Citation Analysis (3)] |
| 2. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55774] [Article Influence: 7967.7] [Reference Citation Analysis (132)] |
| 3. | D'Alessio A, Cammarota A, Zanuso V, Pressiani T, Personeni N, Rimassa L. Atezolizumab plus bevacizumab for unresectable or metastatic hepatocellular carcinoma. Expert Rev Anticancer Ther. 2021;21:927-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Fang P, Hu JH, Cheng ZG, Liu ZF, Wang JL, Jiao SC. Efficacy and safety of bevacizumab for the treatment of advanced hepatocellular carcinoma: a systematic review of phase II trials. PLoS One. 2012;7:e49717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY, Kudo M, Breder V, Merle P, Kaseb AO, Li D, Verret W, Xu DZ, Hernandez S, Liu J, Huang C, Mulla S, Wang Y, Lim HY, Zhu AX, Cheng AL; IMbrave150 Investigators. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N Engl J Med. 2020;382:1894-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2542] [Cited by in RCA: 4672] [Article Influence: 934.4] [Reference Citation Analysis (2)] |
| 6. | Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2800] [Cited by in RCA: 4092] [Article Influence: 584.6] [Reference Citation Analysis (6)] |
| 7. | Hang XF, Xu WS, Wang JX, Wang L, Xin HG, Zhang RQ, Ni W. Risk of high-grade bleeding in patients with cancer treated with bevacizumab: a meta-analysis of randomized controlled trials. Eur J Clin Pharmacol. 2011;67:613-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Hsu C, Rimassa L, Sun HC, Vogel A, Kaseb AO. Immunotherapy in hepatocellular carcinoma: evaluation and management of adverse events associated with atezolizumab plus bevacizumab. Ther Adv Med Oncol. 2021;13:17588359211031141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Huppert LA, Gordan JD, Kelley RK. Checkpoint Inhibitors for the Treatment of Advanced Hepatocellular Carcinoma. Clin Liver Dis (Hoboken). 2020;15:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Kudo M, Finn RS, Qin S, Han KH, Ikeda K, Piscaglia F, Baron A, Park JW, Han G, Jassem J, Blanc JF, Vogel A, Komov D, Evans TRJ, Lopez C, Dutcus C, Guo M, Saito K, Kraljevic S, Tamai T, Ren M, Cheng AL. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3128] [Cited by in RCA: 3816] [Article Influence: 545.1] [Reference Citation Analysis (1)] |
| 11. | Li CC, Tsai HL, Huang CW, Yeh YS, Tsai TH, Wang JY. Iatrogenic pseudoaneurysm after bevacizumab therapy in patients with metastatic colorectal cancer: Two case reports. Mol Clin Oncol. 2018;9:499-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J; SHARP Investigators Study Group. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359:378-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9016] [Cited by in RCA: 10258] [Article Influence: 603.4] [Reference Citation Analysis (2)] |
| 13. | Nagarajan K, Sunilkumar D, Ramakrishnaiah VPN, Amuthabarathi M. Left Gastric Pseudoaneurysm in a Case of Chronic Pancreatitis: A Case Report With Review of Literature. Vasc Endovascular Surg. 2021;55:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Petrick JL, Braunlin M, Laversanne M, Valery PC, Bray F, McGlynn KA. International trends in liver cancer incidence, overall and by histologic subtype, 1978-2007. Int J Cancer. 2016;139:1534-1545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 253] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 15. | Pitton MB, Dappa E, Jungmann F, Kloeckner R, Schotten S, Wirth GM, Mittler J, Lang H, Mildenberger P, Kreitner KF, Oberholzer K, Dueber C. Visceral artery aneurysms: Incidence, management, and outcome analysis in a tertiary care center over one decade. Eur Radiol. 2015;25:2004-2014. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 180] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 16. | Roviello G, Bachelot T, Hudis CA, Curigliano G, Reynolds AR, Petrioli R, Generali D. The role of bevacizumab in solid tumours: A literature based meta-analysis of randomised trials. Eur J Cancer. 2017;75:245-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 17. | Sangro B, Chan SL, Meyer T, Reig M, El-Khoueiry A, Galle PR. Diagnosis and management of toxicities of immune checkpoint inhibitors in hepatocellular carcinoma. J Hepatol. 2020;72:320-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 192] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 18. | Shin CH, Lee WY, Hong SW, Chang YG. Characteristics of gastric cancer recurrence five or more years after curative gastrectomy. Chin J Cancer Res. 2016;28:503-510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Shord SS, Bressler LR, Tierney LA, Cuellar S, George A. Understanding and managing the possible adverse effects associated with bevacizumab. Am J Health Syst Pharm. 2009;66:999-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 85] [Article Influence: 5.3] [Reference Citation Analysis (1)] |
| 20. | Sudo G, Tanuma T, Nakase H. Gastric Ulcer Bleeding Due to Left Gastric Artery Pseudoaneurysm. Am J Gastroenterol. 2018;113:1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Suzuki H, Iwamoto H, Shimose S, Niizeki T, Shirono T, Noda Y, Kamachi N, Yamaguchi T, Nakano M, Kuromatsu R, Koga H, Kawaguchi T. Case Report: Exacerbation of varices following atezolizumab plus bevacizumab treatment of hepatocellular carcinoma: A case series and literature review. Front Oncol. 2022;12:948293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Tang A, Hallouch O, Chernyak V, Kamaya A, Sirlin CB. Epidemiology of hepatocellular carcinoma: target population for surveillance and diagnosis. Abdom Radiol (NY). 2018;43:13-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 302] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 23. | Valluru B, Yang B, Sharma K, Adam AA, Wei D, Zhou Z, Ali MO. Significance of radiology in the diagnosis and management of ruptured left gastric artery aneurysm associated with acute pancreatitis: Case report. Medicine (Baltimore). 2019;98:e14824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |