Published online May 27, 2023. doi: 10.4240/wjgs.v15.i5.940
Peer-review started: December 21, 2022
First decision: January 17, 2023
Revised: January 28, 2023
Accepted: April 7, 2023
Article in press: April 7, 2023
Published online: May 27, 2023
Processing time: 156 Days and 1.5 Hours
Percutaneous endoscopic gastrostomy (PEG) is a well-established, minimally invasive, and easy to perform procedure for nutrition delivery, applied to individuals unable to swallow for various reasons. PEG has a high technical success rate of insertion between 95% and 100% in experienced hands, but varying complication rates ranging from 0.4% to 22.5% of cases.
To discuss the existing evidence of major procedural complications in PEG, mainly focusing on those that could probably have been avoided, had the endoscopist been more experienced, or less self-confident in relation to the basic safety rules for PEG performance.
After a thorough research of the international literature of a period of more than 30 years of published “case reports” concerning such complications, we critically analyzed only those complications which were considered - after assessment by two experts in PEG performance working separately - to be directly related to a form of malpractice by the endoscopist.
Malpractice by the endoscopist were considered cases of: Gastrostomy tubes passed through the colon or though the left lateral liver lobe, bleeding after puncture injury of large vessels of the stomach or the peritoneum, peritonitis after viscera damage, and injuries of the esophagus, spleen, and pancreas.
For a safe PEG insertion, the overfilling of the stomach and small bowel with air should be avoided, the clinician should check thoroughly for the proper trans-illumination of the light source of the endoscope through the abdominal wall and ensure endoscopically visible imprint of finger palpation on the skin at the center of the site of maximum illumination, and finally, the physician should be more alert with obese patients and those with previous abdominal surgery.
Core Tip: For a safe percutaneous endoscopic gastrostomy insertion, the physician should avoid overfilling the stomach and small bowel with air, check thoroughly for the proper trans-illumination of the light source of the endoscope through the abdominal wall, ensure endoscopically visible imprint of finger palpation on the skin at the center of the site of maximum illumination, and be more alert with obese patients and those with previous abdominal surgery.
- Citation: Stavrou G, Gionga P, Chatziantoniou G, Tzikos G, Menni A, Panidis S, Shrewsbury A, Kotzampassi K. How far is the endoscopist to blame for a percutaneous endoscopic gastrostomy complication? World J Gastrointest Surg 2023; 15(5): 940-952
- URL: https://www.wjgnet.com/1948-9366/full/v15/i5/940.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i5.940
Percutaneous endoscopic gastrostomy (PEG) was introduced into clinical practice by Gauderer et al[1] in 1980. Nowadays it is a widely used, minimally invasive procedure-a flexible feeding tube placed endoscopically through the mouth into the stomach and exiting via the abdominal wall-to administer enteral nutrition, fluids, and drugs to individuals unable to swallow for various reasons[2,3]. It is a well-established method for nutrition delivery with a high technical success rate of insertion between 95% and 100% in experienced hands[4,5].
However, there still exists a complication rate, varying from 0.4% to 22.5% of cases[6-9]. For teaching and communication purposes, the complications are classified as major and minor, depending on the severity of resulting illness; severe bleeding due to injury of visceral vessels or liver damage, perforation of hollow viscera, as well as cardiopulmonary events and aspiration pneumonia, although rare, are generally severe or even fatal, and thus categorized as major complications, which happen at a rate of 1.0%-2.4% with a mortality of 0.8%. Minor complications include, among others, peristomal infection, peristomal leakage, tube dislodgment, pneumo-peritoneum, gastric outlet obstruction, and buried bumper syndrome. An alternative classification is based on the time elapsing after PEG performance: Early and late complications, but, for no reason should a “late” complication be considered as “minor”[3,8,10-15].
For the present commentary review, we decided to focus on those complications that could have been avoided if the endoscopist had been more experienced or less self-confident and therefore less casual about the basic safety rules for PEG performance. Gastrostomy tubes passed through the colon or though the left lateral liver lobe, bleeding after puncture injury of large vessels of the stomach or the peritoneum, peritonitis after viscera damage and injuries of the esophagus, spleen, and pancreas are critically discussed in relation to who should assume the responsibility.
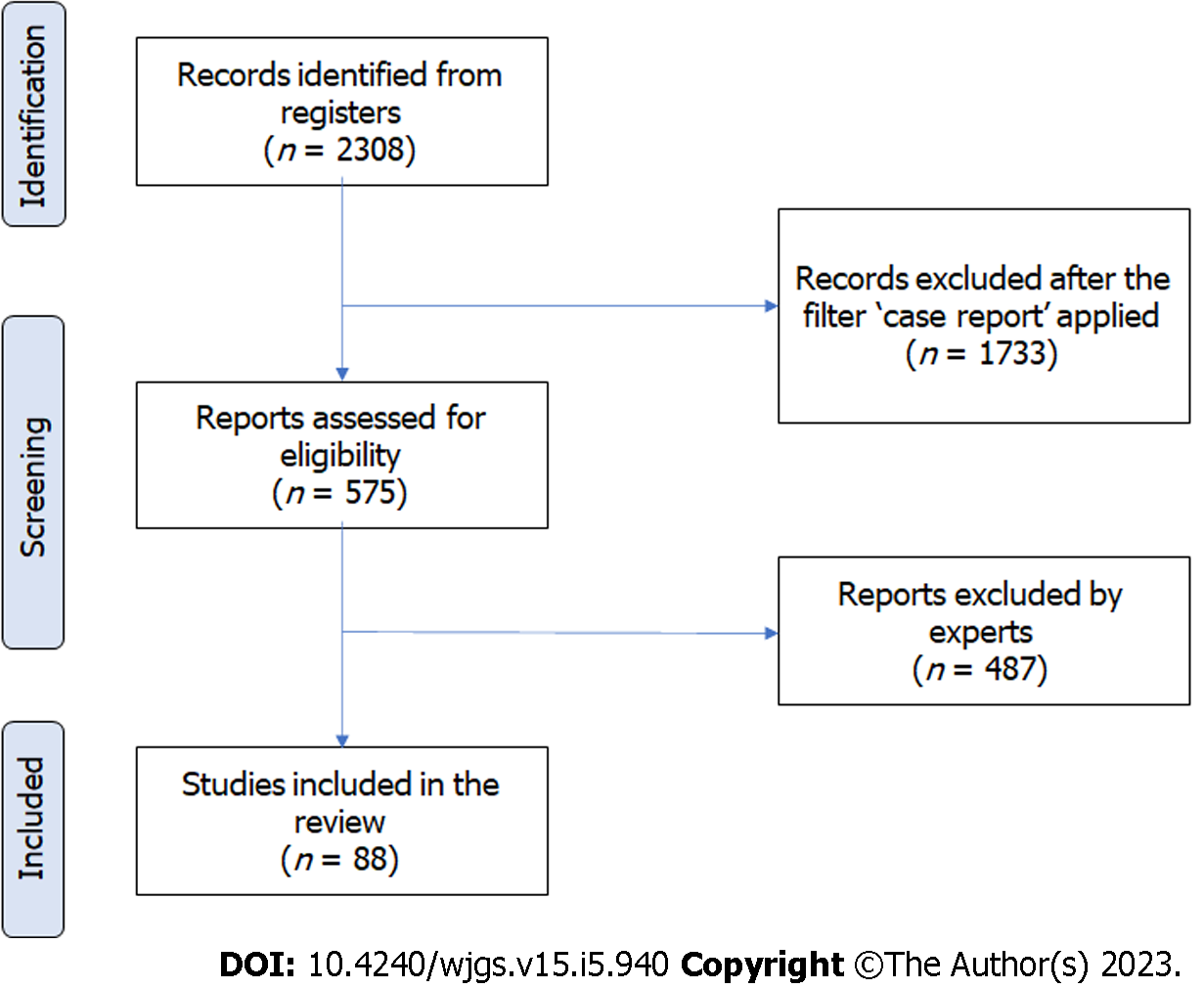
An electronic literature search of PubMed databases from their inception in 1980 to 2022 was performed to detect all published case reports or case series pertinent to a complication after PEG tube insertion. An ultimate check of databases was carried out on November 15, 2022.
For literature search purposes, the subject heading “percutaneous endoscopic gastrostomy” combined with “complications”, with AND as Boolean term, was applied to retrieve data related to the objectives of this study. The inclusion criteria were: (1) Either a “case report” or “case series”; (2) Full-text available; and (3) Human cases only. No language restriction was applied, except for Chinese.
The titles and abstracts of all publications identified were first screened and assessed and those obviously irrelevant were discarded. If eligibility could not be ascertained from the title or abstract, the full text of the article was examined. Papers deemed suitable were then reviewed by two independent reviewers to exclude, manually, all cases related to PEG tube malfunction or peristomal wound care, peristomal infections/leakage, buried bumper syndrome, and accidental dislodgement of the tube, as well as those related to sedation itself (aspiration, cardiac arrest, and similar). The references in the remaining papers were then scrutinized for additional cases, in a further effort to ensure that relevant publications were not missed.
Two qualified endoscopists (EE and KK), working independently of each other, thoroughly studied all the remaining articles describing major complications: Vascular injuries-intra/retroperitoneal bleeding, colon injuries, liver injuries, and splanchnic organ injuries. For each article that they studied, they asked themselves: “Was this complication preventable?” and “what was the wrong maneuver on the part of the endoscopist which resulted in this complication?” Based on their 35+ years’ experience each and the large number of procedures that they had performed, they separately judged and then discussed and agreed which of the complications could have been avoided had the endoscopist strictly followed the guidelines for a gastrostomy insertion.
A total of 88 complications out of the 575 cases screened were identified, i.e., those which both endoscopists agreed could have been avoided (Figure 1). They were classified according to the organ/anatomical structure injured, as follows (Table 1).
| Classification of complications |
| Colonic injuries |
| Liver injuries |
| Vascular injuries/bleeding |
| R. gastric artery |
| L. gastric artery |
| Splenic artery |
| Gastroepiploic artery |
| Portal vein |
| Splenic artery and pancreas |
| Sup. pancreatic branch of SMA and pancreas |
| Lesser curvate small vessels |
| Gastroepiploic artery pseudoaneurysm |
| L. gastric artery pseudoaneurysm |
| Gastroduodenal artery pseudoaneurysm |
| Gastric wall intramural hematoma |
| Visceral injuries |
| Esophagus |
| Posterior gastric wall |
| Jejunum |
| Spleen |
| Peritonitis |
There were a total of 50 reports on transverse colon accidental penetration by the gastrostomy tube before it entered the stomach. In detail, 29 patients remained for between 6 wk and 4 years with a PEG tube in their stomach, after it had passed through the colon; this complication was recognized only during the process of changing the gastrostomy tube, when the new one failed to be inserted into the stomach and remained in the colon. Mainly diarrhea and fecal odor sent the patient to hospital for investigation. Another 11 cases of a similar complication were recognized early, from 25 h to 2.5 mo, mainly due to fecal material exiting from the tube and/or around the gastrostomy tube (Table 2). The same complication occurred in 4 patients with previous abdominal surgery: Two cases with a history of surgical jejunostomy[16] and an exploratory laparotomy[17], with diagnosis only occurring upon gastrostomy tube replacement; in one case[18] with a right hemicolectomy in the past and difficulties in transillumination, the PEG tube was inserted through the colon and 1 wk later the internal bumper had moved within the colon lumen. A poly-trauma patient previously subjected to splenectomy[19] received a PEG inserted through the splenic flexure, recognized 2 years later within the colon lumen due to fecal odor. Two infants presented with fecal emesis 2 to 3 mo after a PEG, which was passed from the skin, through the colon, into the posterior stomach wall[20]. Finally, there were 4 more cases: One presenting 10 d later with rectal bleeding[21]; one presenting a year after PEG insertion, when the tube was obstructed[22]; one presented 3 d after PEG with abdominal distention, with the bumper being in the splenic flexure[23]; and, the last case, presenting with diarrhea 15 d after PEG placement, was found to have a colo-jejuno-gastric communication after the PEG tube had passed through the colon and jejunum before entering the stomach[24].
| Ref. | Cited | Clinical signs |
| Aschl et al[72] | Z Gastroenterol 2010; 48: 760-762 | Diarrhea and fecal odor |
| Bertolini et al[18] | World J Gastroenterol 2014; 20: 11439-11442 | Diarrhea and fecal odor |
| Brown et al[73] | Pediatr Radiol 2007; 37: 229-231 | Fecal material exiting from the tube |
| Burke et al[74] | Diagn Ther Endosc 2011; 2011: 849460 | Fecal material exiting from the tube |
| Chime et al[75] | Gastrointest Med 2020 | Fecal material exiting from the tube |
| Diéguez Castillo et al[76] | Gastroenterología y Hepatología (English Edition) 2019; 42: 39-40 | Fecal material exiting from the tube |
| Fernandes et al[77] | Gastrointestinal endoscopy 1988; 34: 368-369 | Diarrhea and fecal odor |
| Friedmann et al[78] | Parenter Enteral Nutr 2007; 31: 469-476 | Diarrhea and fecal odor |
| Guloglu et al[79] | J Laparoendosc Adv Surg Tech A 2003; 13: 69-72 | Fecal material exiting from the tube |
| Heuss et al[80] | Dtsch Med Wochenschr 2012; 137: 2043-2046 | Diarrhea and fecal odor |
| Huang et al[81] | AJR Am J Roentgenol 2005; 184: S65-66. | Fecal material exiting from the tube |
| Hwang et al[82] | Clin Endosc 2012; 45: 95-98 | Fecal material exiting from the tube |
| Kim et al[83] | Intest Res 2014; 12: 251-255 | Diarrhea and fecal odor |
| Kuriyama et al[84] | Intern Med 2016; 55: 3549 | Fecal material exiting from the tube |
| Lee et al[85] | Korean J Gastroenterol 2014; 63: 120-4 | Diarrhea and fecal odor |
| Lee et al[86] | Clin Endosc 2018; 51:196-200 | Fecal material exiting from the tube |
| Lenzen et al[19] | Journal of Gastroenterology and Hepatology 2012; 27: 1254 | Diarrhea and fecal odor |
| Lohiya et al[87] | J Am Board Fam Med 2010; 23: 681-684 | Fecal material exiting from the tube |
| Murphy et al[16] | J Am Geriatr Soc 1991; 39: 532-533 | Diarrhea and fecal odor |
| Nunes et al[88] | Turk J Gastroenterol 2019; 30:761-763 | Diarrhea and fecal odor |
| Nunes et al[89] | GE Port J Gastroenterol 2019; 26:441-447 | Diarrhea and fecal odor |
| Okutani et al[90] | Acta Med Okayama 2008; 62: 135-138 | Diarrhea and fecal odor |
| Pitsinis et al[91] | Eur J Clin Nutr 2003; 57: 876-878 | Diarrhea and fecal odor |
| Saltzberg et al[92] | JPEN J Parenter Enteral Nutr 1987; 11: 86-87 | Diarrhea and fecal odor |
| Smyth et al[93] | Nutrition 2003; 19: 905-906 | Diarrhea and fecal odor |
| Taheri et al[94] | JPEN J Parenter Enteral Nutr 2011; 35: 56-60 | Diarrhea and fecal odor |
| Tong et al[95] | Endoscopy 2007; 39 Suppl 1: E69 | Diarrhea and fecal odor |
| van Gossum et al[96] | Endoscopy 1988; 20: 161 | Diarrhea and fecal odor |
| Jiménez Varo et al[97] | Nutricion hospitalaria 2014; 29: 460-463 | Diarrhea and fecal odor |
| Winder et al[17] | Gastrointest Endosc 2016; 83: 1290-1291 | Fecal material exiting from the tube |
| Yamazaki et al[98] | Surg Endosc 1999; 13:280-282 | Diarrhea and fecal odor |
In the cases where the PEG tube penetrated the liver prior to insertion into the stomach without causing severe bleeding, patients experienced pain either a few hours later, upon feeding induction[25], or within a week (5 cases)[26-29], or after 2 wk in the case of a patient having total colectomy and ileostomy[30]. In 3 patients, the liver injury was only recognized later as a liver abscess, after the gastrostomy internal bumper accidentally moved out of the stomach[31-33]. In another patient, during the process of changing gastrostomy tube, the new one failed to be inserted into the stomach and remained in the liver, thus becoming symptomatic[34]. Finally, it is of interest to separately mention the unfortunate case of an obese patient scheduled for gastrostomy by means of radiology. The presence of a colonic loop anterior to the stomach caused the radiologic procedure to be aborted and endoscopic gastrostomy was thus decided on and performed uneventfully. On day 3 post-procedure, a computed tomography scan was performed to totally exclude the possibility of colon injury - this revealed that the gastrostomy tube had traversed hepatic segment 3, making a large adjacent hematoma, resulting in the patient’s death a few days later[35].
Additionally, there were 4 cases in which the passage of the gastrostomy tube through the left hepatic lobe parenchyma caused severe hemorrhage (hemoperitoneum), requiring surgical intervention[29,36-38].
Ectopic insertion of the needle in the anatomical area of the major gastric curvature caused injury of the gastric artery (2 cases)[15], or its left branch[39], of the splenic artery[40], and of the gastro-epiploic artery (2 cases)[41,42]. Needle puncture at the lesser curvature led to: A huge retroperitoneal hemorrhage due to rupture of the splenic and superior mesenteric veins near the confluence to the portal vein[38] and severe injury to the splenic artery and pancreas[42], both occurring in previous cholecystectomy patients; massive hemoperitoneum after injury of small vessels on the lesser curvature, probably related to a first failed attempt to insert the needle into the stomach, followed by a second attempt[43]; and severe injury to the pancreas and the pancreatic branch of the superior mesenteric artery after needle insertion from the anterior stomach wall and penetration of the posterior wall towards the pancreas being just behind[44].
The formation of a pseudo-aneurysm after puncture of the gastro-epiploic artery[45]; of the left gastric artery[45,46]; and of the gastro-duodenal artery[47] was also reported. An intra-mural hematoma of the gastric wall also developed in a patient with platelet dysfunction and on a low dose of aspirin[48].
Two cases of esophageal catastrophic damage related to PEG placement were reported. In a 3-mo-old boy weighing 3.7 kg, the pulling of a 18CH gastrostomy tube immediately led to esophageal intussusception towards the stomach and thus complete esophageal transection[49]. The other case was an obese, multi-trauma patient, on whom PEG procedure was difficult[50]. Without the help of transillumination, and only using finger pressure, 3 attempts, at a 45° angle, were made to insert the needle into the stomach. The patient became tachycardic, hypotensive, and progressively febrile, with upper abdominal tenderness, mediastinitis, thickening of the pericardium, and bilateral pleural effusions, leading, finally, on day 14 to an urgent left lateral-posterior thoracotomy which revealed a small hole on the anterior esophageal wall at the esophagogastric junction, covered by omentum. Additionally, the PEG was dislocated in the subcutaneous adipose tissue.
A case of gastric volvulus was reported in a 10-mo-old infant; PEG was performed at the age of 1 mo, under general anaesthesia. Unfortunately, the gastrostomy tube passed between the gastric curvature and the transverse colon to be inserted finally into the posterior gastric wall, causing the stomach to twist along its organo-axis and compromising the gastric outlet[51].
Four cases of PEG tube passage through the jejunal lumen prior to entering the stomach were also found. These cases remained silent from 8.5 to 24 mo, and were only discovered by symptoms occurring upon tube replacement[52-55].
Microbial peritonitis occurred in 3 cases: One following PEG on the posterior gastric wall[15] and another two after penetration of the jejunum[15] and transverse colon[40], both being between the abdominal and the gastric wall. Finally, there were two cases of severe spleen injuries[48,56] in patients with previous surgeries.
The PEG procedure is a well-established method for safe creation of a gastrostomy, without surgery, and in most cases, without general anaesthesia. The goal of PEG is to endoscopically insert a flexible gastrostomy catheter via the mouth-esophagus-stomach route - by pulling it from the outside - to be externalized in the mid-abdomen, which allows easy delivery of commercially available liquid nutrients to the patient. While most PEG procedures have yielded positive long-term outcomes, there are substantial adverse events associated with their performance; some of them, directly related to the technical part of the operation itself, would have been avoided if the manipulations for tube implantation had been carried out in accordance with the generally accepted guidelines[2-4,6-9]. In our opinion, only an inexperienced or super-experienced endoscopist would dare to ignore these rules: The former from ignorance of danger and of basic rules and the latter from excessive self-confidence or arrogance.
In the present study, we decided to review and comment on the adverse events reported in the literature, irrespective of their being either major or minor, early or late, after two experienced endoscopists, each with almost 40 years of experience in performing PEG, were tasked to critically examine the literature and identify those complications that could have been prevented.
The displacement of the transverse colon in close proximity to or over the anterior gastric wall, due mainly to stomach and small bowel overinflation at the beginning of the procedure, can predispose the patient to colonic injury during the needle puncture for PEG placement[8,10,24,57-59]. The endoscopist must take into consideration that the laxity of the colonic mesentery is more common among elderly patients[23] and that both chronic constipation and previous abdominal surgery are serious parameters which further increase the risk of colon penetration if the colon interposes between the abdominal wall and the stomach, creating colo-gastric communication[60,61]. Although colon perforation is considered a severe trauma needing emergency treatment due to incipient fecal peritonitis, in most cases it is totally asymptomatic. Some transient episodes of fever or ileus may occur in a few patients, the diagnosis of which is often difficult, given the problems in communication due to underlying altered mental status[3]. In most cases, colon compression between the external and internal bumpers of the gastrostomy tube partially closes the opening and thus minimizes the leakage, while the artificial liquid enteral formulas given for feeding further minimize the existence of colon over-distension due to a bulk mass of feces.
On the other hand, when the PEG is removed for replacement or accidentally pulled back a little, it is almost impossible to reinsert the replacement tube through the colon, into the stomach; for this reason, the technique of exchanging the tube over a guidewire can prove a safe solution. Once feeding restarts, diarrhea occurs, due to the acceleration of increased motility of the colon and thus the rapid passage of undigested food to the anus, this being the most common symptom for referral of the patient to the treating physician, leading to recognition of the complication. In a few cases, leakage of feces through the cutaneous opening helps diagnosis, while in the case of total removal of the tube a colo-cutaneous fistula is created[8,11,61].
Passage of the gastrostomy tube through the liver may happen in a similar way to that occurring with the colon, when the left lateral liver lobe interposes between the abdominal wall and the stomach. Although such an injury, which is puncture of the “bloody” liver and passage of the PEG tube through into the stomach, would be expected to be associated with severe intraperitoneal bleeding, most of the cases have no prominent hemorrhage, probably because of liver compression between the internal and external bumpers of the gastrostomy tube. However, bleeding occurs both at the time of PEG tube removal for replacement, and more extensively as the endoscopist tries to insert and inflate the balloon of a new tube[8,10,11,57,61].
The main reason for this complication is the violation of standard rules: (1) When liver tissue exists between the abdominal wall and the stomach, it is impossible to identify an area of maximum trans-illumination on the abdominal wall, since there is only a rather diffuse light, only visible in thin individuals; (2) Even more distinctly, the finger imprint from the outside palpation is not clearly identifiable as a “point” but rather only as an extra-lumen pressure moving the anterior wall of the stomach; (3) Regarding the “safe tract” technique - that is the technique involving constant aspiration while advancing the needle - it is our personal opinion that it proves more reliable when performed in such cases. In case the needle enters the liver accidentally, it is much easier to aspirate blood and be aware of the complication. On the contrary, if the needle enters the colon, fecal matter may not be aspirated, making the endoscopist unaware of the complication until it is possibly too late; and (4) Finally, liver hilum palpation is a good practice, totally forgotten nowadays[3,11,62].
Significant bleeding happens when the needle “blindly” punctures the underlying tissues; large or small arteries of the great and lesser gastric curvature or the gastric insisura may occasionally - and easily - be found on the route of the needle. Of course, just below the epigastrium is located the anterior gastric wall, which does not have large vessels; when excess air volume over-inflates the stomach, it can be twisted either clockwise or counterclockwise along its organ axis, thus exposing the great or the lesser curvature and their vessels, and more extremely, perhaps the posterior gastric wall - there were at least 5 cases of PEG performed in the posterior gastric wall[15,20,44,51]. This stomach rotation has been fully documented by Croaker et al[63], who inserted a laparoscopic camera into the abdomen in order to study the movement of the viscera when inflated[58,64].
Another dangerous condition for bleeding is the previously operated abdomen. Thick adhesion bundles, sometimes containing a large vessel, pull and rotate the stomach and the gut, changing their orientation in the abdominal cavity. Characteristic are the cases of previous cholecystectomy patients, in whom shrinkage of the area between the liver, duodenum, and gastric insisura led to severe needle-induced splenic artery and pancreatic tissue injury[38,42]. Much more dangerous is the situation after a previous colectomy or gastrectomy of any type, pancreatic surgery, or aortic surgery[60]. However, in these cases there is the surgical incision scar to warn the operator that some anatomical alterations may exist in the abdominal cavity - they must, however, notice it.
Finally, there are reported injuries of the splenic artery, the mesenteric veins, and even the aorta, all leading to hemo-peritoneum and/or retro-peritoneal hematomas. Additionally, but of less seriousness, are injuries to abdominal wall vessels and the rectus sheath, which, fortunately, are immediately recognizable and therefore, generally, stopped by applying constant pressure for a few minutes between the internal and external gastrostomy bumpers and over the abdominal wound[3,8]. A negative paradigm is if the operator, despite recognizing a large intramural hematoma in progress, stops the procedure. The expansion of the hematoma would be controlled if it was immediately compressed by the bumpers after finishing PEG insertion[48].
On the other hand, although there are detailed guidelines and strict warnings to stop some antiplatelet drugs, there are cases where these are not heeded. When the endoscopist decides to perform the PEG simply at the request of the treating physician, despite the European Society of Gastrointestinal Endoscopy (ESGE) recommendations on anti-coagulant use[4,65,66], the responsibility rests entirely with the endoscopist. There is no case for an urgent endoscopic gastrostomy.
Among the described injuries to the small bowel and colon causing peritonitis, as well as to the spleen and pancreas due to over-inflation of the stomach followed by rotation along the organ axis, three cases of great importance need to be noted[8,58,59]. The first is an esophageal intussusception and then transection in a 3-mo-old boy, weighing 3.7 kg, to whom insertion of an adult gastrostomy tube of 18Ch was attempted[49]. The second case is a gastric volvulus, following insertion of the PEG into the posterior gastric wall, due to stomach over-inflation, finally causing compromised gastric emptying[51]. The third is the case of an obese, multi-trauma patient; without trans-illumination, 3 puncture attempts at a 45° angle, resulted in a gastrostomy placement but also an esophageal perforation which were fortunately recognized after 14 d of suffering mediastinitis[50].
It is common sense that PEG-procedure-related complications are undoubtedly associated with the endoscopist’s skill and adherence to the basic principles of good practice; both an inexperienced and a super-expert endoscopist, based on the one hand on lack of skill and the other on an excess of confidence, are likely to be implicated in an iatrogenic injury. While the inexperienced practitioner would probably persist longer, possibly resulting in a serious complication, likely to remain temporarily unrecognized, an expert might consider that he could rush the rules, because of his skill, and thus also involve the patient in severe complications, only recognized much later.
But what is the meaning of ‘inexperienced’ and ‘super-expert’ in relation to the endoscopist? Practically, an experienced practitioner is somebody well-trained in the past, who continuously renews his skills and maintains his competence by means of frequent, repetitive practice over the years. Officially, there is no standard curriculum for endoscopy training in performing PEG, as with many other much newer interventional techniques. The latest curricula, from 2019 thereafter, issued by the ESGE are those for training in performing endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound, and electrostatic discharge (ESD), which highly recommend a minimum, non-interrupted training period of 12 mo in a high volume, qualified, training center and involving the performance of more than 300 ERCPs. As a foundation, the endoscopist should have previously achieved competence in upper gastrointestinal endoscopy, through personal experience of at least 300 gastroscopies, followed by at least a further year, and ideally 3 years, of dedicated training that is likely required to reach competence. For ESD, initial experience of at least 20 procedures in animal or ex vivo models is highly recommended, and in order to maintain proficiency, ESGE recommends a minimum case load of 25 ESD procedures per year to demonstrate maintenance of competence. The attainment of competence in interventional or therapeutic endoscopy is not a single event, but a career-long process - meaning that endoscopists should be continually performing such procedures[67-69].
In this commentary review, we discuss the existing evidence of major procedural complications after a PEG insertion, while focusing on the exact cause of malpractice, as documented by cases meticulously collected from the literature over a period of more than 35 years. In other words, we have tried to find and underline the errors in the manipulations made which result in each specific complication.
Initially we note that the serious complications may occur related mainly to the type and location of the needle puncture[35,36]. However, to the best of our knowledge, few reports have addressed the relationship between PEG site and complications. Lee et al[13] found by a multivariate analysis that PEG tube insertion in the upper body of the stomach was a significant risk factor for complication occurrence, with the most obvious reason being the relatively long distance between the gastric and abdominal walls in the upper body as compared with the lower gastric body; this distance produces stronger tension between the abdominal and gastric walls during stomach contraction, inducing slow or incomplete adherence and thus fistula formation[64].
An experienced endoscopist, prior to performing the PEG procedure, lays the patient in a reverse or anti-Trendelemburg position, so that viscera moves downward to the pelvis. He/she also avoids overfilling the stomach and small bowel with air, which may ‘lift’ the transverse colon and increase the probability of colon, or even intestinal injury. He/she then checks thoroughly for the proper trans-illumination through the abdominal wall of the light source of the distal tip of the endoscope, and ensures the endoscopically visible imprint of his finger palpation on the patient’s skin, at the center of the site of maximum illumination[7,57,62,70,71]. He/she is also extra cautious in the case of previous abdominal surgery, which remains a relative contra-indication for the young and inexperienced endoscopist[60], as is also obesity. In every case, he is careful to insert the needle strictly at a 90° angle to the skin, to ensure both the shortest route of the tube within the body and, mainly, so the abdominal opening is in line with the gastric opening, both of which will facilitate the proper adhesion between the stomach and abdominal walls. When the two openings are not aligned, the tension is likely to lead to tube dislodgement and peritonitis. Finally, he/she avoids multiple needle punctures - failure means that there is a violation of rules of trans-illumination and finger palpation, and even one additional puncture may be the cause of peritonitis or severe bleeding.
When transillumination or visible imprint or both are not clear, the endoscopist must understand that he/she violates the standard requirements and take full responsibility for any subsequent complications. Phrases such as “I have the feeling the stomach is just behind the xiphoid” are absolutely inappropriate, indeed wrong, and a bad example for younger endoscopists. The same applies to the use of the “safe tract” technique, which is endoscopic visualization of the needle and simultaneous return of air into the fluid-filled[57]. Return of fluid or gas prior to endoscopic visualization of the tip of the needle in the stomach lumen when it is inserted under continuous suction, means that the needle has passed through another organ interposed between the stomach and the abdominal wall, although a negative test does not provide a hundred percent certainty of no viscera in-between[17].
As a conclusion, we have to accept that complications will continue to occur, even in high volume centers with well qualified practitioners; however, both young and experienced endoscopists must understand and deeply believe that they will not be blamed for stopping a PEG procedure in the case of obscure trans-illumination and an unsatisfactory palpation test, and much more in the case of a previously operated abdomen. On the contrary, they will and should be blamed in the case of a preventable injury, which may finally cost even the life of an albeit high risk patient.
This study was carried out by specialists who are involved on a daily basis both in the performance of gastrostomies and in the management of their complications, which often have disastrous consequences. This study aimed to identify the problems internationally and to find possible methods of preventing them.
Trying to figure out and analyze the percutaneous endoscopic gastrostomy (PEG) tubes' complications, and focus on those that could be predicted and furthermore avoided.
To investigate the international literature in order to clarify the importance and the severity of these complications, and the possible ways of avoiding them.
A 30-year database research was carried out, investigating the literature on PubMed, using the terms “percutaneous endoscopic gastrostomy” AND “complications”, and all the case reports or case series were included, with the only language restriction being Chinese.
We identified 2308 articles. Only 575 were included according to the research criteria placed. After expertise investigation, 88 articles were in the final selection.
The complications that can arise from the potentially simple technique of the PEG are of great concern to the international scientific community.
Complications of PEG tube placement should be avoided.
We would like to express our sincere thanks to Emeritus Prof. Efthymios Eleftheriadis, Surgeon-Endoscopist, and former Head of the Endoscopy Department, Aristotle University of Thessaloniki, for the critical revision of the collected literature.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Masaki S, Japan; Tang P, China S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Chen YX
| 1. | Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1408] [Cited by in RCA: 1299] [Article Influence: 28.9] [Reference Citation Analysis (1)] |
| 2. | Bischoff SC, Austin P, Boeykens K, Chourdakis M, Cuerda C, Jonkers-Schuitema C, Lichota M, Nyulasi I, Schneider SM, Stanga Z, Pironi L. ESPEN guideline on home enteral nutrition. Clin Nutr. 2020;39:5-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 164] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 3. | Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20:7739-7751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 416] [Cited by in RCA: 340] [Article Influence: 30.9] [Reference Citation Analysis (8)] |
| 4. | Arvanitakis M, Gkolfakis P, Despott EJ, Ballarin A, Beyna T, Boeykens K, Elbe P, Gisbertz I, Hoyois A, Mosteanu O, Sanders DS, Schmidt PT, Schneider SM, van Hooft JE. Endoscopic management of enteral tubes in adult patients - Part 1: Definitions and indications. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2021;53:81-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 51] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 5. | Tsaousi G, Stavrou G, Kapanidis K, Michalopoulos A, Kotzampassi K. Unsedated Outpatient Percutaneous Endoscopic Gastrostomy in Stroke Patients: Is It Feasible and Safe? Surg Laparosc Endosc Percutan Tech. 2019;29:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Dietrich CG, Schoppmeyer K. Percutaneous endoscopic gastrostomy - Too often? World J Gastroenterol. 2020;26:2464-2471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (9)] |
| 7. | Hucl T, Spicak J. Complications of percutaneous endoscopic gastrostomy. Best Pract Res Clin Gastroenterol. 2016;30:769-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 8. | Schrag SP, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, Martin ND, Hoey BA, Stawicki SP. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407-418. [PubMed] |
| 9. | Stenberg K, Eriksson A, Odensten C, Darehed D. Mortality and complications after percutaneous endoscopic gastrostomy: a retrospective multicentre study. BMC Gastroenterol. 2022;22:361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 10. | Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20:8505-8524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 325] [Cited by in RCA: 269] [Article Influence: 24.5] [Reference Citation Analysis (10)] |
| 11. | Boeykens K, Duysburgh I. Prevention and management of major complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol. 2021;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Boeykens K, Duysburgh I, Verlinden W. Prevention and management of minor complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol. 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Reference Citation Analysis (0)] |
| 13. | Lee SP, Lee KN, Lee OY, Lee HL, Jun DW, Yoon BC, Choi HS, Kim SH. Risk factors for complications of percutaneous endoscopic gastrostomy. Dig Dis Sci. 2014;59:117-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Lynch CR, Fang JC. Prevention and management of complications of percutaneous endoscopic gastrostomy (PEG) tubes. Pract Gastroenterology. 2004;28:66-76. |
| 15. | Schurink CA, Tuynman H, Scholten P, Arjaans W, Klinkenberg-Knol EC, Meuwissen SG, Kuipers EJ. Percutaneous endoscopic gastrostomy: complications and suggestions to avoid them. Eur J Gastroenterol Hepatol. 2001;13:819-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Murphy S, Pulliam TJ, Lindsay J. Delayed gastrocolic fistula following percutaneous endoscopic gastrostomy (PEG). J Am Geriatr Soc. 1991;39:532-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Winder JS, Staszak RM, Pauli EM. Multimodal endoscopic management of iatrogenic transverse colon injuries from a percutaneous endoscopic gastrostomy tube. Gastrointest Endosc. 2016;83:1290-1291. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Bertolini R, Meyenberger C, Sulz MC. First report of colonoscopic closure of a gastrocolocutaneous PEG migration with over-the-scope-clip-system. World J Gastroenterol. 2014;20:11439-11442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Lenzen H, Weismüller T, Bredt M, Bahr M. Education and imaging. Gastrointestinal: PEG feeding tube migration into the colon; a late manifestation. J Gastroenterol Hepatol. 2012;27:1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Stefan MM, Holcomb GW 3rd, Ross AJ 3rd. Cologastric fistula as a complication of percutaneous endoscopic gastrostomy. JPEN J Parenter Enteral Nutr. 1989;13:554-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 21. | Alhazmi G, Alsabri M, Alsuwat S, Al-Zangabi A, Al-Zahrani A, Shariff MK. Rectal Bleeding after Insertion of a Percutaneous Endoscopic Gastrostomy Tube. Case Rep Gastroenterol. 2020;14:637-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Siddique I, Krishnamurthy M, Choubey S, Gudavalli P, Bharathan T, Pachter BR. Colocutaneous fistula: a rare and silent complication of percutaneous endoscopic gastrostomy. Dig Dis Sci. 1996;41:301-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Ahmad J, Thomson S, McFall B, Scoffield J, Taylor M. Colonic injury following percutaneous endoscopic-guided gastrostomy insertion. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Berger SA, Zarling EJ. Colocutaneous fistula following migration of PEG tube. Gastrointest Endosc. 1991;37:86-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Picazo-Ferrera K, Escobedo-Paredes DM, Herrera-Servín MA, Hernández-Guerrero AI, Ramírez-Solis ME. Incidental transhepatic placement of a percutaneous endoscopic gastrostomy tube. Presentation of a rare complication and a literature review. Rev Gastroenterol Mex (Engl Ed). 2020;85:479-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Gubler C, Wildi SM, Bauerfeind P. Liver injury during PEG tube placement: report of two cases. Gastrointest Endosc. 2005;61:346-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 27. | Herta T, Hecker M, van Boemmel F, Hoffmeister A, Karlas T. Sonographic diagnosis of transhepatic placement of a percutaneous endoscopic gastrostomy (PEG) tube. Endoscopy. 2015;47 Suppl 1 UCTN:E453-E454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Mercky P, Le Goffic A, Ah-Soune P. Transhepatic endoscopic gastrostomy. Endoscopy. 2014;46 Suppl 1 UCTN:E385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Shaw J, Casey K. A PEG tube through the liver. Am J Gastroenterol. 2009;104:1323-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Imam Z, Simons-Linares CR. Transhepatic Insertion of Percutaneous Endoscopic Gastrostomy Tube. Case Rep Gastrointest Med. 2020;2020:4516032. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Adams SD, Baker D, Takhar A, Beattie RM, Stanton MP. Complication of percutaneous endoscopic gastrostomy. Arch Dis Child. 2014;99:788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 32. | Atalaia-Martins C, Barbeiro S, Marcos P, Gil I, Cotrim I. Intrahepatic Migration of Gastrostomy Tube after Inadvertent Transhepatic PEG Placement. ACG Case Rep J. 2017;4:e76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Rafiq A, Abbas N, Tariq H, Nayudu SK. Gastro-Hepatic Fistula with Liver Abscess: A Rare Complication of a Common Procedure. Am J Case Rep. 2015;16:652-657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Chaer RA, Rekkas D, Trevino J, Brown R, Espat J. Intrahepatic placement of a PEG tube. Gastrointest Endosc. 2003;57:763-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Chhaparia A, Hammami MB, Bassuner J, Hachem C. Trans-Hepatic Percutaneous Endoscopic Gastrostomy Tube Placement: A Case Report of A Rare Complication and Literature Review. Gastroenterology Res. 2018;11:145-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Burke DT, Geller AI. Peritonitis secondary to the migration of a trans-hepatically-placed percutaneous endoscopic gastrostomy tube: a case report. Arch Phys Med Rehabil. 2009;90:354-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Fyock CJ, Kethu SR. PEG placement causing liver perforation. J Clin Gastroenterol. 2009;43:385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 38. | Lau G, Lai SH. Fatal retroperitoneal haemorrhage: an unusual complication of percutaneous endoscopic gastrostomy. Forensic Sci Int. 2001;116:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Bunai Y, Akaza K, Nagai A, Tsujinaka M, Jiang WX. Iatrogenic rupture of the left gastric artery during percutaneous endoscopic gastrostomy. Leg Med (Tokyo). 2009;11 Suppl 1:S538-S540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Amann W, Mischinger HJ, Berger A, Rosanelli G, Schweiger W, Werkgartner G, Fruhwirth J, Hauser H. Percutaneous endoscopic gastrostomy (PEG). 8 years of clinical experience in 232 patients. Surg Endosc. 1997;11:741-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 41. | Lewis MB, Lewis JH, Marshall H, Lossef SV. Massive hemorrhage complicating percutaneous endoscopic gastrostomy: treatment by means of transcatheter embolization of the right and left gastroepiploic arteries. J Vasc Interv Radiol. 1999;10:319-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Smale E, Davison AM, Smith M, Pritchard C. Fatal intra-abdominal haemorrhage following percutaneous endoscopic gastrostomy. BMJ Case Rep. 2009;2009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 43. | Bordes J, Hornez E, Kenane N, Carrere C, Asencio Y, Goutorbe P. The complications of percutaneous endoscopic gastrostomy. Crit Care. 2008;12:422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 44. | Lee SH, Moon HS, Park JH, Kim JS, Kang SH, Lee ES, Kim SH, Sung JK, Lee BS, Jeong HY. Percutaneous Endoscopic Gastrostomy Tube Insertion-induced Superior Mesenteric Artery Injury Treated with Angiography. Korean J Gastroenterol. 2018;72:308-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Shigoka H, Maetani I, Saito M. Pseudoaneurysm developed after percutaneous endoscopic gastrostomy: a report of two cases. Eur J Gastroenterol Hepatol. 2013;25:1484-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Zivari K, Niknam N, Lapin S, Rahmani R, Mayer I. Ruptured Gastric Artery Pseudoaneurysm: A Life-threatening Complication of Percutaneous Endoscopic Gastrostomy (PEG): 1874. Am J Gastroenterol. 2017;112:S1031-S1032. [DOI] [Full Text] |
| 47. | João M, Alves S, Carvalheiro V, Areia M. An Astounding Percutaneous Endoscopic Gastrostomy Complication: A Pseudoaneurysm of Gastroduodenal Artery. GE Port J Gastroenterol. 2021;28:294-296. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Lee CC, Ravindranathan S, Choksi V, Pudussery Kattalan J, Shankar U, Kaplan S. Intraoperative Gastric Intramural Hematoma: A Rare Complication of Percutaneous Endoscopic Gastrostomy. Am J Case Rep. 2016;17:963-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Güvenç BH, Raşa K, Güvenç S. The presence of percutaneous endoscopic gastrostomy (PEG)-related postprocedural pneumoperitoneum. Endoscopy. 2009;41 Suppl 2:E269-E270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 50. | Papakonstantinou K, Karagiannis A, Tsirantonaki M, Konstantinidis A, Spirou S, Skottis I, Karabinis A. Mediastinitis complicating a percutaneous endoscopic gastrostomy: a case report. BMC Gastroenterol. 2003;3:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 51. | Sookpotarom P, Vejchapipat P, Chongsrisawat V, Mahayosnond A. Gastric volvulus caused by percutaneous endoscopic gastrostomy: a case report. J Pediatr Surg. 2005;40:e21-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Karhadkar AS, Schwartz HJ, Dutta SK. Jejunocutaneous fistula manifesting as chronic diarrhea after PEG tube replacement. J Clin Gastroenterol. 2006;40:560-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | Kubiak R, Wilcox DT, Spitz L. Gastrojejunal fistula after insertion of percutaneous endoscopic gastrostomy. J Pediatr Surg. 1999;34:1287-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 54. | Lim JU, Shin HP, Lee JI, Cha JM, Joo KR. Malposition of a percutaneous endoscopic gastrostomy tube in the jejunum. Endoscopy. 2010;42 Suppl 2:E116. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 55. | Quadri AH, Puetz TR, Dindzans V, Canga C, Sincaban M. Enterocutaneous fistula: a rare complication of PEG tube placement. Gastrointest Endosc. 2001;53:529-531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 56. | Patel BB, Andrade C, Doraiswamy V, Amodeo D. Splenic Avulsion Following PEG Tube Placement: A Rare but Serious Complication. ACG Case Rep J. 2014;2:21-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 57. | Baskin WN. Acute complications associated with bedside placement of feeding tubes. Nutr Clin Pract. 2006;21:40-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 58. | Okita A, Ohtani J. A Rare Case of Gastrojejunocutaneous Fistula after Percutaneous Endoscopic Gastrostomy. Acta Med Okayama. 2019;73:177-180. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 59. | Patwardhan N, McHugh K, Drake D, Spitz L. Gastroenteric fistula complicating percutaneous endoscopic gastrostomy. J Pediatr Surg. 2004;39:561-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 60. | Eleftheriadis E, Kotzampassi K. Percutaneous endoscopic gastrostomy after abdominal surgery. Surg Endosc. 2001;15:213-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 61. | Fugazza A, Capogreco A, Cappello A, Nicoletti R, Da Rio L, Galtieri PA, Maselli R, Carrara S, Pellegatta G, Spadaccini M, Vespa E, Colombo M, Khalaf K, Repici A, Anderloni A. Percutaneous endoscopic gastrostomy and jejunostomy: Indications and techniques. World J Gastrointest Endosc. 2022;14:250-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (3)] |
| 62. | Kinoshita Y, Udagawa H, Kajiyama Y, Tsutsumi K, Ueno M, Nakamura T, Watanabe G, Akiyama H. Cologastric fistula and colonic perforation as a complication of percutaneous endoscopic gastrostomy. Surg Laparosc Endosc Percutan Tech. 1999;9:220-222. [PubMed] |
| 63. | Croaker GD, Najmaldin AS. Laparoscopically assisted percutaneous endoscopic gastrostomy. Pediatr Surg Int. 1997;12:130-131. [PubMed] |
| 64. | Suzuki H, Joshita S, Nagaya T, Sato K, Ito A, Suga T, Umemura T. Relationship of early acute complications and insertion site in push method percutaneous endoscopic gastrostomy. Sci Rep. 2020;10:20551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 65. | Lucendo AJ, Sánchez-Casanueva T, Redondo O, Tenías JM, Arias Á. Risk of bleeding in patients undergoing percutaneous endoscopic gastrotrostomy (PEG) tube insertion under antiplatelet therapy: a systematic review with a meta-analysis. Rev Esp Enferm Dig. 2015;107:128-136. [PubMed] |
| 66. | Veitch AM, Vanbiervliet G, Gershlick AH, Boustiere C, Baglin TP, Smith LA, Radaelli F, Knight E, Gralnek IM, Hassan C, Dumonceau JM. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Gut. 2016;65:374-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 67. | Bisschops R, Dekker E, East JE, Johnson G, Pimentel-Nunes P, Sanders DS, Dinis-Ribeiro M, Ponchon T. European Society of Gastrointestinal Endoscopy (ESGE) curricula development for postgraduate training in advanced endoscopic procedures: rationale and methodology. Endoscopy. 2019;51:976-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 68. | Johnson G, Webster G, Boškoski I, Campos S, Gölder SK, Schlag C, Anderloni A, Arnelo U, Badaoui A, Bekkali N, Christodoulou D, Czakó L, Fernandez Y Viesca M, Hritz I, Hucl T, Kalaitzakis E, Kylänpää L, Nedoluzhko I, Petrone MC, Poley JW, Seicean A, Vila J, Arvanitakis M, Dinis-Ribeiro M, Ponchon T, Bisschops R. Curriculum for ERCP and endoscopic ultrasound training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2021;53:1071-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 72] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 69. | Pimentel-Nunes P, Pioche M, Albéniz E, Berr F, Deprez P, Ebigbo A, Dewint P, Haji A, Panarese A, Weusten BLAM, Dekker E, East JE, Sanders DS, Johnson G, Arvanitakis M, Ponchon T, Dinis-Ribeiro M, Bisschops R. Curriculum for endoscopic submucosal dissection training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2019;51:980-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 103] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 70. | Bui HD, Dang CV, Schlater T, Nghiem CH. A new complication of percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1988;83:448-451. [PubMed] |
| 71. | Shou-jiang T, Ruonan W. Percutaneous Endoscopic Gastrostomy (pull method) and Jejunal Extension Tube Placement. Video J Encyclopedia GI Endoscopy. 2:40-45. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 72. | Aschl G, Fritz E, Stadler B, Fleischer M, Priglinger H, Knoflach P. [Colocutaneous fistula after a PEG procedure with introducer technique and gastropexy]. Z Gastroenterol. 2010;48:760-762. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 73. | Brown S, McHugh K, Ledermann S, Pierro A. CT findings in gastrocolic fistula following percutaneous endoscopic gastrostomy. Pediatr Radiol. 2007;37:229-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 74. | Burke DT, Geller AI, Carayannopoulos AG, Goldstein R. Inadvertent Percutaneous Endoscopic Gastrostomy Tube Placement through the Transverse Colon to the Stomach Causing Intractable Diarrhea: A Case Report. Diagn Ther Endosc. 2011;2011:849460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 75. | Chime C, Baiomi A, Kumar K, Patel H, Dev A, Makker J. Endoscopic Repair of Gastrocolic and Colocutaneous Fistulas Complicating Percutaneous Endoscopic Gastrostomy Tube. Case Rep Gastrointest Med. 2020;2020:7262514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 76. | Diéguez Castillo C, Roa Colomo A, Díaz Alcázar MDM, Martínez Tirado P, Palacios Pérez Á. Late detection of early complication after placement of percutaneous endoscopic gastrostomy: Asymptomatic transluminal perforation of the colon. Gastroenterol Hepatol. 2019;42:39-40. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 77. | Fernandes ET, Hollabaugh R, Hixon SD, Whitington G. Late presentation of gastrocolic fistula after percutaneous gastrostomy. Gastrointest Endosc. 1988;34:368-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 78. | Friedmann R, Feldman H, Sonnenblick M. Misplacement of percutaneously inserted gastrostomy tube into the colon: report of 6 cases and review of the literature. JPEN J Parenter Enteral Nutr. 2007;31:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 79. | Guloglu R, Taviloglu K, Alimoglu O. Colon injury following percutaneous endoscopic gastrostomy tube insertion. J Laparoendosc Adv Surg Tech A. 2003;13:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 80. | Heuss LT, Spalinger R. [The colocutaneous fistula - a rare complication of percutaneous endoscopic gastrostomy]. Dtsch Med Wochenschr. 2012;137:2043-2046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 81. | Huang SY, Levine MS, Raper SE. Gastrocolic fistula with migration of feeding tube into transverse colon as a complication of percutaneous endoscopic gastrostomy. AJR Am J Roentgenol. 2005;184:S65-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 82. | Hwang JH, Kim HW, Kang DH, Choi CW, Park SB, Park TI, Jo WS, Cha DH. A case of endoscopic treatment for gastrocolocutaneous fistula as a complication of percutaneous endoscopic gastrostomy. Clin Endosc. 2012;45:95-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 83. | Kim HS, Bang CS, Kim YS, Kwon OK, Park MS, Eom JH, Baik GH, Kim DJ. Two cases of gastrocolocutaneous fistula with a long asymptomatic period after percutaneous endoscopic gastrostomy. Intest Res. 2014;12:251-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 84. | Kuriyama A. Gastrocolocutaneous Fistula due to Percutaneous Endoscopic Gastrostomy Placement. Intern Med. 2016;55:3549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 85. | Lee HJ, Choung RS, Park MS, Pyo JH, Kim SY, Hyun JJ, Jung SW, Koo JS, Lee SW, Choi JH. Two cases of uncommon complication during percutaneous endoscopic gastrostomy tube replacement and treatment. Korean J Gastroenterol. 2014;63:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 86. | Lee J, Kim J, Kim HI, Oh CR, Choi S, Noh S, Na HK, Jung HY. Gastrocolocutaneous Fistula: An Unusual Case of Gastrostomy Tube Malfunction with Diarrhea. Clin Endosc. 2018;51:196-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 87. | Lohiya GS, Tan-Figueroa L, Krishna V. Intermittent diarrhea as a delayed presentation of percutaneous endoscopic gastrostomy (PEG)-associated fistula. J Am Board Fam Med. 2010;23:681-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 88. | Nunes G, Oliveira G, Cortez-Pinto J, Cruz J, Fonseca J. Gastrocolocutaneous fistula: An undetected complication of colon transfixation during percutaneous endoscopic gastrostomy. Turk J Gastroenterol. 2019;30:761-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 89. | Nunes G, Paiva de Oliveira G, Cruz J, Santos CA, Fonseca J. Long-Term Gastrocolocutaneous Fistula after Endoscopic Gastrostomy: How Concerned Should We Be? GE Port J Gastroenterol. 2019;26:441-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 90. | Okutani D, Kotani K, Makihara S. A case of gastrocolocutaneous fistula as a complication of percutaneous endoscopic gastrostomy. Acta Med Okayama. 2008;62:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 91. | Pitsinis V, Roberts P. Gastrocolic fistula as a complication of percutaneous endoscopic gastrostomy. Eur J Clin Nutr. 2003;57:876-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 92. | Saltzberg DM, Anand K, Juvan P, Joffe I. Colocutaneous fistula: an unusual complication of percutaneous endoscopic gastrostomy. JPEN J Parenter Enteral Nutr. 1987;11:86-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 93. | Smyth GP, McGreal GT, McDermott EW. Delayed presentation of a gastric colocutaneous fistula after percutaneous endoscopic gastrostomy. Nutrition. 2003;19:905-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 94. | Taheri MR, Singh H, Duerksen DR. Peritonitis after gastrostomy tube replacement: a case series and review of literature. JPEN J Parenter Enteral Nutr. 2011;35:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 95. | Tong K, Khan Z. Unexplained diarrhea in a patient with a percutaneous endoscopic gastrostomy (PEG) tube. Endoscopy. 2007;39 Suppl 1:E69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 96. | van Gossum A, DesMarez B, Cremer M. A colo-cutaneous-gastric fistula: a silent and unusual complication of percutaneous endoscopic gastrostomy. Endoscopy. 1988;20:161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 97. | Jiménez Varo I, Gros Herguido N, Parejo Campos J, Tatay Domínguez D, Pereira Cunill JL, Serrano Aguayo P, Socas Macías M, García-Luna PP. Fístula gastrocólica como complicación de gastrostomía percutánea de alimentación, a propósito de tres casos y revisión de la literatura [Gastrocolic fistula as a complication of percutaneous feeding gastrostomy, description of three cases and review of the literature]. Nutr Hosp. 2014;29:460-463. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 98. | Yamazaki T, Sakai Y, Hatakeyama K, Hoshiyama Y. Colocutaneous fistula after percutaneous endoscopic gastrostomy in a remnant stomach. Surg Endosc. 1999;13:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |