Published online May 27, 2023. doi: 10.4240/wjgs.v15.i5.859
Peer-review started: December 13, 2022
First decision: March 1, 2023
Revised: March 11, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: May 27, 2023
Processing time: 164 Days and 2.9 Hours
Previously, some studies have proposed that total laparoscopic gastrectomy (TLG) is superior to laparoscopic-assisted gastrectomy (LAG) in terms of safety and feasibility based on the related intraoperative operative parameters and incidence of postoperative complications. However, there are still few studies on the changes in postoperative liver function in patients undergoing LG. The present study compared the postoperative liver function of patients with TLG and LAG, aiming to explore whether there is a difference in the influence of TLG and LAG on the liver function of patients.
To investigate whether there is a difference in the influence of TLG and LAG on the liver function of patients.
The present study collected 80 patients who underwent LG from 2020 to 2021 at the Digestive Center (including the Department of Gastrointestinal Surgery and the Department of General Surgery) of Zhongshan Hospital affiliated with Xiamen University, including 40 patients who underwent TLG and 40 patients who underwent LAG. Alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ-glutamyltransferase (GGLT), total bilirubin (TBIL), direct bilirubin (DBIL) and indirect bilirubin (IBIL), and other liver function-related test indices were compared between the 2 groups before surgery and on the 1st, 3rd, and 5th d after surgery.
The levels of ALT and AST in the 2 groups were significantly increased on the 1st to 2nd postoperative days compared with those before the operation. The levels of ALT and AST in the TLG group were within the normal range, while the levels of ALT and AST in the LAG group were twice as high as those in the TLG group (P < 0.05). The levels of ALT and AST in the 2 groups showed a downward trend at 3-4 d and 5-7 d after the operation and gradually decreased to the normal range (P < 0.05). The GGLT level in the LAG group was higher than that in the TLG group on postoperative days 1-2, the ALP level in the TLG group was higher than that in the LAG group on postoperative days 3-4, and the TBIL, DBIL and IBIL levels in the TLG group were higher than those in the LAG group on postoperative days 5-7 (P < 0.05). No significant difference was observed at other time points (P > 0.05).
Both TLG and LAG can affect liver function, but the effect of LAG is more serious. The influence of both surgical approaches on liver function is transient and reversible. Although TLG is more difficult to perform, it may be a better choice for patients with gastric cancer combined with liver insufficiency.
Core Tip: Previously, some studies have proposed that total laparoscopic gastrectomy (TLG) and laparoscopic-assisted gastrectomy (LAG) in terms of safety and feasibility based on the related intraoperative operative parameters and incidence of postoperative complications. However, there are still few studies on the changes in postoperative liver function in patients undergoing LG. The present study compared the postoperative liver function of patients with TLG and LAG, aiming to explore the influence of liver function after LAG vs TLG.
- Citation: Xiao F, Qiu XF, You CW, Xie FP, Cai YY. Influence of liver function after laparoscopy-assisted vs totally laparoscopic gastrectomy. World J Gastrointest Surg 2023; 15(5): 859-870
- URL: https://www.wjgnet.com/1948-9366/full/v15/i5/859.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i5.859
As a common tumor of the digestive system, gastric cancer (GC) has high morbidity and mortality rates. According to statistics from the International Agency for Research on Cancer (IARC), GC ranked fifth in incidence and fourth in mortality among new cancer patients worldwide in 2020[1].
Surgery is an indispensable part of the comprehensive treatment of GC. Total or distal gastrectomy (DG) with D2 lymphadenectomy is recommended for GC[2]. The commonly used radical gastrectomy for GC includes open gastrectomy (OG) and laparoscopic gastrectomy (LG). Compared with OG, LG is becoming more available in clinical practice, and it can be subdivided into total laparoscopic gastrectomy (TLG) and laparoscopic-assisted gastrectomy (LAG).
Previously, some studies have proposed that TLG is superior to LAG in terms of safety and feasibility based on the related intraoperative operative parameters and incidence of postoperative complications[3]. However, there are still few studies on the changes in postoperative liver function in patients undergoing LG. The present study compared the postoperative liver function of patients with TLG and LAG, aiming to explore whether there is a difference in the influence of TLG and LAG on the liver function of patients.
The present study collected 80 patients who underwent LG from 2020 to 2021 at the Digestive Center (including the Department of Gastrointestinal Surgery and the Department of General Surgery) of Zhongshan Hospital affiliated with Xiamen University, including 40 patients who underwent TLG and 40 patients who underwent LAG.
The inclusion criteria were as follows: Patients were diagnosed with gastric carcinoma for the first time; patients had surgical indications for LG without obvious surgical contraindications; and the postoperative pathology was consistent with gastric carcinoma.
The exclusion criteria included patients with hepatitis B, hepatitis C, fatty liver, cirrhosis, and other related basic diseases; patients with liver disease who underwent liver surgery; and patients with gallbladder and biliary tract diseases who underwent biliary system surgery[4].
After anesthesia, a conventional disinfection cloth was applied, and a trocar was placed in the 1 cm transverse incision below the umbilical region to establish pneumoperitoneum (12-15 mmHg). Laparoscopy was performed, and a trocar was placed in the left and right upper abdomen under direct vision to explore the entire abdominal cavity and determine the surgical method. The left liver was suspended with a fine line, and to release the greater omentum, part of the intestine and mesangium, the adhesion of the abdominal wall was observed. Surgical site dissociation and D2 lymph node dissection were performed with an ultrasonic scalpel and noninvasive forceps. A 60 mm cutting closure device was used in surgery.
TLG: The digestive tract was reconstructed in the lumen. The specimen was removed with a small incision of 4 cm in the umbilical section (Figure 1A and B).
ALG: Another 7 cm longitudinal incision was made in the middle of the lower abdomen of the xiphoid process. The left liver was pulled externally with an S-type retractor to expose the field of vision. Digestive tract reconstruction was completed under direct vision (Figure 1C).
The levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ-glutamyltransferase (GGLT), total bilirubin (TBIL), direct bilirubin (DBIL) and indirect bilirubin (IBIL) in the 2 groups were recorded before the operation, 1-2 d after the operation, 3-4 d after the operation, and 5-7 d after the operation. The normal range of the above test indices is as follows: ALT, 9-50 U/L; AST, 15-40 U/L; ALP, 45-125 U/L; GGLT, 10-60 U/L; TBIL, 5-21 µmol/L; DBIL, 0-4 µmol/L; and IBIL, 0-17 µmol/L.
SPSS 26.0 was used for statistical analysis to compare whether the liver function-related indicators of the two groups before and after surgery were significantly different. Continuous data are expressed as mean ± SD and were analyzed by the independent t test. Categorical data are expressed as percentages and were analyzed by the chi-square test. A P value < 0.05 was considered statistically significant.
Among the 40 patients who underwent TLG, there were 27 males and 13 females; 13 patients underwent total gastrectomy (TG), and 27 underwent DG, with an age of 64.63 year ± 8.40 year and a body mass index (BMI) of 22.45 kg/m2 ± 3.90 kg/m2. Among the 40 patients who underwent LAG, there were 26 males and 14 females, 19 patients who underwent TG and 21 patients who underwent DG, with an age of 64.78 year ± 9.50 year and BMI of 22.47 kg/m2 ± 2.89 kg/m2. There were no significant differences in sex, age, BMI or surgical resection extent between the 2 groups (P > 0.05) (Table 1).
| Variable | TLG group (n = 40) | ALG group (n = 40) | t value | P value |
| Age (yr) | 64.63 ± 8.40 | 64.78 ± 9.50 | 0.075 | 0.941Nonsig |
| BMI (kg/m2) | 22.45 ± 3.90 | 22.47 ± 2.89 | 0.020 | 0.984Nonsig |
| M/F (case) | 27/13 | 26/14 | 0.056 | 0.813Nonsig |
| TG/GG (case) | 13/27 | 19/21 | 1.875 | 0.171Nonsig |
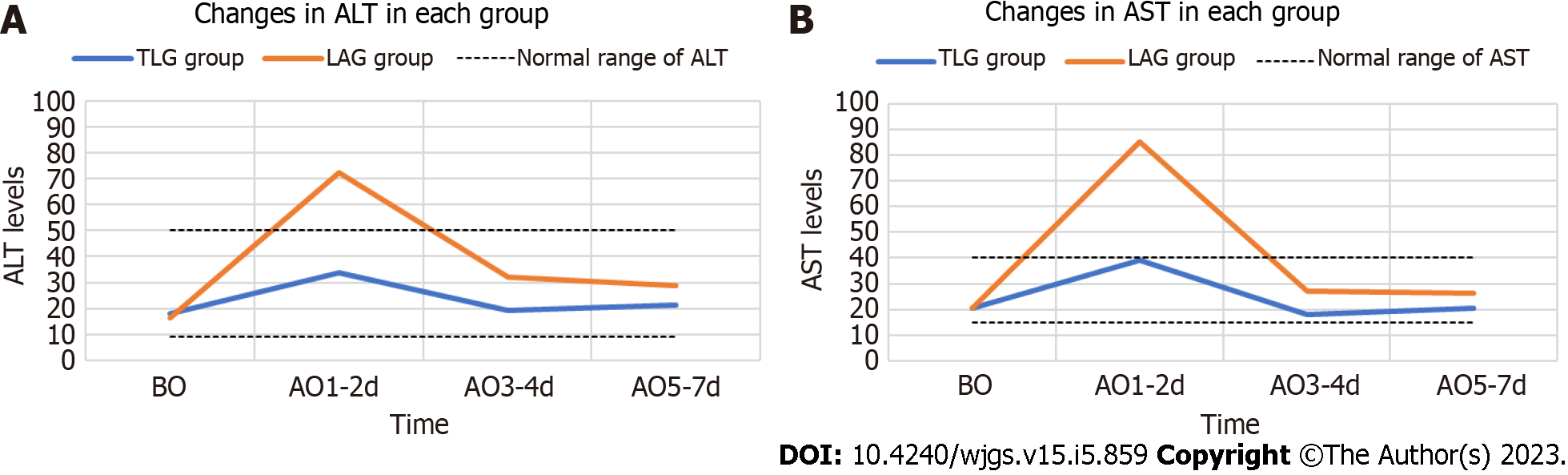
The levels of preoperative ALT and AST were approximately the same in the 2 groups, both within the normal range; moreover, there was no significant difference in preoperative transaminase levels between the 2 groups (P > 0.05) (Table 2, Figure 2).
| Variable | TLG group (n = 40) | ALG group (n = 40) | t value | P value |
| ALT (U/L) | ||||
| BO | 17.98 ± 11.44 | 16.28 ± 8.24 | 0.763 | 0.448Nonsig |
| AO | ||||
| 1-2 d | 33.54 ± 15.28 | 72.49 ± 58.70 | 4.061 | < 0.001Sig |
| 3-4 d | 19.02 ± 8.18 | 32.03 ± 25.27 | 3.099 | 0.003Sig |
| 5-7 d | 21.18 ± 10.13 | 28.90 ± 17.20 | 2.447 | 0.017Sig |
| AST (U/L) | ||||
| BO | 20.47 ± 5.88 | 20.56 ± 5.97 | 0.068 | 0.946Nonsig |
| AO | ||||
| 1-2 d | 39.02 ± 14.67 | 85.27 ± 79.95 | 3.598 | 0.001Sig |
| 3-4 d | 17.99 ± 8.38 | 26.94 ± 19.35 | 2.684 | 0.010Sig |
| 5-7 d | 20.59 ± 8.64 | 26.16 ± 14.52 | 2.084 | 0.040Sig |
There were increases in the levels of ALT and AST from the preoperative value in the 2 groups on the 1st to 2nd d after the operation, and the increase was more significant in the LAG group, that is, approximately twice that of the TLG group. The ALT and AST levels in the TLG group were within the normal range, while the ALT and AST levels in the LAG group were beyond the normal range. There was a difference in transaminase levels between the 2 groups on the 1st to 2nd d after the operation (P < 0.05) (Table 2, Figure 2).
The ALT and AST levels in the 2 groups decreased on days 3-4 after surgery compared with days 1-2 after surgery, among which the levels in the TLG group had decreased to approximately the preoperative level and those in the LAG group had decreased to the normal value. There was a significant difference in the transaminase levels in the 2 groups on days 3-4 after surgery (P < 0.05) (Table 2, Figure 2).
The ALT and AST levels in the 2 groups showed little change on the 5th to 7th d after surgery compared with the 3rd to 4th d after surgery, presenting a general downward trend, both within the normal range, and there was a difference in the transaminase levels between the 2 groups on the 5th to 7th d after the operation (P < 0.05) (Table 2, Figure 2).
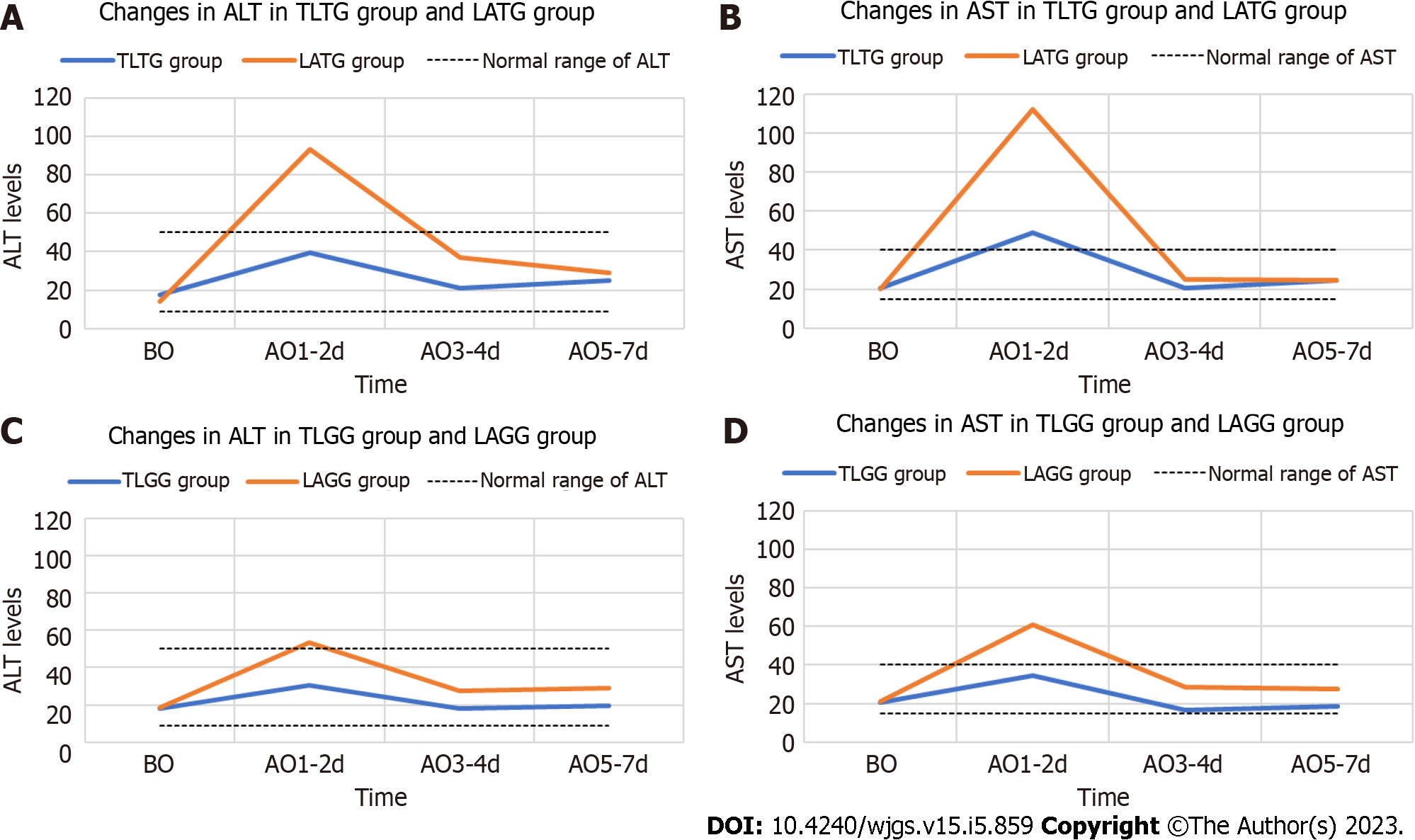
The 2 groups were further stratified according to TG or DG; that is, total laparoscopic TG (TLTG) was compared with laparoscopic-assisted TG (LATG), and total laparoscopic distal gastrectomy (TLGG) was compared with laparoscopic-assisted distal gastrectomy (LAGG). The overall change trend of transaminases between the TLTG group and the LATG, TLGG, and LAGG groups was approximately the same as that between the TLG and LAG groups. The preoperative transaminase levels in the TLTG group, LATG group, TLGG group and LAGG group were all within the normal range. The transaminase levels in the TLTG group, LATG group, TLGG group and LAGG group were increased 1-2 d after the operation, even beyond the normal range, and the increase was more significant in the LATG group and LAGG group. Transaminase levels in the TLTG group, LATG group, TLGG group and LAGG group showed a declining trend on postoperative days 3-4 and 5-7 and gradually decreased to the preoperative level. At the same time, it was found that the transaminase levels in the TLTG group increased significantly compared with those in the TLGG group, and the transaminase levels increased significantly in the LATG group compared with the LAGG group. There were significant differences in transaminase levels between the TLTG group and the LATG group at 1-2 d after surgery and between the TLGG group and the LAGG group at 1-2 d after surgery, 3-4 d after surgery, and 5-7 d after surgery (P < 0.05), while there were no other significant differences (P > 0.05) (Table 3, Figure 3).
| Variable | TLTG group (n = 13) | LATG group (n = 19) | TLGG group (n = 27) | LAGG group (n = 21) | P value |
| ALT (U/L) | |||||
| BO | 17.50 ± 8.85 | 13.94 ± 6.47 | 18.21 ± 12.65 | 18.39 ± 9.21 | 0.1981,Nonsig, 0.9562,Nonsig |
| AO | |||||
| 1-2 d | 39.60 ± 16.03 | 93.41 ± 77.54 | 30.63 ± 14.31 | 53.57 ± 22.72 | 0.0081,Sig, < 0.0012,Sig |
| 3-4 d | 20.93 ± 10.11 | 36.93 ± 31.96 | 18.10 ± 7.10 | 27.60 ± 16.80 | 0.0921,Nonsig, 0.0232,Sig |
| 5-7 d | 24.82 ± 11.65 | 28.99 ± 15.59 | 19.42 ± 9.03 | 28.81 ± 18.91 | 0.4191,Nonsig, 0.0452,Sig |
| AST (U/L) | |||||
| BO | 20.52 ± 5.96 | 20.13 ± 7.21 | 20.44 ± 5.96 | 20.94 ± 4.72 | 0.8741,Nonsig, 0.7542,Nonsig |
| AO | |||||
| 1-2 d | 48.78 ± 13.56 | 112.37 ± 104.91 | 34.33 ± 12.94 | 60.74 ± 35.04 | 0.0171,Sig, 0.0032,Sig |
| 3-4 d | 20.44 ± 10.63 | 24.96 ± 13.41 | 16.81 ± 6.99 | 28.74 ± 23.70 | 0.3181,Nonsig, 0.0362,Sig |
| 5-7 d | 24.43 ± 8.54 | 24.49 ± 9.71 | 18.74 ± 8.20 | 27.66 ± 17.92 | 0.9861,Nonsig, 0.0442,Sig |
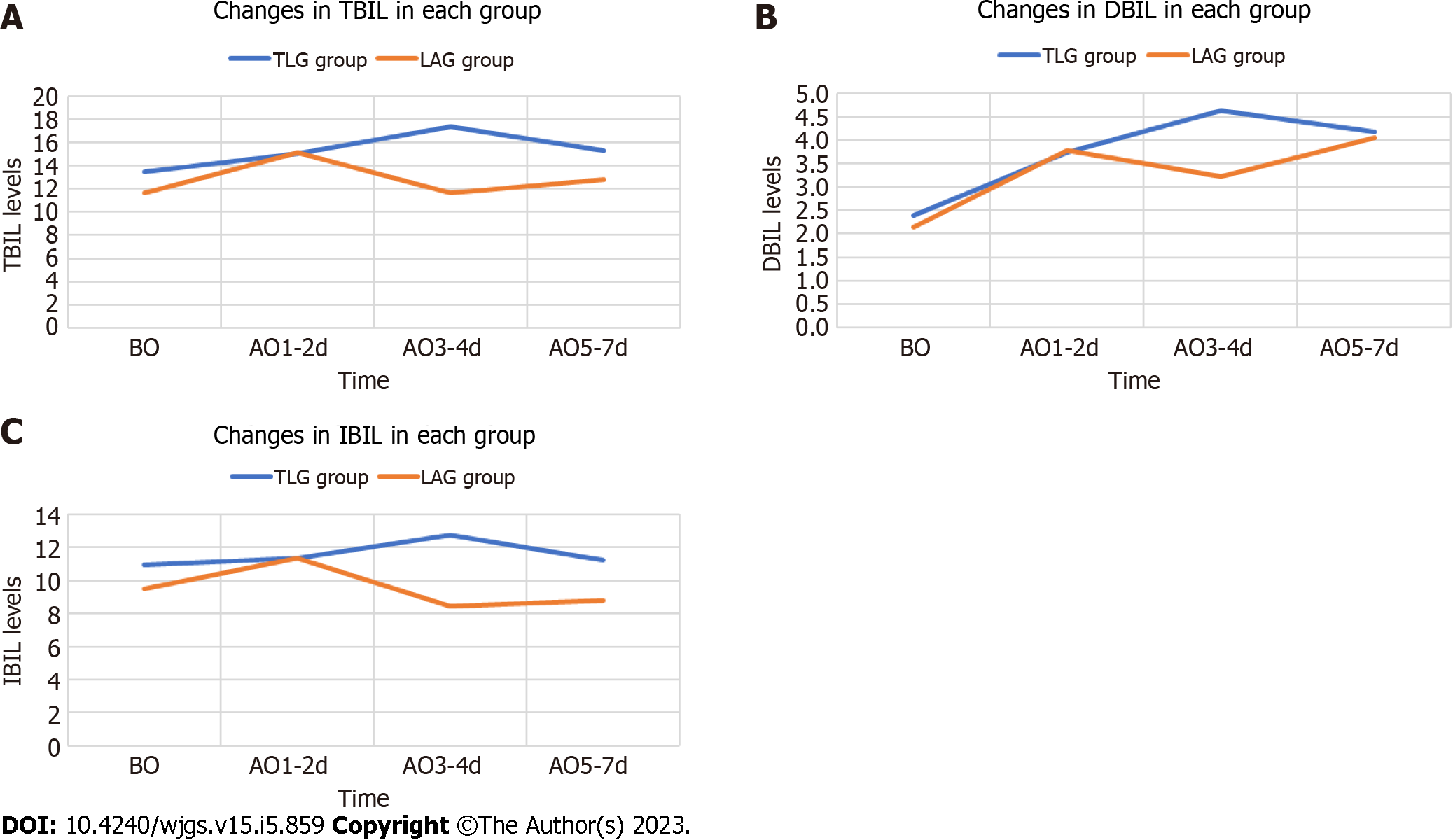
The levels of TBIL, DBIL, and IBIL were roughly the same between the 2 groups before surgery and on day 1-2 after the operation, and all were within the normal range. There was no significant difference in bilirubin levels between the 2 groups before surgery and on day 1-2 after the operation (P > 0.05) (Table 4, Figure 4).
| Variable | TLG group (n = 40) | ALG group (n = 40) | t value | P value |
| TBIL (μmol/L) | ||||
| BO | 13.44 ± 6.57 | 11.62 ± 4.85 | 1.409 | 0.163Nonsig |
| AO | ||||
| 1-2 d | 15.05 ± 7.10 | 15.11 ± 7.27 | 0.042 | 0.967Nonsig |
| 3-4 d | 17.38 ± 8.44 | 11.65 ± 6.72 | 3.358 | 0.001Sig |
| 5-7 d | 15.26 ± 5.91 | 12.82 ± 6.70 | 1.728 | 0.088Nonsig |
| DBIL (μmol/L) | ||||
| BO | 2.40 ± 1.05 | 2.15 ± 0.99 | 1.074 | 0.286Nonsig |
| AO | ||||
| 1-2 d | 3.74 ± 1.73 | 3.79 ± 2.05 | 0.112 | 0.911Nonsig |
| 3-4 d | 4.63 ± 3.32 | 3.22 ± 2.03 | 2.286 | 0.025Sig |
| 5-7 d | 4.17 ± 2.31 | 4.05 ± 4.09 | 0.155 | 0.877Nonsig |
| IBIL (μmol/L) | ||||
| BO | 10.93 ± 5.58 | 9.47 ± 3.93 | 1.355 | 0.179Nonsig |
| AO | ||||
| 1-2 d | 11.36 ± 5.68 | 11.33 ± 5.45 | 0.020 | 0.984Nonsig |
| 3-4 d | 12.75 ± 5.90 | 8.43 ± 5.02 | 3.530 | 0.001Sig |
| 5-7 d | 11.21 ± 4.17 | 8.77 ± 3.54 | 2.819 | 0.006Sig |
The levels of TBIL, DBIL, and IBIL on the 3rd to 4th d after the operation and IBIL on the 5th to 7th d after the operation in both groups were within the normal range, and the TLG group had higher levels than the LAG group. There were significant differences in bilirubin levels on the 3rd to 4th d after the operation and in the IBIL levels on the 5th to 7th d after the operation between the 2 groups (P < 0.05). There were no significant differences in the levels of TBIL and DBIL between the 2 groups on the 5th to 7th d after surgery (P > 0.05) (Table 4, Figure 4).
The 2 groups were further stratified according to TG or DG; that is, TLTG was compared with LATG, and TLGG was compared with LAGG. The overall change trend of bilirubin between the TLTG group and the LATG, TLGG and LAGG groups was roughly the same as that between the TLG and LAG groups. The bilirubin levels at all time points in each group were within the normal range. There were significant differences in bilirubin levels between the TLGG group and LAGG group 3-4 d after surgery, in the indirect bilirubin levels between the TLGG group and LAGG group 5-7 d after surgery, and in the indirect bilirubin levels between the TLTG group and LATG group 3-4 d after surgery (P < 0.05). The bilirubin levels in the TLTG group and TLGG group increased significantly, while there were no other significant differences (P > 0.05) (Table 5).
| Variable | TLTG group (n = 13) | LATG group (n = 19) | TLGG group (n = 27) | LAGG group (n = 21) | P value |
| TBIL (μmol/L) | |||||
| BO | 16.65 ± 9.40 | 11.77 ± 5.85 | 11.90 ± 4.04 | 11.49 ± 3.89 | 0.0801,Nonsig, 0.7262,Nonsig |
| AO | |||||
| 1-2 d | 16.53 ± 7.32 | 15.17 ± 9.32 | 14.33 ± 7.01 | 15.06 ± 4.98 | 0.6621,Nonsig, 0.6872,Nonsig |
| 3-4 d | 19.62 ± 11.28 | 12.67 ± 8.17 | 16.30 ± 6.66 | 10.73 ± 5.11 | 0.0521,Nonsig, 0.0032,Sig |
| 5-7 d | 16.69 ± 6.58 | 13.75 ± 8.33 | 14.57 ± 5.56 | 11.98 ± 4.84 | 0.2951,Nonsig, 0.0972,Nonsig |
| DBIL (μmol/L) | |||||
| BO | 2.83 ± 1.42 | 2.12 ± 1.44 | 2.19 ± 0.76 | 2.18 ± 0.86 | 0.1311,Nonsig, 0.9692,Nonsig |
| AO | |||||
| 1-2 d | 3.97 ± 1.67 | 3.69 ± 2.44 | 3.63 ± 1.77 | 3.87 ± 1.67 | 0.7221,Nonsig, 0.6282,Nonsig |
| 3-4 d | 4.78 ± 2.56 | 3.70 ± 2.46 | 4.56 ± 3.67 | 2.80 ± 1.48 | 0.2371,Nonsig, 0.0442,Sig |
| 5-7 d | 4.65 ± 1.51 | 4.63 ± 5.38 | 3.93 ± 2.60 | 3.53 ± 2.44 | 0.9871,Nonsig, 0.5872,Nonsig |
| IBIL (μmol/L) | |||||
| BO | 13.48 ± 8.09 | 9.65 ± 4.76 | 9.70 ± 3.42 | 9.30 ± 3.09 | 0.1021,Nonsig, 0.6782,Nonsig |
| AO | |||||
| 1-2 d | 12.56 ± 5.83 | 11.48 ± 7.10 | 10.78 ± 5.62 | 11.20 ± 3.54 | 0.4541,Nonsig, 0.7652,Nonsig |
| 3-4 d | 14.83 ± 8.88 | 8.97 ± 6.07 | 11.75 ± 3.57 | 7.94 ± 3.94 | 0.0341,Sig, 0.0012,Sig |
| 5-7 d | 12.38 ± 5.33 | 9.12 ± 4.33 | 10.64 ± 3.46 | 8.45 ± 2.71 | 0.0661,Nonsig, 0.0212,Sig |
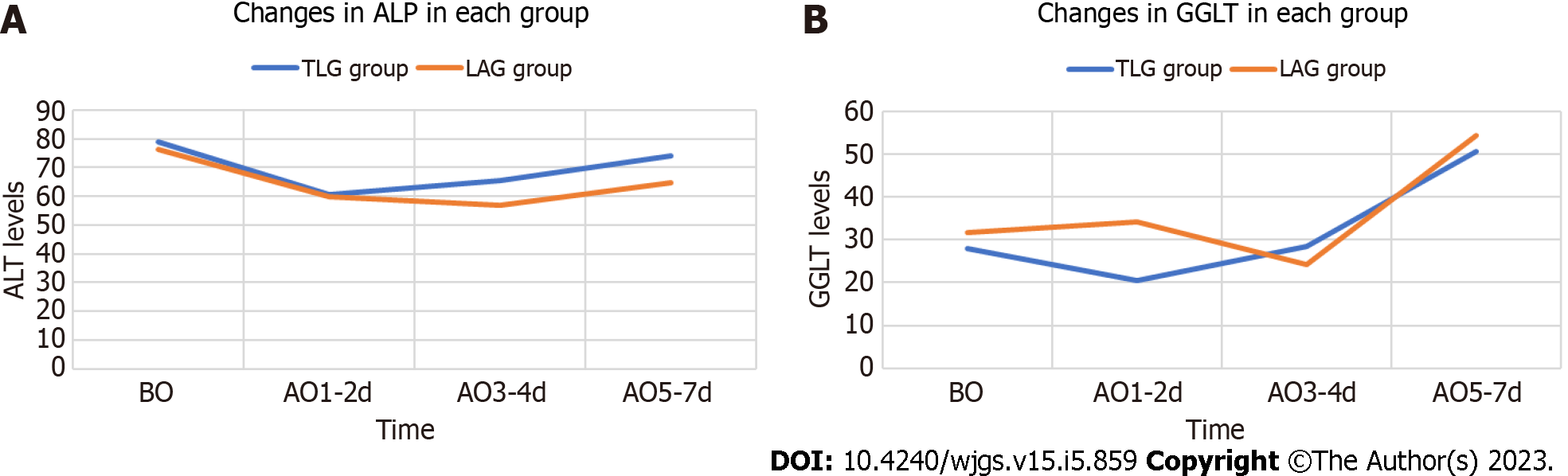
The levels of ALP and GGLT in the 2 groups were approximately the same before surgery and 5-7 d after surgery, both within the normal range, with no significant difference (P > 0.05) (Table 6, Figure 5).
| Variable | TLG group (n = 40) | ALG group (n = 40) | t value | P value |
| ALP (U/L) | ||||
| BO | 78.78 ± 16.73 | 76.10 ± 20.28 | 0.644 | 0.521Nonsig |
| AO | ||||
| 1-2 d | 60.59 ± 14.26 | 59.86 ± 13.99 | 0.231 | 0.818Nonsig |
| 3-4 d | 65.40 ± 15.58 | 57.06 ± 13.76 | 2.539 | 0.013Sig |
| 5-7 d | 73.97 ± 17.62 | 64.77 ± 26.06 | 1.850 | 0.068Nonsig |
| GGLT (U/L) | ||||
| BO | 28.06 ± 32.63 | 31.70 ± 28.05 | 0.536 | 0.593Nonsig |
| AO | ||||
| 1-2 d | 20.46 ± 25.74 | 34.07 ± 26.10 | 2.347 | 0.021Sig |
| 3-4 d | 28.47 ± 29.22 | 24.11 ± 16.19 | 0.825 | 0.413Nonsig |
| 5-7 d | 50.66 ± 37.38 | 54.33 ± 39.28 | 0.428 | 0.670Nonsig |
The ALP level on postoperative days 3-4 and the GGLT level on postoperative days 1-2 in the 2 groups were within the normal range. ALP in the TLG group was higher than that in the LAG group, and GGLT was higher than that in the TLG group, with significant differences (P < 0.05). There were no differences in ALP levels on the 1st to 2nd postoperative days or in the GGLT levels on the 3rd to 4th postoperative days between the 2 groups (P > 0.05) (Table 6, Figure 5).
The 2 groups were further stratified according to TG or DG; that is, TLTG was compared with LATG, and TLGG was compared with LAGG. The overall change trend of ALP and GGLT between the TLTG group and LATG group and between the TLGG group and LAGG group was roughly the same as that between the TLG group and LAG group. The ALP and GGLT levels at each time point in each group were within the normal range. There were significant differences in GGLT levels 1-2 d after the operation and in the ALP levels 3-4 d after the operation between the TLTG group and the LATG group (P < 0.05). The former levels were higher in the TLTG group, while the latter levels were higher in the LATG group, and there were no significant differences in the other groups (P > 0.05) (Table 7).
| Variable | TLTG group (n = 13) | LATG group (n = 19) | TLGG group (n = 27) | LAGG group (n = 21) | P value |
| ALP (U/L) | |||||
| BO | 83.63 ± 13.24 | 76.36 ± 25.15 | 76.44 ± 17.92 | 75.87 ± 15.27 | 0.3481,Nonsig, 0.9072,Nonsig |
| AO | |||||
| 1-2 d | 59.95 ± 9.59 | 57.47 ± 15.06 | 60.89 ± 16.19 | 62.01 ± 12.93 | 0.6041,Nonsig, 0.7962,Nonsig |
| 3-4 d | 68.39 ± 15.53 | 56.44 ± 15.68 | 63.96 ± 15.70 | 57.61 ± 12.12 | 0.0421,Sig, 0.1332,Nonsig |
| 5-7 d | 83.56 ± 19.69 | 66.68 ± 31.49 | 69.35 ± 14.78 | 63.04 ± 20.63 | 0.0971,Nonsig, 0.2232,Nonsig |
| GGLT (U/L) | |||||
| BO | 27.42 ± 30.31 | 33.03 ± 32.33 | 28.36 ± 34.25 | 30.50 ± 24.29 | 0.6251,Nonsig, 0.8092,Nonsig |
| AO | |||||
| 1-2 d | 19.15 ± 19.42 | 37.11 ± 28.46 | 21.09 ± 28.61 | 31.32 ± 24.15 | 0.0421,Sig, 0.1962,Nonsig |
| 3-4 d | 34.22 ± 36.82 | 26.34 ± 19.69 | 25.70 ± 25.12 | 22.10 ± 12.39 | 0.4901,Nonsig, 0.5002,Nonsig |
| 5-7 d | 59.74 ± 34.97 | 56.77 ± 44.02 | 46.29 ± 38.34 | 52.13 ± 35.42 | 0.8401,Nonsig, 0.5922,Nonsig |
Currently, studies have pointed out that LG has survival benefits similar to those of OG[5,6]. With the development of laparoscopic technology and the update and progress of surgical instruments, LG is becoming increasingly common in the clinic. However, TLG and LAG are still not clearly preferred in the clinic. Although relevant studies[7-11] have reported that TLG has advantages in many aspects, such as intraoperative dissection and postoperative recovery, the small incision in LAG also limits the intraoperative field of vision and operating space. However, TLG has higher requirements for surgical technique and operation coordination.
Comparative studies on the short-term therapeutic effect and long-term quality of life resulting from the 2 surgical methods have been completed, but there is still a lack of research on the postoperative liver function of patients receiving either of the 2 surgical methods. In this study, we found that in terms of transaminases, ALT and AST levels in the TLG group and the LAG group increased significantly after surgery; peaked on the 1st to 2nd d after surgery; gradually decreased, returning to the normal range on approximately the 3rd to 4th d after surgery; and then returned to the preoperative level on the 5th to 7th d after surgery. Among these values, the levels of ALT and AST in patients with LAG were significantly increased and beyond the normal range, and even the ALT and AST levels in patients with ALG were more than twice as high as those in patients with TLG on the 1st to 2nd d after surgery. Previous studies[12-15] have pointed out that CO2 pneumoperitoneum reduces portal vein blood flow through intra-abdominal pressure and hypercapnia, thus causing liver function injury. In addition, both the TLG group and the LAG group underwent the operation of exposing the field of vision with liver traction by a fine line, and both groups underwent the operation of blocking the possible left vagal hepatic artery, which was the reason why the ALT and AST levels in the TLG group and the LAG group were higher than those before surgery. However, in this study, under the same CO2 pneumoperitoneum conditions, the TLG group needed to complete all surgical steps under endoscopy, while the LAG group could complete digestive tract reconstruction under open conditions; that is, the effect of CO2 pneumoperitoneum in the TLG group lasted longer than that in the LAG group. However, the ALT and AST levels in the LAG group were higher than those in the TLG group; in other words, the postoperative liver function injury in the LAG group was higher than that in the TLG group, so the effect of CO2 pneumoperitoneum was not considered the reason for the difference between the 2 groups. At the same baseline in this study, the difference between the TLG group and the LAG group was only due to differences in surgical methods. In the LAG group, a 7 cm longitudinal incision was made in the middle of the lower xiphoid, and the left liver was continuously pulled externally with the help of an S-type retractor to expose the field of vision during digestive tract reconstruction. Therefore, we considered that the operation of continuous squeezing and pulling of the liver with an S-type retractor was the main factor leading to the higher postoperative ALT and AST levels in the LAG group than in the TLG group. In addition, the 2 groups were further stratified according to TG or DG; that is, TLTG was compared with LATG, and TLGG was compared with LAGG. We found that the ALT and AST levels in the TLTG group were higher than those in the TLGG group, and the ALT and AST levels in the LATG group were higher than those in the LAGG group. Compared with DG, TG requires a more fully exposed field of vision for reconstruction of the digestive tract; that is, there is a higher degree of continuous squeezing and pulling of the left liver, which also confirms that continuous squeezing and pulling of the liver with an S-type retractor is the main factor leading to the difference in ALT and AST levels after surgery. Therefore, we considered that the higher postoperative transaminase level in the LAG group compared with the TLG group was caused by the different surgical methods; that is, the damage to liver function in the LAG group was greater than that in the TLG group. However, the levels of ALT and AST in the 2 groups recovered to the normal range approximately 3-4 d after surgery and returned to the preoperative level 5-7 d after surgery, indicating that the liver function injury was transient and reversible.
In this study, TBIL, DBIL, IBIL, ALP and GGLT levels at each time point in the 2 groups were all within the normal range. Between the 2 surgical methods, only the bilirubin levels on postoperative days 3-4, the indirect bilirubin levels on postoperative days 5-7, the ALP levels on postoperative days 3-4, and the GGLT levels on postoperative days 1-2 were significantly different, while the changes in TBIL, DBIL, IBIL, ALP, GGLT, and other indicators showed no obvious regularity. Among them, the GGLT level in the TLG group was higher than that in the LAG group on the 1st to 2nd d after the operation, which was similar to the changes in postoperative transaminase in the 2 groups. Although the ALP level in the LAG group was higher than that in the TLG group 3-4 d after surgery, the postoperative ALP level in the 2 groups remained unchanged or decreased compared with the preoperative ALP level, which was similar to the results of Singal et al[16] in comparing liver function after laparoscopic cholecystectomy and open cholecystectomy. In addition, the levels of bilirubin in the TLG group on days 3-4 after surgery and the levels of indirect bilirubin in the TLG group on days 5-7 after surgery were higher than those in the LAG group. Relevant studies by Zhang et al[3] have pointed out that TLG patients exhaust for the first time earlier than LAG patients; therefore, we believed that TLG enables exhaust earlier than LAG does and restores intestinal function faster, thus opening the enterohepatic circulation, and bilirubin circulates into the blood through the portal vein. As a result, the postoperative bilirubin level in the TLG group was higher than that in the LAG group. Certainly, further clinical studies are required to confirm these findings.
The limitation of this retrospective study lies in the fact that the digestive center of Zhongshan Hospital Affiliated to Xiamen University included gastrointestinal surgery and general surgery. Therefore, the 40 patients with TLG and 40 patients with LAG in this retrospective study may be from different surgical treatment groups, which means that there are deviations in the surgical process caused by the difference in operational level of the operators. In addition, different surgical groups may also lead to certain differences in the diagnosis and treatment protocols adopted after surgery. For example, patients undergoing TLG resume enteral nutrition path earlier, enterohepatic circulation is opened, bilirubin circulates into the blood through the portal vein, and postoperative transient increase of bilirubin. This may also be the reason why the level of bilirubin on days 3-4 after surgery and indirect bilirubin on days 5-7 after surgery are both higher in the patients undergoing TLG.
In conclusion, both TLG and LAG can affect liver function, and this effect is transient and reversible. The effect of LAG on liver function is more serious. TLG is not only superior to LAG in terms of short-term efficacy and long-term quality of life but also in terms of liver function protection. Although TLG is more difficult to perform, it may be a better choice in radical gastrectomy.
Previously, some studies have proposed that totally laparoscopic gastrectomy (TLG) is superior to laparoscopy-assisted gastrectomy (LAG) in terms of safety and feasibility based on the related intraoperative operative parameters and incidence of postoperative complications. However, there are still few studies on the changes in postoperative liver function in patients undergoing LG. The present study compared the postoperative liver function of patients with TLG and LAG, aiming to explore whether there is a difference in the influence of TLG and LAG on the liver function of patients.
To compare the postoperative liver function of patients with TLG and LAG.
To investigate whether there is a difference in the influence of TLG and LAG on the liver function of patients.
The present study collected 80 patients who underwent LG from 2020 to 2021 at the Digestive Center (including the Department of Gastrointestinal Surgery and the Department of General Surgery) of Zhongshan Hospital affiliated with Xiamen University, including 40 patients who underwent TLG and 40 patients who underwent LAG. Alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), γ-glutamyltransferase (GGLT), total bilirubin (TBIL), direct bilirubin (DBIL), and indirect bilirubin (IBIL), and other liver function-related test indices were compared between the 2 groups before surgery and on the 1st, 3rd, and 5th d after surgery.
The levels of ALT and AST in the 2 groups were significantly increased on the 1st to 2nd postoperative days compared with those before the operation. The levels of ALT and AST in the TLG group were within the normal range, while the levels of ALT and AST in the LAG group were twice as high as those in the TLG group (P < 0.05). The levels of ALT and AST in the 2 groups showed a downward trend at 3-4 d and 5-7 d after the operation and gradually decreased to the normal range (P < 0.05). The GGLT level in the LAG group was higher than that in the TLG group on postoperative days 1-2, the ALP level in the TLG group was higher than that in the LAG group on postoperative days 3-4, and the TBIL, DBIL and IBIL levels in the TLG group were higher than those in the LAG group on postoperative days 5-7 (P < 0.05). No significant difference was observed at other time points (P > 0.05).
Both TLG and LAG can affect liver function, but the effect of LAG is more serious. The influence of both surgical approaches on liver function is transient and reversible. Although TLG is more difficult to perform, it may be a better choice for patients with gastric cancer combined with liver insufficiency.
In conclusion, both TLG and LAG can affect liver function, and this effect is transient and reversible. The effect of LAG on liver function is more serious. TLG is not only superior to LAG in terms of short-term efficacy and long-term quality of life but also in terms of liver function protection. Although TLG is more difficult to perform, it may be a better choice in radical gastrectomy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aurello P, Italy; Maslennikov R, Russia S-Editor: Chen YL L-Editor: A P-Editor: Zhao S
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 63990] [Article Influence: 15997.5] [Reference Citation Analysis (174)] |
| 2. | Caruso S, Scatizzi M. Laparoscopic gastrectomy for gastric cancer: has the time come for considered it a standard procedure? Surg Oncol. 2022;40:101699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Zhang YX, Wu YJ, Lu GW, Xia MM. Systematic review and meta-analysis of totally laparoscopic vs laparoscopic assisted distal gastrectomy for gastric cancer. World J Surg Oncol. 2015;13:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Jeong GA, Cho GS, Shin EJ, Lee MS, Kim HC, Song OP. Liver function alterations after laparoscopy-assisted gastrectomy for gastric cancer and its clinical significance. World J Gastroenterol. 2011;17:372-378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, Kim HI, Kim HH, Ryu SW, Hur H, Kim MC, Kong SH, Cho GS, Kim JJ, Park DJ, Ryu KW, Kim YW, Kim JW, Lee JH, Han SU; Korean Laparoendoscopic Gastrointestinal Surgery Study Group. Long-Term Outcomes of Laparoscopic Distal Gastrectomy for Locally Advanced Gastric Cancer: The KLASS-02-RCT Randomized Clinical Trial. J Clin Oncol. 2020;38:3304-3313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (1)] |
| 6. | Yu J, Huang C, Sun Y, Su X, Cao H, Hu J, Wang K, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Hu Y, Liu H, Zheng C, Li P, Xie J, Liu F, Li Z, Zhao G, Yang K, Liu C, Li H, Chen P, Ji J, Li G; Chinese Laparoscopic Gastrointestinal Surgery Study (CLASS) Group. Effect of Laparoscopic vs Open Distal Gastrectomy on 3-Year Disease-Free Survival in Patients With Locally Advanced Gastric Cancer: The CLASS-01 Randomized Clinical Trial. JAMA. 2019;321:1983-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 522] [Article Influence: 87.0] [Reference Citation Analysis (1)] |
| 7. | Choi CI, Lee CM, Park JH, Jee YS, Lee HH, Jeong O, Park S. Recent Status of Laparoscopic Distal Gastrectomy in Korea: A Multicenter Retrospective Cohort Study (Pre-study Survey of KLASS-07 Trial). Front Oncol. 2019;9:982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Ikeda O, Sakaguchi Y, Aoki Y, Harimoto N, Taomoto J, Masuda T, Ohga T, Adachi E, Toh Y, Okamura T, Baba H. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc. 2009;23:2374-2379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Kim BS, Yook JH, Choi YB, Kim KC, Kim MG, Kim TH, Kawada H, Kim BS. Comparison of early outcomes of intracorporeal and extracorporeal gastroduodenostomy after laparoscopic distal gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A. 2011;21:387-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Kim MG, Kawada H, Kim BS, Kim TH, Kim KC, Yook JH. A totally laparoscopic distal gastrectomy with gastroduodenostomy (TLDG) for improvement of the early surgical outcomes in high BMI patients. Surg Endosc. 2011;25:1076-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Woo J, Lee JH, Shim KN, Jung HK, Lee HM, Lee HK. Does the Difference of Invasiveness between Totally Laparoscopic Distal Gastrectomy and Laparoscopy-Assisted Distal Gastrectomy Lead to a Difference in Early Surgical Outcomes? A Prospective Randomized Trial. Ann Surg Oncol. 2015;22:1836-1843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Giraudo G, Brachet Contul R, Caccetta M, Morino M. Gasless laparoscopy could avoid alterations in hepatic function. Surg Endosc. 2001;15:741-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Jakimowicz J, Stultiëns G, Smulders F. Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc. 1998;12:129-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 202] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 14. | Tan M, Xu FF, Peng JS, Li DM, Chen LH, Lv BJ, Zhao ZX, Huang C, Zheng CX. Changes in the level of serum liver enzymes after laparoscopic surgery. World J Gastroenterol. 2003;9:364-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Tsugawa K, Hashizume M, Migou S, Tanoue K, Kishihara F, Kawanaka H, Sugimachi K. The effect of carbon dioxide pneumoperitoneum on the portal hemodynamics in a portal-hypertensive rat model. Surg Laparosc Endosc Percutan Tech. 1999;9:338-347. [PubMed] |
| 16. | Singal R, Singal RP, Sandhu K, Singh B, Bhatia G, Khatri A, Sharma BP. Evaluation and comparison of postoperative levels of serum bilirubin, serum transaminases and alkaline phosphatase in laparoscopic cholecystectomy vs open cholecystectomy. J Gastrointest Oncol. 2015;6:479-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |