Published online May 27, 2023. doi: 10.4240/wjgs.v15.i5.847
Peer-review started: December 3, 2022
First decision: December 26, 2022
Revised: January 12, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: May 27, 2023
Processing time: 173 Days and 18.4 Hours
Hydatid liver disease remains an important issue in endemic areas, which may require immediate surgery. Although laparoscopic surgery is on the rise, the presence of certain complications may require conversion to the open approach.
To compare the results of laparoscopic treatment and the open approach in the context of a 12-year single institution experience, and to perform a further comparison between results from the current study and those from a previous study.
Between January 2009 and December 2020, 247 patients underwent surgery for hydatic disease of the liver in our department. Of the 247 patients, 70 underwent laparoscopic treatment. A retrospective analysis between the two groups was performed, as well as a comparison between current and previous laparoscopic experience (1999-2008).
There were statistically significant differences between the laparoscopic and open approaches regarding the cyst dimension, location, and presence of cystobiliary fistula. There were no intraoperative complications in the laparoscopic group. The cutoff value for the cyst size regarding the presence of cystobiliary fistula was 6.85 cm (P = 0.001).
Laparoscopic surgery still plays an important role in the treatment of hydatid disease of the liver, with an increase in its usage over the course of years that has shown benefits regarding the postoperative recovery with a decreased rate of intraoperative complications. Although experi
Core Tip: Laparoscopic surgery for the treatment of liver hydatid disease has grown significantly in the last decade, due to increased accessibility and better training. Although, some limits were reported on previously regarding the cyst size, location, and presence of complications such as cystobiliary fistulas. This article discusses our experience over 12 years in the surgical treatment of hydatid liver disease, highlighting key aspects of surgical timing as well as differences between the open approach and laparoscopic approach in terms of case selection, comorbidities, and postoperative management.
- Citation: Zaharie F, Valean D, Zaharie R, Popa C, Mois E, Schlanger D, Fetti A, Zdrehus C, Ciocan A, Al-Hajjar N. Surgical management of hydatid cyst disease of the liver: An improvement from our previous experience? World J Gastrointest Surg 2023; 15(5): 847-858
- URL: https://www.wjgnet.com/1948-9366/full/v15/i5/847.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i5.847
Hydatid disease is a parasitic disease that is widespread across the world, with endemic areas in Central Asia, the Mediterranean Region, Northern and Central Africa, and South America, especially in rural areas where animals are raised. Echinococcus granulosis and Echinococcus multilocularis are the primary agents of the disease, with the liver being the most affected organ, followed by the lungs and spleen[1]. Despite being considered a benign disease, it can have a considerable socioeconomic impact, with important comorbidities and a mortality rate of 1%-4%[2]. Although in some cases, spontaneous healing can occur through the parasite’s death and calcification, treatment remains mandatory, especially in symptomatic and/or viable cysts. Anthelmintic treatment is mandatory; however, it should not be used as a standalone treatment, as most published studies suggest that radical surgery is a better option than conservative treatment[3].
Despite surgery remaining the treatment of choice, there has been an increased interest in non-surgical techniques in the current literature. Since open procedures present a higher risk of morbidity, the laparoscopic approach has grown in popularity; although, the benefits that laparoscopy provides and the risk of recurrence remain debatable[4,5]. Even though robotic surgery is on the rise, the importance of laparoscopy should not be understated since the former technique is less accessible in underdeveloped centers, due to its high cost. In addition, recent developments in the laparoscopic technique as well as its cost-effectiveness have made the procedure much more accessible for less experienced as well as veteran surgeons.
This retrospective study evaluated results from the laparoscopic treatment of hydatic disease of the liver compared to those from the open approach in the context of a 12-year single institution experience and in terms of the morphological characteristics of the cysts and the perioperative parameters. Furthermore, this study compared the results with previous 10-year experience from 1999 to 2008 regarding laparoscopic treatment, in terms of case selection, duration, case volume, postoperative complications, and recurrence rate. The objective of the study was to highlight the possible selection criteria regarding the surgical treatment of choice.
Between January 2009 and December 2020, 258 patients underwent surgery for hydatic disease of the liver in our surgical department. Patients were reviewed retrospectively. The primary inclusion criteria were patients who underwent surgery for hydatid disease of the liver, were over 18 years of age, and provided written informed consent. The exclusion criteria were patients with incomplete records, not providing written informed consent, who had experienced spontaneous rupture, who underwent conversion to open surgery, or who underwent percutaneous treatment. There were no exclusion criteria regarding cyst location, cyst size, or number of cysts. Data from all eligible patients were collected from an electronic database, and the earlier cases were collected from the medical archives of the hospital.
All patients received antiparasitic medical treatment 14 d prior to surgery. All patients were evaluated via ultrasound or contrast computed tomography (CT), which was used to classify the cysts as well (according to Gharbi classification). Magnetic resonance cholangiopancreatography (MRCP) was used preoperatively for patients with dilated biliary ducts, elevated liver enzymes, or hydatid elements in the bile ducts associated with jaundice. Preoperatively, all patients underwent treatment with albendazole (10 mg/kg), 7 to 14 d before surgery. Treatment was continued for 30 d postoperatively. Of the 268 patients, 77 underwent laparoscopic treatment, among which 7 required conversions to open surgery. Eleven cases presented with spontaneous rupture of the cyst and ten had incomplete data, and thus were excluded. Therefore, two groups were created: The first group (group A) comprised 70 patients who underwent laparoscopic treatment, and the second group (group B) comprised 170 patients who underwent open surgery. In both groups, there were 73 patients with cystobiliary communication. Associated cholecystectomy was performed in 62 of the cases. The groups were analyzed based on their demographic, preoperative and postoperative parameters, and cyst parameters, as well as follow-up and morbidity.
Recurrence in hydatid disease is considered when new cysts are discovered after therapy. This can mean reappearance and growth at the previously treated site, or appearance of other cysts at another site due to spillage. Our study defined recurrence as visible lesions via ultrasound or CT, with or without elevated eosinophils and liver enzymes over the follow-up duration. Follow-up was routinely performed every 6 mo, for a minimum duration of 18 mo. A minimum of three/four controls were performed for each patient. The study was approved by the Ethics Committee of the Regional Institute of Gastroenterology and Hepatology “O. Fodor”, Cluj-Napoca.
The main aspects regarding the possible surgical approach are in terms of selecting whether a lagrot (partial) pericystectomy or a total pericystectomy is performed. Partial pericystectomy involves resection of the externalized pericyst at the border of the liver parenchyma, followed by aspiration of the contents with the residual cavity staying in place, thus requiring extra drainage or closure of the residual cavity; whereas, total pericystectomy involves removing the cyst in its entirety with the adjacent parenchyma and without spilling its contents.
There were no significant changes in the laparoscopic surgical technique from our previous study. We inserted a 10-mm supraumbilical port, through which a 30-degree telescope was inserted. The abdominal cavity was insufflated with carbon dioxide to create adequate working space. Afterwards, the remainder of the telescopes were inserted in a camera-guided manner, as follows: A 10-mm port was inserted in the epigastric area as near as possible to the cyst, to be used as a working channel, and then two 5-mm ports were inserted based on the cyst location. Furthermore, any adhesions between the cysts and the nearby organs were cauterized. After exposing and isolating the hydatid lesions from the rest of the peritoneal cavity (through wicks soaked in an inactivation solution - metronidazole or hypertonic saline solution), the cysts were punctured with the vacuum cannula and aspiration of the cystic cavity was performed. If there was certainty of the absence of any cystobiliary communication, inactivation solution could be injected in the cystic cavity. Another vacuum cannula was inserted through another port, which was permanently maintained near the puncture to prevent hydatid spillage.
After the entire content was aspirated, cystostomy was performed and the content was extracted in an endo-bag. After the parasite was inactivated and then removed, the surgical treatment for the residual cavity was applied. In the case of a cystobiliary fistula, application of metal clips or an “X” suture was performed. One or two drains were placed (especially in the lagrot pericystectomy). Preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed in cases of intrabiliary rupture to minimize the risk of cholangitis. Postoperatively, ERCP was performed to decrease the pressure in the biliary tract, if necessary.
Laparoscopic total pericystectomy was performed without puncturing the cyst wall during the procedure (“closed” technique), using ligation devices for resection through the healthy adjacent parenchyma. Hemostasis was performed and afterwards, a close inspection for cystobiliary communication or biliary leaks was performed. The specimen was then extracted into an endo-bag through the epigastric port. If required, the incision for the epigastric port could be enlarged. Injection of methylene blue to evaluate the biliary involvement of large cysts was not routinely performed; however, in cases where the existence of a cystobiliary communication was certain but could not be adequately identified, this method was used.
For the open surgical approach, we used a supraumbilical midline incision or a subcostal incision. Any adhesion between the cysts and the neighboring organs was lysed. To prevent any hydatid spillage, the peritoneal cavity was isolated with wicks soaked in 20% hypertonic saline solution before any maneuver on the hydatid cyst was performed. Parasite inactivation was performed by injecting 20% hypertonic saline solution. After 5 min, the hydatid content was aspirated. Starting from the puncture site, cystotomy was performed, with extraction of the germinal membrane and daughter vesicles. Afterwards, surgical treatment for the residual cavity was applied. Open total pericystectomy was performed in a similar manner as the laparoscopic technique, with a much easier extraction of the specimen, via the laparotomy incision.
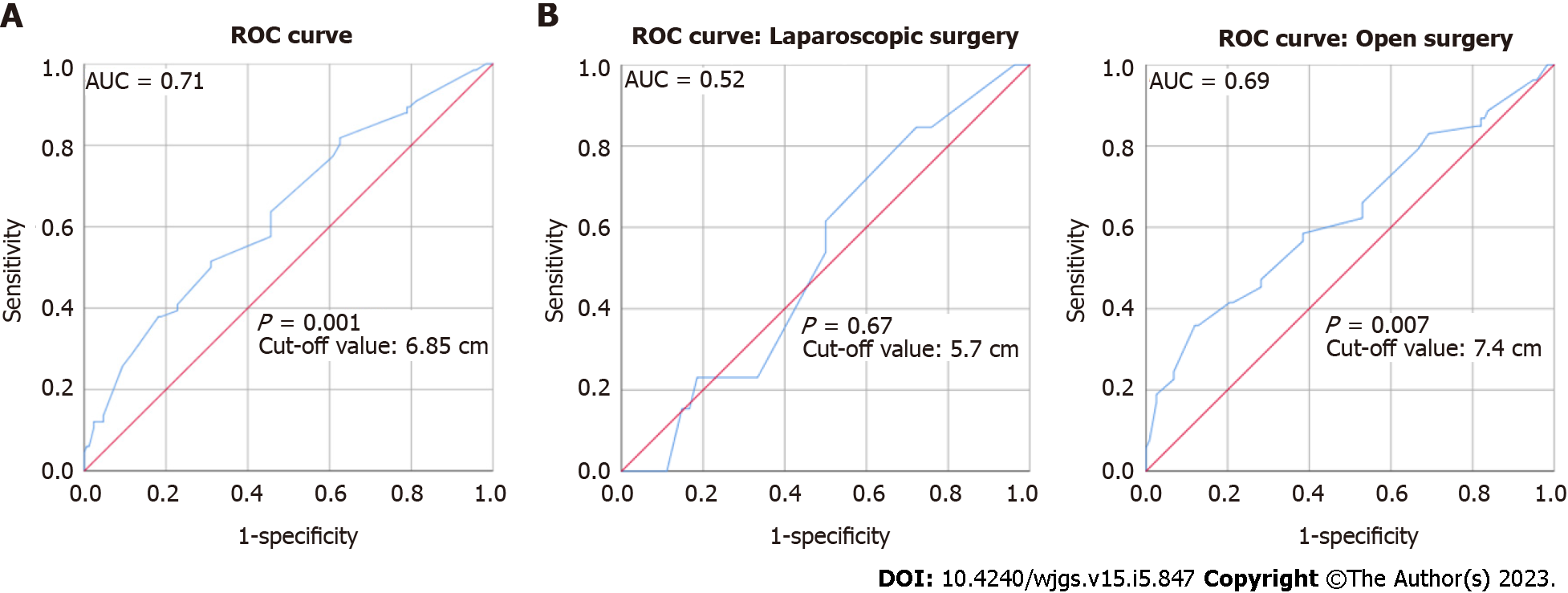
All the statistical tests were made using the IBM SPSS v26.0 program (IBM Corp., Armonk, NY, United States). Comparisons between the two groups were performed. Categorical values and qualitative variables were analyzed using Pearson’s chi-squared test. When accounting for quantitative variables such as surgery duration, estimated blood loss, and cyst diameter, normality tests were used to verify the data distribution (using Kolmogorov-Smirnov and Shapiro-Wilk tests). Thus, non-normal distributed data were evaluated by comparing median values using Mann-Whitney U tests, and normal distributed data were evaluated by comparing mean values using the t-test for independent variables (mean age). To determine the value of the cyst diameter from which there is an elevated risk of cystobiliary fistula, a receiver operating characteristic curve (ROC) curve was generated to determine the cutoff point, as was the area under the curve (AUC), with an AUC value of over 0.7 being an acceptable estimator. The value for statistical significance was P < 0.05. To minimize the potential sources of bias, additional related parameters were compared to verify the potential differences between the two groups as well as to control the potential confounding variables.
The demographic data regarding the age, sex, environment, symptoms at presentation, and comorbidities are detailed in Table 1. Both groups were relatively similar in terms of age, sex, frequency of symptoms, comorbidities, and preoperative risk profile [American Society of Anesthesiologists (ASA) classification]. The mean age of the laparoscopic group was lower than that of the open approach group (39.87 years vs 44.36 years, P = 0.03). Although the relative frequency of the obese patients was higher in the open group than in the laparoscopic group, there were no statistically significant differences between the groups (8.57% vs 11.9%, P = 0.43). The most frequently reported symptom was pain in the right-upper quadrant (71.42% vs 70.1%). When addressing the median alanine transaminase and aspartate transaminase values, no statistically significant differences were recorded. In total, 6 of 70 patients (8.57%) presented with hydatid elements in the common bile duct compared to 19 patients in the open group (11.17%); although, the difference was not statistically significant (P = 0.34).
| Parameter | Laparoscopic, n = 70 (%) | Open approach, n = 170 (%) | P value | |
| Age | Mean age | 39.87 ± 14.4 | 44.36 ± 15.99 | 0.03 |
| Sex | Male | 29 (41.42) | 80 (47.28) | 0.4 |
| Female | 41 (58.58) | 90 (52.72) | ||
| Environment | Urban | 29 (41.42) | 65 (38.04) | 0.61 |
| Rural | 41 (58.58) | 105 (61.96) | ||
| Symptoms | Pain in the RUQ | 50 (71.42) | 119 (70.1) | 0.83 |
| Biliary dispeptic syndrome | 12 (17.14) | 40 (23.36) | 0.28 | |
| Cutaneous eruption | 0 (0) | 4 (2.71) | 0.16 | |
| Hepatomegalia w/palpable mass | 1 (1.42) | 7 (4.3) | 0.46 | |
| Comorbidities | Hypertension | 9 (12.85) | 32 (19.02) | 0.24 |
| Ischemic cardiopathy | 2 (2.85) | 14 (8.15) | 0.13 | |
| Type II diabetes | 4 (5.71) | 12 (7.06) | 0.78 | |
| Obesity | 6 (8.57) | 20 (11.9) | 0.43 | |
| ASA | 1 or 2 | 37 (52.85) | 90 (53.2) | 0.36 |
| 3 | 29 (41.42) | 68 (40.2) | 0.97 | |
| 4 | 4 (5.71) | 12 (6.5) | 0.95 | |
| Hydatid elements in the CBD | 6 (8.57) | 19 (11.17) | 0.34 | |
| Median ALT value | 45 (25-180) | 42 (25-220) | 0.88 | |
| Median AST value | 40 (25-190) | 45 (20-225) | 0.76 | |
The pathological characteristics of the cysts and the surgical treatment are presented in Table 2. The median size of the liver hydatid cyst in the laparoscopic group was 6.5 cm (range: 2-17 cm). Compared with the open approach group, in which the median size was 7.5 (range: 2-20 cm), the difference was statistically significant (P = 0.001). Although both groups were relatively similar in the lobe distribution of the cysts and the number of cysts involved, as well as the distribution of the cysts regarding the size, there were statistically significant differences in the involvement of segments 7 and 8 (28.57% vs 43.47%, P = 0.03 and 21.42% vs 35.86%, P = 0.027 respectively). Conversion to open surgery was required in 7 cases, with the reasons listed in Table 3.
| Parameter | Laparoscopic, n = 70 (%) | Open approach, n = 170 (%) | P value | |
| Liver segments | II-IV | 27 (38.5) | 41 (24.11) | 0.04 |
| V-VI | 28 (40) | 48 (28.23) | 0.14 | |
| VII | 20 (28.57) | 63 (37.05) | 0.03 | |
| VIII | 15 (21.42) | 54 (31.24) | 0.02 | |
| I | 1 (1.42) | 11 (6.47) | 0.06 | |
| Distribution | Right lobe | 44 (62.85) | 105 (61.95) | 0.89 |
| Left lobe | 18 (25.72) | 31 (18.48) | 0.2 | |
| Both lobes | 8 (11.43) | 34 (20) | 0.14 | |
| Number of cysts | Unique cysts | 59 (84.28) | 134 (72.82) | 0.04 |
| Multiple cysts | 11 (15.72) | 50 (27.18) | ||
| Dimension of cysts | Smaller than 5 cm | 17 (24.28) | 37 (20.13) | 0.41 |
| 5-10 cm | 47 (67.14) | 113 (61.42) | 0.38 | |
| Larger | 6 (8.57) | 34 (18.45) | 0.06 | |
| Median diameter (cm) | 6.5 (2-17) | 7.5 (2-20) | 0.001 | |
| No cystobiliary communication (cm) | 5.5 (2-17) | 7 (2-17) | 0.02 | |
| With cystobiliary communication (cm) | 6 (4-10) | 8 (3-20) | 0.01 | |
| Type of cyst | Pure clear fluid cyst | 16 (22.85) | 39 (22.82) | 0.93 |
| Hydatid daughter cyst | 33 (47.14) | 70 (41.3) | 0.86 | |
| Calcified cyst | 9 (12.85) | 33 (19.56) | 0.43 | |
| Avital hydatid cyst | 6 (8.57) | 5 (2.92) | 0.07 | |
| Secondarily infected cyst | 6 (8.57) | 23 (13.58) | 0.22 | |
| Type of surgery | Lagrot percystectorny | 56 (80) | 118 (69.56) | 0.26 |
| Total percystectomy | 8 (11.45) | 33 (20.1) | 0.14 | |
| Hepatic resection | 6 (9.55) | 19 (11.34) | 0.67 | |
| Surgical parameters | Intraoperative complications | 0 (0) | 9 (4.89) | 0.04 |
| Postoperative complications | 4 (5.7) | 13 (7.06) | 0.76 | |
| Presence of cysto-biliary fistula | 13 (18.57) | 56 (32.9) | 0.01 | |
| Median operative time (min) | 75 (50-110) | 100 (55-280) | 0.001 | |
| Median blood loss (mL) | 35 (0-120) | 90 (0-400) | 0.001 | |
| Postoperative mortality | 0 (0) | 0 (0) | 1 | |
| Reasons for conversion to open surgery | |
| Unable to find the cyst based on the imaging | 2 |
| Difficult access | 2 |
| Unable to suture the cystobiliary fistula | 1 |
| Unable to provide adequate haemostasis | 1 |
| Difficulty in mobilizing the liver | 1 |
| Total | 7 |
The median operative time was 75 min (range: 50-110) in the laparoscopic group and 100 min (range: 55-280 min) in the open approach group (P < 0.001). Median blood loss was 35 mL (range: 0-100 mL) for the laparoscopic group, and 90 mL (rang: 0-400 mL) for the open approach group (P < 0.001). The mortality rate was 0% in both groups. The intraoperative complication rate in the laparoscopic group was significantly lower in the laparoscopic group (0% vs 4.89%, P = 0.04). Of the 73 cases that presented with cystobiliary fistula, 13 were found in the laparoscopic group and 60 in the open approach group, with a statistically significant difference (18.57% vs 32.60%, P = 0.02).
Regarding the postoperative complications (Table 4), although there was no statistically significant difference in the overall postoperative complications (5.7% vs 7.06%, P = 0.76), there was a significant difference regarding the abdominal wound complications between the groups (0% vs 4.7%, P = 0.04). In the laparoscopic group, there were 3 cases of liver abscesses of the residual cavities that were laparoscopically drained. One case developed an external fistula that was treated conservatively. Most of the postoperative complications in the open approach group were comprised of the abdominal wound complications (suppuration, seromas, and infection), which required a longer hospitalization stay and daily antiseptic treatment and/or collection evacuation, presenting a good prognosis. One case developed an external fistula, which was adequately drained with complete closure in 7 d.
| Complications | Laparoscopic, n = 70 (%) | Open approach, n = 170 (%) | P value |
| Postoperative complications | 4 (5.7) | 13 (7.06) | 0.76 |
| Abdominal wound complications | 0 (0) | 8 (4.7) | 0.04 |
| External fistulas | 1 (1.4) | 1 (0.58) | 0.93 |
| Liver abscesses | 3 (4.28) | 4 (2.35) | 0.21 |
To assess the risk of developing cystobiliary fistula based on cyst dimension, an ROC curve was generated to determine whether the cyst size is a good predictor of developing cystobiliary fistula (Figure 1A). Thus, a cutoff point of 6.85 cm was determined with an AUC of 0.71 (moderate to good predictor, P = 0.001). Therefore, cysts larger than 6.85 cm present a higher risk of developing cystobiliary fistula for which MRCP is required for a full assessment. ROC curves were used to determine if the cyst size is a good predictor based on surgery type (Figure 1B). Thus, cyst size in the laparoscopic group was considered a poor predictor with an AUC of 0.52 (P = 0.67, cutoff value of 5.7 cm). In the open surgery group, cyst size was considered a poor to moderate predictor (AUC = 0.69, P = 0.007, cutoff value of 7.4 cm).
The median hospital stay was 4 d (range: 2-11 d) in the laparoscopic group and 6 d (range: 3-21 d) in the open approach group, with the stay being significantly longer for the second group (P = 0.01). There were no differences regarding the median follow-up period (24 mo vs 26 mo, P = 0.35). The recurrence rate for the laparoscopic approach group was lower than that for the open approach group, although the difference was not statistically significant (4.2% vs 5.2%, P = 0.63). These elements are showcased in Table 5.
| Postoperative parameter | Laparoscopic, n = 70 (%) | Open approach, n = 170 (%) | P value |
| Recurrence rate | 3 (4.2) | 9 (5.2) | 0.63 |
| Median hospital stay | 4 (2-11) | 6 (3-21) | 0.01 |
| Median follow-up period | 24 (9-48) | 26 (648) | 0.35 |
A comparison of the general preoperative and postoperative parameters as well as the surgical technique between the two groups was performed, as listed in Table 6. The frequency of the laparoscopic approach was significantly higher in the current laparoscopic group (27.55% vs 17.71%, P = 0.005), with slightly higher conversion rate (8.10% vs 4.80%, P = 0.17) and median hospitalization (4 d vs 6 d, P = 0.001). Regarding the surgical technique, there were no differences in lagrot pericystectomy and total pericystectomy (80% vs 91.52%, P = 0.11 and 11.45% vs 8.48%, P = 0.79 respectively). There were 6 cases of laparoscopic liver resection, and the difference was statistically significant (9.55% vs 0%, P = 0.001). No other statistically significant difference in the median operative time, mean cyst size, or postoperative morbidity was recorded.
| Postoperative parameter | Cument laparoscopic group, n = 70 (%) | Previous laparoscopic group, n = 59 (%) | P value | |
| Surgery type | Lagrot pericystectomy | 56 (80) | 54 (91.52) | 0.11 |
| Total pericystectorny | 8 (11.45) | 5 (8.48) | 0.79 | |
| Hepatic resection | 6 (9.55) | 0 (0) | 0.04 | |
| Postoperative morbidity | 4 (5.71) | 6 (10.16) | 0.11 | |
| Frequency (%) | 28.34 | 17.71 | 0.005 | |
| Median cyst size | 6.5 (2-17) | 6.4 (2-15) | 0.28 | |
| Median duration (min) | 75 (50-110) | 72 (45-130) | 0.41 | |
| Conversion rate (%) | 8.10 | 4.80 | 0.17 | |
| Median hospital stay (d) | 4 (2-11) | 6 (1-28) | 0.001 | |
Although the risk of complications in the laparoscopic treatment of hydatid disease of the liver has not been fully evaluated, there has been a continuous increase in its usage during the last decade[6]. The important steps in this surgery remain removal of the cyst contents with as minimum risk of spillage as possible, sterilization of the cyst cavity, and closure of the remaining cavity. Moreover, even though surgery remains one of the main choices of treatment in hydatid disease of the liver, there is still a debate regarding the optimal choice of surgical treatment. A meta-analysis performed by Sokouti et al[7] highlighted the advantages of the minimally invasive puncture, aspiration, injection, and respiration technique in uncomplicated cysts, such as being more cost-effective with minimal risks; however, it is usually recommended for patients who cannot benefit from surgery due to various reasons (comorbidities and refusal of treatment) and it is contraindicated in patients with cystobiliary communication, while also having a higher recurrence rate. The indication of cholecystectomy was either elective, due to the presence of gallstones, which would pose a high risk of migration, or tactical to obtain adequate access to the cysts. In addition, in cases where ERCP associated with sphincterectomy or stenting for biliary decompression is needed, cholecystectomy is mandatory.
Compared to our previous article, this study had less exclusion criteria, which allowed us to showcase the differences between the previous and the current 10 years of laparoscopic surgery in the treatment of hydatid disease of the liver. Our previous series of 231 patients (59 laparoscopic approach vs 172 open approach) remains one of the largest series in the literature[8], with the current series showcasing a significant volume as well. One of the major differences between our two series resides in a slightly higher conversion rate and a lower hospitalization duration. The increase of conversion rate, although not statistically significant, can reflect the lack of selection criteria.
Regarding the demographic parameters, a statistically significant difference between the mean age of the two groups was recorded. This mean difference gap of 4.49 years could highlight the tendency for a minimally invasive approach in younger patients due to their better health condition; however, more reports are required in that regard. There were no statistically significant differences regarding sex, environment, symptoms at presentation, comorbidities, or ASA score. Although our previous study reported differences related to the patient’s body mass index regarding the surgical approach, there were no statistically significant differences highlighted by our current study.
We did not use the cyst location as an exclusion criterion, although the differences between the laparoscopic approach and the open approach were statistically significant for the 7th segment. A statistically significant difference between the two groups regarding the cyst diameter was recorded, which could indicate a tendency towards open approach in cysts over 10 cm in diameter, although a reasonable number of cases with cysts of over 10 cm in diameter were treated laparoscopically. There is a constant change regarding the indications for the laparoscopic approach; however, due to improved imaging and better training, most of the contraindications regarding cyst diameter, cyst location, and cystobiliary fistula are in direct proportion with the surgeon’s skill. Thus, the biggest limitation remains the surgeon’s personal experience in hepatic surgery. However, some selection criteria need to be maintained, especially regarding the less accessible liver segments and for less experienced surgeons. Therefore, caution must be maintained when selecting cases in the posterior segments and in the caudate lobe as candidates for laparoscopic surgery.
There were statistically significant differences regarding the intraoperative parameters between the two groups, such as mean duration, blood loss, and presence of intraoperative complications. A lower mean duration in the laparoscopic approach can be explained by the fact that the more difficult cases are reserved for the open approach, thus taking longer to be resolved. Net duration of the open procedures was compared, although a slight bias might exist regarding the reporting of net duration (excluding the time from accessing and exiting the abdominal cavity) due to a shift to the electronic database which occurred in the late 2000s. Compared to our previous study, although not significant, there was a median difference of 3 min recorded between our current and previous studies, which can be further explained by the increasing complexity of the laparoscopically treated cases in our current group. The most frequent reasons for conversion to open surgery were in terms of difficult access and incompatibility of the diagnosis based on imaging. Establishing the diagnosis of hydatid cyst of the liver via imaging methods can sometimes prove to be a difficult task; therefore, such inconsistencies are reported in the literature[9,10].
One of the major advantages of the laparoscopic approach remains the magnified imaging of the cyst. Being able to insert the camera into the cystic cavity can permit a thorough inspection, allowing early detection of cystobiliary communications or remnant membranes. Thirteen cases presented with biliocystic fistula, which underwent the laparoscopic approach. The biliocystic communication was closed by either clipping or placing a laparoscopic suture, depending on the size and the surgeon’s experience, although this method can sometimes prove difficult to be achieved laparoscopically, thus supporting the observed statistically significant difference between the laparoscopic and open approaches regarding the presence of cystobiliary fistula. However, due to the improved imaging and the possibility of postoperative ERCP for lowering the biliary pressure or in case of the presence of biliary fistulas, the laparoscopic approach is more widely considered, even in the presence of biliocystic communication, with more studies supporting this statement[11-13].
Although the usage of MRCP in our study was limited, due to its low accessibility in the earlier cases, it can pose a selection bias, since cases evaluated via MRCP might be more carefully selected, with easier cases benefitting from laparoscopic surgery and thus improving the postoperative parameters. However, it is important to assess the size of the biliocystic communication through various methods (e.g., intraoperative cholangiography or preoperative MRCP) to establish the viability of laparoscopic closure of the fistula. Our study encountered two external fistulas that were resolved conservatively. Although MRCP was not routinely performed, we recommend based on our findings that MRCP should routinely be performed for cysts over 6.5 cm to evaluate the presence of cystobiliary communication.
There were no statistically significant differences regarding the postoperative morbidity between the open and laparoscopic approach groups, nor between the current and previous laparoscopic approach groups. There were no fatalities registered. The median hospital stay was significantly shorter for the laparoscopic group, and compared to our previous study, there was a lower hospitalization duration for the current laparoscopic group (4 d vs 6 d). There were no differences regarding the recurrence rate between the laparoscopic and open approaches; however, we encountered a slightly higher recurrence rate compared to our previous study. Compared to similar studies, the recurrence rate was relatively similar, ranging from 1% to 20%[1,2,6].
There were no statistically significant differences in the type of the cyst or the type of surgery between the two groups. In contrast to our previous experience, 6 cases underwent laparoscopic resection on cases in which the cysts would occupy more than 70% of one segment with the presence of cystobiliary communication, in peripheric segments, developing no postoperative complications or comorbidities. Although this is a radical method, laparoscopic liver resection in the hydatid disease of the liver can be considered an alternative, feasible method of surgical treatment, with an increase in popularity in the last decade, showcased by recent studies[14,15]. However, the lack of a statistically significant difference between the techniques highlights the fact that the surgical approach is specifically based on each patient.
Recent practices exemplify the emergence of robotic surgery in the treatment of hydatid cysts. Robotic surgery is known for its superiority in terms of maneuverability, a better fine dissection which can allow removal of deeper intraparenchimatous cysts, as well as maintaining a similar rate of complication and recurrence in comparison with laparoscopic surgery[16-18]. However, one of the major disadvantages of robotic surgery consists of its cost effectiveness, which can be a deterrent for some tertiary centers. Therefore, robotic surgery is currently practiced by a select number of high-volume centers.
Our study has some limitations. First, being a retrospective study, the data completed in both electronic databases and medical archives might have errors in completion, which was one of the main reasons for excluding patients with incomplete data. Second, as a retrospective analysis, the choice for open or laparoscopy surgery can be purely subjective based on the surgeon’s experience, which in a retrospective setting cannot be adequately quantified. One of the main reasons for comparing the current laparoscopic experience with the one from our previous study was to diminish this limit, highlighting a significant improvement with a broadened case selection, improved postoperative recovery as well as maintaining intraoperative parameters. Finally, compared to the current literature, our results showcase similar findings in terms of effectiveness of the laparoscopic procedure with relative changes in the management of the patients which can be explained by the current setting of our tertiary center. Some of these results might be difficult to reproduce in smaller-volume centers.
The laparoscopic treatment of hydatid cysts of the liver has been continuously evolving over the course of the last decade, due to improvements in diagnostic techniques, imaging, and instrumentation. Therefore, the barrier was constantly pushed in terms of cyst diameter, cyst location, the presence of cystobiliary communications, the presence of comorbidities, and the cyst type. An increasing number of studies have shown improving results regarding all characteristics mentioned above. There are currently no randomized clinical trials to compare the treatment modalities. However, taking all of these issues into consideration, the rapid postoperative recovery with improved aesthetic results, minimal scarring, and a low recurrence rate with minimal comorbidities should be taken into consideration when advocating for a laparoscopic treatment for hydatid disease of the liver.
Based on our current experience, laparoscopic surgery remains a safe approach for the treatment of hydatid disease of the liver, with minimal to no regard towards the comorbidities, preoperative complications, and constant increase in cyst dimension. Although some selection criteria need to be maintained, especially regarding cyst location, laparoscopic surgery can provide benefits regarding a broadened case selection, improved surgical timing, and a shorter postoperative stay. Compared with our previous laparoscopic experience, an increase in the difficulty of cases, as well as a tendency for improvement, which trends along with the surgeon’s learning curve, some selection criteria need to be maintained to minimize the risk of conversion and achieve a better outcome.
Hydatid disease of the liver is a prevalent problem in endemic areas, and surgery plays an important role in resolution. Although laparoscopic treatment is on the rise due to its increased accessibility, there are some limits that need to be addressed.
This study highlighted our experience in terms of the laparoscopic approach over the last 12 years, as well as the differences between the current laparoscopic experience and the previous one. Our aim was to showcase the improvements of the laparoscopic approach as well as its current limits.
This retrospective study compared the differences between open and laparoscopic approaches in terms of demographic data, preoperative assessment, intraoperative characteristics, and postoperative parameters, as well as follow-up, morbidity, and mortality, thus highlighting key aspects, differences, and the pearls and pitfalls of the laparoscopic approach in the treatment of this disease.
In this retrospective cohort study, patients were divided into two groups, for which the differences were showcased based on the inclusion and exclusion criteria. The database consisted of all patients who had received surgical treatment for hydatid disease of the liver over an experience of 12 years.
Despite the fact that some of the exclusion criteria were dropped, there are still some issues regarding cyst location and cyst size that impose careful selection criteria. These selection criteria should be taken into account by inexperienced surgeons. Furthermore, some imaging criteria need to be instated in larger cysts.
Based on our experience, the laparoscopic approach remains a safe, feasible approach which can be implemented in smaller volume centers, as long as some selection criteria are maintained. These selection criteria can be broadened; thus, more patients can benefit from this procedure, which accounts for better postoperative parameters, shorter postoperative hospitalization, and comparable morbidities and risks of recurrence with the open procedure.
Based on our experience, the laparoscopic approach remains a safe, feasible approach which can be implemented in smaller volume centers, as long as some selection criteria are maintained. These selection criteria can be broadened; thus, more patients can benefit from this procedure, which accounts for better postoperative parameters, shorter postoperative hospitalization, and comparable morbidities and risks of recurrence with the open procedure.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Romania
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Shalli K, United Kingdom; Zou Y, China S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Grosso G, Gruttadauria S, Biondi A, Marventano S, Mistretta A. Worldwide epidemiology of liver hydatidosis including the Mediterranean area. World J Gastroenterol. 2012;18:1425-1437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 164] [Cited by in RCA: 200] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 2. | McManus DP, Gray DJ, Zhang W, Yang Y. Diagnosis, treatment, and management of echinococcosis. BMJ. 2012;344:e3866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 249] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 3. | Gomez I Gavara C, López-Andújar R, Belda Ibáñez T, Ramia Ángel JM, Moya Herraiz Á, Orbis Castellanos F, Pareja Ibars E, San Juan Rodríguez F. Review of the treatment of liver hydatid cysts. World J Gastroenterol. 2015;21:124-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 4. | El Malki HO, El Mejdoubi Y, Souadka A, Zakri B, Mohsine R, Ifrine L, Abouqal R, Belkouchi A. Does primary surgical management of liver hydatid cyst influence recurrence? J Gastrointest Surg. 2010;14:1121-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Velasco-Tirado V, Romero-Alegría Á, Belhassen-García M, Alonso-Sardón M, Esteban-Velasco C, López-Bernús A, Carpio-Perez A, Jimenez López MF, Muñoz Bellido JL, Muro A, Cordero-Sanchez M, Pardo-Lledias J, Muñoz-Bellvis L. Recurrence of cystic echinococcosis in an endemic area: a retrospective study. BMC Infect Dis. 2017;17:455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Tuxun T, Zhang JH, Zhao JM, Tai QW, Abudurexti M, Ma HZ, Wen H. World review of laparoscopic treatment of liver cystic echinococcosis--914 patients. Int J Infect Dis. 2014;24:43-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Sokouti M, Sadeghi R, Pashazadeh S, Abadi SEH, Sokouti M, Ghojazadeh M, Sokouti B. A systematic review and meta-analysis on the treatment of liver hydatid cyst using meta-MUMS tool: comparing PAIR and laparoscopic procedures. Arch Med Sci. 2019;15:284-308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 8. | Zaharie F, Bartos D, Mocan L, Zaharie R, Iancu C, Tomus C. Open or laparoscopic treatment for hydatid disease of the liver? Surg Endosc. 2013;27:2110-2116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Derbel F, Mabrouk MB, Hamida MBH, Mazhoud J, Youssef S, Ali AB, Jemni H, Mama N, Ibtissem H, Nadia A, Ouni CE, Naija W, Mokni M, Hamida RBH. Hydatid Cysts of the Liver - Diagnosis, Complications and Treatment. In: Derbel F. Abdominal Sur. London: IntechOpen, 2012. [DOI] [Full Text] |
| 10. | Marrone G, Crino' F, Caruso S, Mamone G, Carollo V, Milazzo M, Gruttadauria S, Luca A, Gridelli B. Multidisciplinary imaging of liver hydatidosis. World J Gastroenterol. 2012;18:1438-1447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 11. | Chopra N, Gupta V; Rahul; Kumar S, Joshi P, Gupta V, Chandra A. Liver hydatid cyst with cystobiliary communication: Laparoscopic surgery remains an effective option. J Minim Access Surg. 2018;14:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Toumi O, Ammar H, Gupta R, Ben Jabra S, Hamida B, Noomen F, Zouari K, Golli M. Management of liver hydatid cyst with cystobiliary communication and acute cholangitis: a 27-year experience. Eur J Trauma Emerg Surg. 2019;45:1115-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Bayrak M, Altıntas Y. Current approaches in the surgical treatment of liver hydatid disease: single center experience. BMC Surg. 2019;19:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Jia C, Li H, Wen N, Chen J, Wei Y, Li B. Laparoscopic liver resection: a review of current indications and surgical techniques. Hepatobiliary Surg Nutr. 2018;7:277-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 15. | Coelho FF, Kruger JA, Fonseca GM, Araújo RL, Jeismann VB, Perini MV, Lupinacci RM, Cecconello I, Herman P. Laparoscopic liver resection: Experience based guidelines. World J Gastrointest Surg. 2016;8:5-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 71] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (1)] |
| 16. | Zou H, Luo L, Xue H, Wang G, Wang X, Yao Y, Xiang G, Huang X. Preliminary experience in laparoscopic resection of hepatic hydatidectocyst with the Da Vinci Surgical System (DVSS): a case report. BMC Surg. 2017;17:98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Zhao ZM, Yin ZZ, Meng Y, Jiang N, Ma ZG, Pan LC, Tan XL, Chen X, Liu R. Successful robotic radical resection of hepatic echinococcosis located in posterosuperior liver segments. World J Gastroenterol. 2020;26:2831-2838. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Christodoulidis G, Samara AA, Diamantis A, Floros T, Sgantzou IK, Karakantas KS, Zotos PA, Koutras A, Janho MB, Tepetes K. Reaching the Challenging Diagnosis of Complicated Liver Hydatid Disease: A Single Institution's Experience from an Endemic Area. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |