Published online May 27, 2023. doi: 10.4240/wjgs.v15.i5.825
Peer-review started: December 27, 2022
First decision: January 20, 2023
Revised: January 29, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: May 27, 2023
Processing time: 143 Days and 17.4 Hours
During laparoscopic resection for colorectal cancer, there is controversy regarding whether the left colic artery (LCA) should be preserved at its origin.
To investigate the prognostic significance of preservation of the LCA in colorectal cancer surgery.
Patients were divided into two groups. The high ligation (H-L) technique (refers to ligation performed 1 cm from the beginning of the inferior mesenteric artery) group consisted of 46 patients, and the low ligation (L-L) technique (refers to ligation performed below the initiation of the LCA) group consisted of 148 patients. Operative time, blood loss, lymph nodes with tumor invasion, post
The average number of lymph nodes detected in postoperative pathological specimens was 17.4/person in the H-L group and 15.9/person in the L-L group. There were 20 patients (43%) with positive lymph nodes (lymph node metastasis) in the H-L group and 60 patients (41%) in the L-L group. No statistical differences were found between the groups. Complications occurred in 12 cases (26%) in the H-L group and in 26 cases (18%) in the L-L group. The incidences of postoperative anastomotic complications and functional urinary complications were significantly lower in the L-L group. The 5-year survival rates in H-L and L-L groups were 81.7% and 81.6%, respectively, and relapse-free survival rates were 74.3% and 77.1%, respectively. The two groups were similar statistically.
Complete mesenteric resection combined with lymph node dissection around the inferior mesenteric artery root while preserving the LCA is a beneficial surgical approach during laparoscopic resection for colorectal cancer.
Core Tip: Colorectal cancer is a common disease. The operative method is related to the prognosis. We studied the correlation between different ligation sites of the inferior mesenteric artery and curative effect. There were 20 patients (43%) in the high ligation group and 60 patients (41%) in the low ligation group with positive lymph nodes. There was no significant difference in survival between the two groups. However, the incidences of postoperative anastomotic complications and functional urinary complications were significantly lower in the L-L group. This study confirmed that preservation of the left colic artery should be recommended in the surgery.
- Citation: Liu FC, Song JN, Yang YC, Zhang ZT. Preservation of left colic artery in laparoscopic colorectal operation: The benefit challenge. World J Gastrointest Surg 2023; 15(5): 825-833
- URL: https://www.wjgnet.com/1948-9366/full/v15/i5/825.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i5.825
During laparoscopic resection of colorectal cancer there is controversy about the ligation site of the inferior mesenteric artery (IMA). There are currently two main opinions. Some doctors believe that the ligature should be performed at the beginning of IMA (high ligation, H-L), while others believe that the ligature should be performed after the dissection of the left colic artery (LCA) [preserving the LCA, low ligation (L-L)][1]. H-L, which is beneficial for removal of lymphatic tissue from the root of the IMA completely (especially lymph node No. 253), allows accurate staging of the postoperative tumor stage. H-L technology is easier to perform, and the anastomosis is essentially tension-free for complete mesenteric release. It is also easy for beginners to learn. However, because the anastomotic blood supply after high tie comes exclusively from the superior mesenteric vessels, for some patients, especially those with congenital absence of the marginal aortic arch, the anastomotic blood supply is significantly reduced, which increases the chance of intestinal fistula. Furthermore, autonomic nerve injury impacts postoperative bowel and urinary function recovery[2].
According to the Japan Colon and Rectal Cancer Association, the positive rate of lymph node metastasis around the root of the IMA root was 3.6% for colon cancer (stage T3-T4) and 5.1% for rectal cancer from 2011 to 2021, which were similar to statistics in Europe and the United States. Therefore, dissecting lymph node (LND) No. 253 is a necessary surgical step[3]. There are insufficient data to support whether simultaneous No. 253 LND while preserving the LCA and autonomic nerves can achieve satisfactory outcomes while reducing adverse events and complications. To overcome the shortcomings of the traditional surgical approach, we performed a surgical trial of L-L of the IMA combined with dissection of peri-IMA LND. We evaluated the patients’ clinical data and prognosis between the L-L and H-L approaches.
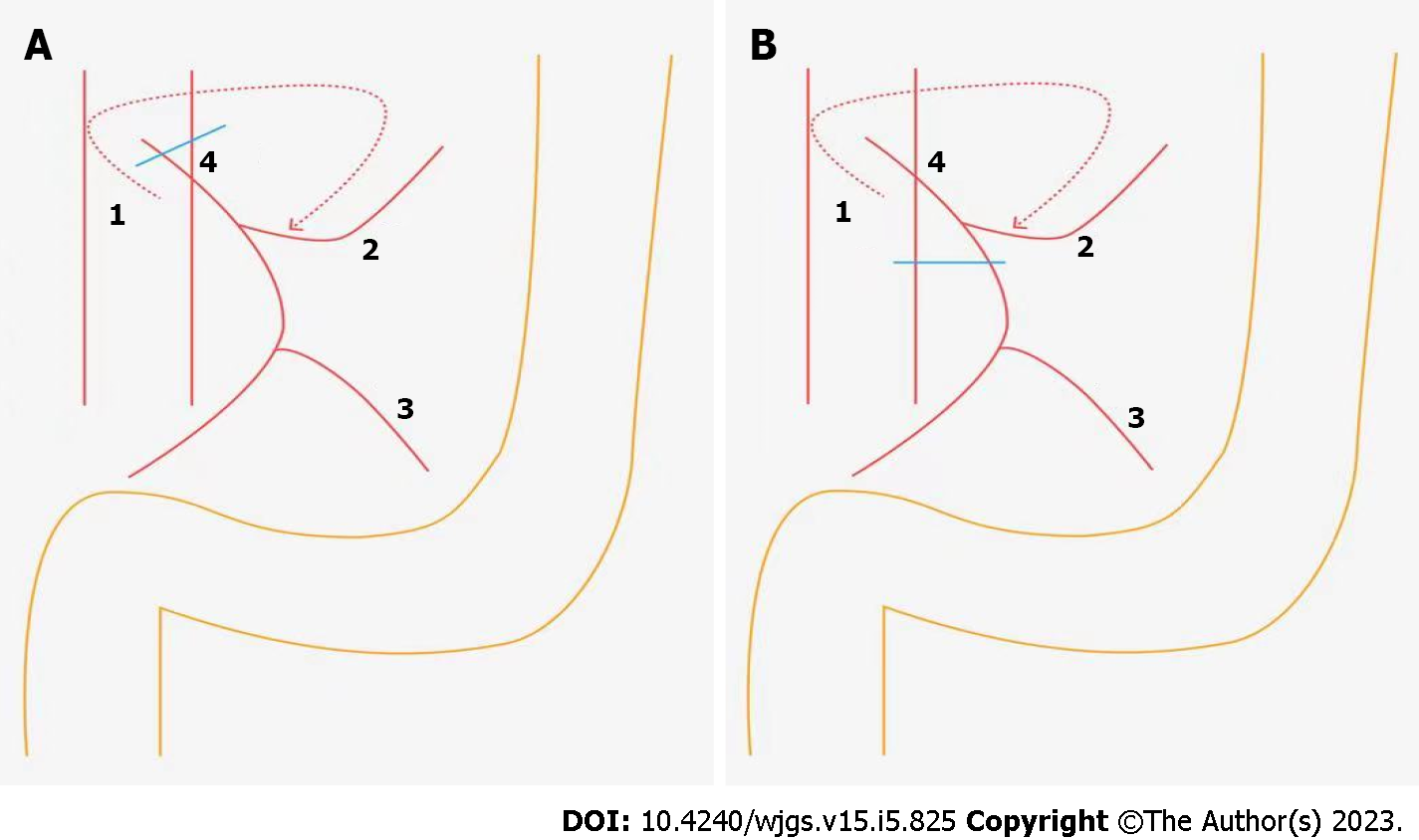
A retrospective case-control study including patients with sigmoid or rectal cancer treated surgically in the Department of General Surgery, Beijing Friendship Hospital, Capital Medical University were prospectively recorded and retrospectively analyzed between February 2014 to February 2016. According to the location of the vessel ligation the patients were divided into two groups, the H-L group and L-L group (Figure 1). The diagnostic criteria of colorectal cancer were postoperative pathological examination.
Inclusion criteria were: (1) Patients with clearly diagnosed colorectal cancer who had preoperative indications for surgery diagnosed by magnetic resonance imaging or computed tomography; (2) No invasion of the adipose tissue surrounding the intestinal tract and no encapsulation of major vascular structures; and (3) No distant metastasis or peritoneal implantation.
Exclusion criteria were: (1) Patients with acute perforation or obstruction prior to surgery; (2) Patients with abdominal perineal resection combined with radical resection of rectal cancer; and (3) Patients with concurrent intestinal lesions.
The study was approved by the Ethics Committee of Beijing Friendship Hospital Affiliated to Capital Medical University, with the approval No. PM6475.
Clinical data characteristics of all enrolled patients were analyzed, including age of onset, sex, tumor site, operation time, blood loss, number of lymph nodes with tumor metastasis (positive nodes), number of lymph nodes around the IMA root, total number of lymph nodes in the sample, recovery time of intestinal function, and national standard tumor staging. The tumor staging was defined according to the TNM staging System (7th edition) updated by the United Cancer Council and the United International Cancer Center.
The subjects were regularly examined in the outpatient department after discharge and were routinely examined in the outpatient department every 6 mo from discharge. The last follow-up date was September 15, 2022. The 5-year survival rate and recurrence-free survival rate were observed. Among them, overall survival referred to the time from the date of the operation to the date of death by the tumor. Patients were followed-up regularly by performing 1-2 colonoscopies or computed tomography examinations annually.
The surgical modalities were radical resection of sigmoid or rectal cancer. The location of the IMA ligation site (preserving or not preserving the LCA) was determined by each surgeon on a case-by-case basis according to the presence of intraoperative bleeding, visibly enlarged lymph nodes around the artery, the operator’s skill, and the ease of separating the vessels.
Data with normal distribution were expressed as mean ± standard deviation, and the χ2 test was adopted to check whether the population rates of independent samples were the same. The t-test was used to compare whether the sample means of two independent samples were statistically significant. The 5-year survival rate between the two groups was compared by the log-rank test. We used SAS statistical software (version 23.0; IBM Corp.) for all analyses, and P < 0.05 was considered statistically significant.
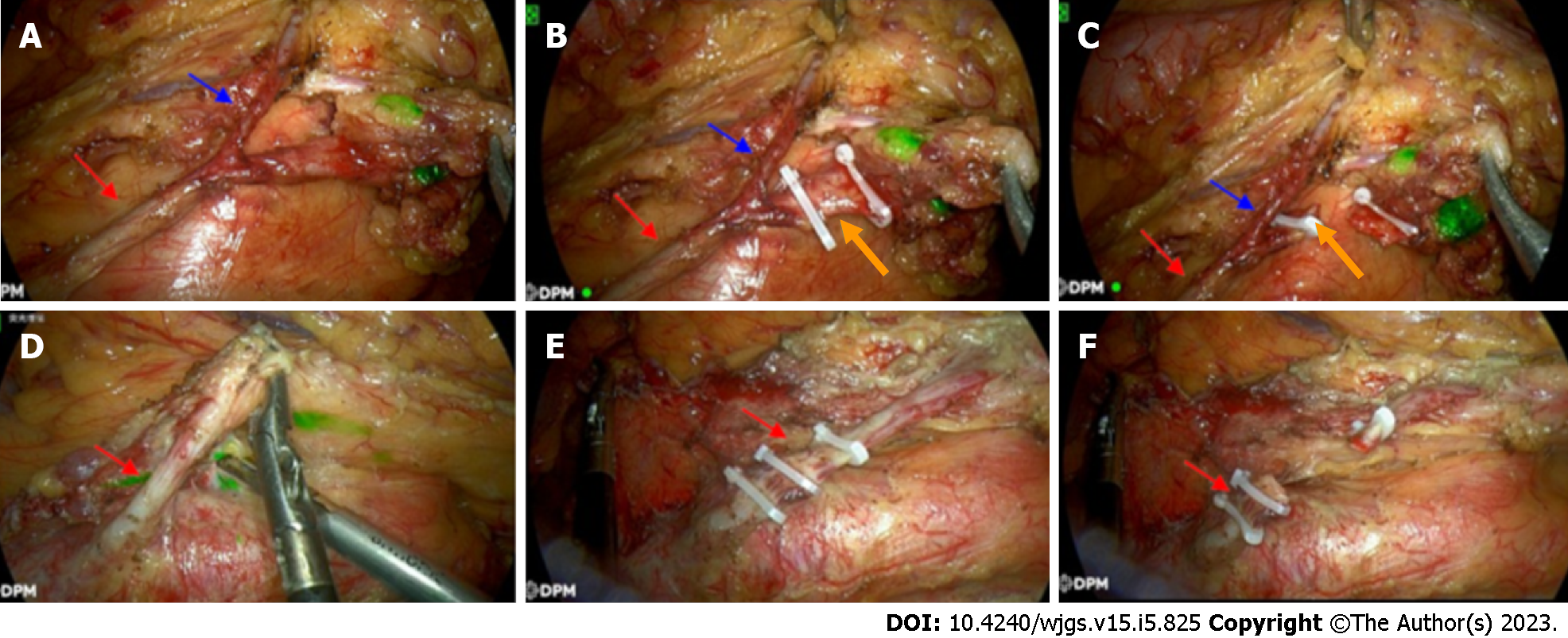
This study involved 194 patients, who were divided into two groups according to the location of the vessel ligation: 46 in the H-L group, where the ligation was performed at the root of the IMA; and 148 in the L-L group (preservation LCA in the operation), where the vessel ligation was performed at the beginning of the LCA (Figures 1 and 2). No. 253 LND was also performed in both groups. There were no statistical differences in age, sex, and tumor site between the two groups as shown in Table 1.
| Group | High ligation group, n = 46 | Low ligation group, n = 148 | P value |
| Sex as male/female | 28/18 | 90/58 | 0.897 |
| Age in yr, mean ± SD | 58.3 ± 10.1 | 60.4 ± 9.4 | 0.645 |
| Tumor site | 0.178 | ||
| Sigmoid colon | 16 | 46 | - |
| Recto-sigmoid junction | 13 | 34 | - |
| Upper rectum | 10 | 39 | - |
| Lower rectum | 7 | 29 | - |
The average number of lymph nodes detected was 17.4/person for the H-L group and 15.9/person for the L-L group in postoperative pathological specimens. There were 20 patients (43%) in the H-L group and 60 patients (41%) in the L-L group with positive lymph nodes. We found no significant difference between the two groups. Regarding the IMA root lymph nodes (No. 253), there were 2 positive cases in the H-L group (4%) and 5 positive cases in the L-L group (3%). There was still no significant difference between the two groups. The recovery time of bowel function was shorter in the L-L group (Table 2).
| Variable | High ligation group, | Low ligation group, | P value |
| Operative time in min, mean ± SD | 210.0 ± 34.2 | 232.0 ± 28.3 | 0.482 |
| Blood loss in mL, mean ± SD | 145.0 ± 30.3 | 187.0 ± 50.3 | 0.165 |
| Patients with positive lymph nodes, n | 20 | 60 | 0.854 |
| Number of lymph nodes dissected, mean | 17.4 | 15.9 | 0.203 |
| Patients with positive lymph nodes in the root of the inferior mesenteric artery, D253 | 2 | 5 | 0.372 |
| Time to recovery of bowel function in d, mean ± SD | 5.0 ± 1.8 | 3.0 ± 1.2 | 0.042 |
No metastasis was found in the lymph nodes of 114 patients (58%), while positive lymph nodes were observed in 80 patients (42%), including 7 cases (3%) at station 3 (No. 253), 5 of which had positive station 1 and 2 lymph nodes. Positive lymph nodes were observed most often at station 1 and station 2 but rarely at station 3.
Complications occurred in 12 cases (26%) in the H-L group and 26 cases (18%) in the L-L group. Wound infection (n = 17) was the most common complication in both groups, and the incidences of postoperative anastomotic complications and functional urinary complications were significantly lower in the L-L group. The incidences of other complications were similar between the two groups (Table 3).
| Complication | High ligation group, n = 46 | Low ligation group, n = 148 | P value |
| Number of complications | 12 (26) | 26 (186) | 0.436 |
| Wound infection | 4 (9) | 13 (9) | 0.286 |
| Stress ulcers | 2 (4) | 6 (4) | 0.316 |
| Anastomotic fistula and stricture | 3 (7) | 5 (3) | 0.045 |
| Urinary dysfunction | 3 (7) | 2 (1) | 0.029 |
There were 11 cases (24%) in the H-L group and 32 cases (22%) in the L-L group of postoperative recurrence, which was similar between the two groups. There were 2 cases (4%) in the H-L group and 6 cases (4%) in the L-L group of local lymph node recurrence, with no significant difference between the groups. The most common organ of recurrence in the H-L group (4 cases, 9%) and the L-L group (11 cases, 7%) was the lung, with no significant difference between the groups (Table 4).
| Recurrence site | High ligation group, n = 46 | Low ligation group, n = 148 | P value |
| Overall recurrence rate | 11 (24%) | 32 (21%) | 0.607 |
| Liver | 3 | 9 | - |
| Lung | 4 | 11 | - |
| Lymph nodes | 2 | 6 | - |
| Local recurrence (intestinal tract) | 0 | 2 | - |
| Peritoneum | 2 | 4 | - |
The 5-year survival rates in the H-L and L-L groups were 81.7% and 81.6%, respectively, and the relapse-free survival rates were 74.3% and 77.1%, respectively. The two groups were similar statistically. In patients with lymph node metastases the 5-year survival rates were 68.1% vs 66.2% and the relapse-free survival rates were 65.3% vs 64.9% in the H-L and L-L groups, respectively, with no significant differences.
The presence or absence of lymph node metastasis is significantly related to the prognosis of patients with colorectal cancer, and detailed examination of each surgical specimen is an important index. According to the American Joint Committee on Cancer/Union for International Cancer Control guidelines, a minimum of 12 lymph nodes must be diagnosed in postoperative specimens. However, clinically reaching the recommended number of lymph nodes is sometimes very difficult[4]. In such cases, fine dissection of the intestinal vessels, especially the IMA, is essential to achieve the recommended number of lymph nodes. Therefore, choosing high- or low-tie IMA ligation remains controversial.
Except for a few colon cancers without lymphatic metastases in early stages, LND at the root of the IMA is a key step. Considering the completeness of tumor treatment, IMA ligation at the root is the standard procedure in many hospitals in China. An analysis by Rutegård et al[5] found that only 8.7% of patients had positive IMA root lymph nodes, and the rate of positive IMA root lymph nodes in this study was 4%. This is an important finding suggesting that No. 253 LND should be performed in all patients with distal colorectal cancer; otherwise approximately 4%-8%[6] of patients may have residual tumor at this site. The second reason for this anatomical dissection is the phenomenon of skip metastasis, which was found in the No. 253 lymph nodes of 2 cases in our study. This coincides with the findings of Mari et al[7], which identified this metastasis in 1.9% of the patients. Therefore, these findings provide a theoretical basis for LND at the IMA root.
In the present study, there was no difference in the number of lymph nodes obtained by high-tie or low-tie, the number of positive lymph nodes, and the ratio of positive-to-harvested lymph nodes, including the number of lymph nodes at the IMA root, suggesting that complete LND is still feasible even without IMA ligation. The rate of metastasis in the IMA root lymph nodes was relatively constant with or without high ligation. During LND, careful vascular dissection and complete mesenteric resection are more important than the ligation site. Postoperative survival was not related to the tie level in this study but rather to the completeness of radical surgery. With advances in surgical techniques, more studies have observed no significant difference between the two ligation levels regarding LND. In fact, all clinical cases of local recurrence have occurred in incomplete or near-complete rectal mesenteric resections.
To prevent such an insurmountable problem as anastomotic leak after colorectal resection, more hospitals are selectively preserving the LCA to maintain anastomotic blood flow, benefiting from continuous advances in surgical techniques for colon cancer. The incidence of intestinal fistula in rectal cancer in China has ranged from 5% to 26% in the past 5 years[8]. Tension-free anastomosis and good blood supply are the two main considerations to reduce this serious complication. High-tie can reduce blood flow to the colon leading to intestinal ischemia, which may eventually lead to anastomotic leak or stricture and is a common postoperative complication. In this study, there was a significant increase in the incidence of anastomotic stricture in the H-L group. This was confirmed by intraoperative Doppler ultrasonography and the use of indocyanine green angiography in a study by Ogino et al[9], which revealed a 50% decrease in anastomotic blood flow after high tie. Treating anastomotic fistula or stricture is difficult once it occurs. There may also be cases of autonomic nerve disorders (e.g., urinary and sexual dysfunction) owing to disruption of the IMA root plexus (Table 3).
The level of IMA ligation is partly related to the freeness of the proximal colon. In many studies, high tie of the IMA resulted in better free bowel[10]. Some researchers believe that high ligation of the IMA allows adequate free colon and ensures a tension-free colonic anastomosis. However, inadequate free bowel can now be completely resolved by technical means, such as ligation of the inferior mesenteric vein at the level of the lower margin of the pancreas and freeing the splenic flexure of the descending colon[11]. Another advantage of this surgical approach is that because the LCA is preserved it is also possible to reoperate on the residual colon if secondary carcinoma occurs in the ascending or transverse colon after surgery for sigmoid or rectal cancer[12]. Therefore, IMA LND based on LCA preservation has become the main surgical approach in some hospitals. The key in this approach is total mesenteric resection and clearance of group D3 lymph nodes (such as No. 253)[13,14].
In this study, 194 patients underwent radical surgery for sigmoid or rectal cancer, and we compared the postoperative complication rates, recurrence rates, and prognosis of high vs low IMA ligation combined with LND. The results showed that the incidence of anastomotic leak was significantly lower in the low ligation plus LND group. Furthermore, the incidence of postoperative urinary dysfunction was significantly lower, and the recovery time of bowel function was shorter[15]. In addition, there was no significant difference in the 5-year survival and relapse-free survival rates for all enrolled patients. These results demonstrate the reliability of preserving the LCA while performing LND.
High ligation of IMA in colorectal cancer operation is a simple method that can clean the lymph nodes completely. However, the incidence of intestinal fistula increased significantly, and the postoperative recovery was slow[16]. In this study, with the investigation of the prognostic impact of the ligation site of IMA in colorectal cancer surgery in 194 patients, it is found that complete mesenteric resection and IMA root LND while preserving the LCA is a more reliable and safe surgical approach in patients undergoing colorectal cancer surgery.
Sigmoid and rectal tumors are the most common intestinal tumors, accounting for 80% of all colorectal cancers. Surgery is still the preferred and primary treatment of intestinal tumors, and the anatomical basis is total mesangectomy. However, a critical point is that the location of ligation of the inferior mesenteric artery (IMA) is still under debate.
At present, there are two mainstream methods used in laparoscopic colorectal cancer surgery. One is high ligation (H-L), that is, ligation at the beginning of the IMA, and the other is low ligation (L-L) at the distal end of the left colic artery. The two methods have their own advantages. Therefore, we systematically compared the two methods to provide a reference basis for surgeons to choose.
To investigate the prognostic significance of the ligation site of the IMA in colorectal cancer surgery.
We retrospectively analyzed the data of 194 patients undergoing radical R0 resection at Beijing Friendship Hospital between February 2014 to February 2016. Operative time, blood loss, positive lymph nodes and the number of dissected lymph nodes, postoperative complications and recovery, recurrence rate, and 5-year survival rate were compared between the H-L group and L-L group.
The average number of lymph nodes detected in postoperative pathological specimens was 17.4/person in the H-L group and 15.9/person in the L-L group. There were 20 patients (43%) in the H-L group and 60 patients (41%) in the L-L group with positive lymph nodes, with no statistical differences between the groups. Complications occurred in 12 cases (26%) in the H-L group and 26 cases (18%) in the L-L group, with no significant difference in the incidence between the groups. The incidences of postoperative anastomotic complications and functional urinary complications were significantly lower in the L-L group. The incidence of other complications was similar between the two groups. The 5-year survival rates in the H-L and L-L groups were 81.7% and 81.6%, respectively, and relapse-free survival rates were 74.3% and 77.1%, respectively. The two groups were similar statistically.
Complete mesenteric resection and IMA root lymph node dissection while preserving the LCA is a more reliable and safe surgical approach during laparoscopic resection for colorectal cancer.
Our study demonstrated that LCA preservation is highly feasible at its origin in most cases. A preoperative computed tomography scan could predict the feasibility of the determined origin of the LCA (spread out or not) and the route (near or far away from the inferior mesenteric vein) of the LCA. In the future, multicenter prospective studies with a larger sample size are required to verify our results.
Here I would like to express my gratitude to my colleagues and classmates who helped me in the process of writing the article, in particular my mentor Dr. Zhang, who has given me great help in surgery, the clinic, and scientific research. I would also like to thank my family for their encouragement when I first started writing articles. Finally, I would like to thank the editors and reviewers for their advice. With their help, my article has been further improved.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dapri G, Belgium; Miyakita H, Japan S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Keller DS, Ishizawa T, Cohen R, Chand M. Indocyanine green fluorescence imaging in colorectal surgery: overview, applications, and future directions. Lancet Gastroenterol Hepatol. 2017;2:757-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 2. | Cai J, Wen X, Lin W, He Z, Zhu D, Qiu J, Kong D, He X, Shen Q, Wu X, Lan P, Zhou Z, Ke J. [Evaluation of three-dimensional CT reconstruction on the anatomic variation of inferior mesenteric artery and left colic artery]. Zhonghua Wei Chang Wai Ke Za Zhi. 2017;20:1274-1278. [PubMed] |
| 3. | Fan YC, Ning FL, Zhang CD, Dai DQ. Preservation versus non-preservation of left colic artery in sigmoid and rectal cancer surgery: A meta-analysis. Int J Surg. 2018;52:269-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Alici A, Kement M, Gezen C, Akin T, Vural S, Okkabaz N, Basturk E, Yegenoglu A, Oncel M. Apical lymph nodes at the root of the inferior mesenteric artery in distal colorectal cancer: an analysis of the risk of tumor involvement and the impact of high ligation on anastomotic integrity. Tech Coloproctol. 2010;14:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Rutegård M, Hemmingsson O, Matthiessen P, Rutegård J. High tie in anterior resection for rectal cancer confers no increased risk of anastomotic leakage. Br J Surg. 2012;99:127-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Kang J, Hur H, Min BS, Kim NK, Lee KY. Prognostic impact of inferior mesenteric artery lymph node metastasis in colorectal cancer. Ann Surg Oncol. 2011;18:704-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 7. | Mari G, Crippa J, Costanzi A, Mazzola M, Magistro C, Ferrari G, Maggioni D. Genito-Urinary Function and Quality of Life after Elective Totally Laparoscopic Sigmoidectomy after at Least One Episode of Complicated Diverticular Disease According to Two Different Vascular Approaches: the IMA Low Ligation or the IMA Preservation. Chirurgia (Bucur). 2017;112:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Polese L, Bressan A, Savarino E, Vecchiato M, Turoldo A, Frigo A, Sturniolo GC, De Manzini N, Petri R, Merigliano S. Quality of life after laparoscopic sigmoid resection for uncomplicated diverticular disease. Int J Colorectal Dis. 2018;33:513-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Ogino T, Okuyama M, Hata T, Kawada J, Okano M, Kim Y, Tsujinaka T. Evaluation of blood flow on the remnant distal bowel during left-sided colectomy. World J Surg Oncol. 2018;16:188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Cirocchi R, Popivanov G, Binda GA, Henry BM, Tomaszewski KA, Davies RJ, Di Saverio S. Sigmoid resection for diverticular disease - to ligate or to preserve the inferior mesenteric artery? Colorectal Dis. 2019;21:623-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Mari GM, Crippa J, Borroni G, Cocozza E, Roscio F, Scandroglio I, Origi M, Ferrari G, Forgione A, Riggio V, Pugliese R, Costanzi ATM, Maggioni D; on behalf of the AIMS Academy Clinical Research Network. Symptomatic Uncomplicated Diverticular Disease and Incidence of Unexpected Abscess during Sigmoidectomy: A Multicenter Prospective Observational Study. Dig Surg. 2020;37:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Choi EH, Suh S, Foik AT, Leinonen H, Newby GA, Gao XD, Banskota S, Hoang T, Du SW, Dong Z, Raguram A, Kohli S, Blackshaw S, Lyon DC, Liu DR, Palczewski K. In vivo base editing rescues cone photoreceptors in a mouse model of early-onset inherited retinal degeneration. Nat Commun. 2022;13:1830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 54] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 13. | Fan D, Zhang C, Li X, Yao C, Yao T. Evaluation of the clinical efficacy of preserving the left colic artery in laparoscopic resection for rectal cancer: A meta-analysis. Mol Clin Oncol. 2018;9:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Tsubaki M, Ito Y, Fujita M, Kato H. Use of the modified double-stapling technique with vertical division of the rectum during a sphincter-preserving operation for the treatment of a rectal tumor. Asian J Surg. 2012;35:110-112. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Zhang W, Yuan WT, Wang GX, Song JM. Anatomical study of the left colic artery in laparoscopic-assisted colorectal surgery. Surg Endosc. 2020;34:5320-5326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Chavda V, Siaw O, Chaudhri S, Runau F. Management of early rectal cancer; current surgical options and future direction. World J Gastrointest Surg. 2021;13:655-667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |