Published online Apr 27, 2023. doi: 10.4240/wjgs.v15.i4.740
Peer-review started: January 7, 2023
First decision: January 21, 2023
Revised: January 27, 2023
Accepted: March 21, 2023
Article in press: March 21, 2023
Published online: April 27, 2023
Processing time: 106 Days and 4.8 Hours
Colopleural fistula is a rare condition, and only a limited number of cases have been reported. Here, we report a case of idiopathic colopleural fistula in an adult without any known predisposing factors. The patient presented with a lung abscess and refractory empyema and was successfully treated with surgical resection.
A 47-year-old man with a history of lung tuberculosis, which had been completely cured 4 years ago, presented to our emergency department with a productive cough and fever for 3 d. Tracing his history, he had undergone left lower lobe segmentectomy of the left lung due to lung abscess one year ago at another hospital. However, he developed refractory empyema postoperatively despite surgical intervention including decortication and flap reconstruction. After admission, we reviewed his previous medical images and noted a fistula tract between the left pleural cavity and splenic flexure. In addition, according to his medical records, bacterial culture of the thoracic drainage showed growth of Escherichia coli and Bacteroides fragilis. Our lower gastrointestinal series and colonoscopy confirmed the diagnosis of colopleural fistula. The patient underwent a left hemicolectomy, splenectomy, and distal pancreatectomy, and the diaphragm was repaired under our care. No further empyema recurrence was noted during follow-up.
Indicative signs of colopleural fistula include refractory empyema accompanied by the growth of colonic flora in the pleural fluid.
Core Tip: Colopleural fistula is very rare and challenging in diagnosis. We reported a case of idiopathic colopleural fistula in an adult who presented with refractory empyema, and discussed several clinical findings which may help caregivers to diagnose.
- Citation: Wang CL, Cheng KC. Idiopathic colopleural fistula presenting with lung abscess and refractory empyema: A case report. World J Gastrointest Surg 2023; 15(4): 740-744
- URL: https://www.wjgnet.com/1948-9366/full/v15/i4/740.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i4.740
Colopleural fistula is a rare condition and its diagnosis is often challenging. Only a limited number of cases of colopleural fistula have been reported, and these were related to Crohn’s disease, malignancy, colon diverticulum, or abdominal or thoracic surgery[1-4]. Herein, we report a rare case of idiopathic colopleural fistula in a patient without any known predisposing factors. The patient presented with a lung abscess and refractory empyema and was successfully treated with surgical resection.
A 47-year-old man presented to our emergency department with a productive cough and fever for 3 d.
Tracing his medical history, the productive cough and fever had developed one year ago. The patient initially visited another hospital where chest radiography and computed tomography (CT) revealed a cavitating mass in the left lower lobe of the left lung. The tentative diagnosis was lung abscess; however, the possibility of malignancy could not be excluded, and segmentectomy was performed. However, he developed empyema postoperatively, and several surgical interventions, including decortication, latissimus dorsi flap reconstruction, and intercostal muscle flap reconstruction, were performed, but were unsuccessful at treating the empyema. Bacterial culture of the thoracic drainage showed the growth of Escherichia coli and Bacteroides fragilis.
The patient has the history of lung tuberculosis, which had been completely cured 4 years ago.
No relevant personal or family history was recorded.
His vital signs were stable on arrival, and physical examinations showed negative findings except mild crackles on left lung field.
Laboratory data revealed slightly leukocytosis and elevated C-reactive protein, and otherwise were within normal range.
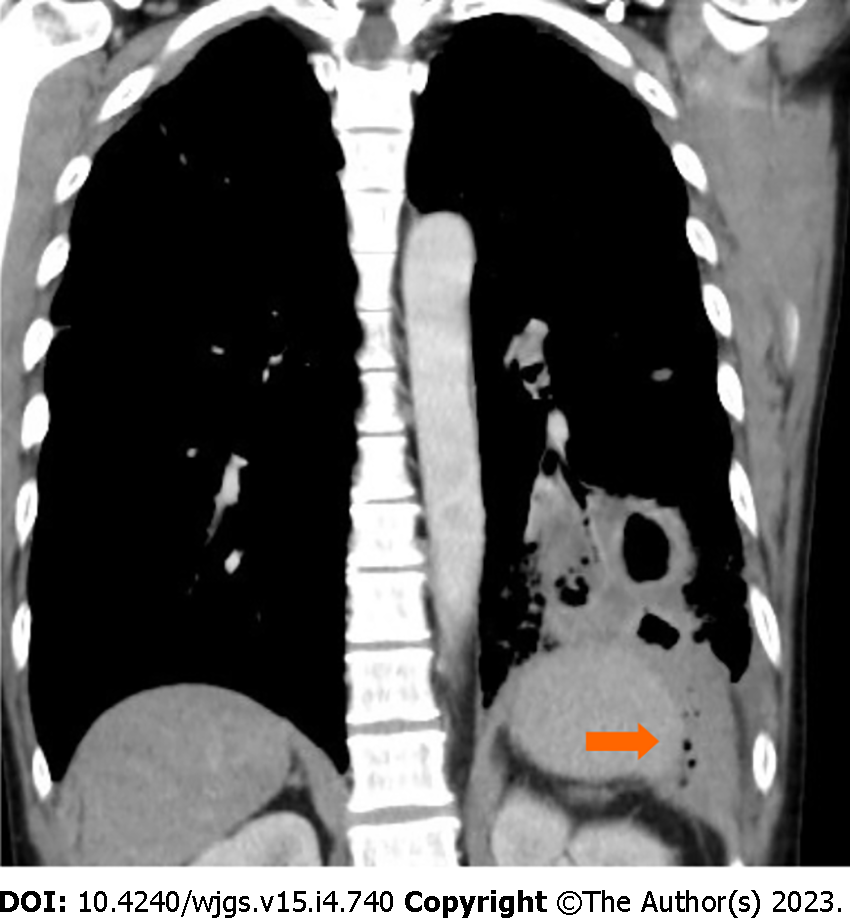
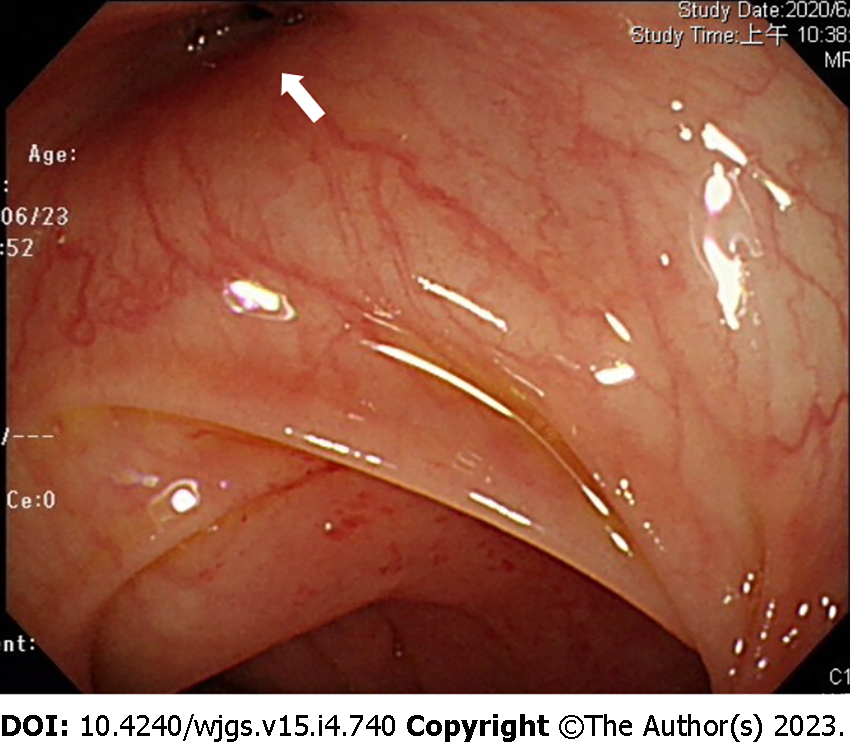
After admission to our hospital, we re-evaluated the patient’s initial chest CT, and a fistula tract was noted between the left pleural cavity and the abdomen (Figure 1). A lower gastrointestinal series with water-soluble contrast agents confirmed the diagnosis of a colopleural fistula (Figure 2). Colonoscopy revealed negative findings, except for the orifice of the fistula at the splenic flexure (Figure 3).
Idiopathic colopleural fistula was diagnosed on this patient.
We performed surgery and found dense adhesions between the splenic flexure, spleen, distal pancreas, and stomach. A diaphragm fistula, including a piece of Gerota's fascia with an internal opening was found at the splenic flexure. The patient underwent a left hemicolectomy, splenectomy, and distal pancreatectomy, and the diaphragm was repaired.
No further empyema recurrence was noted during follow-up.
Colopleural fistula with secondary empyema is an exceptionally rare condition; the rarity delays the diagnosis. Less than 20 cases of colopleural fistula have been reported in the literature. Most cases reported in the past were related to malignancies, Crohn’s disease, or iatrogenic causes[1,2,4]. Here, we report a case of colopleural fistula with an initial presentation of a cystic lesion of the lung that caused refractory empyema after surgery. The patient had no history of abdominal/thoracic surgery, and other risk factors, including malignancy, colonic diverticula, or Crohn’s disease, were excluded after clinical investigations. To our knowledge, this is the first reported case of idiopathic colopleural fistula.
According to the previously reported cases, diagnosing a colopleural fistula is challenging. The diagnosis was usually established by feculent output from chest drains[1,2,4,5], or by medical images directly revealing the fistula tract[3]. Treatment outcomes were satisfactory. Most studies reported surgical resection for the infected site of the colon, and Hayashi et al[5] reported cases treated successfully by conservative treatment after diverting colostomy was performed.
In addition to direct medical imaging findings, some clinical signs or findings may raise suspicion for a colopleural fistula diagnosis. Ibrahim et al[6] reported the Sister Leena sign, a direct relationship between the amount of pleural fluid drained and the amount of oral intake. We could not confirm this sign in this case, as we have no records regarding oral intake in this patient. Another finding that may raise suspicion of a colopleural fistula is the growth of unusual flora in the pleural fluid. In this case, the pleural fluid culture grew Escherichia coli and Bacteroides fragilis, rare organisms in the thoracic cavity but very common in the gastrointestinal tract. Imaging studies, including a lower gastrointestinal series with contrast, colonoscopy, or CT, may help confirm the diagnosis.
There is no established standard management for colopleural fistulas; however, most studies have reported surgical treatment. We performed resections, including left hemicolectomy, splenectomy, and distal pancreatectomy, and repaired the diaphragm in this patient. The patient recovered well without postoperative complications, and no recurrence of empyema was observed during the follow-up.
Coloplerual fistula is a rare condition, and its diagnosis is often challenging. Signs that may indicate a colopleural fistula include refractory empyema accompanied by colonic flora growth in the pleural fluid.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen Y, China; Meena DS, India S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Barisiae G, Krivokapiae Z, Adziae T, Pavloviae A, Popoviae M, Gojniae M. Fecopneumothorax and colopleural fistula - uncommon complications of Crohn's disease. BMC Gastroenterol. 2006;6:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Lian R, Zhang G. Empyema caused by a colopleural fistula: A case report. Medicine (Baltimore). 2017;96:e8165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Papagiannopoulos K, Gialvalis D, Dodo I, Darby MJ. Empyema resulting from a true colopleural fistula complicating a perforated sigmoid diverticulum. Ann Thorac Surg. 2004;77:324-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Grant KMK, Reid F, Crouch G, Lawrence M. Colo-pleural fistula: a rare complication of bariatric surgery. ANZ J Surg. 2020;90:905-907. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Hayashi A, Susaki Y, Ose N, Takeuchi Y, Maeda H. Colopleural fistula caused by aspergillus: an extremely rare complication after lung resection-case report. Surg Case Rep. 2016;2:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Ibrahim WH, Thomas L. Sister Leena's sign: a sign that may be useful in differentiating colopleural fistula (fecal empyema) from usual empyema. Chest. 2007;131: 1616-1617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |