Published online Feb 27, 2023. doi: 10.4240/wjgs.v15.i2.201
Peer-review started: September 9, 2022
First decision: December 26, 2022
Revised: January 11, 2023
Accepted: January 30, 2023
Article in press: January 30, 2023
Published online: February 27, 2023
Processing time: 170 Days and 19.8 Hours
In China, as the population grows older, the number of elderly people who have died from respiratory problems has increased.
To investigate whether enhanced recovery after surgery (ERAS)-based respiratory function training may help older patients who had abdominal surgery suffer fewer pulmonary problems, shorter hospital stays, and improved lung function.
The data of 231 elderly individuals having abdominal surgery was retrospectively analyzed. Based on whether ERAS-based respiratory function training was provided, patients were divided into ERAS group (n = 112) and control group (n = 119). Deep vein thrombosis (DVT), pulmonary embolism (PE), and respiratory tract infection (RTI) were the primary outcome variables. Secondary outcome variables included the Borg score Scale, FEV1/FVC and postoperative hospital stay.
The percentage of 18.75% of ERAS group participants and 34.45% of control group participants, respectively, had respiratory infections (P = 0.007). None of the individuals experienced PE or DVT. The ERAS group’s median postoperative hospital stay was 9.5 d (3-21 d) whereas the control groups was 11 d (4-18 d) (P = 0.028). The Borg score decreased on the 4th d following surgery in the ERAS group compared to the 2nd d prior (P = 0.003). The incidence of RTIs was greater in the control group than in the ERAS group among patients who spent more than 2 d in the hospital before surgery (P = 0.029).
ERAS-based respiratory function training may reduce the risk of pulmonary complications in older individuals undergoing abdominal surgery.
Core Tip: One of the major factors contributing to morbidity and mortality during the perioperative period were postoperative pulmonary complications after abdominal surgery. Clinical judgment and improved outcomes required rapid identification of high-risk individuals and intervention. We compared the pulmonary complications between the two groups using the predefined observation indicators after retrospectively analyzing the postoperative data of 231 older patients divided into two groups based on various preoperative respiratory function training methods. As compared to traditional respiratory function training techniques, enhanced recovery after surgery-based respiratory function training may reduce the probability of pulmonary complications in older patients who have undergone abdominal surgery.
- Citation: Gu YX, Wang XY, Xu MX, Qian JJ, Wang Y. Analysis of the impact of ERAS-based respiratory function training on older patients’ ability to prevent pulmonary complications after abdominal surgery. World J Gastrointest Surg 2023; 15(2): 201-210
- URL: https://www.wjgnet.com/1948-9366/full/v15/i2/201.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i2.201
The age of hospitalized patients is increasing as the rate of the aging population in our nation accelerates. Elderly people have sluggish physical reactions and a variety of basic illnesses, such as a high prevalence of chronic bronchitis, hypertension, coronary heart disease, diabetes, and cerebral infarction. According to statistics, pulmonary complications accounted for 89% of fatalities in adults over 65 who had more than one underlying condition[1]. When referring to pulmonary complications with post-operative clinical manifestations in elderly patients, such as atelectasis, pneumonia, bronchitis, respiratory insufficiency, and others, it was important to note that these complications could have a negative impact on the course of the disease[2]. The incidence of pulmonary complications following abdominal surgery in the elderly ranged from 15% to 75%, which was significantly higher than the incidence of cardiovascular complications[3]. These complications had a significant impact on postoperative recovery and were one of the major causes of perioperative death in elderly patients.
In addition to using traditional treatment approaches like anti-inflammatory medication and oxygen inhalation, elderly patients must also engage in pulmonary breathing exercises in order to decrease the incidence of postoperative pulmonary complications and improve their lung function during the perioperative period. Effective breathing exercises could assist to restore lung function as quickly as feasible and lower the risk of postoperative pulmonary infection[4]. The goal of respiratory function training is to increase the respiratory muscles’ ability to maintain tension and endurance throughout the exercise, decrease the amount of oxygen used for that exercise, and increase the efficiency as a result. Therefore, perioperative respiratory muscle training to enhance lung function can successfully enhance patients’ capacities for spontaneous breathing, expectoration, and cough, hence lowering the risk of problems and postoperative pulmonary infection[5]. This was a crucial topic that touched doctors, patients, and their families on a common level. It was also a strategy to facilitate the rapid recovery of surgical patients.
Enhanced recovery after surgery (ERAS) has abandoned many conventional perioperative therapies and the nursing model by adopting a variety of efficient methods to prevent surgical trauma produced by stress, related complications and helping postoperative patients to recover faster[6,7]. This study investigated the effect of ERAS-based respiratory function training on pulmonary complications in elderly patients undergoing abdominal surgery during the perioperative period in order to evaluate the practical application value of the training.
Two hundred and thirty-one elder patients over 65 who underwent abdominal surgery at Shanghai Fourth People’s Hospital between April 2019 and September 2021 were the subject of a retrospective data collection. Inclusion criteria: Patients who agreed to participate in the study, those who are able to talk well and are aware, those who have undergone abdominal surgery, and those who are older than 65. Exclusion criteria: Mental illness and cognitive decline, the presence of serious lung conditions before surgery, such as pulmonary infection and moderate to large pleural effusions, amalgamated thoracotomy, and the need for mechanical ventilation before surgery. The study received informed consent from the participants, and our hospital’s institutional ethics committee approved it (No. 2022108-001).
Age, sex, smoking, operation type, pulmonary function, arterial blood gas analysis, oxygen saturation, duration of surgery, and data from chest X-rays, computed tomography (CT) scans, and ultrasounds were collected as baseline information. Effective expectoration means that the patient could cough up phlegm easily; ineffective expectoration is sticky expectoration or an erroneous expectoration technique that makes it difficult for the patient to expectorate and requires the guidance and aid of medical staff. Hypoxemia was the lowest subnormal arterial blood oxygen pressure level. The following pulmonary complications could occur: Pleural effusion, atelectasis, pulmonary infection, and respiratory failure, depending on imaging results and a doctor’s clinical judgment. The anticipated endpoint events included postoperative patient deaths, postoperative discharges, and hospital stays longer than 30 d.
Main outcome measures included new or altered chest X-ray abnormalities indicative of infection as well as respiratory tract infection (RTI), which was defined as the occurrence of at least two of the following: (1) Patients receiving medications for respiratory infections; (2) white blood cells (WBC) > 12000/mL; (3) cough and expectoration; and (4) postoperative unexplained tympanic temperature > 38.0 °C (not for other infections). Any clinical or radiographic evidence of deep vein thrombosis (DVT) or pulmonary embolism (PE), such as spiral CT or ultrasound, was also included in the primary outcome measures. Secondary outcomes were subjective respiratory Borg scores from the 2nd d through the 4th d after surgery[8]. Length of postoperative hospital stay was also highlighted as a secondary outcome. We also looked at whether longer preoperative hospital stays in the case and control groups was associated with a greater incidence of respiratory infections.
The group of 11 persons included a project leader who was in charge of developing a training program to enhance respiratory function and 10 team members who were responsible for carrying out the study.
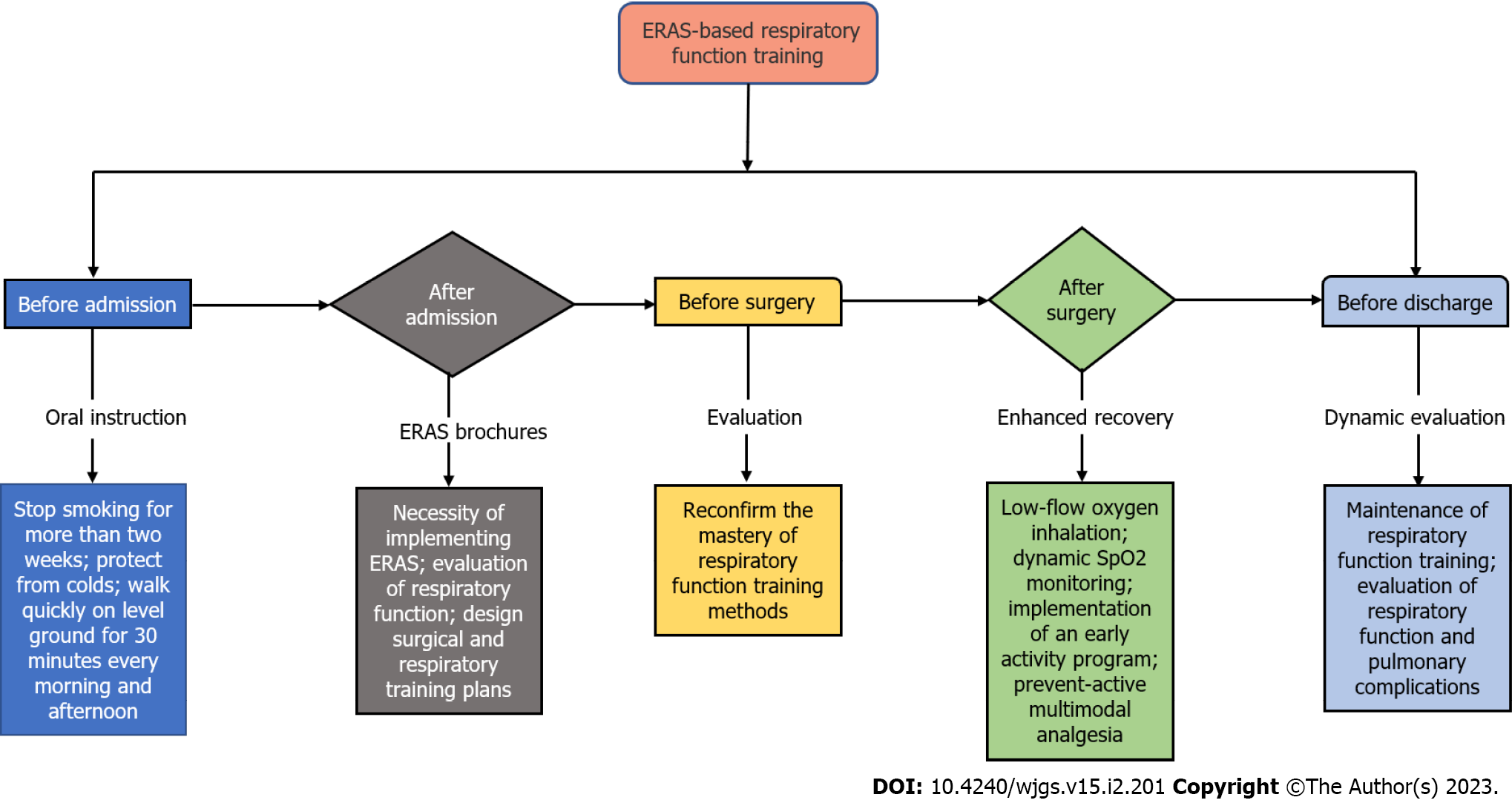
All patients in the case group had ERAS-based respiratory function training. The specific implementation strategy was described in Figure 1.
Before admission, patients should stop smoking for more than 2 wk before they arrive at the hospital, be protected from colds, and instructed to walk quickly on level ground for 30 min every morning and afternoon.
After admission, the responsible nurse would demonstrate and explain ERAS to patients, distribute ERAS brochures to help patients understand the concept, and explain the need for the steps involved in implementing ERAS. The nurse also evaluated the respiratory function associated with admission, made arrangements for patients to undergo testing for blood gas analysis, lung function, chest X-rays, or chest CTs. Together, doctors and nurses evaluated the patients designed surgical and respiratory training plans, and experienced nurses chose the most efficient respiratory training methods based on patient evaluation. The teach-back approach to health education was used to assess the patient’s competence to do breathing training correctly and independently.
Before surgery, the patient’s mastery of the respiratory function training approach was reconfirmed by the doctor and nurse.
After surgery, 1-2 L/min low-flow oxygen inhalation, dynamic oxygen saturation (SpO2) monitoring, and SpO2 94 percent maintenance were done; implemented a program for an early activity and took a semi-decubitus position (above 30 degrees) of rest; active activity steadily increases, moving from in bed to out of bed to bedside activities; program for preventative multimodal analgesia was put in place.
Before discharge, active maintenance of respiratory function training; the chest CT, arterial blood gas analysis, pulmonary function, etc. were examined based on the patient’s condition; dynamic evaluation of pulmonary complications.
Respiratory function training includes lip constriction breathing, abdominal breathing, effective coughing with wound protection, balloon blowing exercises, card education, and other techniques[9-12]. The ERAS group received the ERAS-based concept of respiratory function training in addition to the conventional respiratory function training technique, whereas the control group received the abovementioned traditional respiratory function training approach.
The statistical analysis of counting and measuring data was carried out using SPSS 23.0 statistical software (IBM, 2015, United States). Each variable’s normality was checked using the Kolmogorov-Smirnov and Shapiro-Wilk tests, and further tests were run as necessary. The age distribution of the two groups was compared using the unpaired Student’s t test. Mann-Whitney U test was used to compare the type of surgery. The ratio of male to female, smoking status, and usage of epidural analgesia were all compared between the two groups using the chi-square test. In order to compare key outcomes between the case and control groups, the Chi-square test was also applied. The primary result was compared between the ERAS group and the control group, both of which had spent more than 2 d in the hospital prior to surgery, using the Fischer precision test. Mann-Whitney U test was used to compare the length of postoperative hospital stay between the two groups (secondary outcome). On the 2nd and 4th d following surgery, the Wilcoxon rank-sum test was used to compare the Borg score. Statistics were considered significant for P values under 0.05.
Data on 231 older patients over 65 who underwent abdominal surgery at Shanghai Fourth People’s Hospital were collected from April 2019 to September 2021. There were no statistically or clinically significant differences between ERAS group and control group in terms of demographics, smoking status, American Society of Anesthesiologists (ASA) classification, types of operation, epidural analgesia, and other parameters (Table 1).
| Variable | ERAS group | Control group | P value |
| Age in yr | 72.06 ± 4.72 | 72.40 ± 4.89 | 0.59 |
| Sex as male:female | 61:51 | 55:64 | 0.21 |
| Smoking as yes:no | 45:67 | 53:66 | 0.50 |
| ASA grade | 0.22 | ||
| I | 39 (34.82%) | 50 (42.02%) | |
| II | 40 (35.71%) | 30 (25.21%) | |
| III | 33 (29.47%) | 39 (32.77%) | |
| IV | 0 (0%) | 0 (0%) | |
| Classification of surgical complexity | 0.96 | ||
| 1 | 0 (0%) | 0 (0%) | |
| 2 | 11 (9.82%) | 13 (10.92%) | |
| 3 | 72 (64.29%) | 76 (63.87%) | |
| 4 | 29 (25.89%) | 30 (25.21%) | |
| 5 | 0 (0%) | 0 (0%) | |
| Epidural analgesia | 62 | 52 | 0.08 |
In 231 patients, laparoscopic cholecystectomy and laparoscopic appendectomy accounted for approximately 43.3 percent of the cases; however, there was no obvious difference in surgery types between the ERAS group and the control group. The details of the procedure were displayed in Table 2.
| Surgery | ERAS group | Control group | P value |
| Hepatobiliary and pancreatic surgery: hepatectomy, bile duct exploration, pancreaticoduodenal surgery, etc. | 28 (25.0%) | 26 (21.85%) | 0.72 |
| Cholecystectomy: laparoscopic or open | 31 (27.68%) | 27 (22.69%) | |
| Gastric and esophageal surgery | 9 (8.03%) | 12 (10.09%) | |
| Colorectal surgery | 11 (9.82%) | 10 (8.40%) | |
| Small intestine: small bowel resection | 2 (1.79%) | 1 (0.84%) | |
| Others: hernia repair, splenectomy, appendix, etc. | 31 (27.68%) | 43 (36.13%) |
The ERAS group’s patients all participated in the ERAS-based respiratory function training, and from the second to the 4th postoperative day, Borg scale scores and vital signs were collected. Each patient in the ERAS group received standardized respiratory function training based on ERAS, and there were no negative events during or after the training. After surgery, patients’ vital signs were steady during the 2nd to 4th d (Table 3).
| Parameter | Baseline value | ERAS group | Control group | ||||
| 2 d | 3 d | 4 d | 2 d | 3 d | 4 d | ||
| Borg score median | 2 | 2 | 2 | 2 | 3 | 2 | 2 |
| Heart rate median/min | 86 | 88.5 | 81 | 78 | 84 | 81 | 79 |
| Respiratory frequency median/min | 18 | 19 | 16 | 17 | 18 | 17 | 17 |
| SaO2 median % | 95 | 96 | 97 | 92 | 96 | 97 | 92 |
The total incidence of RTI in this research was 26.84 percent. RTIs were present in 41 (34.45%) of the 119 patients in the control group and 21 (18.75%) of the 112 patients in the ERAS group. According to the findings, there was 15.7% difference between the two groups’ rates of RTIs. Respiratory function training was more successful in the ERAS group, and the frequency of RTIs was low. This difference was statistically significant (P = 0.007; Table 4) and had a 95% confidence interval of 0.239 to 0.805. DVT or PE were not present in any individuals in either group.
| Parameter | ERAS group | Control group | P value |
| Main outcome | |||
| Respiratory tract infection | 21 (18.75%) | 41 (34.45%) | 0.007 |
| New/changed X-ray findings | 48 (42.86%) | 64 (53.78%) | 0.114 |
| White blood cell more than 12 | 39 (34.82%) | 56 (47.06%) | 0.063 |
| Temperature more than 38 degree centigrade | 37 (33.04%) | 54 (45.38%) | 0.060 |
| Positive sputum bacteria | 19 (16.96%) | 31 (26.05%) | 0.111 |
| Antibiotic therapy | 22 (19.64%) | 40 (33.61%) | 0.018 |
| Secondary results | |||
| Preoperative hospitalization time more than 2 d | 59 (52.68%) | 65 (54.62%) | |
| Preoperative hospitalization time more than 2 d in patients with respiratory tract infection | 11 (9.82%) | 24 (20.17%) | 0.029 |
| The postoperative length of stay in d | 9.5 (3-21) | 11 (4-18) | 0.028 |
| FEV1/FVC more than 70% | 86 (76.79%) | 74 (62.18%) | 0.022 |
The average of Borg scores in the ERAS group showed a decline on the 4th postoperative day as compared to the 2nd postoperative day (P = 0.003, Wilcoxon rank-sum test); the average declined considerably by 1.36. The median postoperative hospital stay in the ERAS group was 9.5 d (with a range of 3-21 d), whereas it was 11 d in the control group (with a range of 4-18 d). Since the variables in the ERAS group and the control group did not follow a normal distribution, the Kolmogorov-Smirnov test was employed to compare the length of the postoperative hospital stay between the two groups. With a mean difference of 1.35 d between the two groups’ postoperative hospital stays, the ERAS group was in the hospital for shorter time than the control group. The 95 percent confidence interval for the postoperative hospital stay for both groups was 9.84-10.98. Therefore, ERAS-based respiratory function training significantly reduced the postoperative hospital stay for older patients after abdominal surgery (Mann-Whitney U test, P = 0.028).
The probability of RTI was higher in the control group (24/65, 36.9%) than in the ERAS group (11/59, 18.6%) for patients who had spent more than 2 d in the hospital before surgery (P = 0.029, Fischer’s test; Table 4). Therefore, the incidence of RTIs among patients in the two groups with preoperative hospitalization days longer than 2 d was 28.23 percent, with a range of 17.1 to 89.5 percent. Postoperative lung function tests revealed that the control group’s lungs functioned worse than those of the ERAS group (P = 0.022, Chi-square test). Epidural analgesic usage or smoking habits did not significantly differ between the two groups.
Significantly longer hospital stays and higher medical expenses were linked to an increase in pulmonary problems, postoperative morbidity, and death[13,14]. The literature has documented that pulmonary complications in individuals after abdominal surgery could raise hospital expenditures by US $31000 (US $2000 per person/year) for an 11-d stay. In all, the increase in the typical hospital stay that could be directly linked to postoperative complications was around 8 d[15]. In the ERAS group, we discovered that ERAS-based respiratory function training decreased the frequency of postoperative pulmonary problems in half. In comparison to the regular respiratory function training group, the ERAS group’s postoperative hospital stay was often shorter. The median reduction in postoperative hospital stays in the population might range from 9.84 d to 10.98 d (mean 10.41 d). Based on the concept of ERAS, patients with a longer preoperative hospital stay (case group and control group), i.e. more than 2 d, had a significantly reduced mean risk of respiratory infection if they completed respiratory function training. ERAS-based respiratory function training helped this population’s rates of respiratory infection reduce by 17.1% to 89.5% (28.2 percent on average).
According to the Borg dyspnea scale, postoperative respiratory function was also improved in the ERAS group. Patients in the ERAS group did not experience any negative side effects from respiratory exercise. Postoperative respiratory function decline was involved in the etiology of respiratory problems. These included the reduction in lung mechanics brought on by pain and the suppression of diaphragm function brought on by neuro-reflexes. Various humoral cascade systems, the metabolism of arachidonic acid, cytokines, and endothelial adhesion factors might also be involved. Additionally, standard postoperative treatment, which entailed spending hours each day laying on your back, might impair lung mechanics and oxygenation. There isn’t a single, standard method for enhancing postoperative lung function and avoiding pulmonary complications as of yet[16-18]. In order to enhance patients’ postoperative pulmonary function, we thus created a respiratory function training approach based on the concept of respiratory function training.
Comparisons with patients undergoing abdominal surgery should be done with caution since perioperative training plans in individuals receiving thoracic surgery have been proven to enhance respiratory function. In patients undergoing lung cancer resection, preoperative intervention based on moderate-to-high-intensity aerobic exercise improved lung function and reduced postoperative morbidity, whereas postoperative intervention alone did not appear to reduce respiratory complications or length of hospital stay, according to a systematic review of perioperative physiotherapy in these patients[19]. A randomized controlled trial conducted on lung cancer patients in 2014 found that high strength and endurance and strength training (60 min each time, three times a week, for 20 wk) was well tolerated and significantly improved peak oxygen uptake, muscle strength, total muscle mass, functional health, and quality of life in the intervention group 5 wk to 7 wk after surgery[20]. ERAS-based respiratory function training used in this study lasted longer than the traditional respiratory function training, had clear benefits, and might have had a significant impact on lowering postoperative respiratory complications and postoperative hospital stays.
The comprehensive study by Sullivan et al[21] found no proof that utilizing incentive spirometry might decrease pulmonary complications following upper abdominal surgery. Preoperative rehabilitation treatment and respiratory muscle training significantly decreased postoperative pulmonary problems and the length of hospital stay, according to another comprehensive evaluation of seven randomized controlled studies[22]. Due to improved lung function, ERAS-based respiratory function training could lower the incidence of postoperative respiratory illness. This was consistent with a recently published article that suggested aerobic exercise and induced spirometry might help reduce pulmonary complications following laparoscopic cholecystectomy[23]. The cause for the shorter hospital stay was unknown, although it most likely stems from a number of reasons. Long preoperative hospital stays were a well-known risk factor, and ERAS-based respiratory function training was expected to improve physiological function and shorten preoperative hospital stay.
The elderly’s increased pulmonary parenchyma fiber connective tissue causes their lung compliance, ventilation reserve, and air exchange intensity and volume to decline. Furthermore, having difficulty coughing and expectorating caused a reduction in lung and breathing capacity. Surgery, trauma, and other stresses could increase the risk that pulmonary infection, atelectasis, and other problems would develop in patients with chronic obstructive pulmonary disease who were surgical patients. The diaphragm rising during abdominal surgery, the stimulation of the intercostal nerves, and the traumatic stimulation brought on by the close proximity of the surgical site to the thoracic cavity all resulted in decreased lung compliance and decreased thoracic volume, which temporarily impaired respiratory function by causing hypoventilation and restricted ventilation dysfunction[24,25]. However, these problems of abdominal surgery were plainly solved by ERAS-based respiratory function training, which also greatly minimized the probability of postoperative pulmonary complications.
The research did have certain limitations. There was a chance of bias because there wasn’t a prospective, randomized research on patients. Since this study was retrospective, information about compliance was also difficult to get. To reduce this bias, the findings in Table 1 that there were no appreciable variations in the two groups’ demographic traits, surgical complexity, smoking status, use of epidural analgesia, and surgical techniques. Meanwhile, analgesics and antimicrobial prophylaxis were administered to all ERAS groups and control groups in accordance with the accepted protocol of medical best practices. To determine whether ERAS-based respiratory function training was superior to conventional respiratory function training in reducing postoperative pulmonary complications, additional large-scale randomized controlled, multi-center studies and physiological tests were required.
An efficient respiratory function training approach that could reduce postoperative pulmonary problems in elderly patients who had abdominal surgery was the ERAS-based respiratory function training.
Five to ten percent of surgical patients and nine to forty percent of abdominal surgery patients experienced postoperative pulmonary problems. Following abdominal surgery, postoperative pulmonary complications have been associated with a higher morbidity and fatality rates.
To determine if enhanced recovery after surgery (ERAS)-based respiratory function training was effective at preventing pulmonary complications in elderly patients after abdominal surgery.
Using ERAS-based respiratory function training to decrease pulmonary diseases in elderly patients after abdominal surgery.
Retrospective analysis was performed on the clinical information of 231 elderly individuals having abdominal surgery. According to whether patients utilized ERAS-based respiratory function training following surgery, patients were divided into ERAS group (n = 112) and control group (n = 119). The two groups’ postoperative pulmonary complications were analyzed.
The respiratory infection rate was only 18.75% following the use of ERAS-based respiratory function training which was significantly lower than that of traditional respiratory function training. The length of hospital stay was significantly shortened after using ERAS-based respiratory function training, and the rate of respiratory tract infection in patients who were hospitalized for more than 2 d before surgery was significantly decreased.
An efficient preoperative respiratory function training approach that could minimize postoperative pulmonary complications in patients having abdominal surgery was ERAS-based respiratory function training.
Elderly patients were more likely to experience postoperative pulmonary complications. Effective respiratory function training during the perioperative period could dramatically shorten hospital stays and mortality rates.
We appreciate Professor Yu Hua’s guidance, Shanghai Fourth People’s Hospital Affiliated to Tongji University School of Medicine.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): E
P-Reviewer: Aynalem A, Ethiopia; Ewers A, Austria; Gu W, China; Karna ST, India; Shomura M, Japan S-Editor: Chen YL L-Editor: Filipodia P-Editor: Chen YL
| 1. | Milucky J, Pondo T, Gregory CJ, Iuliano D, Chaves SS, McCracken J, Mansour A, Zhang Y, Aleem MA, Wolff B, Whitaker B, Whistler T, Onyango C, Lopez MR, Liu N, Rahman MZ, Shang N, Winchell J, Chittaganpitch M, Fields B, Maldonado H, Xie Z, Lindstrom S, Sturm-Ramirez K, Montgomery J, Wu KH, Van Beneden CA; Adult TAC Working Group. The epidemiology and estimated etiology of pathogens detected from the upper respiratory tract of adults with severe acute respiratory infections in multiple countries, 2014-2015. PLoS One. 2020;15:e0240309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O'Donnell M, Sullivan R, Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1080] [Cited by in RCA: 1312] [Article Influence: 131.2] [Reference Citation Analysis (0)] |
| 3. | Pantel H, Hwang J, Brams D, Schnelldorfer T, Nepomnayshy D. Effect of Incentive Spirometry on Postoperative Hypoxemia and Pulmonary Complications After Bariatric Surgery: A Randomized Clinical Trial. JAMA Surg. 2017;152:422-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Brocki BC, Andreasen J, Nielsen LR, Nekrasas V, Gorst-Rasmussen A, Westerdahl E. Short and long-term effects of supervised versus unsupervised exercise training on health-related quality of life and functional outcomes following lung cancer surgery - a randomized controlled trial. Lung Cancer. 2014;83:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Valkenet K, Trappenburg JC, Gosselink R, Sosef MN, Willms J, Rosman C, Pieters H, Scheepers JJ, de Heus SC, Reynolds JV, Guinan E, Ruurda JP, Rodrigo EH, Nafteux P, Fontaine M, Kouwenhoven EA, Kerkemeyer M, van der Peet DL, Hania SW, van Hillegersberg R, Backx FJ. Preoperative inspiratory muscle training to prevent postoperative pulmonary complications in patients undergoing esophageal resection (PREPARE study): study protocol for a randomized controlled trial. Trials. 2014;15:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Lv H, Yang N. Clinical effect of application of nursing concept of rehabilitation surgery for improvement of quality of postoperative recovery in orthopedics. J Orthop Surg Res. 2021;16:471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Wang X, Wang N, Wang X, Wei X, Ma M, Sun Y, Ren D, Liu Y, Guo Y, Wang R, Chen Y. Application value of goal-directed fluid therapy with ERAS in patients undergoing radical lung cancer surgery. Am J Transl Res. 2021;13:8186-8192. [PubMed] |
| 8. | Morishita S, Tsubaki A, Hotta K, Inoue T, Qin W, Kojima S, Fu JB, Onishi H. Face Pain Scale and Borg Scale compared to physiological parameters during cardiopulmonary exercise testing. J Sports Med Phys Fitness. 2021;61:1464-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Jiang Y, Liu F, Guo J, Sun P, Chen Z, Li J, Cai L, Zhao H, Gao P, Ding Z, Wu X. Evaluating an Intervention Program Using WeChat for Patients With Chronic Obstructive Pulmonary Disease: Randomized Controlled Trial. J Med Internet Res. 2020;22:e17089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 10. | Dehyab AS, Bakar MFA, AlOmar MK, Sabran SF. A review of medicinal plant of Middle East and North Africa (MENA) region as source in tuberculosis drug discovery. Saudi J Biol Sci. 2020;27:2457-2478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Wu J, Zhang W, Chen J, Fei H, Zhu H, Xie H. Application of and Clinical Research on Enhanced Recovery After Surgery in Perioperative Care of Patients With Supratentorial Tumors. Front Oncol. 2021;11:697699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Li J, Yang P, Fu D, Ye X, Zhang L, Chen G, Yang Y, Luo H, Chen L, Shao M, Li C, Liu Y, Zhou Y, Jiang H, Li X. Effects of home-based cardiac exercise rehabilitation with remote electrocardiogram monitoring in patients with chronic heart failure: a study protocol for a randomised controlled trial. BMJ Open. 2019;9:e023923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Katsura M, Kuriyama A, Takeshima T, Fukuhara S, Furukawa TA. Preoperative inspiratory muscle training for postoperative pulmonary complications in adults undergoing cardiac and major abdominal surgery. Cochrane Database Syst Rev. 2015;2015:CD010356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 14. | Shi Y, Yu H, Huang L, Wang S, Chi D, Chen C, Liu B. Postoperative pulmonary complications and hospital stay after lung resection surgery: A meta-analysis comparing nonintubated and intubated anesthesia. Medicine (Baltimore). 2018;97:e10596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Tefera GM, Feyisa BB, Umeta GT, Kebede TM. Predictors of prolonged length of hospital stay and in-hospital mortality among adult patients admitted at the surgical ward of Jimma University medical center, Ethiopia: prospective observational study. J Pharm Policy Pract. 2020;13:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | de Oliveira Vacchi C, Martha BA, Macagnan FE. Effect of inspiratory muscle training associated or not to physical rehabilitation in preoperative anatomic pulmonary resection: a systematic review and meta-analysis. Support Care Cancer. 2022;30:1079-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 17. | Kokotovic D, Berkfors A, Gögenur I, Ekeloef S, Burcharth J. The effect of postoperative respiratory and mobilization interventions on postoperative complications following abdominal surgery: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2021;47:975-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Paek J, Lim PC. Enhanced Recovery after Surgery (ERAS) Protocol for Early Discharge within 12 Hours after Robotic Radical Hysterectomy. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Rodriguez-Larrad A, Lascurain-Aguirrebena I, Abecia-Inchaurregui LC, Seco J. Perioperative physiotherapy in patients undergoing lung cancer resection. Interact Cardiovasc Thorac Surg. 2014;19:269-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Edvardsen E, Skjønsberg OH, Holme I, Nordsletten L, Borchsenius F, Anderssen SA. High-intensity training following lung cancer surgery: a randomised controlled trial. Thorax. 2015;70:244-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 137] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 21. | Sullivan KA, Churchill IF, Hylton DA, Hanna WC. Use of Incentive Spirometry in Adults following Cardiac, Thoracic, and Upper Abdominal Surgery to Prevent Post-Operative Pulmonary Complications: A Systematic Review and Meta-Analysis. Respiration. 2021;100:1114-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Kendall F, Oliveira J, Peleteiro B, Pinho P, Bastos PT. Inspiratory muscle training is effective to reduce postoperative pulmonary complications and length of hospital stay: a systematic review and meta-analysis. Disabil Rehabil. 2018;40:864-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 23. | El-Marakby AA, Darwiesh A, Anwar E, Mostafa A, El-Gendy SR, Gaowgzeh RA, Jad A. Aerobic Exercise Training and Incentive Spirometry Can Control Postoperative Pulmonary Complications after Laparoscopic Cholecystectomy. Mid East J Sci Res. 2013;13:459-463. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Graf R, Cinelli P, Arras M. Morbidity scoring after abdominal surgery. Lab Anim. 2016;50:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Pang Q, Liu H, Chen B, Jiang Y. Restrictive and liberal fluid administration in major abdominal surgery. Saudi Med J. 2017;38:123-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |