Published online Dec 27, 2023. doi: 10.4240/wjgs.v15.i12.2844
Peer-review started: October 23, 2023
First decision: November 8, 2023
Revised: November 17, 2023
Accepted: December 6, 2023
Article in press: December 6, 2023
Published online: December 27, 2023
Processing time: 65 Days and 9.7 Hours
Study showed that systemic holistic care not only aids in disease treatment and physical recovery to a certain extent but also effectively enhances patient psychological well-being, social support, and overall quality of life (QoL).
To assess systematic holistic care impact on the recovery and well-being of postoperative patients with colon cancer.
Our randomized controlled trial included 98 postoperative patients with colon cancer admitted to our hospital from June 2021 to June 2022. Patients were divided into control and study groups. The control group received conventional postoperative nursing care, whereas the study group received systematic holistic nursing care. We monitored gastrointestinal function recovery, and recorded changes in serum albumin (ALB), prealbumin (PA), psychological state, self-management, self-efficacy, QoL, and the occurrence of complications in patients before, at discharge, and 2 wk post-discharge. Spearman analysis assessed correlations between psychological state, self-management, self-efficacy, and QoL of patients in the study group 2 wk post-discharge.
Following the nursing intervention, we observed significantly shorter post
Systemic holistic nursing significantly benefits postoperative patients with colon cancer by promoting gastrointestinal recovery, improving post-operation well-being, reducing complications, and enhancing QoL.
Core Tip: Systemic holistic care was reported as a comprehensive approach, with a focus on their physical and mental health. This approach not only aids in disease treatment and physical recovery to a certain extent but also effectively enhances patient psychological well-being, social support, and overall quality of life. Consequently, this study employed a randomized controlled trial to investigate the effects of systemic holistic care on the overall condition of postoperative patients with colon cancer.
- Citation: Wang J, Qiao JH. Holistic conditions after colon cancer: A randomized controlled trial of systematic holistic care vs primary care. World J Gastrointest Surg 2023; 15(12): 2844-2854
- URL: https://www.wjgnet.com/1948-9366/full/v15/i12/2844.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i12.2844
In recent years, colon cancer incidence and mortality rates have risen significantly, placing it among the top five global malignancies[1]. Primary clinical treatments rely heavily on surgery, but research indicates unsatisfactory patient outcomes due to extensive surgical trauma, prolonged recovery, and limited mobility. Simultaneously, colon cancer patients undergoing surgery typically deal with a number of problems, such as physical discomfort, inadequate nourishment, bowel movements, and psychological stress, all of which have a negative impact on their ability to heal after surgery[2]. Therefore, providing nursing interventions for patients during the postoperative period is particularly crucial. The conventional nursing model currently used in clinical practice primarily targets diseases and symptoms, with a focus on disease treatment. However, during the postoperative recovery phase for patients with colon cancer, a more comprehensive approach is required, addressing not only their physical, mental, and social needs, but also factors that are not available in routine clinical care. From a nursing perspective, systemic holistic care provides a more comprehensive approach, viewing the patient as a whole, with a focus on their physical and mental health. It emphasizes personalized care and collaborative treatment[3], adhering to a “human-centered” nursing concept that integrates various nursing measures. This approach not only aids in disease treatment and physical recovery to a certain extent but also effectively enhances patient psychological well-being, social support, and overall quality of life (QoL)[4]. Although systematic holistic nursing has been applied successfully in the rehabilitation of numerous diseases[5,6], its impact on postoperative patients with colon cancer remains unexplored. Consequently, this study employed a randomized controlled trial to investigate the effects of systemic holistic care on the overall condition of postoperative patients with colon cancer. The objective is to offer more comprehensive and effective guidance for postoperative care, ultimately improving patient recovery outcomes and QoL.
General information: We conducted a randomized controlled trial involving 98 postoperative patients with colon cancer admitted to our hospital between June 2021 and June 2022, following specific inclusion and exclusion criteria. This study received approval from the Institutional Ethics Committee.
Inclusion criteria included the following: (1) Patients must meet the established diagnostic criteria for colon cancer[7], confirmed through clinicopathological examination, and have undergone laparoscopic surgical treatment at our hospital; (2) Patients must be postoperative and aged > 18 years; (3) Patients should not exhibit tumor metastasis or recurrence; (4) Patients should not have significant late complications; (5) Patients should not have severe comorbidities and must be able to tolerate nursing interventions; and (6) The study adheres to the principles of informed consent and meets the requirements of the Declaration of Helsinki[8].
Exclusion criteria included the following: (1) Patients with other malignant tumors; (2) Those with presence of impaired consciousness; (3) Those with presence of severe advanced disease; (4) Those with presence of previous significant surgical history; (5) Presence of psychiatric system diseases; (6) Those with presence of coagulopathy or immune dysfunction; and (7) Those with inability to provide complete clinical data.
Exclusion criteria included: (1) Patients with very serious illnesses that require special treatment or supervision; (2) Those with serious postoperative complications or poor postoperative recovery, unable to successfully receive systematic overall care or basic care; and (3) Those suffering from serious mental health problems.
Shedding criteria included the following: (1) The patient who voluntarily proposed to withdraw from the experiment; and (2) The patient whose follow-up work was not successfully completed after discharge from the hospital.
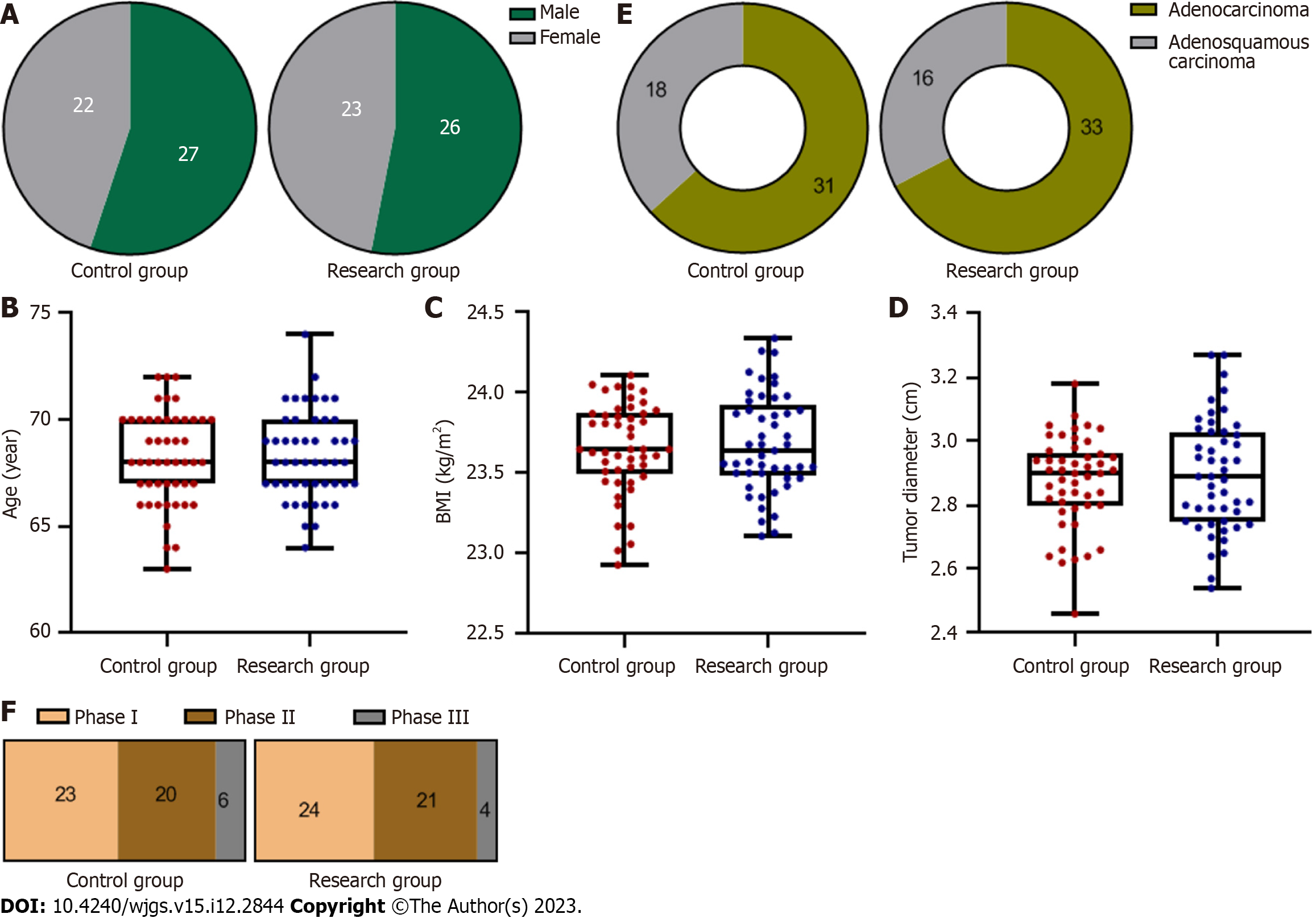
All patients were randomly divided into control group and study group by blind selection method, 49 cases in each group. Among them, the male to female sex ratio of control group was 27:22; their ages ranged from 60 to 72 years, with an average age of 68.22 ± 2.15 years. Body mass index (BMI) ranged from 20.36 to 26.15 kg/m2, with an average of 23.65 ± 0.28 kg/m2; The tumor diameter ranged from 1.57 to 3.87 cm, with an average of 2.87 ± 0.14 cm. Pathological type: Adenocarcinoma in 31 cases; adenosquamous carcinoma in 18 cases; pathological stages: Stage I 23 cases, stage II 20 cases, stage III 6 cases. The ratio of male to female in the study group was 26:23. Their ages ranged from 63 to 74 years, with a mean of 68.32 ± 2.05 years. BMI ranged from 20.40 to 26.20 kg/m2, with an average of 23.68 ± 0.31 kg/m2; The tumor diameter ranged from 1.61 to 3.90 cm, with an average of 2.90 ± 0.18 cm. Pathological type: 33 cases of adenocarcinoma; adenosquamous carcinoma in 16 cases; pathological stage: Stage I 24 cases, stage II 21 cases, stage III 4 cases. There was no significant difference in the general clinical data (Figure 1) between the two groups (P > 0.05), which provided the basis for follow-up research.
Methodology: The control group received routine postoperative nursing care for patients after surgery, including: (1) Closely monitoring changes in postoperative vital signs; (2) Managing postoperative fasting, fluid replenishment, and maintaining water-electrolyte balance; (3) Maintaining gastrointestinal decompression and observing drainage fluid properties; (4) Monitoring postoperative psychological changes and addressing adverse emotions; (5) Encouraging patients to drink more water 5-7 d after the operation to prevent urinary stones; (6) Conducting routine follow-up care for patients and providing health education; and (7) Providing post-discharge follow-up for patients.
The study group received comprehensive holistic nursing based on the control group, and it included the following components:
Nutritional care: Personalized enteral nutritional interventions were developed based on various pertinent factors, including body weight, body condition, body fat rate, basal metabolic rate, and other body composition and biochemical indices. These interventions were tailored to specific patient condition, nutritional status, and gastrointestinal tolerance; personalized enteral nutritional interventions were formulated in accordance with individual patient situation. At the same time, the nutritional intervention was carried out within 24 h after the operation, and the multidimensional carbonic hydration preparation was pumped in by the jejunal fluid bladder tube at a pumping speed of approximately 25 mL/L, which was gradually increased to 50 mL/L, and the amount pumped each time was ≤ 350 mL. For patients who did not have any special conditions, 450 mL of short peptide-type total nutritional preparation was infused for 24 h after the operation, and the speed was controlled at 65 mL/L. In patients without special conditions, a short peptide-type total nutritional preparation was infused at a rate of 65 mL/L. At 48 h after the operation, the enteral nutrition solution can be adjusted to the whole protein type, and at the same time, the concentration of the nutrition solution can be gradually increased according to patient tolerance. The total amount pumped in a day for each patient should be ≤ 1200 mL, and the speed can be controlled at approximately 100-150 mL/L. After patient gastrointestinal function has recovered, the total amount pumped per day should be ≤ 350 mL. After patient gastrointestinal function recovery, the patient was instructed to have a light, easy-to-digest semi-liquid diet and gradually transition to general food; at the same time, according to the actual situation of the patient, vitamins, proteins, and other nutrients were added appropriately.
Infection care: It included postoperative hygiene and health education for patients, while observing the occurrence of edema and exudate in the infected wounds of patients. If exudate occurred, we then immediately used saline to clean up and informed the attending physician to change the medication to avoid aggravation of the infection.
Bleeding care: Following the surgery, patient bleeding was closely monitored, and at the same time, the patient was instructed not to get out of bed or exercise greatly to avoid compression of the wound. Meanwhile, when the wound bleeds, a bandage or cotton ball was used to stop bleeding in time. Patients with intra-abdominal bleeding were treated with hemostatic drugs according to physician instructions, and surgical hemostasis was performed if necessary.
Drainage tube care: We ensured that the drainage tube left in the patient after surgery was smooth, while adjusting the position of the drainage tape to avoid infection caused by reflux of drainage fluid. We observed the amount of drainage and the color of the drainage fluid and reported it to the doctor when any abnormality was found.
Psychological care: We conducted a comprehensive assessment of the situation of a patient, understood their cultural background and personality, and formulated personalized psychological interventions. We patiently listened to their complaints and took targeted measures to address the issues causing their distress. When a patient exhibited psychological or physical improvement, we provided timely recognition and appropriate rewards. We also shared examples of successful cases and provided updates on the progress and feasibility of their treatment. We distributed nursing manuals created by the department to patients, encouraged them to actively study the relevant knowledge in these manuals, and motivated them to take an active role in their rehabilitation treatment, thereby enhancing their self-management abilities.
Exercise nursing: After patient physical tolerance had recovered, they were encouraged to perform simple activities; mainly focusing on bed activities in the early stages and then gradually increasing the amount of exercise and helped them get out of bed.
Discharge nursing: When patients were discharged from the hospital, we explained to them the importance of post-discharge care and simultaneously invited them to join the department WeChat chat group; introduced them to the relevant knowledge of the disease in the form of video pictures and encouraged them to share the problems they encounter in the group. Health education was provided to patient families to help them establish a correct attitude toward the disease and to guide patients to establish a positive and optimistic attitude toward treatment. We informed family members that at least one person will accompany the patient after discharge and provided timely counselling to improve the bad mood of the patients. Nursing interventions were carried out for 1 wk in both groups, whereas patients were followed up for 2 consecutive weeks after discharge from the hospital.
Observation indicators and evaluation methods: Recovery of gastrointestinal function: The recovery times of bowel sounds, anal defecation time, and defecation time of the two groups of patients after surgery were recorded.
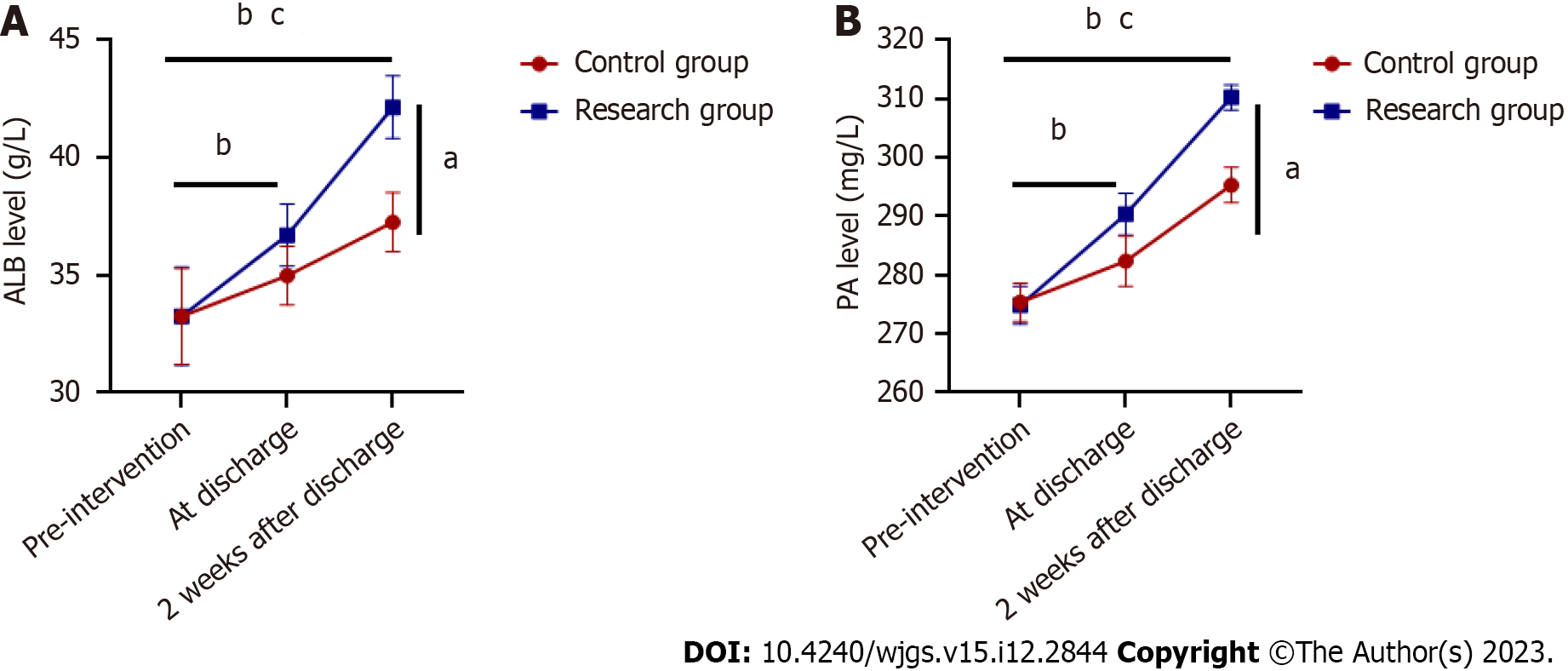
Biochemical indices: Peripheral venous blood (3 mL) was collected from patients on the 1st d after surgery, before discharge, and 2 wk after discharge, and serum albumin (ALB) and prealbumin (PA) levels were measured after centrifugation.
Psychological status: The psychological status of patients in both groups was assessed using the Hamilton Depression Scale (HAMD)[9] and Hamilton Anxiety Scale (HAMA)[10] before surgery, at the time of discharge from the hospital, and 2 wk after surgery. Among them, the HAMD included a total of 24 items, with total scores ranging from 0 to 76; the HAMA scale had a total of 14 items, with total scores ranging from 0 to 56. Patient anxiety and depression states were positively related to their scores.
Self-management and self-efficacy: Patient self-management ability and self-efficacy were assessed before the postoperative nursing intervention at the time of discharge and 2 wk after discharge using the Self-Management Scale (PIH)[11] and General Self-Efficacy Scale (GSES)[12], respectively. The PIH scale consists of three dimensions with a total score of 88, and lower the score, the better was the management ability; the GSES consists of 10 dimensions with a total score of 10-40, and its score is positively proportional to self-efficacy.
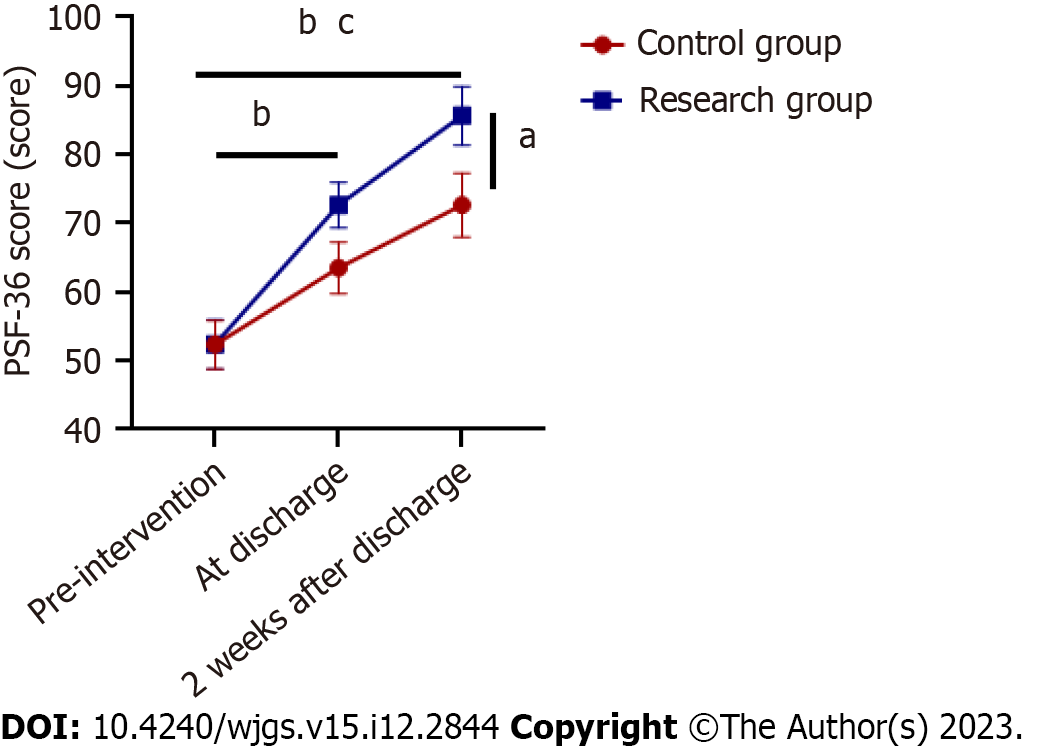
QoL The Brief Health Measurement Scale (SF-36)[13] was used to evaluate the QoL of patients before and after care. The scale has four dimensions: Social functioning, mental health, physical functioning, and somatic pain. The maximum total score for each dimension was 100. Higher scores on this scale indicate a higher QoL for patients. Complications the incidence of complications in both groups was determined from the postoperative period to the end of follow-up.
The obtained research data were analyzed using SPSS21.0, GraphPad Prism software, and P < 0.05 was taken as the test standard if not specifically required. Spearman analysis was also used to analyze the correlation between the psychological state, self-management, self-efficacy, and QoL of patients in the study group 2 wk after discharge. Differences were considered statistically significant at P < 0.05.
After nursing intervention, the postoperative bowel sound recovery time, anal exhaust time and defecation time of the two groups of patients were observed. It was found that the recovery of gastrointestinal function of the research group are significantly shorter than that of the control group, and the difference was significant (P < 0.05), as shown in Figure 2.
The ALB and PA levels of the patients at the time of discharge as well as 2 wk after discharge were significantly improved compared with the pre-intervention period, and at the same time the improvement was more pronounced in the study group, and the difference was significant, P < 0.05, as shown in Figure 3.
Patient HAM-A and HAM-D scores at discharge and 2 wk after discharge were significantly lower than those before the intervention, while the improvement in the psychological state was more obvious in the study group, and the difference was significant (P < 0.05), as shown in Figure 4.
Patient PIH and GSES scores at discharge and 2 wk after discharge were significantly improved compared with pre-intervention, while the improvement was more prominent in the study group, and the difference was significant, P < 0.05, as shown in Figure 5.
Before the intervention, the difference in QoL between the two groups was not significant (P > 0.05). After the nursing intervention, patient QoL scores at the time of discharge as well as 2 wk after discharge were significantly improved. The improvement effect of the study group was significantly better than that of the control group, with a significant difference of P < 0.05, as shown in Figure 6.
After the intervention, patients in both groups still experienced different degrees of complications, but the complication rate was significantly lower in the study group than the control group (3/49, 6.12%); the difference was significant (P < 0.05). The results are shown in Figure 7.
Using correlation analysis, it was found that anxiety, depression scores, self-management scores, and QoL scores of the patients in the study group were significantly negatively correlated 2 wk after discharge (r = -0.273, -0.522, -0.344, P < 0.01); whereas the self-efficacy scores of the patients were positively correlated with the QoL scores 2 wk after discharge (r = 0.410, P = 0.000). The results are shown in Figure 8.
Colon cancer is a prevalent malignant tumor, often requiring surgery as a primary treatment. However, postoperative recovery and management pose substantial challenges for patients, including a heightened risk of complications. These issues not only impact their physical health and nutritional intake but also have adverse effects on their psychological well-being and overall QoL, thereby potentially impeding the recovery process. To address these challenges, systemic holistic care has been proposed and applied to enhance the postoperative condition of patients. The goal of systemic holistic care is to support patient rehabilitation through a multifaceted approach that takes into account social, psychological, and physical factors[14]. Despite the demonstrated effectiveness of systemic holistic care in clinical practice, there remains a for concrete evidence supporting its practical application and effectiveness in postoperative patients with colon cancer. Therefore, our study sought to compare the impact of systematic holistic care with traditional primary care on the overall condition of postoperative patients with colon cancer through a randomized controlled trial, yielding promising results.
Our study found that, following nursing intervention, the study group exhibited significantly shorter recovery times for bowel sounds, anal defecation, and defecation than the control group. This suggests that systematic holistic nursing care can, to a certain extent, expedite the recovery of gastrointestinal function in postoperative patients with colon cancer. This could be attributed to the fact that systematic holistic nursing care assesses the nutritional status of patients, providing personalized nutritional interventions, and dietary advice, thereby aiding patients in selecting the appropriate foods to meet their nutritional requirements and promoting rapid recovery. Additionally, when the study group received nursing care, we saw a significant improvement in their levels of PA and ALB, and these changes continued for two weeks after the group was discharged. This implies that systematic holistic nursing care can influence the biochemical functions of patients with colon cancer, sustaining this effect throughout their hospitalization. ALB and PA serve as vital indicators of patient nutritional status, and the emphasis of holistic nursing care on nutritional guidance and appropriate nutritional intake ensures that patients receive adequate protein, vitamins, minerals, and other essential nutrients, maintaining normal ALB and PA levels[15,16]. Additionally, the holistic care system provides patients with nursing manuals, encouraging them to take an active role in their health education, which contributes to heightened health awareness and the maintenance of optimal nutritional levels. Furthermore, our study also examined changes in patient psychological states. The results showed that patients in the study group experiencing significantly lower levels of anxiety and depression, and their psychological states continued to improve after hospital discharge, suggesting that systematic holistic care effectively enhances patient psychological state and has a lasting impact. This positive effect can be attributed to the comprehensive assessment of patients and the formulation of personalized psychological interventions within the holistic nursing care system. Patients are actively encouraged to address adverse emotions during their nursing care, fostering a positive psychological state[17]. Moreover, upon discharge, the provision of psychological intervention and guidance to the family members of the patients creates a supportive environment that helps patients and their families adopt a positive and optimistic attitude towards treatment, further improving patient emotional well-being.
Additionally, we assessed the self-management and self-efficacy of the patients. We found that, at the time of discharge and 2 wk after discharge, the self-management ability and self-efficacy of the patients in the study group were significantly better than those in the control group. This demonstrated that holistic systemic care effectively enhances patient self-management ability and self-efficacy following colorectal cancer surgery. This improvement stems from the disease-related health education and guidance provided by holistic systemic care. Patients gain a better understanding of their condition, the recovery process, and the importance of self-management ability. Systemic holistic care also prioritizes psychological well-being. During the recovery process, nursing staff offer personalized emotional support and psychological counselling to assess and alleviate psychological pressure, establishing a positive emotional state. This motivates patients to actively manage their health[18]. Furthermore, we observed a significant improvement in the QoL scores of patients in the study group following nursing intervention. This suggests that systematic holistic care can improve the QoL for patients with colon cancer post-surgery. The care includes lifestyle guidance, such as dietary adjustments and exercise recommendations, which help patients manage their habits and reduce the impact of adverse behaviors on their health, thus effectively enhancing overall QoL[19]. Systematic holistic care also provides comprehensive rehabilitation interventions[20]. Nutritional care, exercise, and other rehabilitation measures help restore patient physical functions, increase physical strength, and improve endurance. Psychological support can effectively reduce anxiety and psychological pressure while increasing social support. This along with social support after discharge, enhances social adaptability and, to a certain extent, patient QoL[21]. In this study, we observed the occurrence of postoperative complications in patients with colon cancer and found that the incidence of complications in the study group was significantly lower. This suggests that systemic holistic care can effectively prevent postoperative complications. The primary reason is that systemic holistic nursing involves comprehensive monitoring and assessment of patients in the postoperative stage, including vital signs, pain levels, and wound conditions. Timely monitoring and interventions, such as pain management, infection control, bleeding prevention, and proper drain care, effectively mitigate the risk of complications. Furthermore, in this study, we examined the relationship between patient psychological state, self-management ability, self-efficacy, and QoL in the study group 2 wk following hospital discharge. We discovered that patient anxiety and depression scores, as well as their self-management ability scores, were negatively correlated with their QoL scores. Conversely, patient self-efficacy was positively correlated with their QoL. This finding further demonstrates that systematic and holistic nursing care can enhance patient psychological state, self-management ability, self-efficacy, and overall QoL. These results emphasize that systemic holistic care can improve patient QoL to a certain extent by enhancing their psychological states, self-management abilities, and self-efficacy.
However, there are still some limitations and deficiencies in this study, such as: (1) Although this study used a randomized controlled design, due to the limited sample size, randomization may result in baseline differences between the two groups, which may affect the final comparison results. Therefore, it is still necessary to expand the sample size for observation in the later stage; (2) Most of the observation indicators are scale questionnaires, patients have strong subjective awareness, and there are differences in subjective judgment between different evaluators, which may affect the accuracy and reliability of the results, and cannot fully reflect the improvement of the overall situation of patients after surgery. Therefore, comprehensive and objective indicators should be selected to evaluate the impact of systemic overall nursing on patients in the later stage; and (3) The relative short follow-up duration in this study may not fully capture the long-term effects of systemic holistic care on post-colon cancer surgery recovery, given that the overall improvement after colon cancer surgery typically requires a significant amount of time. Thus, there remains a need for longer-term observations to comprehensively assess these long-term effects.
In summary, the application of systemic holistic nursing in postoperative patients with colon cancer has a significant positive impact. It not only promotes gastrointestinal function recovery but also contributes to overall postoperative well-being, reducing complications and improving patient QoL.
Colon cancer surgery is a common treatment. However, patients often need to face many difficulties after surgery, including postoperative pain, nutritional support during recovery, mental and emotional adjustment, and the prevention of complications. Traditional basic care mainly focuses on postoperative wound healing and monitoring of complications, while systemic holistic care may consider the patient’s physical and mental health more comprehensively, including psychosocial support, nutrition and exercise guidance, pain management, etc. By conducting a randomized controlled trial study of these two types of care, the impact of systematic holistic care on patients after colon cancer surgery can be more objectively assessed. Such a study has a positive significance for improving the quality of postoperative care for colon cancer patients and promoting the rehabilitation of patients.
Bowel cancer surgery is a major trauma and patients face many physical and psychological challenges after surgery. Traditional basic nursing focuses on wound management and complication prevention after surgery, but neglects the overall physical and mental needs of patients. Systematic holistic care is more comprehensive, focusing on patient nutrition, pain management, psychological support and other aspects, can more comprehensively meet the needs of patients. However, there are still few reports about the application of systematic holistic care in postoperative patients with colon cancer.
In addition to the physical recovery of patients after colon cancer surgery, their mental state and quality of life (QoL) are also very important. Therefore, this study evaluated the effect of systematic holistic care in promoting patient recovery by comparing the impact of systematic holistic care and basic care on postoperative patients with colon cancer.
In order to analyze the differences between systematic holistic care and basic care in the care of patients with colon cancer after surgery, 98 patients with colon cancer after surgery admitted to our hospital from June 2021 to June 2022 were selected as research objects in this clinical trial, and a randomized controlled trial was carried out.
Through this study, it can be found that the application of systematic holistic nursing in patients with colon cancer surgery has a significant effect, which can not only promote the recovery of gastrointestinal function of patients, but also adjust the overall status of patients after surgery to a certain extent, reduce the occurrence of complications in patients, and thus improve the QoL of patients. The successful implementation of this study is expected to provide new ideas for the exploration of nursing models, and it will also help improve the quality of rehabilitation of patients with colon cancer after surgery.
In the study, we found that systematic holistic care can significantly improve the recovery process in patients after colon cancer surgery and has a positive impact on psychosocial support and QoL. Through this study, we propose a new theory of personalized care intervention strategies and describe in detail the details of systematic holistic care, while also developing a personalized systematic holistic care plan for patients after colon cancer surgery.
Based on research evidence, the medical community and strategies for the care and rehabilitation of patients after colon cancer surgery are updated and adjusted to better meet the needs of patients and improve the quality of recovery. At the same time, the successful implementation of this study can also lay a foundation for the standardization of systematic holistic nursing model, so as to further develop specific implementation guidelines for systematic holistic nursing, train medical staff to improve their implementation capabilities, and establish related quality assessment and improvement mechanisms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cekici Y, Turkey; Kaya BC, Turkey S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Fabregas JC, Ramnaraign B, George TJ. Clinical Updates for Colon Cancer Care in 2022. Clin Colorectal Cancer. 2022;21:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 74] [Reference Citation Analysis (1)] |
| 2. | Verkuijl SJ, Jonker JE, Trzpis M, Burgerhof JGM, Broens PMA, Furnée EJB. Functional outcomes of surgery for colon cancer: A systematic review and meta-analysis. Eur J Surg Oncol. 2021;47:960-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Mandal L, Seethalakshmi A, Rajendrababu A. Rationing of nursing care, a deviation from holistic nursing: A systematic review. Nurs Philos. 2020;21:e12257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 4. | Wang KR. [Application of systematic holistic nursing in perioperative care of laparoscopic radical gastric cancer surgery]. Health Care Medicine Research and Practice. 2022;19:5. |
| 5. | Si YF. [Effect observation of systematic holistic nursing for patients with reflux gastritis]. Kang Yi. 2021;16:109. |
| 6. | Weng ML. [Application of systematic holistic nursing care in patients with severe pneumonia combined with heart failure]. Xinxueguanbing Fangzhi Zhishi. 2022;19:36-38. |
| 7. | Benson AB, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF, Garrido-Laguna I, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Meyerhardt J, Miller ED, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wuthrick E, Gregory KM, Freedman-Cass DA. NCCN Guidelines Insights: Colon Cancer, Version 2.2018. J Natl Compr Canc Netw. 2018;16:359-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 635] [Cited by in RCA: 685] [Article Influence: 97.9] [Reference Citation Analysis (1)] |
| 8. | Meng XD. [The reference of 2013 Helsinki Declaration to informed consent in China]. Med Philosophy. 2014;15:37-39. |
| 9. | Li WB. [Clinical application of 6-item Hamilton Depression Scale]. Chinese J Neuropsychiatric Disorders. 2007;33:119-120. |
| 10. | Thompson E. Hamilton Rating Scale for Anxiety (HAM-A). Occup Med (Lond). 2015;65:601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 302] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 11. | Smith D, Harvey P, Lawn S, Harris M, Battersby M. Measuring chronic condition self-management in an Australian community: factor structure of the revised Partners in Health (PIH) scale. Qual Life Res. 2017;26:149-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005;139:439-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 772] [Cited by in RCA: 822] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 13. | Newnham EA, Harwood KE, Page AC. Evaluating the clinical significance of responses by psychiatric inpatients to the mental health subscales of the SF-36. J Affect Disord. 2007;98:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Yao XL. [Application effect of systematic holistic nursing based on nursing procedure in intravenous thrombolytic therapy of patients with acute pulmonary embolism in ICU]. Capital Food Med. 2019;26:191-192. |
| 15. | Ge DY. [Analysis of the impact of holistic nursing applied to diabetic haemodialysis patients on their nutritional status and quality of life]. Diabetes New World. 2020;23:2. |
| 16. | Liu L. [Effects of 3H standardized nursing mode on nutritional status, immune function and psychological status of lung cancer patients after radiotherapy]. Hebei Med. 2019;42:1581-1584. |
| 17. | Xin YL. [The effect of holistic nursing management concept used to improve the depressive state of depressed patients]. China Health Industry. 2020;17:12-14. |
| 18. | Li YZ. [Effects of systematic holistic care on psychiatric symptoms and self-efficacy of chronic schizophrenia patients]. J Qiqihar Medical College. 2021;42:3. |
| 19. | Chen J. [Effect of systematic holistic nursing on postoperative traumatic oedema and quality of life in patients with perianal abscess]. Electronic J Clinical General Surg. 2023;11:54-56+60. |
| 20. | Yue BG. [Exploration of systematic holistic nursing care]. Chinese J Hospital Management. 1997;2:27-28. |