Published online Dec 27, 2023. doi: 10.4240/wjgs.v15.i12.2747
Peer-review started: September 29, 2023
First decision: November 1, 2023
Revised: November 1, 2023
Accepted: December 1, 2023
Article in press: December 1, 2023
Published online: December 27, 2023
Processing time: 88 Days and 15.3 Hours
Hajibandeh index (HI), derived from combined levels of C-reactive protein, lactate, neutrophils, lymphocytes and albumin, is a modern predictor of peritoneal contamination and mortality in patients with acute abdominal pathology.
To validate the performance of HI in predicting the presence and nature of peritoneal contamination in patients with acute abdominal pathology in a larger cohort study and to synthesis evidence in a systematic review and meta-analysis.
The STROBE guidelines and the PRISMA statement standards were followed to conduct a cohort study (ChiCTR2200056183) and a meta-analysis (CRD420
A total of 1437 patients were included (700 from the cohort study and 737 from the literature search). ROC curve analysis of the cohort study showed that the AUC of HI for presence of contamination, purulent contamination and feculent contamination were 0.79 [95% confidence interval (CI): 0.76-0.82, P < 0.0001], 0.76 (95%CI: 0.72-0.80, P < 0.0001), and 0.83 (95%CI: 0.79-0.86, P < 0.0001), respectively. The meta-analysis showed that the pooled AUC of HI for presence of contamination, purulent contamination and feculent contamination were 0.79 (95%CI: 0.75-0.83), 0.78 (95%CI: 0.74-0.81), and 0.80 (95%CI: 0.77-0.83), respectively.
The HI is a strong and accurate predictor of intraperitoneal contamination. Although the available evidence is robust, it is limited to the studies conducted by our evidence synthesis group. We encourage other researchers to validate performance of HI in predicting the presence of intraperitoneal contamination and more importantly in predicting mortality following emergency laparotomy.
Core Tip: Hajibandeh index (HI), derived from combined levels of C-reactive protein, lactate, neutrophils, lymphocytes and albumin, can strongly predict presence and nature of peritoneal contamination in acute abdomen. The evidence is robust but limited to studies by our evidence synthesis group, hence we encourage other researchers to validate performance of HI in predicting the presence of intraperitoneal contamination and more importantly in predicting mortality following emergency laparotomy.
- Citation: Hajibandeh S, Hajibandeh S, Evans L, Miller B, Waterman J, Ahmad SJ, Hale J, Higgi A, Johnson B, Pearce D, Helmy AH, Naguib N, Maw A. Predictive value of Hajibandeh index in determining peritoneal contamination in acute abdomen: A cohort study and meta-analysis. World J Gastrointest Surg 2023; 15(12): 2747-2756
- URL: https://www.wjgnet.com/1948-9366/full/v15/i12/2747.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i12.2747
Presence of intraperitoneal contamination is considered as an important predictor of morbidity and mortality in patients with acute abdominal pathology[1]. Due to its prognostic significance, the presence of intraperitoneal contamination is taken into account by the commonly used prognostic scoring tools to predict the risk of postoperative morbidity and mortality in patients undergoing emergency operation for acute abdominal pathology[2,3]. Therefore, early detection of intraperitoneal contamination not only could facilitate the decision to operate in patients with acute abdominal pathology but also could potentially lead to more accurate preoperative risk assessment and more appropriate management decisions.
The knowledge about the presence of intraperitoneal contamination is only available intraoperatively; this would limit the predictive value of preoperative prognostic scoring tools. We developed the Hajibandeh index (HI) in order to be able to predict the presence and nature of intraperitoneal contamination in patients with acute abdominal pathology[4,5]. The HI includes C-reactive protein (CRP), neutrophils and lactate as nominators (their levels increase in abdominal sepsis) and albumin and lymphocytes as denominators (their levels decrease in abdominal sepsis)[4,5]. We previously demonstrated that it can predict the presence of intraperitoneal contamination in patients with acute abdominal pathology and postoperative mortality in patients undergoing emergency laparotomy[4,5]. A recent emergency laparotomy mortality risk predictor model, called HAS, includes the HI as one of its components as it remained in the model after a very strict multivariable analysis[6,7].
In this study we aimed to conduct a cohort study to validate the predictive significance of the HI in a larger cohort of patients and to conduct a systematic review and meta-analysis to determine the pooled accuracy of HI in predicting the presence and nature of intraperitoneal contamination.
The STROBE guidelines for observational studies and the PRISMA statement standards were followed to protocol, conduct and present this retrospective cohort study and systematic review, respectively[8,9]. The cohort study was registered in Chinese Clinical Trial Registry (Registration number: ChiCTR2200056183) and the systematic review was registered in PROSPERO (Registration number: CRD42022306018). The study was conducted in accordance with institutions’ policies and internal arrangements approved by local Clinical Governance Unit. Considering the nature of this study, patient consent and approval by Research Ethics Committees were not needed.
Cohort study: Consecutive adult patients undergoing emergency laparotomy in a General Surgery centre in the South Wales between January 2014 and January 2021 were included. The indications for emergency laparotomy included visceral perforation, intraabdominal sepsis of any source (anastomotic leak, colitis, intestinal fistula), intraabdominal collection, intestinal ischaemia, large bowel obstruction, small bowel obstruction, and intraabdominal bleeding. The patients who had laparotomy due to trauma were excluded. The included population in this study did not comprise the patients who underwent laparoscopic procedure. Moreover, patients without available preoperative levels of CRP, neutrophils, lactate, lymphocytes or albumin and those with haematological malignancy resulting in chronic elevated neutrophils or lymphocytes levels were excluded.
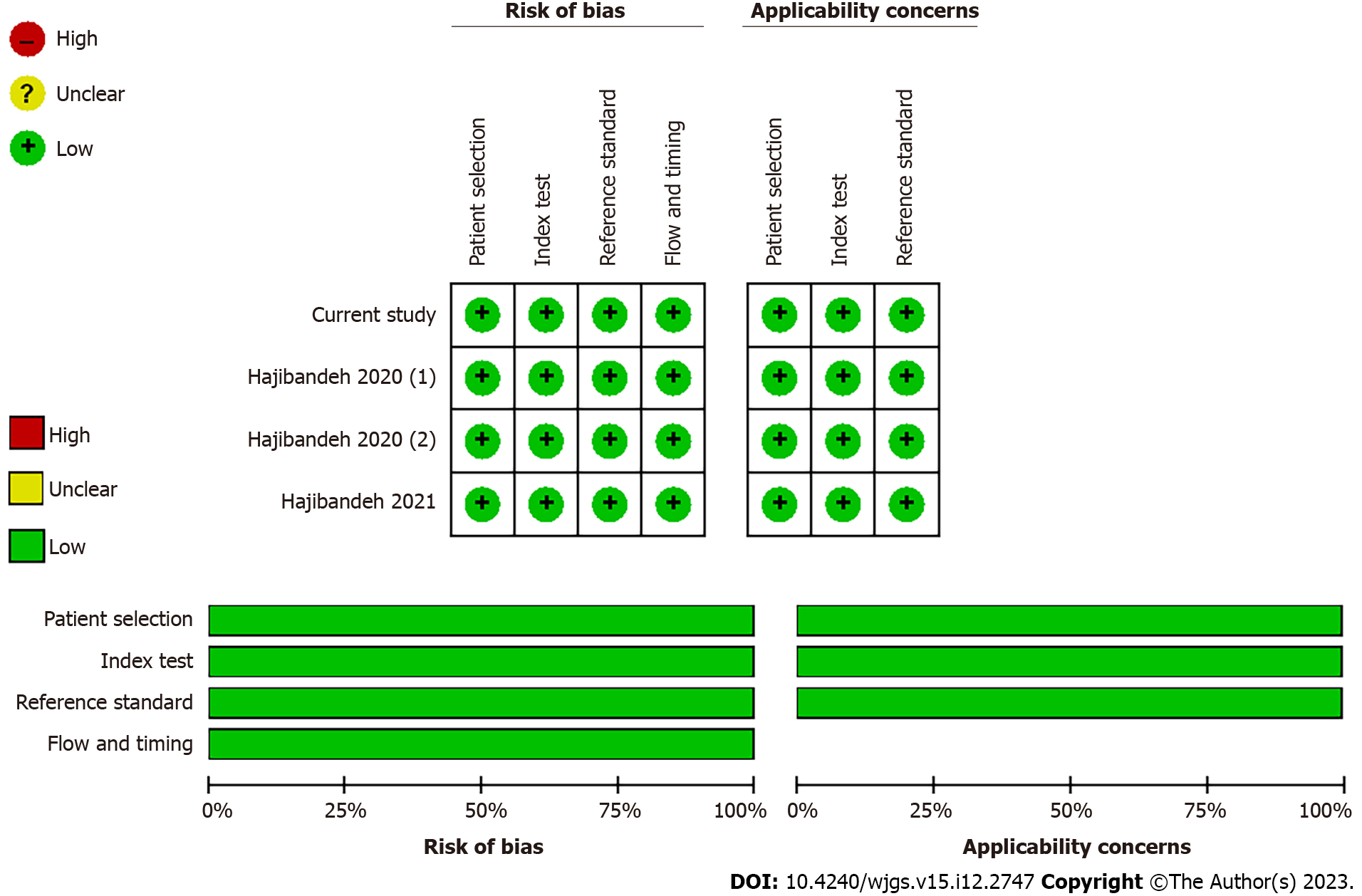
Meta-analysis: Search of electronic databases including CENTRAL, MEDLINE, EMBASE, CINAHL, and Scopus were performed to identify all retrospective or prospective observational studies evaluating accuracy of HI in predicting the presence of intraperitoneal contamination in patients with acute abdominal pathology. Appropriate keywords, thesaurus headings, search limits and operators were used to develop a comprehensive search strategy as shown in Supplementary material. The search strategy had no language restrictions and was last applied on 12 April 2023. Moreover, the reference lists of relevant reviews and articles were screened for more potentially eligible studies. The titles and abstracts of the articles identified through application of the above search strategy were screened, the full-texts of relevant articles were retrieved and the studies that met the eligibility criteria were selected. The methodological quality of the included studies were evaluated using the Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) criteria. The Review manager 5.4.1 software was used for constructing the risk of bias graphs. The above steps were performed by two independent authors and disagreements between the first two authors were resolved by involving a separate third author.
The HI for each patient was calculated based on the formula shown in Supplementary material.
Intraperitoneal contamination (presence and nature) were considered as the outcome measures. Intraperitoneal contamination was classified as serous, purulent, or feculent based on intraoperative finding of operating surgeon.
All steps of data collection were performed by two independent authors and an independent third author was consulted in the event of disagreement. The authors who were involved in data collection were not involved in data analyses. We collected information on age, sex, American Society of Anesthesiologists (ASA) status, components of the HI, nature of intraperitoneal contamination, indication for laparotomy, and procedure performed.
Cohort study: The MedCalc 13.0 software was used for statistical analyses. The demographics, clinical characteristics and outcome data were presented using simple descriptive statistics. Data were summarized with mean ± SD or median and interquartile range (IQR) for continuous variables, and frequencies/percentages for categorical variables. Receiver operating characteristic (ROC) curve analysis was conducted to evaluate the discrimination of the HI by calculating the area under the curve (AUC)[10]. Binary logistic regression was used to evaluate classification of HI; the observed and predicted values for peritoneal contamination were cross-classified to construct classification table. All statistical tests were two-tailed and statistical significance was assumed at P < 0.05.
Meta-analysis: The weighted summary AUC under the fixed and random effects modelling was calculated using the methods described by Zhou et al[11]. The unit of analysis was an individual patient. The heterogeneity was quantified and reported as I2 using Cochran Q test (χ2). I2 was interpreted as 0%-50% means low heterogeneity, 50%-75% means moderate heterogeneity, and 75%-100% means high heterogeneity. The results were reported in a forest plot with 95% confidence intervals (CIs).
A total of 1437 patients were eligible for inclusion; 700 patients from the cohort study and 737 patients from the literature search. Figure 1 demonstrates the study flow chart.
The outcomes of methodological quality assessment based on the QUADAS-2 criteria are shown in Figure 2. In summary, the included studies, including the current study, were judged to be of low risk of bias in terms of patient selection, index test, reference standard, and flow and timing.
Cohort study: Among the included population, 37% (261/700) were male and 63% (439/700) were female with mean age of 63 years (95%CI: 62-65). In terms of ASA status, 5% (35/700) were classified as ASA 1; 35% (245/700) as ASA 2; 39% (273/700) as ASA 3; 19% (131/700) as ASA 4; 2% (16/700) as ASA 5. Emergency laparotomy was performed due to colonic perforation in 16% (110/700), small bowel perforation in 6% (43/700), perforated peptic ulcer in 5% (34/700), large bowel obstruction in 11% (81/700), small bowel obstruction in 39% (270/700), colitis in 4% (26/700), intestinal ischaemia in 8% (54/700), anastomotic leak in 4% (28/700), intraabdominal collection in 4% (31/700), and other indications in 3% (23/700). Intraperitoneal contamination was present in 32% (222/700) patients; 18% (126/700) had purulent contamination and 14% (96/700) had feculent contamination. The median preoperative HI was 19.01 (IQR: 3.89-87.28) (Table 1).
| Current study | Hajibandeh 2021 | Hajibandeh 2020 | Hajibandeh 2020 | Meta-analysis | |
| Country | United Kingdom | United Kingdom | United Kingdom | United Kingdom | United Kingdom |
| Journal | - | Int J Colorectal Dis | J Perioper Pract | J Perioper Pract | - |
| Design | Retrospective cohort | Prospective cohort | Retrospective cohort | Retrospective cohort | Meta-analysis |
| Number of patients | 700 | 269 | 234 | 234 | 1437 |
| Description of included patients | Patients undergoing emergency laparotomy | Patients undergoing emergency laparotomy | Patients undergoing emergency laparotomy | Patients undergoing emergency laparotomy | Patients undergoing emergency laparotomy |
| Age, mean (95%CI) | 63 (62-65) | 64 (62-66) | 60.2 (58-62) | 62(60-65) | 63 (62-64) |
| Male, n (%) | 261 out of 700 (37%) | 123 out of 269 (46%) | 100 out of 234 (43%) | 106 out of 234 (45%) | 590 out of 1437 (41%) |
| Female, n (%) | 439 out of 700 (63%) | 146 out of 269 (54%) | 134 out of 234 (57%) | 128 out of 234 (55%) | 847 out of 1437 (59%) |
| ASA, n (%) | |||||
| 1 | 35 out of 700 (5%) | 9 out of 269 (3%) | 23 out of 234 (10%) | 33 out of 234 (14%) | 100 out of 1437 (7%) |
| 2 | 245 out of 700 (35%) | 54 out of 269 (20%) | 85 out of 234 (36%) | 76 out of 234 (33%) | 460 out of 1437 (32%) |
| 3 | 273 out of 700 (39%) | 158 out of 269 (59%) | 94 out of 234 (40%) | 78 out of 234 (33%) | 603 out of 1437 (42%) |
| 4 | 131 out of 700 (19%) | 43 out of 269 (16%) | 30 out of 234 (13%) | 40 out of 234 (17%) | 244 out of 1437 (17%) |
| 5 | 16 out of 700 (2%) | 5 out of 269 (2%) | 2 out of 234 (1%) | 7 out of 234 (3%) | 30 out of 1437 (2%) |
| Indication for laparotomy, n (%) | |||||
| Small bowel obstruction | 270 out of 700 (39%) | 94 out of 269 (35%) | 88 out of 234 (38%) | 84 out of 234 (36%) | 536 out of 1437 (37%) |
| Large bowel obstruction | 81 out of 700 (11%) | 34 out of 269 (13%) | 39 out of 234 (17%) | 28 out of 234 (12%) | 182 out of 1437 (13%) |
| Perforated peptic ulcer | 34 out of 700 (5%) | 27 out of 269 (10%) | 23 out of 234 (10%) | 28 out of 234 (12%) | 112 out of 1437 (8%) |
| Small bowel perforation | 43 out of 700 (6%) | 10 out of 269 (4%) | 14 out of 234 (6%) | 11 out of 234 (5%) | 78 out of 1437 (5%) |
| Colonic perforation | 110 out of 700 (16%) | 47 out of 269 (17%) | 36 out of 234 (15%) | 42 out of 234 (18%) | 235 out of 1437 (16%) |
| Intestinal ischaemia | 54 out of 700 (8%) | 25 out of 269 (9%) | 5 out of 234 (2%) | 8 out of 234 (3%) | 92 out of 1437 (6%) |
| Intraabdominal collection | 31 out of 700 (4%) | 4 out of 269 (2%) | 12 out of 234 (5%) | 18 out of 234 (8%) | 65 out of 1437 (5%) |
| Colitis | 26 out of 700 (4%) | 5 out of 269 (2%) | 0 out of 234 (0%) | 2 out of 234 (1%) | 33 out of 1437 (2%) |
| Anastomotic leak | 28 out of 700 (4%) | 3 out of 269 (1%) | 4 out of 234 (2%) | 4 out of 234 (2%) | 39 out of 1437 (3%) |
| Other | 23 out of 700 (3%) | 20 out of 269 (7%) | 13 out of 234 (5%) | 9 out of 234 (3%) | 65 out of 1437 (5%) |
| Intraperitoneal contamination, n (%) | 222 out of 700 (32%) | 67 out of 269 (25%) | 72 out of 234 (31%) | 62 out of 234 (27%) | 423 out of 1437 (29%) |
| Purulent contamination, n (%) | 126 out of 700 (18%) | 17 out of 269 (6%) | 44 out of 234 (19%) | 32 out of 234 (14%) | 219 out of 1437 (15%) |
| Feculent contamination, n (%) | 96 out of 700 (14%) | 50 out of 269 (19%) | 28 out of 234 (12%) | 30 out of 234 (13%) | 204 out of 1437 (14%) |
| Preoperative HI, median (IQR) | 19.01 (3.89-87.28) | 25.2 (4.5–121.1) | 23.3 (3.6–130.4) | 32.2 (4.9–144.3) | 21.3 (4.2-117.9) |
Meta-analysis: Among the included population, 41% (590/1437) were male and 59% (847/1437) were female with mean age 63 years (95%CI: 62-64). In terms of ASA status, 7% (100/1437) were classified as ASA 1; 32% (460/1437) as ASA 2; 42% (603/1437) as ASA 3; 17% (244/1437) as ASA 4; 2% (30/1437) as ASA 5. Emergency laparotomy was performed due to colonic perforation in 16 % (235/1437), small bowel perforation in 5 % (78/1437), perforated peptic ulcer in 8% (112/1437), large bowel obstruction in 13% (182/1437), small bowel obstruction in 37% (536/1437) patients, colitis in 2% (33/1437), intestinal ischaemia in 6% (92/1437), anastomotic leak in 3% (39/1437), intraabdominal collection in 5% (65/1437), and other indications in 5% (65/1437). Intraperitoneal contamination was present in 29% (423/1437) patients; 15% (219/1437) had purulent contamination and 14% (204/1437) had feculent contamination. The median preoperative HI was 21.3 (IQR: 4.2-117.9).
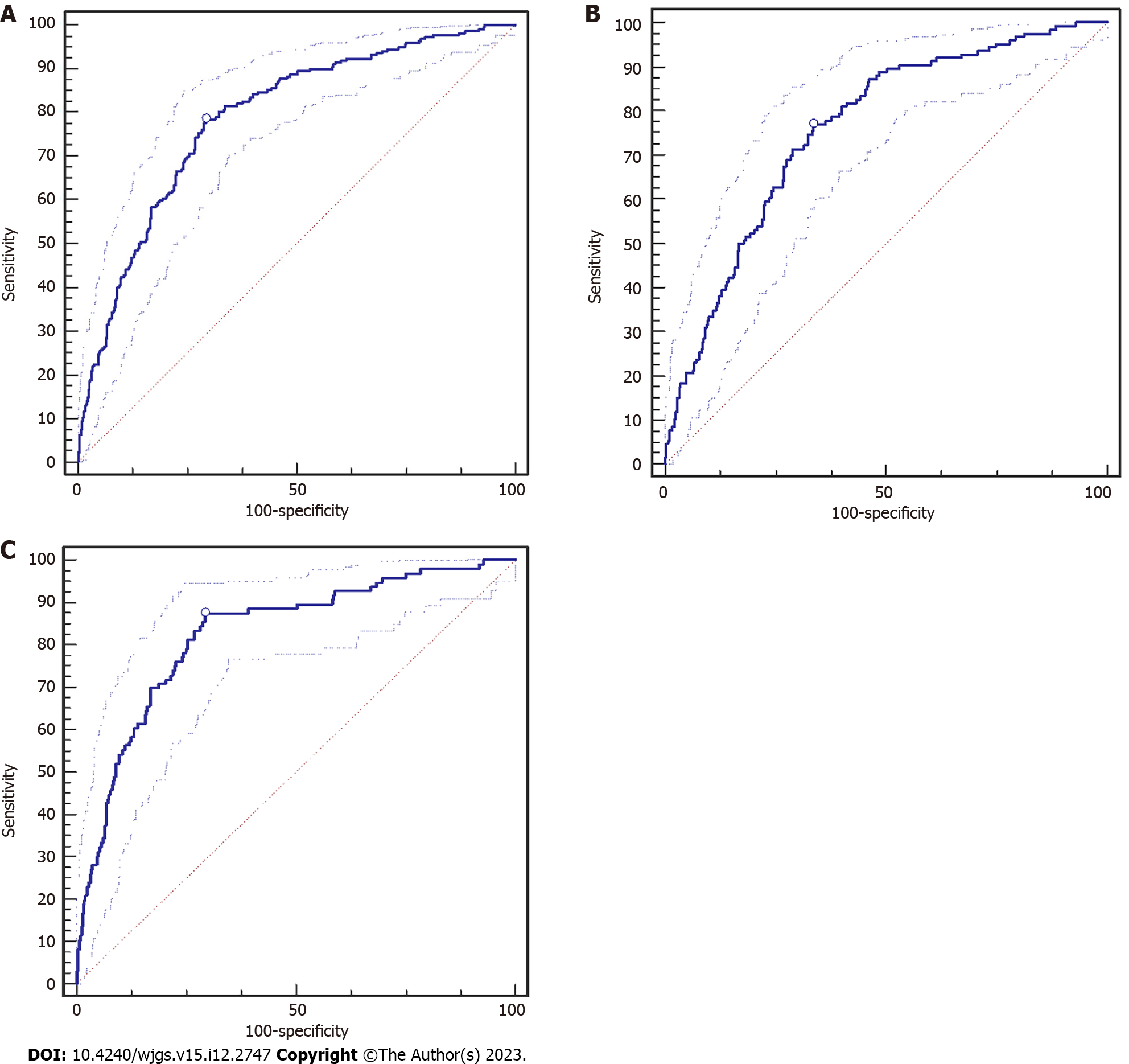
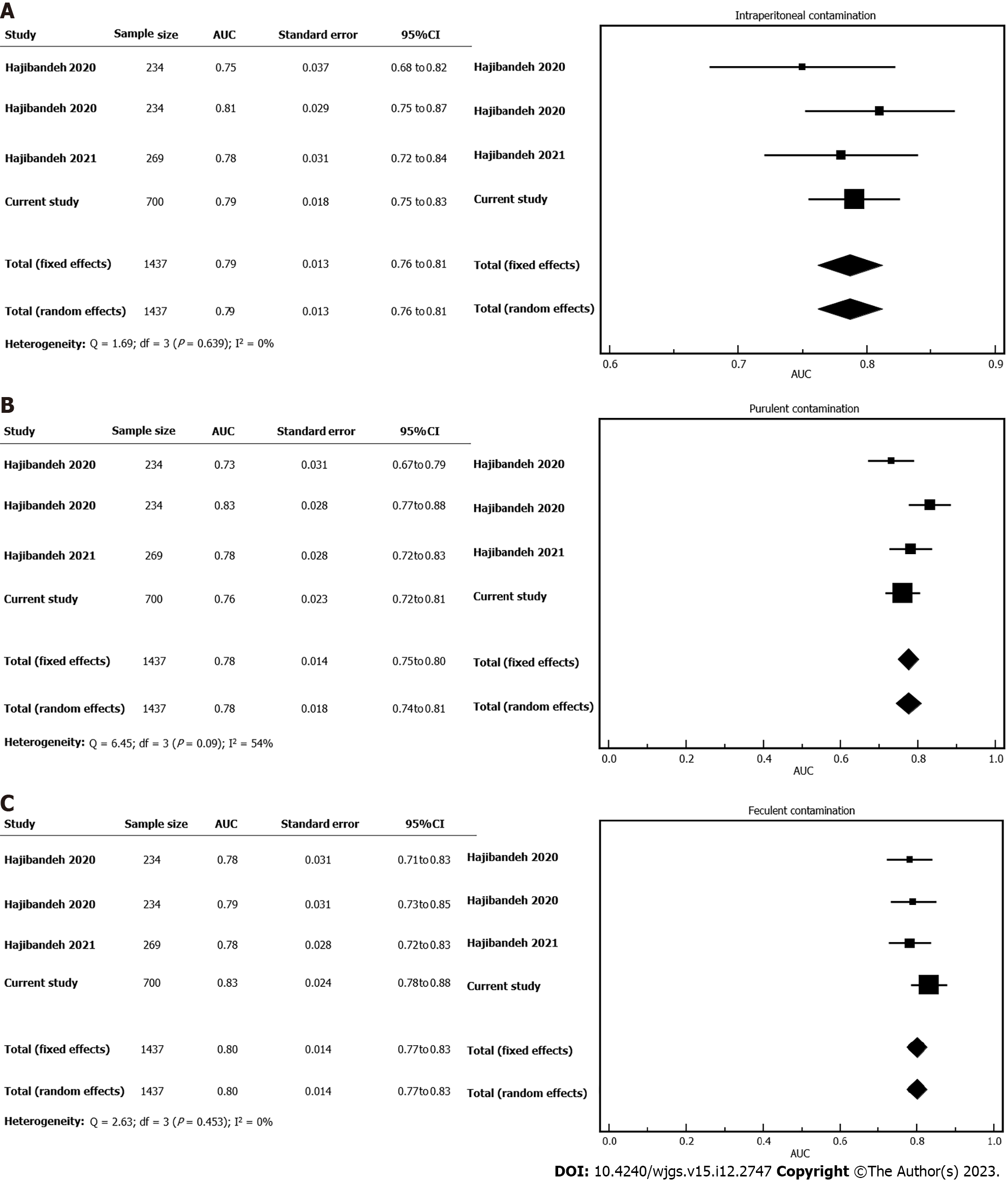
The AUC for HI was 0.79 (95%CI: 0.76-0.82, P < 0.0001) based on ROC curve analysis (Figure 3A). Analysis of classification table showed that HI classified 72% of cases correctly. Meta-analysis of 1437 patients from 4 cohorts of patients showed that the pooled AUC of HI for presence of any peritoneal contamination was 0.79 (95%CI: 0.75-0.83). The heterogeneity was judged to be low (I2 = 0%, P = 0.639) (Figure 4A).
Purulent contamination: Based on ROC curve analysis, the AUC for HI was 0.76 (95%CI: 0.72-0.80, P < 0.0001) (Figure 3B). Analysis of classification table showed that HI classified 80% of cases correctly. Meta-analysis of 1437 patients from 4 cohorts of patients showed that the pooled AUC of HI for purulent contamination was 0.78 (95%CI: 0.74-0.81). The heterogeneity was judged to be moderate (I2 = 54%, P = 0.09) (Figure 4B).
Feculent contamination: Based on ROC curve analysis, the AUC for HI was 0.83 (95%CI: 0.79-0.86, P < 0.0001) (Figure 3C). Analysis of classification table showed that HI classified 84% of cases correctly. Meta-analysis of 1437 patients from 4 cohorts of patients showed that the pooled AUC of HI for feculent contamination was 0.80 (95%CI: 0.77-0.83). The heterogeneity was judged to be low (I2 = 0%, P = 0.453) (Figure 4C).
We conducted a cohort study and a systematic review with meta-analysis to validate the accuracy of HI in predicting the presence and nature of intraperitoneal contamination in patients with acute abdominal pathology. Analysis of 1437 patients showed that the HI is strong and relatively accurate predictor of purulent and feculent intraperitoneal contamination in patients with acute abdominal pathology. The clinical and statistical heterogeneity among the included studies were low and the quality of the available evidence was judged to be high as indicated by low risks of bias in terms of patient selection, index test, reference standard, and flow and timing.
The HI is a novel index which was first developed in 2020. Due to its novelty, the predictive value of HI has only been assessed by our previous studies[4,5]. Although this may induce potential publication bias and may affect the generalisability of the findings, the consistency of our findings within different centres and different populations may reflect the robustness of our results. In fact, we have evaluated the predictive value of HI in patients with acute abdominal pain presenting to different centres in North West of England, North Wales, and South Wales. In doing so, the HI has consistently demonstrated very good predictive value in detection of intraperitoneal contamination in all centres.
The presence of intraperitoneal contamination in patients with acute abdominal pathology has a significant prognostic value and is taken into account for predicting postoperative mortality and morbidity by several prognostic tools including the Portsmouth-Physiological and Operative Severity Score for the enumeration of Mortality and morbidity (P-POSSUM)[2], the National Emergency Laparotomy Audit (NELA) model[3], and the Mannheim peritonitis index (MPI)[12]. However, as mentioned earlier, the knowledge about presence of intraperitoneal contamination is only available intraoperatively which would limit the predictive value of prognostic scoring tools such as P-POSSUM, NELA, and MPI. The HI is the only available index that predicts the presence of peritoneal contamination before performing an operation; this could potentially improve the accuracy of the aforementioned prognostic tools and inform decision-making more objectively.
The good performance of HI in predicting presence of intraperitoneal contamination can be easily explained. Peritoneal contamination, tissue necrosis, or intestinal ischaemia is associated with elevated levels of lactate, neutrophil, and CRP (nominator of HI) and decreased levels of lymphocyte and albumin (denominator of HI)[4,5], hence the more severe the underlying sepsis due to abdominal pathology, the higher the HI. In our previous study, we showed that HI can also predict the risk of mortality following emergency laparotomy[4,6]. Based on the available evidence, sepsis and septic shock are major predictors of mortality[13]. Therefore, high HI due to underlying sepsis can potentially be a predictor of postoperative mortality[6]. We believe that HI may be even better predictor of mortality than being a predictor of intraperitoneal contamination. The main rationale for this is the fact that in presence of intraabdominal tissue ischaemia which is associated with high mortality, the levels of neutrophil, lactate, and CRP would increase significantly resulting in a high HI without evidence of intraperitoneal contamination. In such scenario, the HI could falsely predict presence of intraperitoneal contamination while it would predict the mortality correctly.
The HI has a potential to be included in preoperative mortality risk assessment tools as recently shown in a predictive model called HAS[6]. The HAS model includes HI, ASA status, and sarcopenia as its components and is the first model with excellent discrimination (AUC: 0.96), calibration, and classification in predicting mortality after emergency laparotomy[6]. It uses HI to take into account the severity of abdominal pathology and it uses ASA status and sarcopenia to take into account the physical status of the patient in terms of co-morbidities, frailty, and physiological reserve[6].
The systematic and objective methodology, adequate statistical power, similar baseline characteristics of the included studies and populations, and low risks of bias within the included studies support the internal validity of the results. Nevertheless, this study is associated with some limitations. The included studies have been performed by our team; this may induce potential publication bias and may affect the generalisability of the findings. Considering the fact the number of included studies was less than 10, we could not formally assess the risk of publication bias. Selection bias cannot be excluded due to retrospective design of the study. In order to minimise the risk of selection bias, we recruited two independent authors for data collection, we separated the authors involved in data collection from the authors conducted data analyses, and we performed appropriate subgroup analyses.
The HI is a strong and accurate predictor of the presence and nature of intraperitoneal contamination in patients with acute abdominal pathology. Although the available evidence is robust, it is limited to the studies conducted by our evidence synthesis group. We encourage other researchers to validate performance of HI in predicting the presence of intraperitoneal contamination and more importantly in predicting mortality following emergency laparotomy.
Intraperitoneal contamination leads to increase in levels of C-reactive protein (CRP), lactate, neutrophils and lead to decrease in levels of lymphocytes and albumin. Hajibandeh index (HI), which includes CRP, neutrophils and lactate as nominators and albumin and lymphocytes as denominators, has been developed to predict peritoneal contamination and postoperative mortality in patients with acute abdominal pathology.
Presence of intraperitoneal contamination is an important predictor of morbidity and mortality in patients with acute abdominal pathology and it is taken into account by preoperative prognostic scoring tools. Therefore, early detection of intraperitoneal contamination is very important.
The objective of the study was to validate accuracy of HI in predicting the presence and nature of peritoneal contamination in patients with acute abdominal pathology.
The STROBE guidelines and the PRISMA statement standards were followed to conduct a cohort study and a meta-analysis, respectively. The accuracy of the HI was evaluated using receiver operating characteristic curve analysis in the cohort study and using weighted summary area under the curve (AUC) under the fixed and random effects modelling in the meta-analysis.
Analysis of 1437 patients showed that HI can accurately predict the presence of peritoneal contamination in patients with acute abdominal pathology (AUC: 0.79, 95% confidence interval: 0.75-0.83).
The HI is a strong and accurate predictor of intraperitoneal contamination in patients with acute abdominal pathology.
HI is an objectively derived index from basic biomarkers and is worth attention for inclusion in emergency laparotomy preoperative risk assessment tools. It is a strong predictor of intraperitoneal contamination and postoperative mortality. The available evidence is robust but is limited to the studies conducted by our evidence synthesis group. The predictive performance of HI needs to be externally validated by other researchers.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: de Moraes JB, Brazil; Fabbri N, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Yu HG
| 1. | Ross JT, Matthay MA, Harris HW. Secondary peritonitis: principles of diagnosis and intervention. BMJ. 2018;361:k1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (1)] |
| 2. | Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ. POSSUM and Portsmouth POSSUM for predicting mortality. Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity. Br J Surg. 1998;85:1217-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 508] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 3. | Eugene N, Oliver CM, Bassett MG, Poulton TE, Kuryba A, Johnston C, Anderson ID, Moonesinghe SR, Grocott MP, Murray DM, Cromwell DA, Walker K; NELA collaboration. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: the National Emergency Laparotomy Audit risk model. Br J Anaesth. 2018;121:739-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 4. | Hajibandeh S, Shah J, Hajibandeh S, Murali S, Stephanos M, Ibrahim S, Asqalan A, Mithany R, Wickramasekara N, Mansour M. Intraperitoneal contamination index (Hajibandeh index) predicts nature of peritoneal contamination and risk of postoperative mortality in patients with acute abdominal pathology: a prospective multicentre cohort study. Int J Colorectal Dis. 2021;36:1023-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Hajibandeh S, Hajibandeh S, Hobbs N, Shah J, Harris M, Watton L, Huq Z, Dalmia S, Malik S, Mansour M. A validated novel preoperative index to predict the extent of intraperitoneal contamination in patients with acute abdominal pathology: A cohort study. J Perioper Pract. 2020;30:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Hajibandeh S, Hajibandeh S, Hughes I, Mitra K, Puthiyakunnel Saji A, Clayton A, Alessandri G, Duncan T, Cornish J, Morris C, O'Reilly D, Kumar N. Development and Validation of HAS (Hajibandeh Index, ASA Status, Sarcopenia) - A Novel Model for Predicting Mortality after Emergency Laparotomy. Ann Surg. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 13.0] [Reference Citation Analysis (2)] |
| 7. | HAS Emergency Laparotomy Mortality Risk Calculator. [cited 20 May 2023]. Available from: https://app.airrange.io/#/element/xr3b_E6yLor9R2c8KXViSAeOSK. |
| 8. | Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP. A protocol for the development of the STROCSS guideline: Strengthening the Reporting of Cohort Studies in Surgery. Int J Surg Protoc. 2017;5:15-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13343] [Article Influence: 833.9] [Reference Citation Analysis (0)] |
| 10. | DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13220] [Cited by in RCA: 13268] [Article Influence: 358.6] [Reference Citation Analysis (0)] |
| 11. | Zhou XH, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine. New York: Wiley, 2011. |
| 12. | Wacha H, Linder MM, Feldman U, Wesch G, Gundlach E, Steifensand RA. Mannheim peritonitis index - prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theoretical Surg. 1987;1:169-177. |
| 13. | Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311:1308-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1297] [Article Influence: 117.9] [Reference Citation Analysis (0)] |