Published online Nov 27, 2023. doi: 10.4240/wjgs.v15.i11.2657
Peer-review started: August 20, 2023
First decision: September 4, 2023
Revised: September 14, 2023
Accepted: September 27, 2023
Article in press: September 27, 2023
Published online: November 27, 2023
Processing time: 98 Days and 17.9 Hours
The inflammatory myofibroblastic tumor (IMT) is a rare mesenquimal tumor of doubtful biological behaviour. It’s characterised for affecting mainly children and young adults, although it can appear at any age, being the lungs the primary affected organ (in children it represents 20% of all primary pulmonary tumors).
We present the case of a 45 year old woman, with a computed tomography (CT) finding of injury on the anterior surface of the fundus/gastric body and a solid perigastric injury of 12 mm in the ecoendoscopy. The case is presented in the tumor committee deciding to perform a laparoscopic wedge resection. The histological diagnosis was a IMT. The diagnosis is based on imaging tests like the abdominal CT, abdominal ecography and the ecoendoscopy but to confirm the diagnosis a pathological study is necessary.
Due to the unpredictable nature of this tumor, surgical resection is the best therapeutic option.
Core Tip: The inflammatory myofibroblastic tumor is a rare mesenquimal tumor of doubtful biological behaviour. It’s characterised for affecting mainly children and young adults, although it can appear at any age, being the lungs the primary affected organ. The unusual thing about the case is the gastric location of the tumor (the majority are pulmonary) and the unpredictable nature of this tumor. That is why the surgical resection is the best therapeutic option.
- Citation: Fernandez Rodriguez M, Artuñedo Pe PJ, Callejas Diaz A, Silvestre Egea G, Grillo Marín C, Iglesias Garcia E, Lucena de La Poza JL. Gastric inflammatory myofibroblastic tumor, a rare mesenchymal neoplasm: A case report. World J Gastrointest Surg 2023; 15(11): 2657-2662
- URL: https://www.wjgnet.com/1948-9366/full/v15/i11/2657.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i11.2657
The inflammatory myofibroblastic tumor (IMT) is a rare mesenquimal tumor of doubtful biological behaviour[1]. Previously known as inflammatory pseudotumor, plasmatic cell granulome, inflammatory miofibroblastoma and inflammatory miofibrohistiocityc proliferation, it’s characterised for affecting mainly children and young adults, although it can appear at any age, being the lungs the primary affected organ (in children it represents 20% of all primary pulmonary tumors)[2].
We present the case of a 45 year old woman who requested a follow-up in our center for a second opinión after discovery of injuries that could relate to a peritoneal carcinomatosis in other center.
She was examined in another center given her clinic of difuse abdominal pain of long evolution without association with any other clinical manifestation, identifying in a computed tomography (CT) a “nodular isodense image, at omental level, adyacent to the anterior right abdominal wall, without discarding infiltration of the anterior right abdominal rectum. Increase in density and trabeculation of the mesenteric fat and inespecific micronodular images, findings which could relate to a peritoneal carcinomatosis”.
She has a history of venous insuficiency and cronic gastritis, cesarean and adenoidectomy. She denied family history of malignant tumours.
On physical examination, the vital signs were as follows: Body temperature, 36.8°C; blood pressure, 121/70 mmHg; heart rate, 89 beats per min; respiratory rate: 17 breaths per min. Furthermore, the patient did not have abdominal pain, but minimal ascitites in flanks was found.
Levels of serum tumour markers were normal [carcinoembryonic antigen < 0.5 ng/mL (0.0-3.0), carbohydrate antigen (CA) 125 14.0 U/mL (0.0-35.0), CA 19-9 5.0 U/mL (0.0-40.0), CA 15-3 14.9 U/mL (0.0-28.0)]. No abnormality was found in routine blood analyses.
A gastroscopy is requested evidencing a gastric submucous injury of 1 cm in lesser curvature and a biopsy is performed. The anatomopatological diagnosis was superficial cronic gastritis not observing an intestinal metaplasia.
Subsequently, a positron emission tomography CT is performed with the following results: “Decrease in the size of the nodular image in greater omentum, with a mild affinity for FDG. Improvement of the ascitis and the trabeculation of the omental and mesenteric fat. Hepatic injury without metabolic translation”.
A core needle biopsy is performed of the omental injury observing fibrous tissue with no tumoral infiltration and tumor markers are requested, which come out negative.
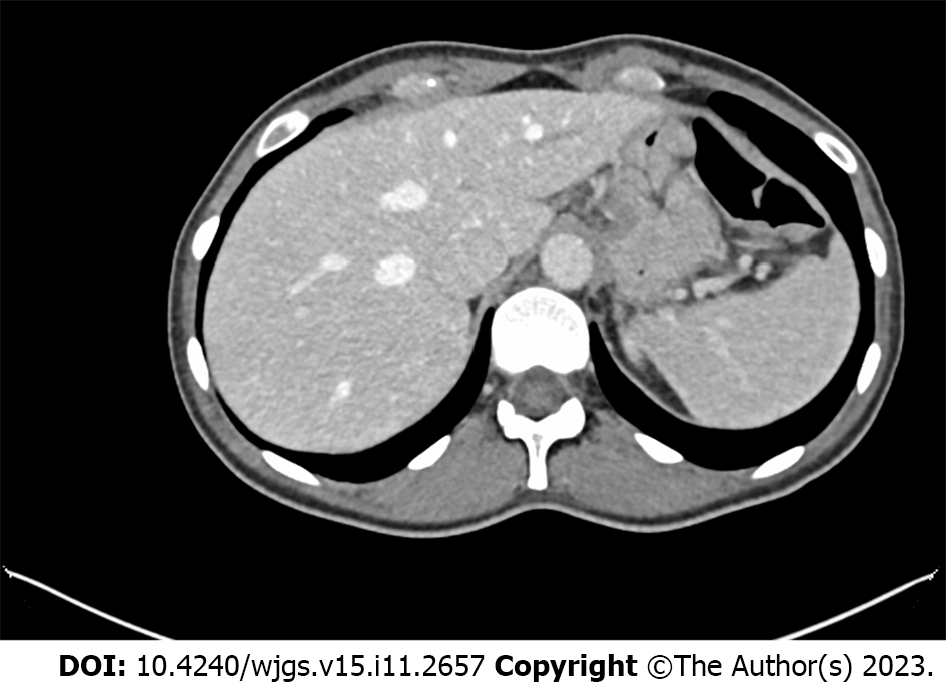
The control CT evidences “resolution of previous peritoneal affectation with persistence and stability of a left subdiafragmatic nodulary injury on the anterior surface of the fundus /gastric body” (Figure 1). A gastric Ecoendoscopy is requested identifying a solid perigastric injury of 12 mm with indeterminate endosonographic appearance. A biopsy is performed on 3 occasions, without obtaining a representative sample.
The case is presented in the tumor committee deciding to perform an exploratory laparoscopy.
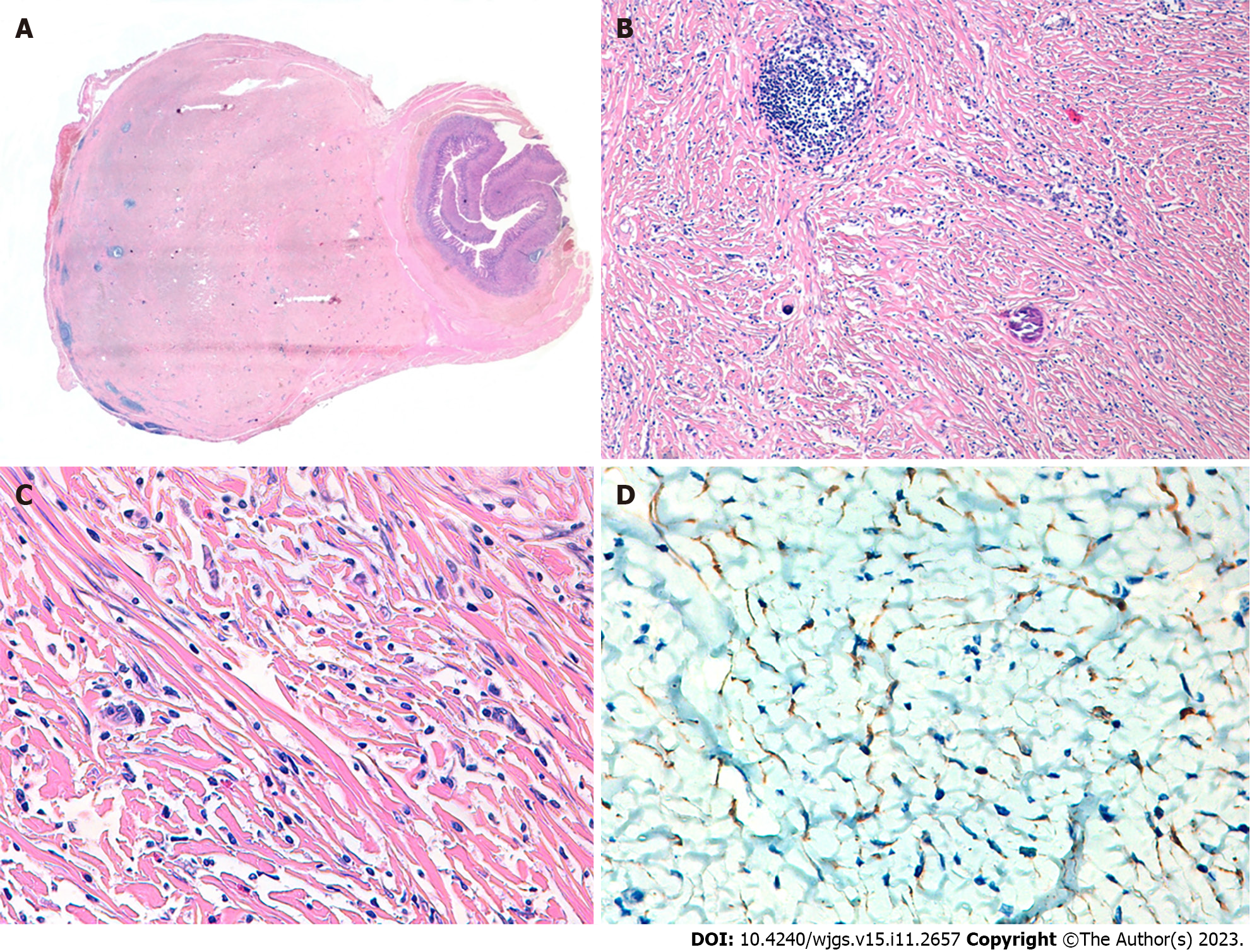
The pathology study reported a “mesenquimal injury of 1.3 cm growing in the muscular layer of the gastric wall, which is in contact with the resection margin. It’s sparsely celular, mainly constituted by fibrous tissue predominantly colagenised, with presence of spindle-shaped cells without significant atypia. Presence of psammomatous calcifications is also observed. The inmunophenotype of the tumor is: CK AE1-AE3+, Actina 1A4+ muy focal, ALK1-, Actina HHF35-, desmina-, caldesmon-, calponina-, CD34-, CKIT-, S100-” (Figure 2). Being the final diagnosis a IMT.
We perform an exploratory laparoscopy. During the intervention, an injury of aproximately 2 cm is identified on the anterior gastric face, and a wedge resection of the injury is performed. The patient evolves favourably and is discharged to the second postoperative day.
At 1 mo postoperatively, the patient was still alive. Given these findings, the case is presented again to the multidisciplinar committee, which decides to carry out an annual Ecoendoscopy and toracic CT to examine the pulmonar nodule.
The IMT is rare tumor, predominantly located in the lungs but can also be found in the retroperitoneum, mesentery, head, neck and stomach. The latter case, presented by our patient, is extremely rare, with very few described in literature (Table 1).
| Ref. | Sex/age | Presenting symptoms | Tumor localization in the stomach | Tumor size (cm) | Mitosis | Histologic pattern | Treatment | Follow-up |
| París-Sans et al[1] | M/88 | AP, vomiting, jaundice | GDJ | 4 | / | Proliferation of spindle-shaped mesenchymal cells mixed with lymphocytes | PG | / |
| Cheng et al[3] | W/52 | AP | Antrum (exophytic) | 4.3 | 0-1 | Proliferation of fusiform cells | DG | 6 mo |
| Bjelovic et al[4] | W/43 | AP, nausea | Distal Stomach | 6 | 44928 | Hypercellular spindle cell proliferation with vague fascicular areas | DG | 2 yr |
| Shi et al[5] | M/36 | AP, AM | Antrum, LC | 4.5 | 44928 | Myxoid hypocellular with some fascicular areas | PG | 5 yr (NED) |
| Shi et al[5] | M/42 | AP, UGH, AM, | Upper body, GC | 8 | 44928 | Fascicular with some myxoid areas | PG | Recurrence at 12 mo |
| Shi et al[5] | M/40 | AM | Upper body, AW | 6.3 | 44928 | Myxoid hypocellular with some fascicular areas | PG | 3 yr (NED) |
| Shi et al[5] | M/45 | AP, AM | Angle | 5.5 | 44928 | Myxoid hypocellular with some fascicular areas | PG | 2.6 yr (NED) |
| Shi et al[5] | W/45 | AP, AM | Lower body, PW | 5.8 | 44928 | Fascicular with some myxoid and sclerotic areas | PG | 4 yr (NED) |
| Katakwar et al[6] | M/45 | AP | AW | 5 | 44928 | Hypocellular, collagenized, myofibroblatic cells | DG | Recurrence at 1 mo |
| Leon et al[7] | W/50 | Vomiting, weight loss | PW | 7 | 44928 | Patternless round and spindle cell proliferation | PG | 2 yr (NED) |
| Park et al[8] | W/55 | AP, hematoperitoneum | Upper body, GC | 8 | 44928 | Vague fascicular proliferation | Gastric wedge resection | / |
| Jadhav et al[9] | M/18 | AM, weight loss | LC | 9 | 44928 | Pleomorphic cells, spindle-shaped to stellate cells arranged in a background of myxoid | Excision | 5 yr |
| Qiu et al[10] | W/61 | Fever | LC | 3 | / | Spindle cells with inflammatory infiltrate of neutrophils, eosinophils, lymphocytes, and plasma cells. | DG | 3 mo (NED) |
| Kim et al[11] | M/25 | AM | GEJ | 8 | / | / | / | / |
| Albayrak et al[12] | W/56 | Nausea, vomiting, UGH | Cardia | 11 | 44928 | Granulation-type and storiform spindle cell proliferation | PG | 8 mo (NED) |
| Our Study | W/ 45 | AP | AW (exophytic) | 1.3 | / | Spindle/stellate cells with inflammatory cells | Gastric wedge resection | 1 mo |
It is characterized by local recurrence but rarely incurs in distant metastasis[3]. Risk factors for the development of IMT have not been established, but cases have been described which suggest association with Virus Epstein bar, genetic alterations like the reorganisation of the anaplastic lymphoma kinase (ALK) gene in the 2p23 cromosome or alterations of the inmune system[3,4]. They are usually asymptomatic or present inespecific symptoms like abdominal pain, toracic pain, and up to 30% develop a constitutional syndrome[1,2].
The diagnosis is based on imaging tests like the abdominal TC, abdominal ecography and the ecoendoscopy[5].
The differential diagnosis includes gastrointestinal stroma tumor, fibroid inflammatory polyp, single fibrous tumor or peripheral nerve tumors, amongst others[6].
Confirmation diagnosis is obtained with histological examination, which evidences proliferations of myofibroblasts, lymphoplasmacytic infiltrate, and a myxoid stroma[5].
Fifty-six percent of IMT present reorganisation of gene ALK. These patients present a higher risk of local recurrence but not distant metastasis (negative ALK), which suggests that reactivity to the ALK could be a protective factor[3].
Due to the unpredictable nature of this tumor, surgical resection is the best therapeutic option. Regarding gastric IMTs, depending on the tumor’s location, options go from a wedge resection to a partial gastrectomy[1-3]. Patients which cannot undergo surgical interventions, can be treated with a combination of radiotherapy and chemotherapy. Patients with metastatic tumors or local advanced tumors resistent to conventional chemotherapy can be treated with Crizotinib if they present a mutation of ALK or Larotrectinib o Entrectinib, if they present mutations in the gene TRK[2].
The recurrence rate in the first year after surgery is of 15%-37%, therefore clinical and radiological follow-ups are indicated, without finding in the literature a defined periodicity for them[3,4].
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kumar M, India; liu QQ, China S-Editor: Lin C L-Editor: A P-Editor: Yu HG
| 1. | París-Sans M, Domènech-Calvet J, Raga-Carceller E, Sabench-Pereferrer F, Del Castillo-Déjardin D. Gastric inflammatory myofibroblastic tumour as a rare cause of biliary duct obstruction. Cir Esp. 2016;94:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | UpToDate. Uncommon sarcoma subtypes. Jul 31, 2023. [cited 20 May 2023]. Available from: https://medilib.ir/uptodate/show/114329. |
| 3. | Cheng B, Yang C, Liu Z, Liu L, Zhou L. Primary gastric inflammatory myofibroblastic tumor: A case report. Medicine (Baltimore). 2018;97:e13423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Bjelovic M, Micev M, Spica B, Babic T, Gunjic D, Djuric A, Pesko P. Primary inflammatory myofibroblastic tumor of the stomach in an adult woman: a case report and review of the literature. World J Surg Oncol. 2013;11:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Shi H, Wei L, Sun L, Guo A. Primary gastric inflammatory myofibroblastic tumor: a clinicopathologic and immunohistochemical study of 5 cases. Pathol Res Pract. 2010;206:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Katakwar A, Gedam BS, Mukewar S, Agasti A. Primary gastric inflammatory myofibroblastic tumor in an adult-case report with brief review. Indian J Surg Oncol. 2014;5:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Leon CJ, Castillo J, Mebold J, Cortez L, Felmer R. Inflammatory myofibroblastic tumor of the stomach: an unusual complication after gastrectomy. Gastrointest Endosc. 2006;63:347-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Park SH, Kim JH, Min BW, Song TJ, Son GS, Kim SJ, Lee SW, Chung HH, Lee JH, Um JW. Exophytic inflammatory myofibroblastic tumor of the stomach in an adult woman: a rare cause of hemoperitoneum. World J Gastroenterol. 2008;14:136-139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Jadhav M, Harvi R, Patil R, Kittur S. Inflammatory Myofibroblastic Tumor of the Stomach Presenting as an Exophytic Mass - A Diagnostic Dilemma. Turk Patoloji Derg. 2019;35:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Qiu JF, Shi YJ, Fang L, Wang HF, Zhang MC. High fever as an initial symptom of primary gastric inflammatory myofibroblastic tumor in an adult woman. Int J Clin Exp Med. 2014;7:1468-1473. [PubMed] |
| 11. | Kim KA, Park CM, Lee JH, Cha SH, Park SW, Hong SJ, Seol HY, Cha IH, Mok YJ, Kim YS. Inflammatory myofibroblastic tumor of the stomach with peritoneal dissemination in a young adult: imaging findings. Abdom Imaging. 2004;29:9-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Albayrak F, Dursun H, Albayrak Y, Altas S, Uyanik A, Yildirim R. Inflammatory myofibroblastic tumor of the stomach in an adult woman: a rare intermittent cause of gastric outlet obstruction. Tumori. 2010;96:492-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |