Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2272
Peer-review started: August 3, 2023
First decision: August 16, 2023
Revised: August 24, 2023
Accepted: September 6, 2023
Article in press: September 6, 2023
Published online: October 27, 2023
Processing time: 85 Days and 1.6 Hours
This study evaluated the safety and effectiveness of endoscopic retrograde cholangiopancreatography (ERCP) in pediatric patients with biliary and pancreatic diseases. A retrospective analysis was conducted on 57 ERCP procedures performed in 41 children, primarily for treating pancreatic diseases. The overall success rate was 91.2%, with no major complications observed. Post-ERCP pancreatitis (PEP) occurred in 8.8% of cases. Follow-up examinations over one year showed no recurrence of biliary or pancreatic diseases. Notably, endoscopic treatment led to a significant increase in body mass index (BMI). These findings demonstrate the valuable role of ERCP in managing such conditions.
To evaluate the safety and efficacy of ERCP for the management of biliary and pancreatic diseases in pediatric patients.
We conducted a retrospective analysis of data from children aged 1-18 years who underwent ERCP for biliary and pancreatic diseases at Beijing Children’s Hospital between January 2021 and December 2022. The collected data included procedure time, endoscopic treatment, success rate, and postoperative complications.
Forty-one children underwent 57 ERCP procedures, including 14 with biliary duct disease and 27 with pancreatic disease. The mean age of the patients was 7.48 ± 3.48 years. Biliary duct-related treatments were performed 18 times, and pancreatic disease treatments were performed 39 times. ERCP was primarily used to treat pediatric pancreatic diseases [68.4% (39/57) of the procedures]. The overall success rate was 91.2% (52/57 patients). PEP was noted in five patients (8.8%, 5/57), and no instances of bleeding, perforation, or cholangitis were observed. The patients were followed up for over one year, and no recurrence of biliary or pancreatic diseases was detected. Importantly, BMI significantly increased after endoscopic treatment compared to that before treatment (P = 0.001).
The high success rate and lack of major complications support the valuable role of ERCP in the management of pediatric biliary and pancreatic diseases in the pediatric population.
Core Tip: We evaluated the safety and efficacy of endoscopic retrograde cholangiopancreatography (ERCP) in pediatric patients with biliary and pancreatic diseases. In total, 57 ERCP procedures were performed in 41 children, primarily for the treatment of pancreatic diseases. The overall success rate was 91.2% with no instances of bleeding, perforation, or cholangitis. Post-ERCP pancreatitis occurred in 8.8% of the cases. The patients were followed up for over one year, and no recurrence of biliary or pancreatic diseases was detected. Importantly, endoscopic treatment significantly increased body mass index. These findings highlighted the valuable role of ERCP in managing these conditions.
- Citation: Qin XM, Yu FH, Lv CK, Liu ZM, Wu J. Endoscopic retrograde cholangiopancreatography for diagnosing and treating pediatric biliary and pancreatic diseases. World J Gastrointest Surg 2023; 15(10): 2272-2279
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2272.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2272
The study indicated that endoscopic retrograde cholangiopancreatography (ERCP) may be a safe and effective diagnostic and therapeutic approach for pediatric biliary and pancreatic diseases. The spectrum of the disease which was the indication of the ERCP of the adult is different from the children. The disease of the children was mainly the pancreatic disease, rather than the biliary tract disease. This also made the ERCP surgery more difficult in children. However, further prospective studies are required to determine the efficacy and safety of ERCP in pediatric patients.
The majority of ERCP experience in pediatric patients is gained by treating adult patients[1,2]. Research on this technique in specialized pediatric hospitals is scarce. In this retrospective study, we shared our experience of performing ERCP in pediatric patients at specialized pediatric hospitals in China. The endoscopic procedures were performed by skilled pediatricians who closely monitored the patients throughout the procedure. We performed ERCP 18 and 39 times in patients with biliary duct and pancreatic diseases, respectively, and achieved an overall success rate of 91.2% (52/57 patients). Remarkably, we found no severe postoperative complications or instances of biliary or pancreatic disease recurrence during the 1-year follow-up period. Furthermore, the improvement in body mass index (BMI) after the procedure indicated the effectiveness of ERCP in treating biliary and pancreatic diseases.
In this study, ERCP was performed 57 times in a cohort of 41 children with a mean age of 7.48 ± 0.48 years. The current study suggested no strict age limitation for children undergoing ERCP[3]. Weng et al[4] reported that ERCP is safe for infants aged 6 mo to 1 year.
The success of ERCP in pediatric patients is affected by several factors, such as age, type of biliary or pancreatic disease, instrument and accessory selection, and depth of anesthesia. Various challenges arise due to the limited tolerance, low cooperation, and delicate digestive tracts of children; therefore, ERCP requires skilled operators and specialized instruments. In addition, in pediatric patients, procedures are performed under anesthesia[5]. In this study, general anesthesia was administered to all the children because of their underlying conditions and poor general health. Anesthesiologists from our hospital assisted with the entire procedure to ensure smooth completion and operational safety. Some studies have suggested that pediatric duodenoscopy using a duodenoscope with a smaller diameter should be the preferred option for children weighing less than 10 kg, while larger duodenoscopes designed for adults can be used for children weighing > 10 kg[6]. In our study, the success rate of the procedure was 91.2%, which is slightly lower than the previously reported rate of 98.3%[7], and can be attributed to the limited number of enrolled patients and the diversity of pancreatic diseases. Furthermore, the success rate of intubation is lower in pancreatic diseases than in biliary diseases[7].
Post-ERCP pancreatitis (PEP) is a common complication that occurs in approximately 3%-14.7% of ERCP cases[8-10]. PEP is associated with intrapancreatic procedures, such as difficult nipple intubation, pre-cut sphincterotomy, pancreatic duct sphincterotomy, contrast agent injection into the pancreatic duct, and balloon dilation of the bile duct[11,12]. A retrospective study involving 313 pediatric patients reported that pancreatic duct injection, papilla, and pancreatic duct sphincterotomy were risk factors for PEP, whereas a history of chronic PEP was a protective factor against PEP[13,14]. In the present study, the incidence of PEP was 8.7% (5/57). Other children exhibited increased amylase levels; however, these levels were within three times the normal ranges. This can be attributed to the impaired function of the pancreatic cells in chronic PEP. The protective effects of chronic PEP against PEP are associated with pancreatic atrophy and decreased enzyme activity[15].
This study had several limitations. This was a single-center study with a relatively small cohort and a short follow-up period. Therefore, the results may be subject to bias due to the limited number of patients. Furthermore, this study has inherent limitations since it was a retrospective study.
A total of 41 children, comprising 17 boys and 24 girls, with biliary or pancreatic disease were enrolled in the study. The mean age was 7.48 ± 3.48 years. A total of 57 ERCP were performed. Among the 14 patients with biliary disease, there were six who had bile duct stones, three with abnormal pancreaticobiliary confluence, two with biliary stricture, and three with biliary fistula (Table 1). The biliary stones comprised sediment-like stones (8 patients) and hard lump stones (one patient). Endoscopic treatments for biliary disease included biliary stent placement (eight procedures), biliary stone extraction (nine procedures), biliary balloon dilation (two procedures), and biliary duct sphincterotomy (two procedures).
| Disease site | Patients (n = 14) | ERCP treatment (n = 18) |
| Bile duct stone | 6 | 7 |
| Abnormal pancreaticobiliary confluence | 3 | 4 |
| Biliary stricture caused by the surgery of the abdominal or digestive tract | 2 | 2 |
| Biliary fistula caused by the abdominal surgery | 3 | 5 |
| Surgery performed through ERCP | ||
| Biliary duct sphincterotomy | 2 | |
| Biliary balloon dilation | 2 | |
| Biliary stones’ extraction | 9 | |
| Biliary stent placement | 8 |
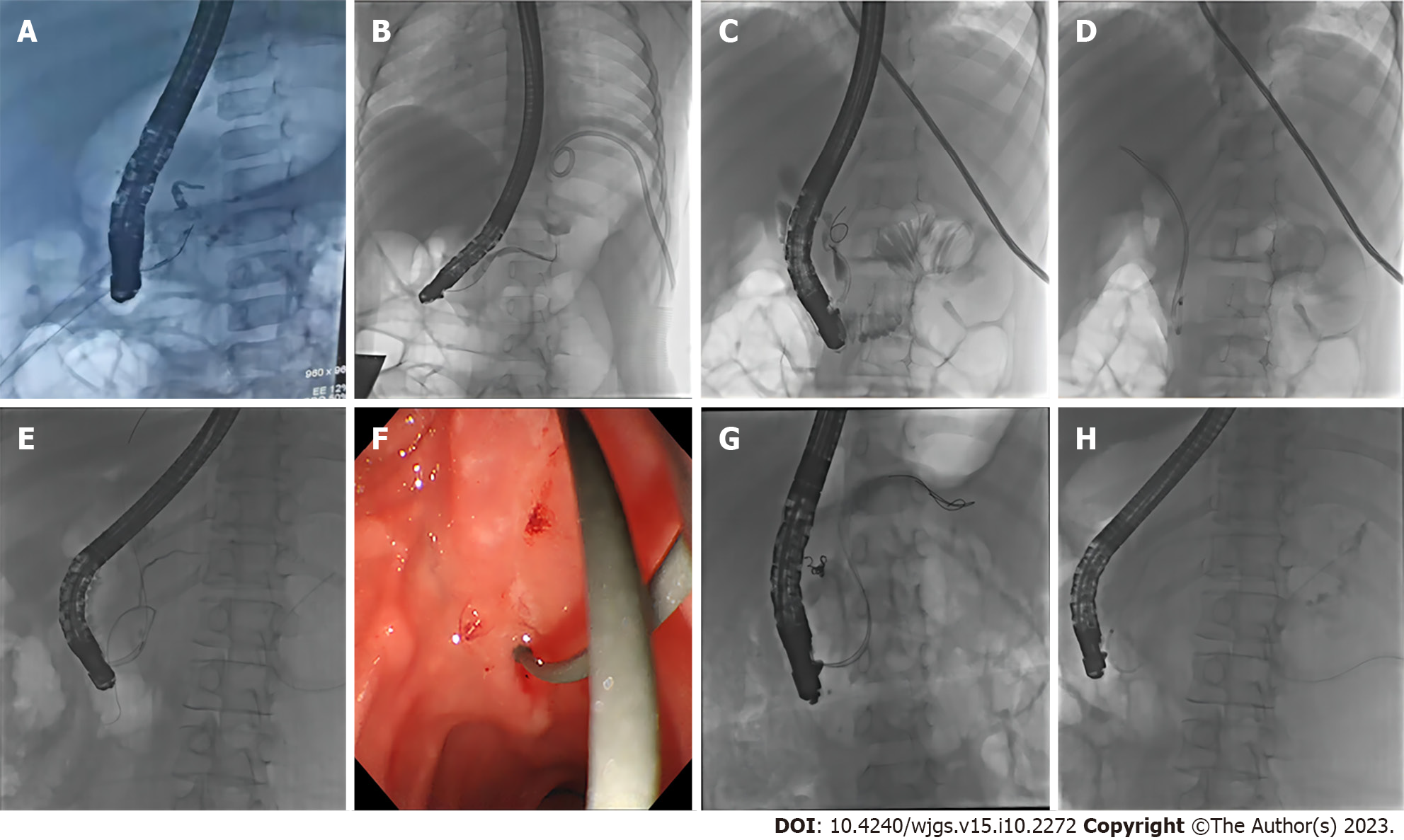
A total of 27 children exhibited pancreatic disease, including 16 with chronic PEP, one with a pseudocyst resulting from acute PEP, four with pancreatic fistula associated with systemic lupus erythematosus (SLE) and acute lymphoblastic leukemia (ALL), two with pancreatic fistula resulting from the procedure, and one with pancreatic duct stricture resulting from ulcerative colitis (UC) (Table 2). Endoscopic treatments for pancreatic disease included pancreatic stent placement (39 procedures), pancreatic stone extraction (23 procedures), and pancreatic duct sphincterotomy (six procedures). Some cases of the ERCP are shown in Figure 1.
| Disease site | Patients (n = 27) | ERCP treatment (n = 39) |
| Chronic pancreatitis | 16 | 22 |
| Pancreas divisum | 7 | 10 |
| Gene mutation | 9 | 12 |
| Pseudocyst caused by acute pancreatitis | 1 | 1 |
| Pancreatic fistula and pseudocyst caused by the SLE (3 cases) and ALL (1 case) | 4 | 10 |
| Pancreatic fistula caused by the trauma | 3 | 3 |
| Pancreatic fistula caused by the abdominal surgery | 2 | 2 |
| Pancreatic duct stricture caused by UC | 1 | 1 |
| Surgery performed through ERCP | ||
| Pancreas duct sphincterotomy | 6 | |
| Pancreas stones extraction | 23 | |
| Pancreas stent placement | 39 |
Eighteen procedures were performed for biliary disease and 39 for pancreatic disease. The overall success rate was 91.2% (52/57 patients). The success rate was 94.4% in the patients with biliary disease (17/18). Two patients underwent multiple bile stone procedures, including one with an abnormal pancreaticobiliary confluence. One patient required three procedures because of the presence of a bile fistula, which resulted from an abdominal surgery that was performed to change the stent. The only unsuccessful case involved a bile duct stricture resulting from duodenal surgery.
Two patients underwent four procedures for pancreatic disease, including those for pancreatic fistulas and pseudocysts resulting from SLE and chronic PEP with CFTR mutation. In total, nine patients underwent two procedures, including those for chronic PEP (three cases), pancreatic fistula and pseudocyst resulting from SLE (one case), and ALL (one case). The success rate was 89.7% (35/39 patients). There were four cases of unsuccessful procedures, including those for pancreatic pleural fistula resulting from chronic PEP (two cases), pancreatic duct stricture resulting from UC (one case), and pancreatic fistula resulting from trauma (one case). The success rates of the biliary and pancreatic procedures were not significantly different (P > 0.05).
The procedure-associated complications included PEP, hemorrhage, perforation, and infection. In total, five cases of PEP (8.87%, 5/57) without hemorrhage, perforation, or infection were present. Approximately 30 patients experienced postoperative hyperamylasemia that was successfully treated symptomatically. The complication rates among patients with biliary and pancreatic diseases were 5.56% (1/18) and 10.2% (4/39), respectively, with no significant difference (P > 0.05). Among the five children with postoperative PEP, one had bile duct stricture resulting from duodenal surgery, one had pancreatic pleural fistula, one had chronic abdominal pain that did not improve significantly after pancreatic duct stent placement, one had recurrent episodes of chronic PEP resulting from pancreatic pleural fistula, pancreatic head pancreatic duct stenosis, and failed ERCP intubation, and one had pancreatic fistula due to ALL.
Five children were followed up for more than one year. Stent replacement was performed 2-4 times at an interval of 3 to 12 mo. Data on disease recurrence, weight, and height were collected, and no disease recurrence was observed among children who underwent successful procedures. Furthermore, the mean preoperative BMI (13.2 ± 1.13) kg/m2 significantly differed from the postoperative BMI (15.3 ± 1.32) kg/m2 (P = 0.001).
Data from children who underwent ERCP for biliary and pancreatic diseases at the Beijing Children’s Hospital between January 2021 and December 2022 were retrospectively analyzed. The inclusion criteria were as follows: (1) Children aged 1-18 years and weighing > 10 kg; and (2) Confirmed diagnosis of biliary and pancreatic diseases using ultrasound, computed tomography (CT), or magnetic resonance cholangiopancreatography (MRCP).
This study was approved by the Ethics Committee of Beijing Children’s Hospital, and the requirement for informed consent from the patients was waived owing to the retrospective nature of the study. All procedures followed the ethical standards outlined in the Declaration of Helsinki, as revised in Brazil in 2013.
Before the procedure, the patients fasted for 6 h and received active rehydration support. Preoperative assessments included routine blood examinations, biochemical tests, coagulation profiles, abdominal ultrasound, CT, or MRCP. Based on these results, the patients were preliminarily diagnosed with bile duct and/or pancreatic disease.
ERCP was performed using equipment from Olympus, Japan, including a T-JF260 electronic duodenoscope, radiography catheter, guidewire, incision knife, stone basket support, and balloon (Cook Company and Boston Company). General anesthesia with tracheal intubation was administered to all children. For procedures lasting > 1 h, indwelling catheterization was performed, considering the patient’s age and preoperative condition. Anesthesiologists continuously monitored heart rate, respiratory rate, and pulse oxygen saturation throughout the procedure.
Experienced endoscopists performed all endoscopic procedures using routine adult duodenoscopy. Various interventions have been performed after successful selective intubation, including endoscopic sphincterotomy, pancreatic duct sphincterotomy, nipple-balloon dilatation, net basket/balloon lithotomy, endoscopic nasobiliary drainage, endoscopic nasopancreatic drainage, endoscopic retrograde biliary drainage, and endoscopic retrograde pancreatic drainage. Radiation protection measures have been implemented to safeguard the thyroid, thymus, breasts, and reproductive systems. Pressure ulcer prevention nursing care was provided.
Following ERCP, all patients were hospitalized for observation of potential post-ERCP complications. At 3 and 24 h after the procedure, serum amylase levels were evaluated to monitor dynamic changes. Complications including PEP, bleeding, perforation, and cholangitis were defined based on the literature[16].
Patient demographics, preoperative symptoms, ERCP completion, consumable data, postoperative complications, and follow-up data were extracted from the FUTang Updating medical REcords Database. Detailed information regarding the data cleaning process has been reported previously[17].
Data were analyzed using SPSS version 20.0 software. Normally distributed continuous data were presented as mean ± SD deviation and were compared using the t-test. The success rate of the procedure and the incidence of complications in the biliary and pancreatic regions were calculated using the chi-square test. Statistical significance was set at P < 0.05.
ERCP is a widely used procedure that combines radiography and upper gastrointestinal (GI) endoscopy to diagnose and treat disorders affecting the bile and pancreatic ducts in adults. Over time, it has evolved from a diagnostic tool to a predominantly therapeutic intervention and is considered a technically demanding and high-risk procedure for GI endoscopy[18]. Recent advances in duodenoscopic design and techniques have extended the application of ERCP to the diagnosis and treatment of biliary and pancreatic diseases in pediatric patients[19]. However, concerns remain regarding the effectiveness, safety, and qualifications of pediatric ERCP examiners.
Recent retrospective studies have revealed that ERCP has comparable efficacy and safety profiles in infants, children, and adolescents. For example, a study by Asenov et al[20] in 2019 reported that patients aged 6-17 years underwent ERCP between 1994 and 2014 and concluded that ERCP is valuable for diagnosing and treating pancreaticobiliary disorders in the pediatric population. Similarly, a two-center retrospective study by Mercier et al[21] in 2022 evaluated ERCP outcomes in children aged ≤ 15 years over the past three years, reporting excellent success and safety outcomes when performed by experienced endoscopists. A Portuguese study reported similar conclusions after evaluating the outcomes of children aged < 18 years who were admitted to a tertiary referral hospital between January 1994 and June 2022[20]. Keil et al[3] conducted 856 ERCP procedures in 626 pediatric patients with biliopancreatic disorders at University Hospital Motol, Prague between January 1999 and January 2018, with 59% of the procedures being therapeutic and 41% diagnostic. Studies have also revealed comparable outcomes between adults and children, although with varying success rates[22]. However, limited research has focused on the use of this technology in specialized pediatric hospitals. Therefore, this retrospective study aimed to assess the safety and efficacy of ERCP in the diagnosis and treatment of biliary and pancreatic diseases in the pediatric population.
The research findings provide important perspectives for future research on endoscopic retrograde cholangiopancreatography (ERCP) in pediatric patients with biliary and pancreatic diseases. Areas of focus include conducting long-term follow-up studies to assess durability and recurrence rates, comparative studies to compare ERCP with other treatments, investigating risk factors for post-ERCP pancreatitis (PEP), assessing the impact on quality of life, and conducting cost-effectiveness analyses. By addressing these research perspectives, further advancements can be made in optimizing the use of ERCP, improving outcomes, and guiding clinical decision-making in managing pediatric biliary and pancreatic diseases.
This study demonstrates that ERCP is both safe and effective for managing biliary and pancreatic diseases in pediatric patients. Among the 57 ERCP procedures performed in 41 children, a high success rate of 91.2% was achieved, with no major complications observed such as bleeding, perforation, or cholangitis. PEP occurred in 8.8% of cases, indicating a potential risk associated with the procedure. However, over a follow-up period of one year, no recurrences of biliary or pancreatic diseases were detected. Importantly, endoscopic treatment led to a significant increase in body mass index (BMI), highlighting its positive impact on nutritional status in pediatric patients. These findings support the valuable role of ERCP in effectively managing pediatric biliary and pancreatic diseases, thereby providing important insights for clinical practice and decision-making.
The research findings from this study evaluating ERCP in pediatric patients with biliary and pancreatic diseases indicate its safety and effectiveness. Among the 57 ERCP procedures performed in 41 children, the overall success rate was 91.2% with no major complications observed. PEP occurred in 8.8% of cases. Over a one-year follow-up period, there were no recurrences of biliary or pancreatic diseases. Notably, endoscopic treatment resulted in a significant increase in BMI, highlighting its potential positive impact on nutritional status. These results affirm the valuable role of ERCP in managing pediatric biliary and pancreatic diseases, emphasizing its efficacy and favorable outcomes in this patient population.
In this study, a retrospective analysis was conducted to evaluate the safety and effectiveness of ERCP in pediatric patients with biliary and pancreatic diseases. Data from 41 children who underwent 57 ERCP procedures at Beijing Children’s Hospital were analyzed. The study assessed the success rate of ERCP procedures, occurrence of major complications, incidence of PEP, recurrence of biliary or pancreatic diseases during follow-up, and changes in BMI. The findings revealed a high overall success rate of 91.2% with no major complications observed. PEP occurred in 8.8% of cases. Follow-up examinations over one year showed no disease recurrence. Notably, endoscopic treatment led to a significant increase in BMI.
The main objectives of this study were to evaluate the safety and efficacy of ERCP in pediatric patients with biliary and pancreatic diseases. These objectives included assessing the success rate of ERCP procedures, determining the occurrence of major complications, investigating PEP incidence, monitoring disease recurrence during follow-up examinations, exploring the impact on BMI, and evaluating the overall effectiveness of ERCP as a management strategy. By addressing these objectives, the study aimed to provide valuable insights into the role of ERCP in managing pediatric biliary and pancreatic diseases, contributing to improved patient care and treatment outcomes.
The management of biliary and pancreatic diseases in pediatric patients presents unique challenges, and there is a lack of research on the effectiveness of ERCP specifically in this population. Therefore, this study aimed to evaluate the safety and efficacy of ERCP in pediatric patients with these conditions. Through a retrospective analysis of ERCP procedures performed at Beijing Children’s Hospital, important insights were gained regarding the success rate, postoperative complications, and long-term outcomes of ERCP in this patient group. These findings provide valuable groundwork for further research and optimization of treatment strategies for pediatric biliary and pancreatic diseases, enhancing the care provided to this vulnerable population.
This study assessed the safety and effectiveness of ERCP in pediatric patients with biliary and pancreatic diseases. A total of 57 ERCP procedures were performed on 41 children, primarily targeting pancreatic diseases. The overall success rate was 91.2%, with no occurrences of bleeding, perforation, or cholangitis. PEP affected 8.8% of cases. Follow-up examinations spanning one year revealed no recurrence of biliary or pancreatic diseases. Notably, endoscopic treatment led to a significant increase in BMI. These findings underscore the valuable role of ERCP in managing such conditions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shafabakhsh R, Iran; Youse B, Saudi Arabia S-Editor: Qu XL L-Editor: A P-Editor: Yu HG
| 1. | Xue N, Lei XF, Xu JJ, Wei XX. [Progression of endoscopic retrograde cholangiopancreatography in children with pancreaticobiliary diseases]. Zhonghua Er Ke Za Zhi. 2021;59:145-149. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Usatin D, Fernandes M, Allen IE, Perito ER, Ostroff J, Heyman MB. Complications of Endoscopic Retrograde Cholangiopancreatography in Pediatric Patients; A Systematic Literature Review and Meta-Analysis. J Pediatr. 2016;179:160-165.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Keil R, Drábek J, Lochmannová J, Šťovíček J, Koptová P, Wasserbauer M, Frýbová B, Šnajdauf J, Matouš J, Kotalová R, Rygl M, Hlava Š. ERCP in infants, children, and adolescents-Different roles of the methods in different age groups. PLoS One. 2019;14:e0210805. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Weng M, Wang L, Weng H, Gu J, Wang X. Utility of endoscopic retrograde cholangiopancreatography in infant patients with conservational endoscopy. Transl Pediatr. 2021;10:2506-2513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Zhong J, Zhang J, Fan Y, Zhu M, Zhao X, Zuo Z, Zhou X, Miao C. Efficacy and safety of Ciprofol for procedural sedation and anesthesia in non-operating room settings. J Clin Anesth. 2023;85:111047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 6. | Troendle DM, Ruan W, Fishman DS, Barth BA, Liu QY, Giefer M, Kim KM, Martinez M, Dall'oglio L, Torroni F, De Angelis P, Faraci S, Bitton S, Wilsey M, Khalaf R, Werlin S, Dua K, Gugig R, Huang C, Mamula P, Quiros JA, Zheng Y, Grover A, Fox VL. Technical Outcomes in Pediatric Endoscopic Retrograde Cholangiopancreatography: Data from an International Collaborative. J Pediatr Gastroenterol Nutr. 2022;75:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 7. | Yu ZP, Zhu L, Yang XP, Cao RL, Chen YX. [Efficacy and safety of endoscopic retrograde cholangiopancreatography in children]. Zhonghua Er Ke Za Zhi. 2022;60:1295-1301. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Xu XD, Dai JJ, Qian JQ, Wang WJ. Nasobiliary drainage after endoscopic papillary balloon dilatation may prevent postoperative pancreatitis. World J Gastroenterol. 2015;21:2443-2449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Ribeiro IB, do Monte Junior ES, Miranda Neto AA, Proença IM, de Moura DTH, Minata MK, Ide E, Dos Santos MEL, Luz GO, Matuguma SE, Cheng S, Baracat R, de Moura EGH. Pancreatitis after endoscopic retrograde cholangiopancreatography: A narrative review. World J Gastroenterol. 2021;27:2495-2506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (2)] |
| 10. | Felux J, Sturm E, Busch A, Zerabruck E, Graepler F, Stüker D, Manger A, Kirschner HJ, Blumenstock G, Malek NP, Goetz M. ERCP in infants, children and adolescents is feasible and safe: results from a tertiary care center. United European Gastroenterol J. 2017;5: 1024-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Zargar SA, Javid G, Khan BA, Yattoo GN, Shah AH, Gulzar GM, Singh J, Rehman BU, ud-din Z. Endoscopic sphincterotomy in the management of bile duct stones in children. Am J Gastroenterol. 2003;98:586-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Giefer MJ, Kozarek RA. Technical outcomes and complications of pediatric ERCP. Surg Endosc. 2015;29:3543-3550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Cahyadi O, Tehami N, de-Madaria E, Siau K. Post-ERCP Pancreatitis: Prevention, Diagnosis and Management. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 14. | Troendle DM, Abraham O, Huang R, Barth BA. Factors associated with post-ERCP pancreatitis and the effect of pancreatic duct stenting in a pediatric population. Gastrointest Endosc. 2015;81:1408-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 15. | Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL, Silverman WB, Dua KS, Aliperti G, Yakshe P, Uzer M, Jones W, Goff J, Lazzell-Pannell L, Rashdan A, Temkit M, Lehman GA. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 433] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 16. | Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:127-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 493] [Article Influence: 98.6] [Reference Citation Analysis (1)] |
| 17. | Wang X, Zeng Y, Tian J, Xu H, Song F, Guo Y, Xu X, Feng G, Ni X. A brief introduction to the FUTang Updating medical REcords (FUTURE) database. Pediatr Investig. 2021;5:247-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Sanders DJ, Bomman S, Krishnamoorthi R, Kozarek RA. Endoscopic retrograde cholangiopancreatography: Current practice and future research. World J Gastrointest Endosc. 2021;13:260-274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Makita S, Amano H, Kawashima H, Hinoki A, Shirota C, Tainaka T, Sumida W, Yokota K, Okamoto M, Takimoto A, Yasui A, Nakagawa Y, Uchida H. Utility of endoscopic retrograde cholangiopancreatography in management of pediatric pancreaticobiliary disease. BMC Pediatr. 2022;22:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Reference Citation Analysis (0)] |
| 20. | Asenov Y, Akın M, Cantez S, Gün Soysal F, Tekant Y. Endoscopic retrograde cholangiopancreatography in children: Retrospective series with a long-term follow-up and literature review. Turk J Gastroenterol. 2019;30:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Mercier C, Pioche M, Albuisson E, Ponchon T, Gonzalez JM, Barthet M, Boytchev I, Vanbiervliet G, Fortier Beaulieu C, Prat F, Belle A, Branche J, Grandval P, Valats JC, Rudler F, Wallenhorst T, Koch S, Comte A, Williet N, Musquer N, Coron E, Derosiere A, Le Mouel JP, Schaefer M, Chabot C, Scheers I, Deprez PH, Chevaux JB. Safety of endoscopic retrograde cholangiopancreatography in the pediatric population: a multicenter study. Endoscopy. 2021;53:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Troendle DM, Barth BA. Pediatric Considerations in Endoscopic Retrograde Cholangiopancreatography. Gastrointest Endosc Clin N Am. 2016;26:119-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |