Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2179
Peer-review started: June 19, 2023
First decision: July 6, 2023
Revised: July 28, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: October 27, 2023
Processing time: 130 Days and 8.8 Hours
Currently, a variety of new nursing methods and routine nursing have been widely used in the nursing of gastrointestinal surgery patients.
To investigate the effect of follow-up protocol based on the Omaha System on self-care ability and quality of life of gastrointestinal surgery patients.
A total of 128 patients with inflammatory bowel disease in gastrointestinal surgery in gastrointestinal surgery from March 2019 to August 2021 were divided into A (n = 64) and B (n = 64) groups according to different nursing methods. The group A received a follow-up program Omaha System-based intervention of the group B, whereas the group B received the routine nursing intervention. Medical Coping Modes Questionnaire, Crohn’s and Colitis Knowledge Score (CCKNOW), inflammatory bowel disease questionnaire (IBDQ), Exercise of Self-nursing Agency Scale (ESCA), The Modified Mayo Endoscopic Score, and Beliefs about Medicine Questionnaire (BMQ) were compared between the two groups.
Following the intervention, the group A were facing score significantly increased than group B, while the avoidance and yield scores dropped below of group B (all P < 0.05); in group A, the level of health knowledge, personal care abilities, self-perception, self-awareness score and ESCA total score were more outstanding than group B (all P < 0.05); in group A the frequency of defecation, hematochezia, endoscopic performance, the total evaluation score by physicians and the disease activity were lower than group B (all P < 0.05); in the group A, the total scores of knowledge in general, diet, drug, and complication and CCKNOW were higher than group B (all P < 0.05); in group A, the necessity of taking medicine, score of medicine concern and over-all score of BMQ were more significant than group B (all P < 0.05); at last in the group A, the scores of syste
For gastrointestinal surgery patients, the Omaha System-based sequel protocol can improve disease awareness and intervention compliance, help them to face the disease positively, reduce disease activity, and improve patients’ self-nursing ability and quality of life.
Core Tip: The Omaha System was applied in the follow-up of gastrointestinal surgery patients in this study, and the previous follow-up care of gastrointestinal surgery was integrated and re-innovated. The purpose of this study was to compare the nursing effect of conventional gastrointestinal surgery care and the follow-up plan based on the Omaha System on gastro
- Citation: Li YD, Qu N, Yang J, Lv CY, Tang Y, Li P. Effects of an Omaha System-based follow-up regimen on self-care and quality of life in gastrointestinal surgery patients. World J Gastrointest Surg 2023; 15(10): 2179-2190
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2179.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2179
The primary cause of inflammatory bowel disease (IBD) is still unknown. It is believed that the damage of intestinal epithelial mucosa cells is an essential pathophysiological basis of IBD. Normal intestinal mucosa constitutes the intestinal barrier of patients, and intestinal mucosal epithelial cells, intestinal flora, and mucus are in a relatively stable state[1]. IBD is a long-course disease that requires prolonged intervention due to easy recurrence and needs long-term nursing. However, most patients receive intervention and nursing in a passive manner, lack awareness of participation, and lack self-nursing after discharge, leading to repeated illness after discharge[2]. Previous studies have suggested that con
Data of 128 patients with IBD in gastrointestinal surgery from March 2019 to August 2021 were retrospectively analyzed, and they were divided into group A and group B according to different nursing methods, with 64 cases in group A and 64 cases in group B.
Patients matched the diagnostic standards of IBD in the Consensus Opinion on the Diagnosis and intervention of Inflammatory Bowel Disease in gastrointestinal surgery (2018, Beijing)[5]; all patients underwent surgical intervention; and patients signed the consent form.
Patients with chronic heart, liver, and kidney function; patients with lingual function and intellectual impairment; patients with ischemic colitis, infectious colitis, and other colonic diseases; patients with intestinal cancer and obstructive diseases; and patients with incomplete clinical case data.
The lecture discussed patients’ health knowledge of inflammatory enteritis during hospitalization and answered the questions on the spot. Propaganda posters were posted in the department, and medication guidance was given to the patients when hospitalized. The patients were instructed to follow the doctor’s prescription in taking medicine, recognize adverse drug reactions, and ask for return visits regularly.
Group A was given a follow-up intervention based on the Omaha System on the basis of routine intervention for a total of three months. As the framework of nursing practice, Omaha System consists of three parts: Problem classification system, intervention system, and effect evaluation.
Problem classification system: Based on the patient’s clinical symptoms, signs, and basic personal situation, the related nursing problems were put forward from the physiology, psychology, health behavior, and ecological perspectives of the Omaha System. The nursing problems were described and ranked in the priority order by evaluating the patients’ coping styles, disease awareness, and self-nursing ability using corresponding scales. The nursing problems include low aware
Health education, guidance, and consultation: Scientific knowledge lectures on inflammatory diseases were organized regularly every week, and on-site guidance and explanation were provided for patients’ problems. A patient association, an example, or a mutual aid group can be established. The patient with outstanding comprehensive quality was selected as the group leader, showing strong self-management ability, outgoing personality, sense of responsibility, and com
Operating procedures: (1) Medication guide: Based on the registration form of the patient during hospitalization and the recovery status of the patient, the relevant knowledge of medication was popularized to the patient and his family members, and the adverse reactions and symptoms of the drug were informed, the time and dosage of medication were told to the patient, and the dosage of medication was ensured; (2) Diet nursing: The nursing staff emphasized the impor
Case management: Achievable goals were made, and corresponding nursing measures were executed based on the ability of patients and caregivers to promote rehabilitation. For example, establishing self-health management, record daily habits, abdominal pain, diarrhea and possible symptoms and signs, guide patients to self-supervision, actively participate in disease management, and improve patients’ self-care awareness and self-health management ability. Patient’s family members can also be invited to participate, urge patients to get rid of bad habits, encourage patients to exercise actively, and promote collaborative management of family members.
Nursing evaluation: The coping style, disease awareness, quality of life, self-nursing ability, disease activity, and compliance of patients after the intervention were evaluated.
Medical Coping Modes Questionnaire (MCMQ)[6], Crohn’s and Colitis Knowledge Score (CCKNOW)[7], Inflammatory bowel disease in gastrointestinal surgery questionnaire (IBDQ)[8], Exercise of Self-nursing Agency Scale (ESCA)[9], The Modified Mayo Endoscopic Score[10], and Beliefs about Medicine Questionnaire (BMQ)[11] date were collected and analyzed of the two groups. MCMQ mainly included three dimensions: Facing (8 objects, 0-32 points), avoidance (7 objects, 0-28 points) and surrender (5 objects, 0-20 points). CCKNOW was used to evaluate patients’ disease awareness before and after the intervention. It mainly included general knowledge (11 questions), diet knowledge (2 questions), drug knowledge (6 questions), and complications knowledge (5 questions). The score ranged from 0 to 23 (the 14th and 15th questions applied to Crohn’s disease and respective ulcerative colitis). The score was positively proportional to the awareness of the disease. IBDQ mainly included four aspects: Systemic symptoms, intestinal symptoms, social function, and emotional function, and each aspect included seven items. Each item ranges from 1-8 points, with an overall score of 28 to 224. ESCA mainly included four aspects, including the level of health knowledge, personal care-abilities, self-perception, and self-awareness score, totaling 43 items. The range of a single object starts from 1 to 4 points, and overall the score ranges between 43-172 points. Modified Mayo scoring system included four aspects: Frequency of defecation, frequency of bloody stool, endoscopic performance, and the overall evaluation of doctors. Single objects range from 0-3 points; overall, the score range was 0-12. The score of the disease was positively correlated with the severity of the disease. BMQ were used to assess patients’ medication beliefs. This scale mainly included two dimensions: Medication necessity (5 items) and medication concern (5 items). A single item from 1 to 5 points, and the range of scores was 10-50 points. The score was directly proportional to the more substantial the medication belief.
Data descriptive statistics were analyzed using SPSS (version 22.0). The scoring data were measured as a percentage (%) and then compared between groups using a χ2 test. The categorical variables were represented as mean ± SD after the normality test, and then the data of both groups were compared using the independent sample t-test. The paired sample of the t-test was used to compare differences within the groups. GraphPad Prism-5 was used for representing the data in graphs keeping the significance level at P < 0.05.
The study showed no significant differences in the general data between these two groups (all P < 0.05, Table 1).
| Group | Group A (n = 64) | Group B (n = 64) | χ2/t | P value |
| Gender | ||||
| Male | 38 | 35 | 0.287 | 0.592 |
| Female | 26 | 29 | ||
| Age | 43.11 ± 4.77 | 41.80 ± 4.48 | 1.605 | 0.111 |
| Course of disease | 1.25 ± 0.25 | 1.18 ± 0.25 | 1.392 | 0.166 |
| Degree of education | ||||
| Junior high school and below | 19 | 21 | 0.145 | 0.703 |
| High school and above | 45 | 43 | ||
| Disease type | ||||
| Ulcerative colitis | 56 | 59 | 0.771 | 0.380 |
| Crohn’s disease | 8 | 5 | ||
| Family history of digestive disorders | 7 | 5 | 0.368 | 0.544 |
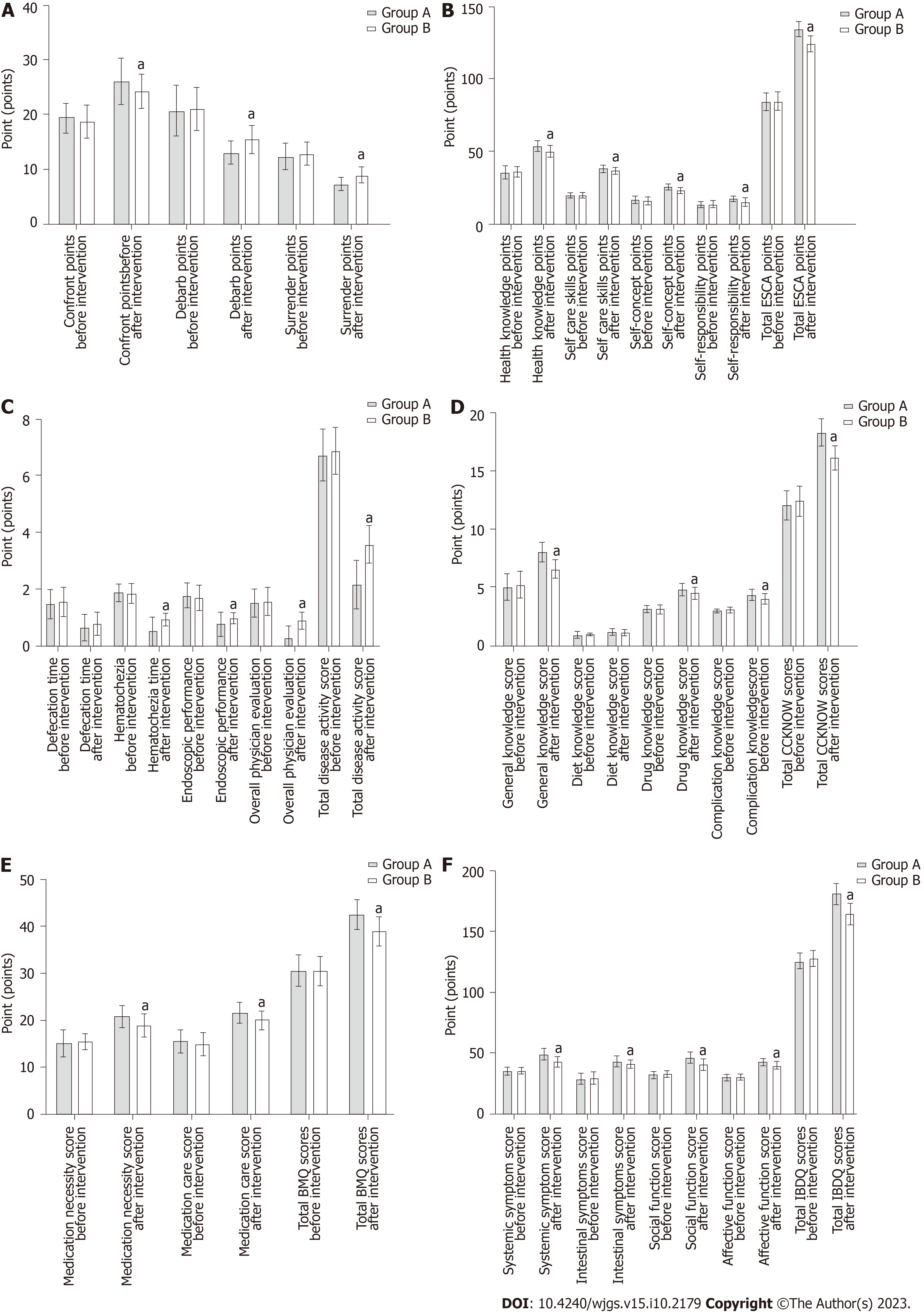
As before, the intervention showed no significant differences in confronting, avoidance, and surrender scores between both groups (all P < 0.05). After an intervention, it showed that the group A scored higher in confronting but lower in avoidance and surrender scores than the group B (all P < 0.05, Figure 1A). The confronting score of the group A was more significant than the group B, and the avoidance and surrender scores were lower than the group B (all P < 0.05, Table 2, Figure 1A).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| Confront points | ||||
| Before intervention | 19.44 ± 2.65 | 18.66 ± 3.11 | 1.528 | 0.129 |
| After intervention | 25.98 ± 4.23a | 24.19 ± 3.11a | 2.741 | 0.007 |
| Debarb points | ||||
| Before intervention | 20.64 ± 4.70 | 20.94 ± 3.97 | 0.386 | 0.700 |
| After intervention | 13.00 ± 2.15a | 15.44 ± 2.54a | 5.859 | < 0.001 |
| Surrender points | ||||
| Before intervention | 12.28 ± 2.51 | 12.84 ± 2.08 | 1.381 | 0.170 |
| After intervention | 7.28 ± 1.34a | 9.02 ± 1.46a | 6.994 | < 0.001 |
Before the intervention, showed no significance in the differences in individual scores and total scores on the ESCA scale between both groups (all P > 0.05). After the intervention, the level of health knowledge, self-nursing skills, self-concept, self-responsibility score, and ESCA total scores of the group A were more significant than the group B (all P < 0.05, Table 3, Figure 1B).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| Health knowledge points | ||||
| Before intervention | 35.13 ± 4.68 | 35.75 ± 3.56 | 0.851 | 0.396 |
| After intervention | 53.33 ± 4.07a | 49.81 ± 4.23a | 4.786 | < 0.001 |
| Self care skills points | ||||
| Before intervention | 19.39 ± 2.00 | 19.66 ± 2.04 | 0.744 | 0.458 |
| After intervention | 37.97 ± 2.77a | 36.45 ± 2.44a | 3.286 | 0.001 |
| Self-concept points | ||||
| Before intervention | 16.14 ± 2.84 | 15.72 ± 2.78 | 0.849 | 0.398 |
| After intervention | 25.47 ± 2.43a | 22.75 ± 2.30a | 6.507 | < 0.001 |
| Self-responsibility points | ||||
| Before intervention | 13.33 ± 2.64 | 13.30 ± 2.65 | 0.067 | 0.947 |
| After intervention | 17.22 ± 2.00a | 14.98 ± 2.83a | 5.154 | < 0.001 |
| Total ESCA points | ||||
| Before intervention | 83.98 ± 6.22 | 84.42 ± 6.26 | 0.397 | 0.692 |
| After intervention | 133.98 ± 5.56a | 124.00 ± 5.56a | 10.153 | < 0.001 |
Before the intervention showed no significant differences in the score of disease activity and total scores between the two groups (all P > 0.05), after the intervention, the hematochezia, endoscopic manifestations, overall physician evaluation score, and total score of disease activity in the group A were lower than in the group B (all P < 0.05, Table 4, Figure 1C).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| Defecation time | ||||
| Before intervention | 1.48 ± 0.50 | 1.55 ± 0.50 | 0.703 | 0.483 |
| After intervention | 0.63 ± 0.49a | 0.78 ± 0.42a | 1.948 | 0.054 |
| Hematochezia | ||||
| Before intervention | 1.89 ± 0.31 | 1.86 ± 0.35 | 0.531 | 0.596 |
| After intervention | 0.52 ± 0.50a | 0.94 ± 0.24a | 6.030 | < 0.001 |
| Endoscopic performance | ||||
| Before intervention | 1.77 ± 0.46 | 1.70 ± 0.46 | 0.766 | 0.445 |
| After intervention | 0.77 ± 0.43a | 0.97 ± 0.18a | 3.521 | < 0.001 |
| Overall physician evaluation | ||||
| Before intervention | 1.50 ± 0.50 | 1.55 ± 0.50 | 0.527 | 0.599 |
| After intervention | 0.27 ± 0.45a | 0.89 ± 0.31a | 9.173 | < 0.001 |
| Total disease activity score | ||||
| Before intervention | 6.72 ± 0.93 | 6.88 ± 0.83 | 1.003 | 0.318 |
| After intervention | 2.17 ± 0.83a | 3.58 ± 0.66a | 10.618 | < 0.001 |
No significant difference was existed between the individual score and total score of the CCKNOW scale (all P > 0.05). After the intervention, the score of general knowledge, drug knowledge, complication knowledge, and total CCKNOW score in the group A was more significant than in the group B (all P < 0.05, Table 5, Figure 1D).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| General knowledge score | ||||
| Before intervention | 5.03 ± 1.18 | 5.23 ± 1.15 | 0.985 | 0.326 |
| After intervention | 8.00 ± 0.84a | 6.55 ± 0.85a | 9.734 | < 0.001 |
| Diet knowledge score | ||||
| Before intervention | 0.91 ± 0.29 | 0.98 ± 0.13 | 1.958 | 0.054 |
| After intervention | 1.14 ± 0.35a | 1.09 ± 0.29a | 0.820 | 0.414 |
| Drug knowledge score | ||||
| Before intervention | 3.13 ± 0.33 | 3.14 ± 0.35 | 0.258 | 0.796 |
| After intervention | 4.78 ± 0.58a | 4.48 ± 0.53a | 3.022 | 0.003 |
| Complication knowledge score | ||||
| Before intervention | 3.02 ± 0.13 | 3.06 ± 0.24 | 1.368 | 0.175 |
| After intervention | 4.31 ± 0.50a | 4.02 ± 0.42a | 3.646 | < 0.001 |
| Total CCKNOW scores | ||||
| Before intervention | 12.08 ± 1.25 | 12.42 ± 1.29 | 1.527 | 0.129 |
| After intervention | 18.23 ± 1.21a | 16.14 ± 1.07a | 10.406 | < 0.001 |
Before the intervention, no significant differences were observed in individual scores and total score of BMQ between the two groups (all P > 0.05). After the intervention, the scores of medication necessity, medication concern, and BMQ total score in the group A were more significant than in the group B (all P < 0.05, Table 6, Figure 1E).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| Medication necessity score | ||||
| Before intervention | 15.05 ± 2.90 | 15.50 ± 1.76 | 1.069 | 0.288 |
| After intervention | 20.80 ± 2.30a | 18.94 ± 2.39a | 4.481 | < 0.001 |
| Medication care score | ||||
| Before intervention | 15.53 ± 2.49 | 14.95 ± 2.41 | 1.336 | 0.184 |
| After intervention | 21.66 ± 2.35a | 20.00 ± 2.08a | 4.222 | < 0.001 |
| Total BMQ scores | ||||
| Before intervention | 30.58 ± 3.42 | 30.45 ± 3.14 | 0.215 | 0.830 |
| After intervention | 42.45 ± 3.22a | 38.94 ± 3.15a | 6.241 | < 0.001 |
Showed no significant differences in individual scores and total scores of IBDQ between both groups (all P > 0.05). After the intervention, the scores of systemic symptoms, intestinal symptoms, social function, emotional function, and IBDQ total score in the group A were more significant than in the group B (all P < 0.05, Table 7, Figure 1F).
| Group | Group A (n = 64) | Group B (n = 64) | t value | P value |
| Systemic symptom score | ||||
| Before intervention | 35.13 ± 3.45 | 35.23 ± 2.91 | 0.194 | 0.847 |
| After intervention | 48.75 ± 4.86a | 42.78 ± 4.70a | 7.069 | < 0.001 |
| Intestinal symptoms score | ||||
| Before intervention | 28.48 ± 4.69 | 29.17 ± 5.28 | 0.778 | 0.438 |
| After intervention | 43.05 ± 4.55a | 40.61 ± 3.49a | 3.399 | 0.001 |
| Social function score | ||||
| Before intervention | 31.92 ± 2.70 | 32.78 ± 3.07 | 1.680 | 0.096 |
| After intervention | 46.27 ± 4.97a | 40.66 ± 4.85a | 6.463 | < 0.001 |
| Affective function score | ||||
| Before intervention | 29.89 ± 2.59 | 30.38 ± 2.09 | 1.163 | 0.247 |
| After intervention | 42.55 ± 2.96a | 39.55 ± 3.32a | 5.397 | < 0.001 |
| Total IBDQ scores | ||||
| Before intervention | 125.42 ± 6.72 | 127.78 ± 6.88 | 1.962 | 0.052 |
| After intervention | 180.61 ± 8.77a | 164.44 ± 8.62a | 10.523 | < 0.001 |
IBD is a known idiopathic inflammatory disease of the intestinal tract. Its onset sites are primarily concentrated in the ileum and rectum, and patients often manifest abdominal pain, diarrhea, and tenesmus. Some patients are also accom
When IBD patients are in the active stage of disease, their abdominal pain, diarrhea, and gastrointestinal bleeding are more severe and frequent, which has a significant impact on their life, work and social life, and they are more likely to be affected by negative emotions, namely anxiety and depression[13]. Hence, it is necessary to strengthen nursing care for IBD patients in the active stage, strictly monitor patients’ vital signs, strengthen pain management, and give psychological support to encourage patients to express their own needs and ideas. Studies have shown that improving coping strategies positively impacts the survival of IBD patients. Cognitive behavioral therapy to improve coping styles can develop the quality of life of IBD children and even lessen their disease activity[15,16]. This study found that after intervention, the scores of defecation, hematochezia, endoscopy, overall evaluation of physicians and total score of disease activity in the group A were lower than those in the group B, indicating that the follow-up plan of IBD patients based on Omaha could reduce disease activity. This is mainly related to the strict diet guidance, exercise nursing, and medication guidance for patients in this study. Abdominal pain is the most common symptom in the active stage of the disease. In this study, nursing staff took precautionary measures to relieve abdominal pain that helped the patients to improve their quality of life and further expand the intervention effect of this nursing mode in IBD.
Self-nursing ability is a kind of ability developed by patients in coping with chronic diseases, including symptom control, intervention monitoring, behavior and emotion regulation, and lifestyle change[17]. Relevant reports indicate that good self-nursing ability can positively affect health outcomes and reduce medical costs[18,19]. Patients with a high level of self-nursing ability can safeguard and enhance their health through their behaviors, monitor and manage signs and symptoms of their diseases, and minimize the impact of diseases on their social functions, emotions, and inter
The follow-up program intervention based on Omaha System for IBD patients in gastrointestinal surgery can improve patients’ disease awareness and intervention compliance, make them face the disease positively, reduce disease activity, and develop their self-nursing ability and quality of life. The limitation of this study is that it is a regressive study with a small sample size, and the results may be biased. It is expected that a large sample and prospective study will further verify the effectiveness of the follow-up protocol based on the Omaha System.
Postoperative follow-up nursing of gastrointestinal surgery patients can effectively improve the quality of life of patients. Currently, a variety of new nursing methods and routine nursing have been widely used in the nursing of gastro
The main content of this study is postoperative follow-up care for gastrointestinal surgery patients. Currently, more effective follow-up care plans are needed to improve the prognosis of gastrointestinal surgery patients. The significance of this study is to affirm the effectiveness of new nursing methods for gastrointestinal surgery patients, encourage clinical teams to continue to explore better nursing methods for gastrointestinal surgery patients, and promote continuous impro
The main objective of this study was to compare the nursing effects of different nursing methods, observe the advantages of the follow-up program based on the Omaha System in the follow-up care of intestinal surgery patients, confirm that the follow-up program based on the Omaha System can effectively improve the disease awareness, treatment compliance, self-care ability and quality of life of gastrointestinal surgery patients, and prove that the nursing method has a good nursing effect. It provides a new reference for postoperative follow-up nursing of gastrointestinal surgery patients.
In this study, data of patients with inflammatory bowel disease in gastrointestinal surgery were retrospectively analyzed and grouped according to nursing methods. Then, independent sample t test, paired sample t test and χ2 test were used to conduct statistical analysis on the general information, disease coping style, disease awareness, quality of life, self-care ability, disease activity and compliance of the two groups of patients. The characteristics of retrospective study are that it is easier to obtain case data by exploring the causes through the results.
The follow-up program based on the Omaha system has a remarkable nursing effect, with better improvements in patients’ disease coping style, disease awareness, quality of life, self-care ability, disease activity and compliance, provi
The postoperative coping style of gastrointestinal surgery patients can affect their prognosis and quality of life, so clinical nursing should pay attention to improving the coping style of patients and strengthening the psychological nursing management. The follow-up plan based on the Omaha System has a good nursing effect, and the best nursing plan should be given priority in clinic.
Follow-up care based on the Omaha System can improve the objective indicators of gastrointestinal surgery patients, while the impact of subjective indicators on patients such as postoperative recovery and complications needs to be further explored.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhansali A, India; Bottalico L, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Marion L, Amélie B, Zoubir D, Guillaume C, Elise MS, Hedia B, Margaux LS, Aude M, Camille BR. Histological Indices and Risk of Recurrence in Crohn's Disease: A Retrospective Study of a Cohort of Patients in Endoscopic Remission. Inflamm Bowel Dis. 2022;28:1395-1404. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Wang SH. [Study on the effect of continuous nursing intervention on the compliance with doctor's orders and disease recurrence rate in patients with ulcerative colitis]. Chinese General Practice. 2019;22. |
| 3. | Wei L, Wang J, Li Z, Zhang Y, Gao Y. Design and implementation of an Omaha System-based integrated nursing management model for patients with newly-diagnosed diabetes. Prim Care Diabetes. 2019;13:142-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, Hayee B, Lomer MCE, Parkes GC, Selinger C, Barrett KJ, Davies RJ, Bennett C, Gittens S, Dunlop MG, Faiz O, Fraser A, Garrick V, Johnston PD, Parkes M, Sanderson J, Terry H; IBD guidelines eDelphi consensus group, Gaya DR, Iqbal TH, Taylor SA, Smith M, Brookes M, Hansen R, Hawthorne AB. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68:s1-s106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1402] [Cited by in RCA: 1568] [Article Influence: 261.3] [Reference Citation Analysis (0)] |
| 5. | Inflammatory Bowel Disease Group; Chinese Society of Gastroenterology; Chinese Medical Association. Chinese consensus on diagnosis and treatment in inflammatory bowel disease (2018, Beijing). J Dig Dis. 2021;22:298-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 6. | Zhang XL, Wang Q, Shen H, Jiang Y, Zeng BF. Minimally invasive two-incision total hip arthroplasty: a short-term retrospective report of 27 cases. Chin Med J (Engl). 2007;120:1131-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Lee KH, Shiu AT. Reliability and validity of the Chinese version of heart disease fact questionnaire. J Clin Nurs. 2012;21:2094-2096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Ruan J, Chen Y, Zhou Y. Development and Validation of a Questionnaire to Assess the Quality of Life in Patients with Inflammatory Bowel Disease in Mainland China. Inflamm Bowel Dis. 2017;23:431-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Gao H, Söderhamn U, Cliffordson C, Guo L, Guo Q, Liu K. Reliability and validity of the Chinese version of the Self-care Ability Scale for the Elderly. J Clin Nurs. 2017;26:4489-4497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Lobatón T, Bessissow T, De Hertogh G, Lemmens B, Maedler C, Van Assche G, Vermeire S, Bisschops R, Rutgeerts P, Bitton A, Afif W, Marcus V, Ferrante M. The Modified Mayo Endoscopic Score (MMES): A New Index for the Assessment of Extension and Severity of Endoscopic Activity in Ulcerative Colitis Patients. J Crohns Colitis. 2015;9:846-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 11. | Kang HB, Li YJ. [Discussion on the clinical application value of the Chinese version of the modified medication belief scale]. Chinese Health Statistics. 2021;38:766-768. [DOI] [Full Text] |
| 12. | D'Amico F, Tasopoulou O, Fiorino G, Zilli A, Furfaro F, Allocca M, Sileri P, Spinelli A, Peyrin-Biroulet L, Danese S. Early Biological Therapy in Operated Crohn's Disease Patients Is Associated With a Lower Rate of Endoscopic Recurrence and Improved Long-term Outcomes: A Single-center Experience. Inflamm Bowel Dis. 2023;29:539-547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 13. | Luo H, Sun Y, Li Y, Lv H, Sheng L, Wang L, Qian J. Perceived stress and inappropriate coping behaviors associated with poorer quality of life and prognosis in patients with ulcerative colitis. J Psychosom Res. 2018;113:66-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Wu HL. [Influence of family-centered personalized nursing model on self-management ability of patients with ulcerative colitis]. Chongqing Med. 2020;425-427. |
| 15. | Sun J, Teng YL. [Application of Omaha system intervention in stroke management]. Chongqing Med. 2019;48. |
| 16. | Zhang M, Lv H, Yang H, Zhang H, Bai X, Qian J. Elderly Patients with Moderate-To-Severe Ulcerative Colitis Are More Likely to Have Treatment Failure and Adverse Outcome. Gerontology. 2023;69:119-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Kamp KJ, West P, Holmstrom A, Luo Z, Wyatt G, Given B. Systematic Review of Social Support on Psychological Symptoms and Self-Management Behaviors Among Adults With Inflammatory Bowel Disease. J Nurs Scholarsh. 2019;51:380-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Knisely MR, Conley YP, Szigethy E. Cytokine Genetic Variants and Health-Related Quality of Life in Crohn's Disease: An Exploratory Study. Biol Res Nurs. 2019;21:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Slipka AF, Monsen KA. Toward Improving Quality of End-of-Life Care: Encoding Clinical Guidelines and Standing Orders Using the Omaha System. Worldviews Evid Based Nurs. 2018;15:26-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Yin S, Ou Y, Ting E. Impacts of Omaha System-Based Continuing Care on the Medication Compliance, Quality of Life, and Prognosis of Coronary Heart Disease Patients After PCI. Braz J Cardiovasc Surg. 2022;37:472-480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 21. | Peng L, Gao Y, Lu R, Zhou R. Efficacy of Omaha system-based nursing management on nutritional status in patients undergoing peritoneal dialysis: A randomized controlled trial protocol. Medicine (Baltimore). 2020;99:e23572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |