Published online Oct 27, 2023. doi: 10.4240/wjgs.v15.i10.2098
Peer-review started: May 30, 2023
First decision: July 18, 2023
Revised: August 1, 2023
Accepted: August 17, 2023
Article in press: August 17, 2023
Published online: October 27, 2023
Processing time: 149 Days and 16.1 Hours
Postcholecystectomy bile duct injury (BDI) remains a devastating iatrogenic complication that adversely impacts the quality of life with high healthcare costs. Despite a decrease in the incidence of laparoscopic cholecystectomy-related BDI, the absolute number remains high as cholecystectomy is a commonly performed surgical procedure. Open Roux-en-Y hepaticojejunostomy with meticulous surgi
Core Tip: Minimally invasive postcholecystectomy biliary stricture repair is an attractive and controversial option to manage this iatrogenic injury with serious health and litigation consequences. Recent evidence suggests a potential role of minimally invasive approaches especially robotic surgery. Refinements in minimally invasive techniques can widen the scope of minimally invasive surgery. Future studies should overcome the current evidence's limitations and help choose the most suitable method for repair in a patient with bile duct injury.
- Citation: Kalayarasan R, Sai Krishna P. Minimally invasive surgery for post cholecystectomy biliary stricture: current evidence and future perspectives. World J Gastrointest Surg 2023; 15(10): 2098-2107
- URL: https://www.wjgnet.com/1948-9366/full/v15/i10/2098.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i10.2098
Iatrogenic post-cholecystectomy bile duct injury (BDI) resulting in biliary stricture is a devastating complication for any patient who experiences it and can be a nightmare to the surgeon responsible for it. The incidence of BDI following laparoscopic cholecystectomy is about 0.2% to 0.6% and slightly less following an open cholecystectomy (0.1%-0.2%)[1,2]. Recent series have shown comparable incidences of BDI between open and laparoscopic cholecystectomy[2,3]. However, considering the number of cholecystectomies done for gallstone disease worldwide, even this lower incidence turns into a substantial absolute number. On admission for elective laparoscopic cholecystectomy, often done as an outpatient procedure, the patient expects a prompt postoperative recovery. Hence, consequences of BDI like large abdominal incisions, the need for multiple drains and stents, a prolonged hospital stay, and the inability to continue routine work make it difficult for the patient to accept, often ending with litigations against the operating surgeon[4,5].
The implication of postcholecystectomy biliary stricture on quality of life mandates a meticulous surgical repair with utmost care. Roux-en-Y hepaticojejunostomy (RYHJ) is the gold standard surgical treatment for benign biliary stricture[5,6]. The reported success rate at 30 mo follow up period is as high as 80%-90%[6]. Conventionally, an open approach is used for performing RYHJ in postcholecystectomy biliary stricture patients. A minimally invasive approach for repairing postcholecystectomy biliary stricture is considered controversial as often the injury is a consequence of a laparoscopic approach. However, in recent years, the application of laparoscopy has yielded promising results in managing complex biliary tract diseases, including the repair of iatrogenic bile duct injuries[7-10]. Also, the robotic platform with a stable camera, tremor filtration, immersive 3-dimensional imaging, intuitive movement of surgeon’s wrist, and enhanced dexterity allow the performance of complex procedures with increased precision[11-13]. Better cosmetic outcomes and early postoperative recovery with laparoscopic and robotic approaches could decrease the patient’s attitude towards litigations[11]. However, literature on laparoscopic and robotic approaches for managing postcholecystectomy biliary stricture is still limited. The current evidence is reviewed to give an overview of the minimally invasive management of postcholecystectomy biliary strictures and future perspectives.
Both authors independently did a PubMed search of relevant articles. Further, the reference lists of selected manuscripts were searched for additional appropriate studies. The keywords and combinations included in the search were: “Bile leak”; OR “hepaticojejunostomy”; OR “biliary anastomosis”; OR “bile duct injury repair”; OR “iatrogenic bile duct injury”; OR “biliary anastomosis,” OR “laparoscopic cholecystectomy”; “hepaticojejunostomy” AND “laparoscopic”; “hepaticojejunostomy” AND “robotic”. The search was limited to publications in English literature till March 2023. Case reports and case series with less than five patients were not included in the review. All the authors agreed that the articles selected for review were relevant.
The fundamental principles of surgical repair in a patient with postcholecystectomy biliary stricture are exposure of well-vascularized ducts, tension-free anastomosis and drainage of all segments[6]. While the principles of surgical repair remain the same in both open and minimally invasive approaches, the critical differences in operative steps between both approaches are highlighted in this section. In most series, elective repair is undertaken after a waiting period of 6-10 wk or even longer if an uncomplicated external biliary fistula is present[10-12]. Several case studies report applying minimally invasive methods for the on-table repair of BDI[10-12]. However, the availability of expert Hepato-Pancreato-Biliary surgeons to repair BDI is a challenge and can be considered in the presence of adequate expertise. Also, the rate of conversion to open surgery is high (31%) for on-table BDI repair[11,12]. As a minimally invasive approach is still not a standard technique to repair benign biliary stricture, appropriate informed consent and shared decision making is imperative.
The patient is positioned supine or supine with a leg split, with the operating surgeon standing on the left side of the patient or between the patient’s legs. Trocar position is determined after creating the pneumoperitoneum and initial exploratory laparoscopy. In the laparoscopic approach, commonly, five trocars are placed in a semi-circular line at the level of the umbilicus[9,10]. In patients undergoing robotic repair, four robotic trocars are placed in a straight line at the level of the umbilicus, with an assistant trocar placed in the infraumbilical region.
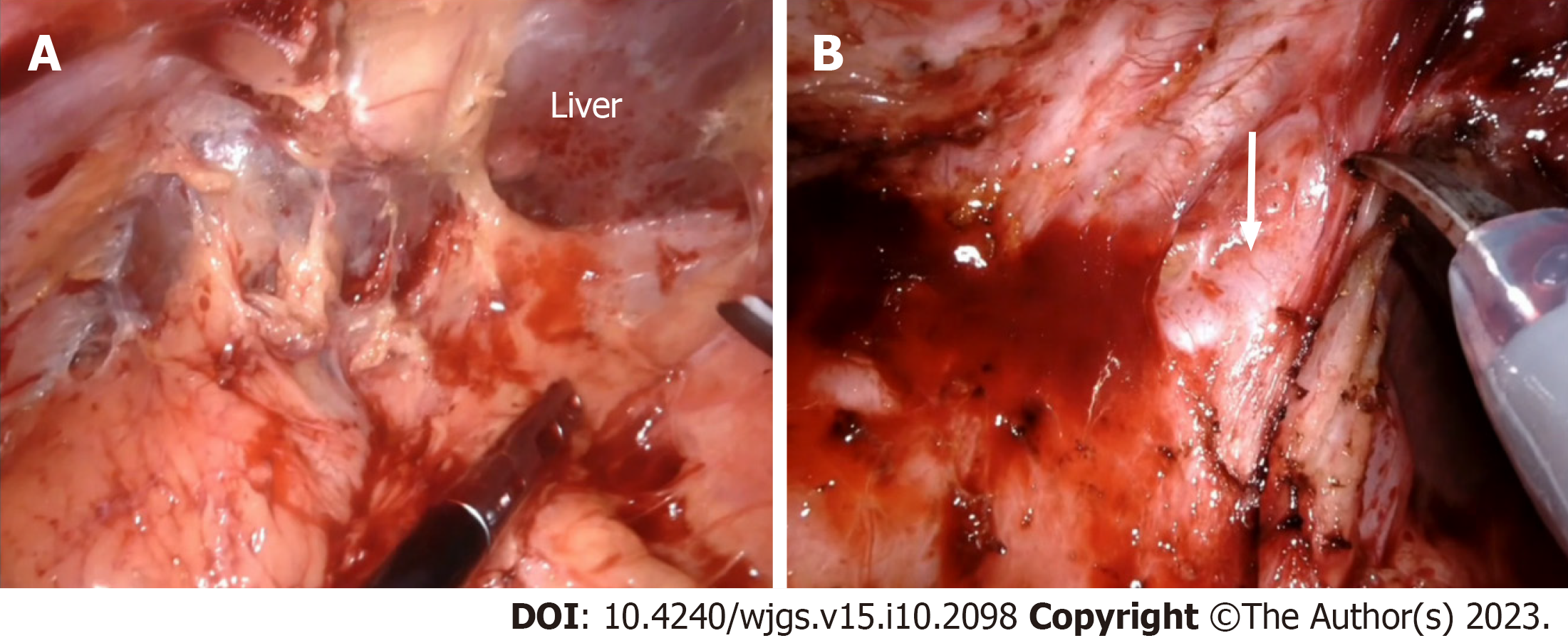
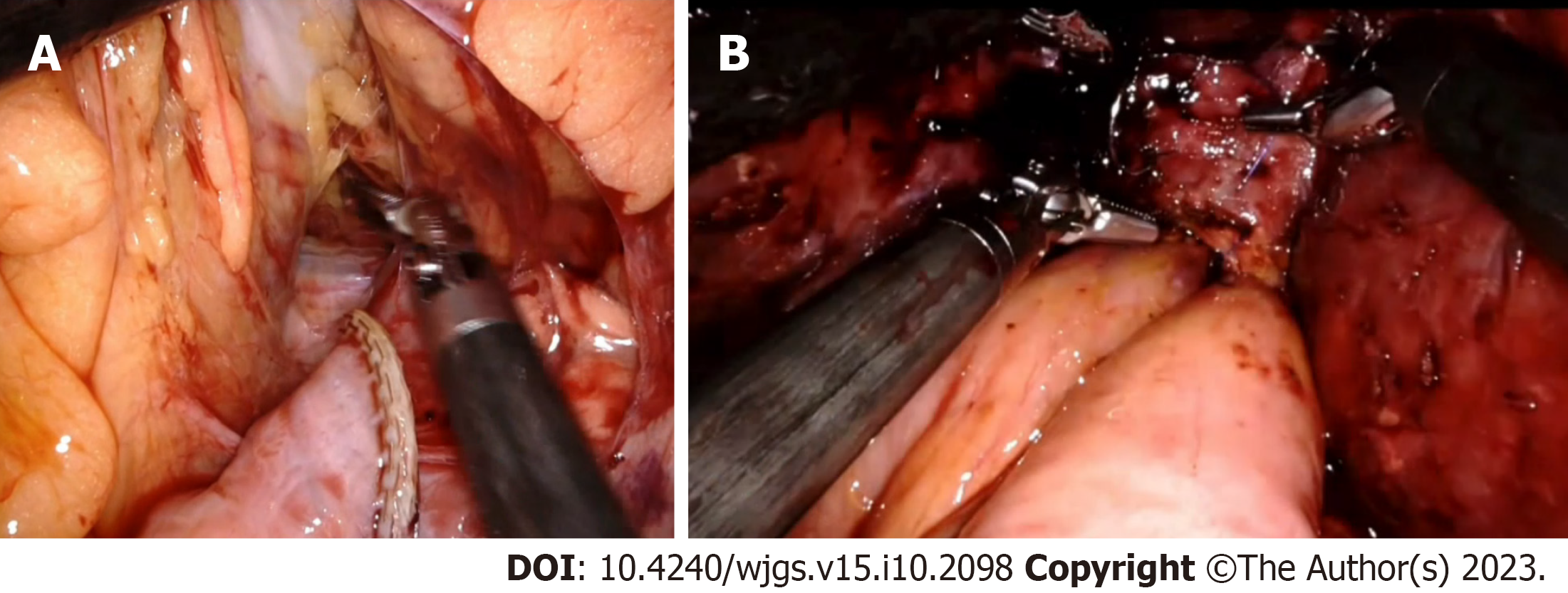
Most patients with postcholecystectomy biliary have dense intra-abdominal adhesions that require careful adhesiolysis. In open surgery, perihepatic adhesions are completely released before reaching the hepatic hilum. Whereas in minimally invasive surgery, perihepatic adhesions, if present, are left undisturbed because they serve as a natural source of liver retraction facilitating exposure and dissection of the hilum (Figure 1)[10]. In biliary stricture patients undergoing robotic repair, docking of the robotic arms is usually done after laparoscopic intra-abdominal adhesiolysis.
The dissection started in the inferior surface of the liver to identify the base of segment four. Gastro hepatic ligament is taken down to facilitate the same. Dissection proceeds towards the umbilical fissure with careful identification and preservation of the left hepatic artery, as this may be the sole artery supplying the liver and bile duct in patients with associated right hepatic artery injury (Figure 1). The lack of tactile sensation of palpating blood vessels in minimally invasive surgery is compensated by visualization of pulsations under magnified vision[11,12]. While intravenous indocyanine green (ICG) can be used to identify the blood vessels, it is often used to determine the ductal anatomy.
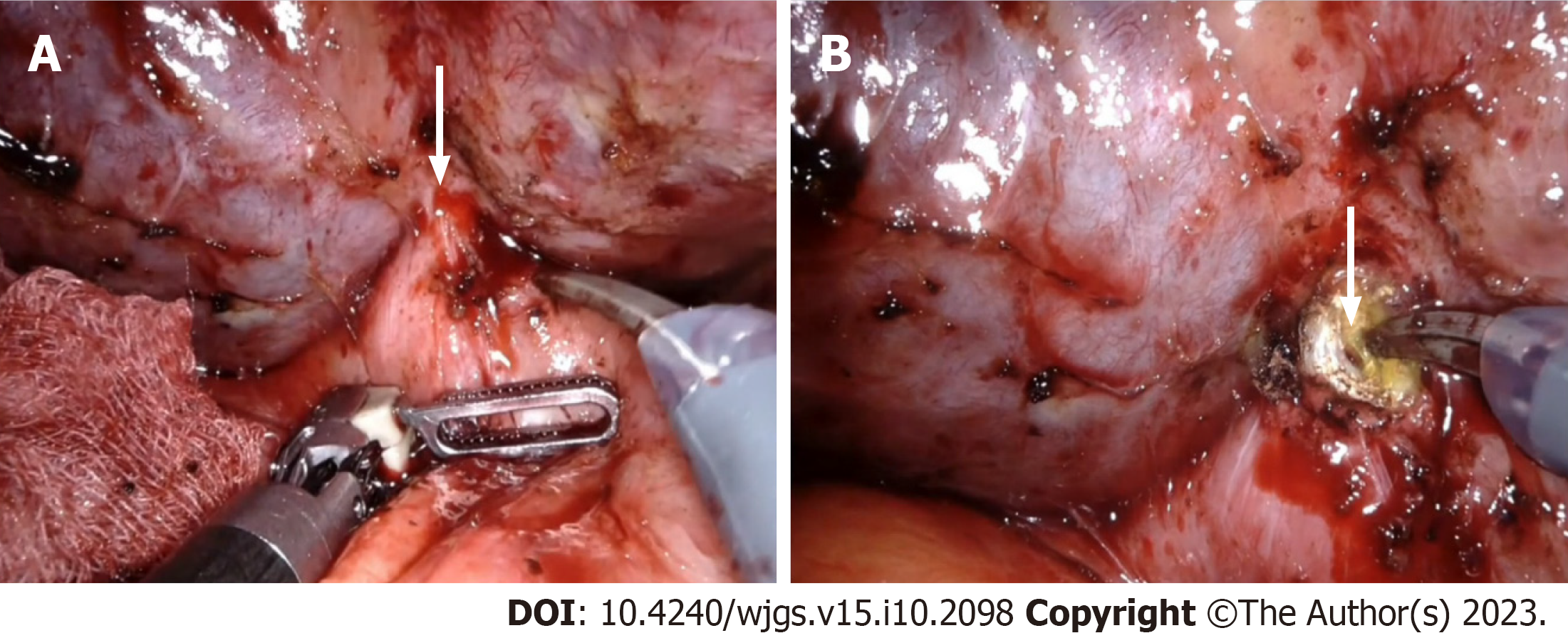
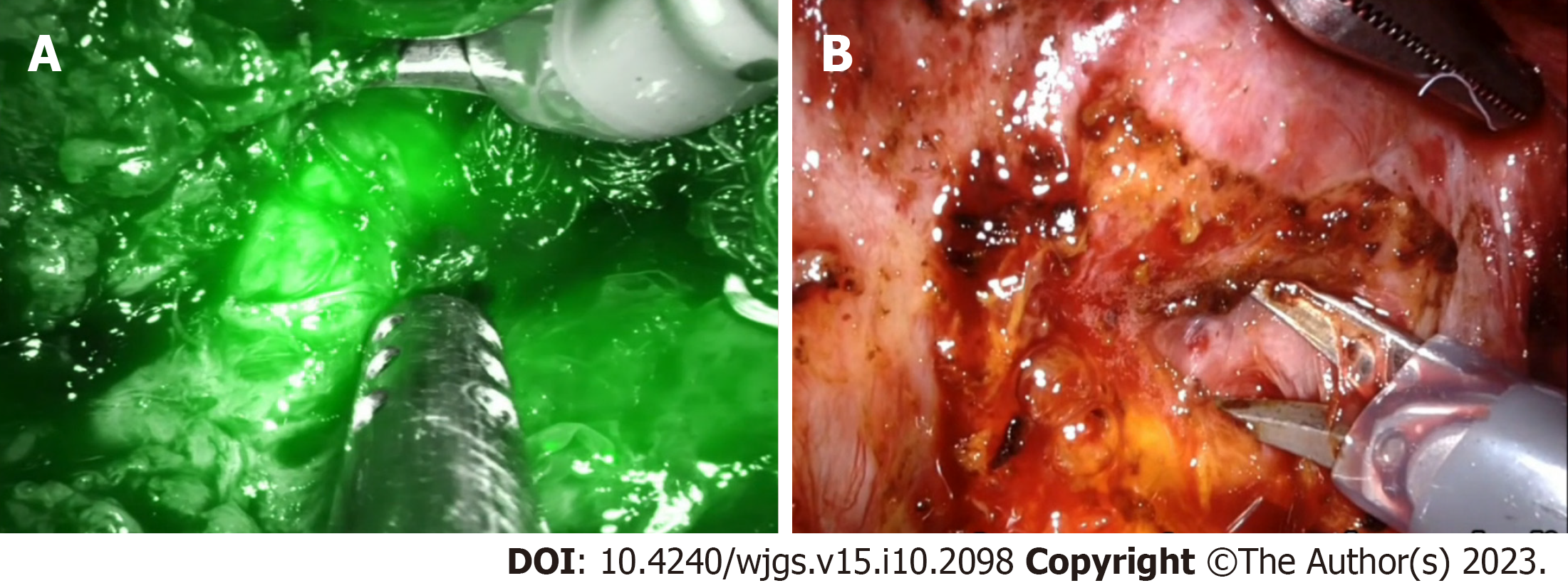
After delineation of the porta hepatis, the next step is identifying the left hepatic duct and lowering the hilar plate. In patients with internal fistula, frequently with the duodenum, dismantling the fistula facilitates duct identification (Figure 2). ICG is frequently used in minimally invasive approaches to identify the hepatic ducts (Figure 3). Identification of biliary anatomy is facilitated by intravenous injection at least 6 h before the procedure to minimize background liver fluorescence. However, background fluorescence interferes with ductal anatomy delineation once an intraoperative bile leak occurs.
Lowering the hilar plate is achieved by dissection between the Glissonean sheath surrounding portal structures and Laennec’s capsule surrounding the liver (Figure 3). Magnified vision in a minimally invasive approach facilitates the identification of the correct plane to lower the hilar plate. Once the left hepatic duct is identified, it is widely opened, and its confluence with the right hepatic duct is defined (Figure 4). In patients with type IV and V stricture, coring of hilar liver tissue or partial resection of segment IV may be required to have good exposure to the ducts. Delineation of the distal bile duct is neither required nor recommended, as it may result in vascular injury.
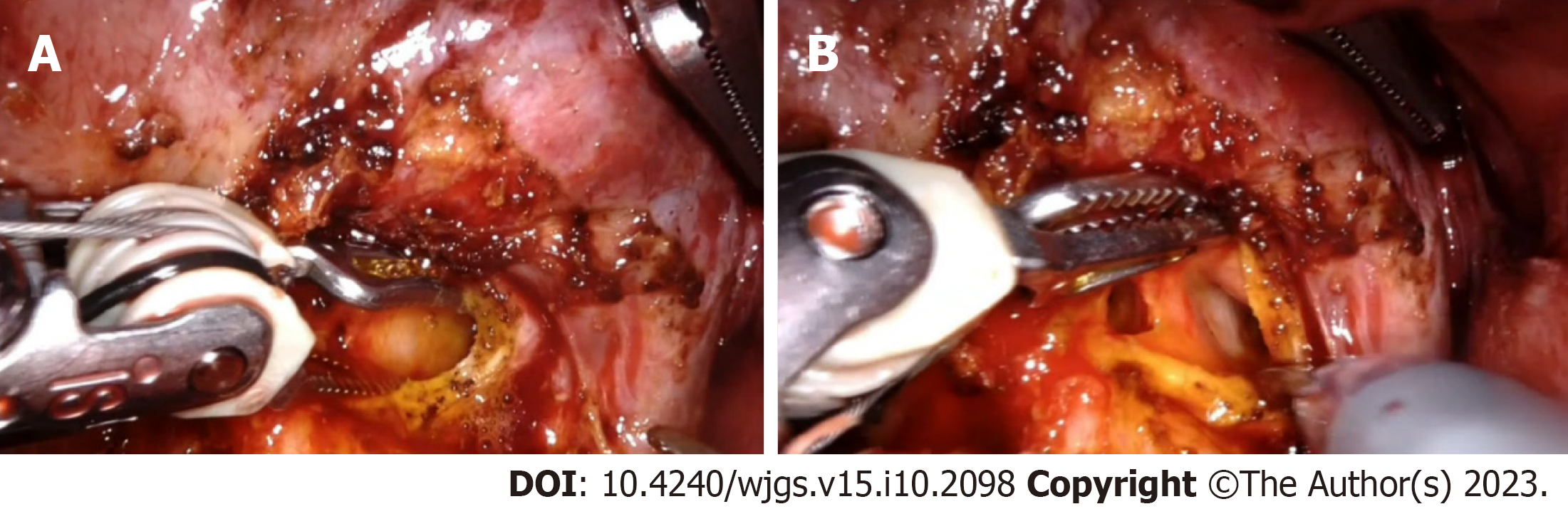
The loop of the jejunum about 30 cm from the duodenojejunal flexure is identified and divided using an endoscopic bowel stapler. Creation of a Roux limb can be technically challenging, especially in a robotic approach due to changes in the quadrant. Similarly, the creation of a mesocolic window in minimally invasive surgery is complex in patients with extensive periduodenal adhesions and inflammation. A wide side-to-side tension-free hepaticojejunostomy to the healthy bile duct, ensuring complete drainage of all the bile ducts, is a crucial step of the surgical procedure (Figure 5). Due to difficulty in handling multiple sutures, stay sutures on the hepatic duct are not commonly used in a minimally invasive approach. Also, continuous sutures are frequently used in minimally invasive surgery, especially the laparoscopic approach[8-10]. Absorbable suture materials are preferred for anastomosis. As in the open technique, 3-0 or 4-0 polydioxanone sutures are commonly used to create hepaticojejunostomy. Barbed sutures, initially used in tendon repair to reduce the need for knot tying and increase gripping strength, are increasingly used in minimally invasive pancreatobiliary surgeries, including BDI repair for anastomosis. Avoidance of repeated suture tightening and traction after each stitch during continuous suturing is the primary advantage of barbed sutures. However, more evidence is required regarding its safety in BDI repair, especially in patients with thin bile ducts.
Preservation of perihepatic adhesions, frequent use of ICG to delineate ducts and anastomosis technique are some of the critical technical differences in the minimally invasive repair of postcholecystectomy biliary stricture compared to open RYHJ.
The feasibility of laparoscopic repair of postcholecystectomy biliary stricture was first reported in 2002 by Crema et al[14]. Despite the encouraging results, the laparoscopic approach was not widely used, and publications were limited only to case reports. Apprehension of abdominal adhesion due to previous bile leak and technical challenges in dissecting the scarred tissues were the primary reasons for surgeon’s hesitation to adopt a minimally invasive approach. In 2016, Cuendis-Velázquez et al[7] published the first laparoscopic reconstruction series, which included 29 patients with post-cholecystectomy biliary strictures. The authors have given a detailed description of the procedure and reported excellent outcomes with minimal morbidity. During a median follow-up of 36 mo, one patient developed hepatico-jejunostomy stricture requiring endoscopic intervention. While most laparoscopic series had a single study arm, Javed et al[10], in a retrospective study, compared the outcomes of 29 patients who underwent laparoscopic repair with 34 patients who underwent open RYHJ. More than three fourth of patients in both groups had high strictures (Strasberg E3, E4 and E5 types). While median operative time was comparable between the two groups (210 vs 200 min, P = 0.93), the mean blood loss (50 vs 200 mL, P = 0.001), time to resume oral diet (2 vs 4 d, P= 0.023), and duration of hospital stay (6 vs 8 d, P = 0.04) were significantly less in the laparoscopic group. While all patients in the open group underwent RYHJ, hepaticoduodenostomy for biliary reconstruction was used in more than half of the patients included in the laparoscopic group. Median operative time (190 vs 230 min, P = 0.034) was significantly less in the laparoscopic hepaticoduodenostomy group as it requires single anastomosis compared to additional small bowel anastomosis with hepaticojejunostomy.
Hepaticoduodenostomy is commonly used for reconstruction following choledochal cyst excision in the pediatric age group[15-17]. However, its use in postcholecystectomy biliary stricture is documented only in a single series[10]. Authors suggested that in patients with choledochoduodenal fistula or those with dense adhesion of the duodenum to the hilum, hepaticoduodenostomy can be safely performed without difficulties in mobilizing the duodenal knuckle. Hepaticoduodenostomy is primarily used in Strasberg E1-2 and some E3 strictures. In addition to the single anastomosis, the feasibility of the endoscopic intervention in patients with postoperative stricture is an added advantage of hepaticoduodenostomy. More severe presentation of anastomotic leak compared to hepaticojejunostomy is the primary risk with hepaticoduodenostomy. As the current evidence is limited, more studies are required to document the safety of hepaticoduodenostomy in patients with a postcholecystectomy biliary stricture. A few other series published from high-volume centres with significant experience in advanced laparoscopic hepatobiliary procedures report that the laparoscopic approach may be equivalent, if not better, for managing post-cholecystectomy biliary strictures[18-21]. Published laparoscopic case series with at least ten patients included in the analysis are summarized in Table 1.
| Ref. | Year | Patients | Strasberg injury type | Method of reconstruction | Mean operative time (min) | Blood loss (mL) | Conversion to open | Overall morbidity | Specific biliary complications | Length of stay (d) | Follow up |
| Cuendis- | 2016 | 29 | C, E1-E4 | HJ | 240 | 200 | 1 | 31.03 | Bile leak–5 patients. One patient required laparotomy and drainage of bile collection | 8 | 36 (range 7-36) mon, Anastomotic patency rate 96.6% |
| Gomez et al[9] | 2020 | 20 | E1-E4 | HJ | 146.5 | 15-50 | None | 10% | One patient had bile leak and was managed conservatively | 4.5 (mean) | 5 yr–no long-term complications |
| Sahoo et al[8] | 2021 | 16 | HJ | 280 | 176 | None | 12.5% | Two patients had bile leak and were managed conservatively | 8.5 | 28 mo | |
| Javed et al[10] | 2021 | 29 | E1-E5 | HJ-13 patients, HD-16 patients | 210 | 50 | None | 20% | Four patients had bile leak and were managed conservatively | 6 | 9 mo–one patient had anastomotic strictest and managed with repeater dilations |
With the development of Devol's first robotic machines using a magnetic process controller in the 1940s, robotic surgery made immense progress in recent years[22]. Since the first robotic cholecystectomy performed by Himpens in 1997, the use of robotics in hepatobiliary and pancreatic surgery, including complex surgeries, has shown noticeable growth[23,24].The initial case series on the use of robots for biliary stricture repair was published by Giulianotti et al[11] in 2018, which analyzed fourteen patients. Interestingly, 42.9% of included patients had Bismuth type II injuries underscoring the careful selection of patients for the robotic approach in the initial phase. However, complex reconstructions were also performed in their series. Two patients, one with isolated right hepatic duct stricture and the other with type IV stricture because of small duct size, underwent Robotic assisted Kasai procedure. One patient with previous Roux en-y gastric bypass underwent dismantling of gastric bypass, sleeve gastrectomy of the remnant stomach, and an anastomosis between the gastric pouch and sleeve gastrectomy portion with the use of Roux limb for biliary anastomosis. The authors highlighted the potential advantage of the robotic approach over the laparoscopic repair of bile duct injuries: improved magnification (10X), enhanced range of motion, ambidextrous handling with precise dissection and tremor filtration with better ergonomics. The study concluded that robot-assisted biliary reconstruction for postcholecystectomy biliary stricture is feasible and safe in expert hands[11]. Marino et al[12] published the only prospective series on Robotic assisted repair of biliary stricture in 2019. Twelve patients who underwent robotic repair from 2014 to 2017 were analyzed. However, the duration of follow-up was only 12 mo. Sucandy et al[13] compared the robotic approach with open surgery and reported less blood loss in the robotic group (50 vs 150 mL). However, the study had only eight patients in the robotic arm. Since then, a few other series have documented the usefulness of the robotic approach, although the number of patients included was small with a short follow-up period[25-27]. Published robotic case series with at least five patients included in the analysis are summarized in Table 2[12].
| Ref. | Year | Patients | Strasberg injury type | Method of reconstruction | Operative time (min) | Blood loss (mL) | Overall morbidity | Length of stay (d) | Specific complications | Follow up |
| Giulianotti et al[11] | 2018 | 14 | E1-E5 | HJ-12 patients, Kasai procedure-2 patients | 280.6 | 135 | 28.6% | 8.4 | Bile leak-two patients and 1 patient required pigtail catheter insertion. Subhepatic abscess-one patient | 36.1 mo, 2 patients had mild HJ stenosis and cholangitis. Managed by PTBD and multiple transhepatic dilatations |
| Marino et al[12] | 2019 | 12 | E1-E4 | HJ | 260 | 252 | 16.7% | 9.4 | 1 patient developed subhepatic abscess and required pigtail catheter insertion | 12 mo–1 patient had anastomotic stenosis and revision robotic HJ was done |
| Sucandyet al[13] | 2021 | 8 | HJ | 259 | 50 | 14% | 8 | None | 22 mo–1 patient had anastomotic stenosis at 10 mo and required transhepatic dilatation |
Only one study compared the outcomes of two minimally invasive approaches for biliary reconstruction in post-cholecystectomy biliary stricture patients[28]. Of the 75 patients included in the study 40 were managed laparoscopically, and 35 underwent robotic reconstruction. The BDI types were as follows: E1 (7.5% vs 14.3%), E2 (22.5% vs 14.3%), E3 (40% vs 42.9%), E4 (22.5% vs 28.6%), and E5 (7.5% vs 0), for laparoscopic hepaticojejunostomy and robotic-assisted hepaticojejunostomy respectively. The blood loss, operative times, length of hospital stay and anastomotic patency rate at the 90-day index period were comparable between the two groups (Table 3). Though overall morbidity and anastomotic patency rate were slightly superior in the robotic group, the difference was not statistically significant. The authors concluded that both minimally invasive approaches are safe and effective for biliary reconstruction in a high-volume centre[28]. However robotic approach has technical superiority over the laparoscopic approach. As the duration of follow-up was different in the two groups, the 90-day-index treatment period rather than the actuarial anastomotic patency rate was compared, which is a limitation of the study. Also, the selection of patients for the robotic and laparoscopic approach was based on the availability of the equipment, which could result in selection bias. A cost-effective analysis between the two approaches was not performed as the robot adds cost to the surgical procedure.
| Ref. | Year | Patients | Strasberg injury type | Method of reconstruction | Mean operative time (min) | Blood loss (mL) | Conversion to open | Overall morbidity | Specific complications | Length of stay (d) | Follow up (mo) |
| Cuendis-Velázquez et al[28] | 2019 | 75 (laparoscopic–40, robotic–35) | E1-E5 | Roux-en-Y hepaticojejunostomy | Laparoscopic–240, Robotic–270 | Laparoscopic–215, Robotic–150 | 1 patient in laparoscopic group due to dense adhesions | Laparoscopic–27.5, Robotic–22.8 | Bile leak, laparoscopic–2 patients, robotic–1 patient, one patient in each group underwent laparotomy, lavage with additional drain placement for bile leak | Laparoscopic–7, Robotic–6 | Laparoscopic–49, anastomotic patency rate–92.5%, robotic–16, anastomotic patency rate–100% |
Although minimally invasive surgery has gained immense popularity in recent years for treating various hepatobiliary and pancreatic disorders, it has limitations, especially in complex procedures[29]. The technical drawbacks related to the laparoscopic approach are an unsteady surgical field, restricted degrees of freedom of movement, a steep learning curve and difficulties in complex suturing[30]. The complexity of the surgery and the steep learning curve comes from the fact that most patients with BDI would have suffered a bile leak and peritonitis, resulting in extensive adhesions, and altered anatomy[30,31]. Also, most patients with BDI have complex strictures (Strasberg E3-E5 types). The need to anastomose delicate and supple lobar ducts to the jejunum necessitates steady vision and a high degree of laparoscopic suturing skills. Difficulty in handling multiple sutures during minimally invasive surgery results in increased usage of continuous suture technique. While meta-analysis comparing two suture techniques has reported comparable outcomes, the evidence in the setting of postcholecystectomy biliary stricture is limited[32]. Hence, the long-term patency rate with the continuous suture technique commonly used in minimally invasive surgery must be analyzed. As documented in most studies, laparoscopic repair of postcholecystectomy biliary stricture was performed by surgeons who have completed more than 30 complex hepatopancreatobiliary surgeries, including laparoscopic Whipple’s procedure[18]. On the other hand, the robotic repair of biliary strictures has documented advantages over the laparoscopic approach in terms of magnification, stable vision, and a greater degree of freedom of movement with ease of intracorporeal suturing[11]. However, robotic repair of biliary stricture is not without limitations, the foremost being the availability of equipment, high equipment and maintenance costs restricting its availability to a few centres. Undoubtedly robotic approach increases the treatment cost for patients with severe economic hardships due to the disease.
Regarding drawbacks in the published literature on minimally invasive surgery, most studies were retrospective analyses with several reporting biases. The diagnostic criteria for postoperative complications, timing, and duration of follow-up were non-homogenous. It eventually translated to difficulty in acquiring raw data for some long-term follow-up parameters, including the anastomotic patency rate. Upcoming studies have to consider reporting long-term follow-up and ten year patency rates of bilio-enteric anastomosis, which could confirm the better quality of life with the minimally invasive repair of BDI.
Studies published in the last five years, despite their limitations, provide hope that minimally invasive procedures could play a greater role in the management, thereby offering short- and long-term advantages to patients experiencing this devastating complication. The availability and expertise of a hepatobiliary surgeon are of prime importance in managing BDI patients, and the application of minimally invasive procedures would complement the surgery results. As minimally invasive surgery can be relatively easily employed in patients with Strasberg E1-E3 strictures, future prospective trials should compare open and minimally invasive approaches in this subgroup of patients. As postcholecystectomy biliary stricture repair requires fine dissection in a small, narrow operating field along with extreme accuracy in suture place
Open surgical repair remains the gold standard for managing postcholecystectomy biliary stricture, a dreadful compli
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: International Hepato-Pancreato Biliary Association, No.M02056.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Bencini L, Italy; Głuszyńska P Poland; Shelat VG, Singapore; Sugimoto M, Japan S-Editor: Lin C L-Editor: A P-Editor: Xu ZH
| 1. | Alexander HC, Bartlett AS, Wells CI, Hannam JA, Moore MR, Poole GH, Merry AF. Reporting of complications after laparoscopic cholecystectomy: a systematic review. HPB (Oxford). 2018;20:786-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Kaman L, Sanyal S, Behera A, Singh R, Katariya RN. Comparison of major bile duct injuries following laparoscopic cholecystectomy and open cholecystectomy. ANZ J Surg. 2006;76:788-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Fletcher R, Cortina CS, Kornfield H, Varelas A, Li R, Veenstra B, Bonomo S. Bile duct injuries: a contemporary survey of surgeon attitudes and experiences. Surg Endosc. 2020;34:3079-3084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Booij KAC, de Reuver PR, van Dieren S, van Delden OM, Rauws EA, Busch OR, van Gulik TM, Gouma DJ. Long-term Impact of Bile Duct Injury on Morbidity, Mortality, Quality of Life, and Work Related Limitations. Ann Surg. 2018;268:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 5. | Schreuder AM, Busch OR, Besselink MG, Ignatavicius P, Gulbinas A, Barauskas G, Gouma DJ, van Gulik TM. Long-Term Impact of Iatrogenic Bile Duct Injury. Dig Surg. 2020;37:10-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 6. | Marichez A, Adam JP, Laurent C, Chiche L. Hepaticojejunostomy for bile duct injury: state of the art. Langenbecks Arch Surg. 2023;408:107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 7. | Cuendis-Velázquez A, Morales-Chávez C, Aguirre-Olmedo I, Torres-Ruiz F, Rojano-Rodríguez M, Fernández-Álvarez L, Cárdenas-Lailson E, Moreno-Portillo M. Laparoscopic hepaticojejunostomy after bile duct injury. Surg Endosc. 2016;30:876-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Sahoo MR, Ali MS, Sarthak S, Nayak J. Laparoscopic hepaticojejunostomy for benign biliary stricture: A case series of 16 patients at a tertiary care centre in India. J Minim Access Surg. 2022;18:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Goméz D, Cabrera LF, Pedraza-Ciro M, Mendoza A, Pulido J. Laparoscopic Roux-en-Y hepaticojejunostomy reconstruction after iatrogenic bile duct injury: case series report. Cir Cir. 2020;88:608-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Javed A, Shashikiran BD, Aravinda PS, Agarwal AK. Laparoscopic versus open surgery for the management of post-cholecystectomy benign biliary strictures. Surg Endosc. 2021;35:1254-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 11. | Giulianotti PC, Quadri P, Durgam S, Bianco FM. Reconstruction/Repair of Iatrogenic Biliary Injuries: Is the Robot Offering a New Option? Short Clinical Report. Ann Surg. 2018;267:e7-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Marino MV, Mirabella A, Guarrasi D, Lupo M, Komorowski AL. Robotic-assisted repair of iatrogenic common bile duct injury after laparoscopic cholecystectomy: Surgical technique and outcomes. Int J Med Robot. 2019;15:e1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 13. | Sucandy I, Jabbar F, Syblis C, Crespo K, App S, Ross S, Rosemurgy A. Robotic Versus Open Extrahepatic Biliary Reconstruction for Iatrogenic Bile Duct Injury. Am Surg. 2022;88:345-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Crema E, Silva AA, Lenza RM, de Oliveira CB, Bridi VA, Martins A Jr. Excluded-loop hepatojejunal anastomosis with use of laparoscopy in late management of iatrogenic ligature of the bile duct. Surg Laparosc Endosc Percutan Tech. 2002;12:110-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Yeung F, Chung PH, Wong KK, Tam PK. Biliary-enteric reconstruction with hepaticoduodenostomy following laparoscopic excision of choledochal cyst is associated with better postoperative outcomes: a single-centre experience. Pediatr Surg Int. 2015;31:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Yeung F, Fung ACH, Chung PHY, Wong KKY. Short-term and long-term outcomes after Roux-en-Y hepaticojejunostomy versus hepaticoduodenostomy following laparoscopic excision of choledochal cyst in children. Surg Endosc. 2020;34:2172-2177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Narayanan SK, Chen Y, Narasimhan KL, Cohen RC. Hepaticoduodenostomy versus hepaticojejunostomy after resection of choledochal cyst: a systematic review and meta-analysis. J Pediatr Surg. 2013;48:2336-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Dokmak S, Amharar N, Aussilhou B, Cauchy F, Sauvanet A, Belghiti J, Soubrane O. Laparoscopic Repair of Post-cholecystectomy Bile Duct Injury: an Advance in Surgical Management. J Gastrointest Surg. 2017;21:1368-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Chowbey PK, Soni V, Sharma A, Khullar R, Baijal M. Laparoscopic hepaticojejunostomy for biliary strictures: the experience of 10 patients. Surg Endosc. 2005;19:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Julian D, Martín S, Martín P, Rodrigo SC, Guillermo A, Oscar M, Juan P. Role of laparoscopy in the immediate, intermediate, and long-term management of iatrogenic bile duct injuries during laparoscopic cholecystectomy. Langenbecks Arch Surg. 2022;407:663-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Gupta V, Jayaraman S. Role for laparoscopy in the management of bile duct injuries. Can J Surg. 2017;60:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Abbott P. The McGraw‐Hill Illustrated Encyclopedia of Robotics and Artificial Intelligence. Assem Autom. 1998;18:89-89. [DOI] [Full Text] |
| 23. | Himpens J, Leman G, Cadiere GB. Telesurgical laparoscopic cholecystectomy. Surg Endosc. 1998;12:1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 152] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 24. | Shukla A, Gnanasekaran S, Kalayarasan R, Pottakkat B. Early experience with robot-assisted Frey's procedure surgical outcome and technique: Indian perspective. J Minim Invasive Surg. 2022;25:145-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (2)] |
| 25. | Prasad A, De S, Mishra P, Tiwari A. Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. World J Gastroenterol. 2015;21:1703-1706. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Cuendis-Velázquez A, Bada-Yllán O, Trejo-Ávila M, Rosales-Castañeda E, Rodríguez-Parra A, Moreno-Ordaz A, Cárdenas-Lailson E, Rojano-Rodríguez M, Sanjuan-Martínez C, Moreno-Portillo M. Robotic-assisted Roux-en-Y hepaticojejunostomy after bile duct injury. Langenbecks Arch Surg. 2018;403:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 27. | D'Hondt M, Wicherts DA. Robotic biliary surgery for benign and malignant bile duct obstruction: a case series. J Robot Surg. 2023;17:55-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Cuendis-Velázquez A, Trejo-Ávila M, Bada-Yllán O, Cárdenas-Lailson E, Morales-Chávez C, Fernández-Álvarez L, Romero-Loera S, Rojano-Rodríguez M, Valenzuela-Salazar C, Moreno-Portillo M. A New Era of Bile Duct Repair: Robotic-Assisted Versus Laparoscopic Hepaticojejunostomy. J Gastrointest Surg. 2019;23:451-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG; Dutch Pancreatic Cancer Group. Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 2019;4:199-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 409] [Article Influence: 68.2] [Reference Citation Analysis (0)] |
| 30. | Cubisino A, Dreifuss NH, Cassese G, Bianco FM, Panaro F. Minimally invasive biliary anastomosis after iatrogenic bile duct injury: a systematic review. Updates Surg. 2023;75:31-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Guerra F, Coletta D, Gavioli M, Coco D, Patriti A. Minimally invasive surgery for the management of major bile duct injury due to cholecystectomy. J Hepatobiliary Pancreat Sci. 2020;27:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Hajibandeh S, Hajibandeh S, Parente A, Bartlett D, Chatzizacharias N, Dasari BVM, Hartog H, Perera MTPR, Marudanayagam R, Sutcliffe RP, Roberts KJ, Isaac JR, Mirza DF. Meta-analysis of interrupted versus continuous suturing for Roux-en-Y hepaticojejunostomy and duct-to-duct choledochocholedochostomy. Langenbecks Arch Surg. 2022;407:1817-1829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Lopez-Lopez V, Maupoey J, López-Andujar R, Ramos E, Mils K, Martinez PA, Valdivieso A, Garcés-Albir M, Sabater L, Valladares LD, Pérez SA, Flores B, Brusadin R, Conesa AL, Cayuela V, Cortijo SM, Paterna S, Serrablo A, Sánchez-Cabús S, Gil AG, Masía JAG, Loinaz C, Lucena JL, Pastor P, Garcia-Zamora C, Calero A, Valiente J, Minguillon A, Rotellar F, Ramia JM, Alcazar C, Aguilo J, Cutillas J, Kuemmerli C, Ruiperez-Valiente JA, Robles-Campos R. Machine Learning-Based Analysis in the Management of Iatrogenic Bile Duct Injury During Cholecystectomy: a Nationwide Multicenter Study. J Gastrointest Surg. 2022;26:1713-1723. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |