Published online Aug 27, 2022. doi: 10.4240/wjgs.v14.i8.778
Peer-review started: April 6, 2022
First decision: April 25, 2022
Revised: May 10, 2022
Accepted: July 27, 2022
Article in press: July 27, 2022
Published online: August 27, 2022
Processing time: 140 Days and 1.5 Hours
The prevalence of constipation in the Chinese population over 60 years of age is 11.5%, and this prevalence increases with age, which seriously affects the quality of life in older adults. Therefore, reducing the incidence of constipation in older adults is necessary to promote a healthy lifestyle as well as biochemical health.
To explore the value of preoperative guidance and education to improve the effects of bowel cleaning in older adult patients undergoing colonoscopy.
In this study, 160 older adult patients with constipation requiring colonoscopy at Shandong Provincial Hospital between January 2019 and March 2021 were selected and randomly divided into a study group and a control group, with 80 patients in each group. The study group received medication guidance and targeted educational guidance before the operation, while the control group received only medication and dietary guidance. The baseline data, colonoscopy duration, bowel preparation compliance, Boston bowel preparation (BBPS) assessment score, intestinal bubble score, the incidence of adverse reactions during bowel preparation, and nursing appointment satisfaction were compared between the two groups.
The colonoscopy duration times and intestinal bubble scores of the study group were shorter than those of the control group, with statistically significant differences. The BBPS scores for the right, left, and interrupted colon in the study group were also higher than those in the control group, and the difference was statistically significant. Additionally, the study group had a higher rate of liquid diet one day before the examination, higher rate of correct bowel-clearing agent dilution method, higher rate of accurate time of ingesting the bowel-clearing agent, and a higher proportion of patients ingesting bowel-clearing agent at the specified time than the control group, with statistically significant differences. The incidence of nausea and vomiting during bowel clearance in the study group was significantly lower than that in the control group. The incidence of abdominal pain, abdominal distension, dizziness, and fatigue was compared between the two groups, but the difference was not statistically significant. The scores of service attitude, detailed notification of dietary precautions, clear and easy-to-understand health educational content, and receiving care and comfort in the study group were significantly higher than those in the control group.
Preoperative special guidance and education were shown to significantly improve bowel clearance and compliance and reduce the incidence of adverse reactions in older adult patients with constipation undergoing colonoscopy. These factors are beneficial for improving patient satisfaction with nursing services.
Core Tip: Oral education on bowel preparation before colonoscopy in digestive endoscopy room, so some patients cannot understand the requirements of bowel preparation, especially in elderly patients with hearing impairment and lower education level patients, cannot be very good bowel preparation.
- Citation: Wang H, Wang Y, Yuan JH, Wang XY, Ren WX. Pre-colonoscopy special guidance and education on intestinal cleaning and examination in older adult patients with constipation. World J Gastrointest Surg 2022; 14(8): 778-787
- URL: https://www.wjgnet.com/1948-9366/full/v14/i8/778.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i8.778
Colonoscopy is the most important screening test for colon and anal diseases because it provides a realistic picture of diseased sections, which allows early diagnosis of diseases[1]. Intestinal preparation before a colonoscopy examination is usually performed using an enema or an oral intestinal cleaning agent, which is crucial in ensuring that the desired examination effects are achieved for older adult patients with constipation[2]. The ideal method of intestinal preparation allows the patient to empty the intestine in a short time, and the colonic mucosa does not change. The patient feels comfortable, water and electrolytes levels are stable, and the procedure has few or no complications[3,4]. At present, most of the informational literature and educational methods for intestinal preparation before colonoscopy are delivered orally, and nurses must provide education on medication and other topics within a limited time[5]. Some patients are unable to understand the instructions of intestinal preparation, especially older adult patients with hearing impairment and patients with low education levels. Hence, these patients cannot adequately perform intestinal preparation. Therefore, to improve the quality of bowel preparation in older adult patients, we must explore personalized and targeted methods for delivering guidance to these patients. This study discusses the value of special preoperative guidance and educational methods for older adult patients with constipation undergoing colonoscopy.
This study was conducted on 160 older adult patients with constipation, who were scheduled for colonoscopy at Shandong Provincial Hospital between January 2019 and March 2021. Patients were selected and randomly divided into a study group and a control group, with 80 patients in each group. The age range of the subjects was 60–85 years, and all had the typical manifestations of chronic constipation and met the diagnostic criteria for constipation (Rome III). Patients had healthy understanding and communication skills. Those suspected of having intestinal organic lesions or polyps were required to undergo intestinal endoscopy. There was detailed communication with the patients and their families before the implementation of this study, and patients did not use laxatives for one week prior to the study. Exclusion criteria were: (1) any examination contraindications; (2) gastrointestinal perforation; (3) electrolyte disorders, dehydration, severe infection, or galactose intolerance; and (4) lactation, pregnancy, or occurrence of a menstrual period.
The control group received oral health education in which patients were asked to refrain from high-fiber food intake 2 d before the examination and were advised to consume semi-liquid or liquid foods with less residual fiber. Liquid diet was prescribed 1 d before the examination, and the use of compound polyethanol electrolyte powder (Heshuang, Shenzhen Wanhe Pharmaceutical Co., Ltd.) and medication administration were both explained to the patients. The following were confirmed the day before examination: dinner had been consumed (with water allowed) and medication was administered 1 h after dinner (oral dosage, with 2 L administered at a rate of approximately 1 L per hour). On the day of the examination, medication was checked, breakfast was not allowed (with water allowed), and medication was administered about 6 h before the scheduled examination. Medication was terminated once the discharge liquid became transparent; however, if the defecation form was not up to the standard, the doctor advised to continue administration, with the total dose not exceeding 4 L.
The study group received special guidance and education beyond what was given to the control group. To fully understand the patient's situation, nursing staff conducted a multi-dimensional assessment of the patient's condition, including age, personality, living habits, rest, bowel routine, and other basic conditions. Information tables were prepared, including detailed records of the patients' basic conditions, colonoscopy duration times, main condition, convenient time for telephone follow-up, and other contact details required for nurses to individualize education and care. If the patients had any doubts, they can consult by telephone. The language and behavior of the patients was observed, and their psychological status was evaluated to fully understand their condition. During the special guidance sessions, patients were informed about the basic principles and importance of bowel preparation and the role of prescriptions to encourage compliance. This was done to increase patients’ cooperation and establish good nurse–patient relationships. Nursing staff printed out the basic points for bowel preparation, used a written form, and guided patients to watch a video regarding bowel preparation medication and precautions to increase the impact of the information. Defecation standards were also placed in the toilet to facilitate comparisons for patients. Medication was kept consistent within the control group, and patients and their families were guided to massage the abdomen, engage in moderate exercise to increase gastrointestinal peristalsis, and check for intestinal cleanliness. Patients were also able to communicate with doctors through the WeChat platform, and telephone, so that doctors could respond to any sudden issues quickly, and nurses were able to strengthen ward inspection work.
All patients underwent electronic colonoscopy. Patients were placed on the left lateral position and instructed to bend their knees. The colonoscope was then slowly inserted into the patients’ anus to explore the rectum, sigmoid colon, transverse colon, ascending colon, and terminal ileum. Pathological manifestations in the intestinal mucosa and intestine were recorded.
The colonoscopy duration time, bowel preparation compliance, Boston bowel preparation assessment scale (BBPS) score, intestinal bubble score, the incidence of adverse reactions during bowel preparation, and nursing appointment satisfaction were compared between the two groups.
The BBPS score[7] divided the patient’s colon into the right, left, and middle colon. The score of each colon ranged from 0 to 3 points, where 3 points indicated that the bowel was prepared very well, the vision was clear, and the internal intestinal structure was observed; 2 points: the bowel was ready, the vision was clear, and did not affect the observation of the internal structure of the bowel; 1 point: the intestinal tract was well prepared; however, the visual field clarity was poor, which affected the observation of internal intestinal wall under endoscopy; and 0 point: poor bowel preparation, fecal water, and feces in the intestinal wall, which seriously affected visualization.
The total score of bubbles in intestinal endoscopy was also 0–3 points, with 3 points indicating: bubbles in the intestinal cavity and a large number of bubbles in the intestinal tract; 2 points: a moderate number of bubbles in the intestinal tract; 1 point: a small number of bubbles were detected; and 0 points: no bubbles were detected.
The factor of nursing appointment satisfaction took into account the treatment environment, service attitude, medication guidance, detailed information on bowel preparation and dietary precautions, health education content being clear and easy to understand, care and comfort provided, and attention to privacy protection. Each aspect was divided into very satisfied (3 points), satisfied (2 points), general (1 point), or dissatisfied (0 points).
The evaluation of intestinal preparation compliance mainly included the type of diet (solid, liquid, or semi-liquid diet) consumed on the day before the colonoscopy, whether fasting was observed on the day of the examination (yes/no), whether the correct dilution method of the intestinal cleaning agent was followed (yes/no), whether the time taken for the intestinal cleaning agent was accurate (yes/no), and whether the intestinal cleaning agent was consumed within the specified time (yes/no).
In this study, colonoscopy time, intestinal bubble score, and other measurement indexes of the patients were tested by normal distribution, which was in line with either the approximate normal distribution or normal distribution and expressed as mean ± SD. A t-test was used for comparisons between the two groups. The non-counting data were represented as percentages, and the comparison was performed using the χ2 test; SPSS 21.0, software was used for data processing with a test level α = 0.05.
Statistical analysis comparison was conducted between the study group and the control group using the factors of age, BMI, duration of constipation, sex, and comorbidities (P > 0.05, Table 1).
| Normal information | Research group (n = 80) | Control group (n = 80) | t/χ2 | P value |
| Age (yr) | 68.2 ± 5.4 | 68.4 ± 5.4 | -0.218 | 0.827 |
| BMI (kg/m2) | 24.5 ± 2.7 | 24.1 ± 2.7 | 1.009 | 0.158 |
| Duration of constipation (yr) | 6.3 ± 1.6 | 6.4 ± 2.3 | 040 | 0.158 |
| Sex | 0.905 | 0.341 | ||
| Male | 46 (57.50) | 40 (50.00) | ||
| Female | 34 (42.50) | 40 (50.00) | ||
| Hypertension | 0.227 | 0.634 | ||
| Yes | 38 (47.5) | 35 (43.75) | ||
| No | 42 (52.5) | 45 (56.25) | ||
| Diabetes | 0.038 | 0.845 | ||
| Yes | 17 (21.25) | 16 (20.00) | ||
| No | 63 (78.75) | 64 (80.00) | ||
| Smoking | 0.000 | 1.000 | ||
| Yes | 14 (17.50) | 14 (17.50) | ||
| No | 66 (82.50) | 66 (82.50) | ||
| Drinking | 0.316 | 0.574 | ||
| Yes | 20 (25.00) | 17 (21.25) | ||
| No | 60 (75.00) | 63 (78.75) |
The colonoscopy time of the study group was shorter than that of the control group, and the intestinal bubble score of the study group was lower than that of the control group; these differences were statistically significant (P < 0.05, Table 2).
| Groups | Colonoscopy time (min) | Intestinal bubble score (points) |
| Research group (n = 80) | 15.21 ± 1.81 | 0.59 ± 0.22 |
| Control group (n = 80) | 16.28 ± 2.04 | 1.00 ± 0.26 |
| t value | -3.509 | -10.767 |
| P value | 0.001 | 0.000 |
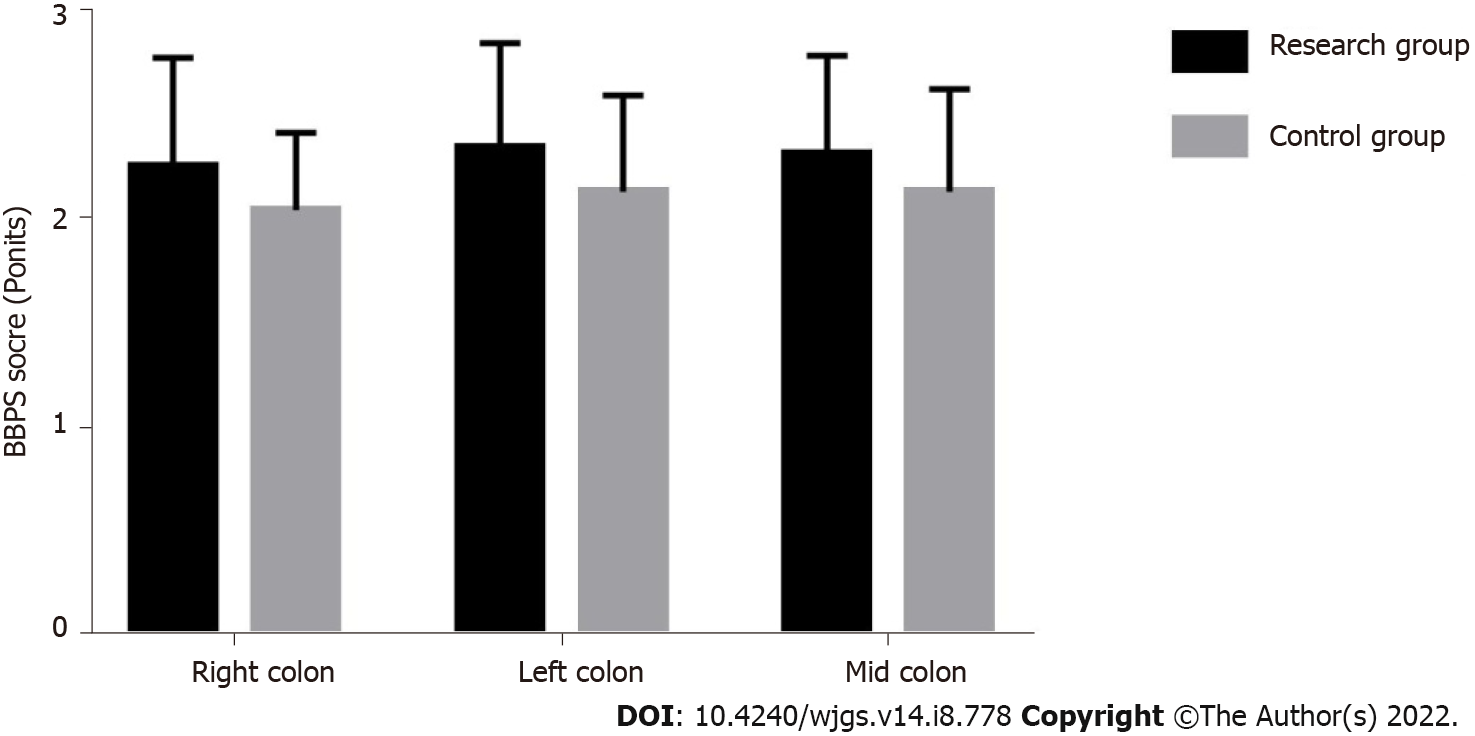
The BBPS scores of the right colon, left colon, and transverse colon in the study group were higher than those in the control group, and the difference was statistically significant (P < 0.05, Table 3, Figure 1).
| Groups | Right colon | Left colon | Mid colon |
| Research group (n = 80) | 2.25 ± 0.52 | 2.34 ± 0.50 | 2.31 ± 0.47 |
| Control group (n = 80) | 2.04 ± 0.37 | 2.13 ± 0.46 | 2.13 ± 0.49 |
| t value | 2.943 | 2.765 | 2.371 |
| P value | 0.004 | 0.006 | 0.019 |
The study group had a higher fluid diet rate 1 d before examination, the correct bowel-clearing agent dilution method, an accurate time of ingesting the bowel-clearing agent, and a higher proportion of patients ingesting the bowel-clearing agent within the specified time compared to the control group, and the difference was statistically significant (P < 0.05, Table 4).
| Compliance index | Research group (n = 80) | Control group (n = 80) | χ2 | P value |
| Check the diet of the day before | 5.010 | 0.025 | ||
| Liquid or semi-liquid | 77 (96.25) | 69 (86.25) | ||
| Solid | 3 (3.75) | 11 (13.75) | ||
| Check if fasting on the day | 1.858 | 0.173 | ||
| Yes | 79 (98.75) | 76 (95.00) | ||
| No | 1 (1.25) | 4 (5.00) | ||
| The correct method of diluting bowel cleansers | 4.113 | 0.043 | ||
| Yes | 73 (91.25) | 64 (80.00) | ||
| No | 7 (8.75) | 16 (20.00) | ||
| Is the time of taking the bowel cleansing correct | 4.440 | 0.035 | ||
| Yes | 74 (92.50) | 65 (81.25) | ||
| No | 6 (7.50) | 15 (18.75) | ||
| Drink the bowel cleanser within the specified time | 4.113 | 0.043 | ||
| Yes | 73 (91.25) | 64 (80.00) | ||
| No | 7 (8.75) | 16 (20.00) |
The incidence of nausea and vomiting in the study group was lower than that in the control group, and the difference was statistically significant (P < 0.05). The incidence of abdominal pain, bloating, dizziness, and fatigue was compared between the two groups, and the difference was not statistically significant (P > 0.05, Table 5).
| Adverse reactions | Research group (n = 80) | Control group (n = 80) | χ2 | P value |
| Nausea | 5.301 | 0.022 | ||
| Yes | 22 (27.50) | 36 (45.00) | ||
| No | 58 (72.50) | 44 (55.00) | ||
| Vomiting | 6.144 | 0.013 | ||
| Yes | 6 (7.50) | 17 (21.25) | ||
| No | 74 (92.50) | 63 (78.75) | ||
| Stomach ache | 1.002 | 0.317 | ||
| Yes | 7 (8.75) | 11 (13.75) | ||
| No | 73 (91.25) | 69 (86.25) | ||
| Bloating | 1.406 | 0.236 | ||
| Yes | 13 (16.25) | 19 (23.75) | ||
| No | 67 (83.75) | 61 (76.25) | ||
| Dizziness | 1.441 | 0.230 | ||
| Yes | 4 (5.00) | 8 (10.00) | ||
| No | 76 (95.00) | 72 (90.00) | ||
| Fatigue | 1.707 | 0.191 | ||
| Yes | 7 (8.75) | 3 (3.75) | ||
| No | 73 (91.25) | 77 (96.25) |
The scores measuring service attitude, detailed diet instructions, clear and understandable health education content, and care and comfort in the study group were higher than those in the control group, and the difference was statistically significant (P < 0.05, Table 6).
| Nursing satisfaction | Research group (n = 80) | Control group (n = 80) | t value | P value |
| Appointment and consultation environment | 2.09 ± 0.46 | 1.98 ± 0.42 | 1.580 | 0.116 |
| Service attitude | 2.20 ± 0.40 | 2.08 ± 0.35 | 2.019 | 0.045 |
| Medication guidance | 2.15 ± 0.39 | 2.09 ± 0.43 | 0.924 | 0.357 |
| Inform in detail about dietary precautions | 2.14 ± 0.33 | 1.91 ± 0.41 | 3.909 | 0.000 |
| Health education content is clear and easy to understand | 2.04 ± 0.37 | 1.84 ± 0.48 | 2.952 | 0.004 |
| Give care and comfort | 2.14 ± 0.47 | 1.91 ± 0.36 | 3.475 | 0.001 |
| Pay attention to privacy protection | 1.98 ± 0.55 | 1.95 ± 0.35 | 0.412 | 0.681 |
Before a colonoscopy, a patient's diet and drug intake can influence the effectiveness of intestinal preparation, thereby affecting the effectiveness of the examination and increasing the possibility of complications such as intestinal perforation and intestinal bleeding[8]. Early studies have shown[9,10] that the provision of health education before a colonoscopy is closely related to the degree of intestinal cleanliness, which can indirectly affect the diagnosis and treatment of the procedure. Thus, helping patients master the pertinent health knowledge prior to the procedure improves the effectiveness of colonoscopy[11]. In the past, patient preparation by the nurses before colonoscopy was often too procedural and not targeted, frequently ignoring the occurrence of complications, resulting in insufficient bowel preparation and incomplete bowel clearance that directly decreased the effectiveness of colonoscopy. When nursing staff guide patients to prepare their intestinal tracts, special instruction methods must be adopted and individualized. Standardized and targeted guidance should be provided regarding medication, diet, and prevention of complications, with suggestions that patients take medicine as directed on time.
The results of this study showed that the colonoscopy duration time in the study group was shorter, and the intestinal bubble scores were lower compared to those in the control group. The BBPS scores of the right, left, and transverse colon of patients in the study group were higher than those in the control group (P < 0.05). This shows that the intestinal preparation of the study group is better, which is consistent with previous research results[12,13]. Special guidance can enhance adherence to correct behavior in older adult patients, deepen patients' memory of bowel preparation, improve compliance with bowel preparation guidance content, and improve the quality of bowel preparation. This indicated that the special guidance education method was effective, patients more easily accepted the information, health knowledge was mastered faster and better, and the nurse–patient relationship was greatly improved. Nurses could increase patients' trust at a professional level to encourage patients to listen to their medical advice.
Fear of autonomic nervous system disturbances induced by colonoscopy in elderly patients can also lead to symptoms such as nausea and vomiting[14,15]. The incidence of nausea and vomiting during bowel clearance in the study group was significantly lower than that in the control group. Our results show that special guidance prior to ingesting intestinal cleaning agents can increase the incidence of correct intestinal preparation in older adult patients and reduce adverse reactions caused by emotional and timing factors. The results of this study are consistent with those of existing studies[16,17]. Analysis of the reasons mainly before the inspection and effective methods are necessary to alleviate the stressful emotions of patients so that they realize these emotions could trigger physical problems, listen to the guidance of medical staff, and improve the quality of their bowel preparation. The nurses in this study took care in explaining matters needing special attention during intestinal preparation, such as the pace of ingestion of intestinal cleaning agents (not too fast or too slow), and ingesting them within 2 h, thereby relieving tension and helping to reduce the incidence of adverse reactions in older adult patients.
The scores of service attitude, detailed notification of dietary precautions, clear and easy-to-understand health education content, and providing care and comfort in the study group were significantly higher than those in the control group. The method used to educate the control group was cursory and cannot take into account the individual differences of elderly patients, while the method used in the research group overcomes these drawbacks and meets the requirements of nursing, with high rationality and accurate targeting of patients. Knowledge gaps and biases may compromise the quality of bowel preparation. The special guidance adopted by the research group can provide a one-to-one personalized education reminder service. Patients should feel that they have received attention and that nursing staff would answer their questions patiently. It is easier to accept health education plans that are individualized to the patient, which significantly improves patient’s understanding of their condition or disease and helps to improve the relationship between nurses and patients. Special guidance health education is based on the basic concept of modern high-quality nursing and patient-centeredness. In the implementation process, nursing staff must master the knowledge of colonoscopy, bowel preparation methods, influencing factors, related drug contraindications, adaptive population, usage and dosage of medication, and be able to adjust the bowel preparation plan flexibly according to each situation. When this is done, compliance and satisfaction of patients are significantly improved, reflecting the strong effectiveness of health education.
In this study, we used existing nursing studies[18-20] to guide our investigation of whether personalized preoperative special guidance for colonoscopy has a better effect on bowel preparation, patient acceptance, and safety in older adult patients with constipation, and whether the practice is worthy of clinical application. However, the sample size of this study was small, and the inclusion criteria were not representative. In future follow-up studies, it will be necessary to further expand the sample range to make the research results more representative and further explore the education methods used to improve the quality of bowel preparation for colonoscopy subjects.
In summary, preoperative special guidance and education significantly improve bowel clearance compliance and bowel clearance effect and reduce the incidence of adverse reactions in older adult patients with constipation undergoing colonoscopy. This is also conducive to improving the satisfaction of patients interacting with nursing staff.
The prevalence of constipation in the Chinese population over 60 years of age is 11.5%. Intestinal preparation before a colonoscopy examination is usually performed using an enema or an oral intestinal cleaning agent, which is crucial in ensuring that the desired examination effects are achieved for older adult patients with constipation.
Oral education was provided on bowel preparation before colonoscopy in the digestive endoscopy room.
This study aimed to improve the quality of bowel preparation in older adult patients, we must explore personalized and targeted methods for delivering guidance to these patients.
Nurses could increase patients’ trust at a professional level to encourage patients to listen to their medical advice.
Preoperative special guidance and education significantly improve bowel clearance compliance and bowel clearance effect and reduce the incidence of adverse reactions in older adult patients with constipation undergoing colonoscopy.
This study discusses the value of special preoperative guidance and educational methods for older adult patients with constipation undergoing colonoscopy.
This is conducive to improving the satisfaction of patients interacting with nursing staff.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Christiansen EH, Denmark; Yumiba T, Japan S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Liu C, Song X, Hao H. Educational Video Followed by Retelling Bowel Preparation Process to Improve Colonoscopy Bowel Preparation Quality: A Prospective Nursing Intervention Study. Med Sci Monit. 2018;24:6029-6037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Ho LH, Montealegre JR, Al-Arabi S, Jibaja-Weiss ML, Suarez MG. Impact of Colonoscopy Preparation Video on Boston Bowel Preparation Scale Score. Gastroenterol Nurs. 2019;42:251-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Liang Y, Xin W, Yang Y, Li X. Application of care bundles in bowel preparation for colonoscopy in children. Ann Palliat Med. 2019;8:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Argyropoulos SK, Mahmood SK, Campbell EJ, Richter JM. Improving the Quality of Inpatient Bowel Preparation for Colonoscopies. Dig Dis Sci. 2018;63:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Parra-Blanco A, Ruiz A, Alvarez-Lobos M, Amorós A, Gana JC, Ibáñez P, Ono A, Fujii T. Achieving the best bowel preparation for colonoscopy. World J Gastroenterol. 2014;20:17709-17726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 53] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (10)] |
| 6. | . Retraction: Valproic acid protects neurons and promotes neuronal regeneration after brachial plexus avulsion. Neural Regen Res. 2022;17:250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009;69:620-625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 930] [Cited by in RCA: 925] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 8. | Kızılcık Özkan Z, Ünver S, Yıldız Fındık Ü, Albayrak D, Fidan Ş. Effect of Short Message Service Use on Bowel Preparation Quality in Patients Undergoing Colonoscopy. Gastroenterol Nurs. 2020;43:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Fatima H, Johnson CS, Rex DK. Patients' description of rectal effluent and quality of bowel preparation at colonoscopy. Gastrointest Endosc. 2010;71:1244-1252.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Ho SB, Hovsepians R, Gupta S. Optimal Bowel Cleansing for Colonoscopy in the Elderly Patient. Drugs Aging. 2017;34:163-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Chen J, Teng J, Ma L, Tong H, Ren B, Wang L, Li W. Flavonoids Isolated From the Flowers of Limonium bicolor and their In vitro Antitumor Evaluation. Pharmacogn Mag. 2017;13:222-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | McNabb-Baltar J, Dorreen A, Al Dhahab H, Fein M, Xiong X, O' Byrne M, Ait I, Martel M, Barkun AN. Age Is the Only Predictor of Poor Bowel Preparation in the Hospitalized Patient. Can J Gastroenterol Hepatol. 2016;2016:2139264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Yang MD, Chen XL, Hu XQ, Xie XZ, Zhou WJ, Zhou CG, Jiang B, Ji Q, Li Q, Wang P, Meng ZQ, Wang WH, Hu YJ, Su SB. Traditional Chinese medicine syndromes distribution in colorectal cancer and its association with western medicine treatment and clinical laboratory indicators. World J Tradit Chin Med. 2019;5:81-87. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Zhang YY, Niu M, Wu ZY, Wang XY, Zhao YY, Gu J. The incidence of and risk factors for inadequate bowel preparation in elderly patients: A prospective observational study. Saudi J Gastroenterol. 2018;24:87-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Garg R, Singh A, Ahuja KR, Mohan BP, Ravi SJK, Shen B, Kirby DF, Regueiro M. Risks, time trends, and mortality of colonoscopy-induced perforation in hospitalized patients. J Gastroenterol Hepatol. 2020;35:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Harrison NM, Hjelkrem MC. Bowel cleansing before colonoscopy: Balancing efficacy, safety, cost and patient tolerance. World J Gastrointest Endosc. 2016;8:4-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 17. | Jaiswal AK, Chaudhary S. Effectiveness in Bowel Cleansing and Patient Tolerability of Polyethylene Glycol versus Sodium Picosulphate in Patients Undergoing Colonoscopy. Adv Med. 2020;2020:1234341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Liu Z, Zhang MM, Li YY, Li LX, Li YQ. Enhanced education for bowel preparation before colonoscopy: A state-of-the-art review. J Dig Dis. 2017;18:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Grassini M, Verna C, Battaglia E, Niola P, Navino M, Bassotti G. Education improves colonoscopy appropriateness. Gastrointest Endosc. 2008;67:88-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Evans B, Pace D, Borgaonkar M, Harnett J, Miné-Goldring M, Ge MM, Brodie J, Boone D, McGrath J. Effect of an educational intervention on colonoscopy quality outcomes. Surg Endosc. 2020;34:5142-5147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |