Published online Jul 27, 2022. doi: 10.4240/wjgs.v14.i7.685
Peer-review started: March 25, 2022
First decision: May 29, 2022
Revised: June 5, 2022
Accepted: July 5, 2022
Article in press: July 5, 2022
Published online: July 27, 2022
Processing time: 124 Days and 4.7 Hours
At present, there is no perfect system to evaluate pulmonary complications of liver surgery using perioperative variables.
To design and verify a risk assessment system for predicting postoperative pulmonary complications (PPCs) after hepatectomy based on perioperative variables.
A retrospective analysis was performed on 1633 patients who underwent liver surgery. The variables were screened using univariate and multivariate analyses, and graded scores were assigned to the selected variables. Logistic regression was used to develop the liver operation pulmonary complication scoring system (LOPCSS) for the prediction of PPCs. The LOPCSS was verified using the receiver operating characteristic curve.
According to the multivariate correlation analysis, the independent factors which influenced PPCs of liver surgery were age [≥ 65 years old/< 65 years old, odds ratio (OR) = 1.926, P = 0.011], medical diseases requiring drug treatment (yes/no, OR = 3.523, P < 0.001), number of liver segments to be removed (≥ 3/≤ 2, OR = 1.683, P = 0.002), operation duration (≥ 180 min/< 180 min, OR = 1.896, P = 0.004), and blood transfusion (yes/no, OR = 1.836, P = 0.003). The area under the curve (AUC) of the LOPCSS was 0.742. The cut-off value of the expected score for complications was 5. The incidence of complications in the group with ≤ 4 points was significantly lower than that in the group with ≥ 6 points (2.95% vs 33.40%, P < 0.001). Furthermore, in the validation dataset, the corresponding AUC of LOPCSS was 0.767.
As a novel and simplified assessment system, the LOPCSS can effectively predict PPCs of liver surgery through perioperative variables.
Core Tip: In this study, a binomial logistic regression model was established to obtain the liver operation pulmonary complication scoring system (LOPCSS). The area under the curve of the LOPCSS was 0.742. As a novel and simplified assessment system, the LOPCSS can effectively predict postoperative pulmonary complications of liver surgery through perioperative factors; therefore, it can be used to evaluate the risk of liver surgical pulmonary complications.
- Citation: Xu LN, Xu YY, Li GP, Yang B. Individualized risk estimation for postoperative pulmonary complications after hepatectomy based on perioperative variables. World J Gastrointest Surg 2022; 14(7): 685-695
- URL: https://www.wjgnet.com/1948-9366/full/v14/i7/685.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i7.685
Compared to other surgical areas, liver surgery is still a relatively complex discipline that requires continuous theoretical exploration and accumulated experience[1,2]. However, liver surgery technology has developed rapidly as a result of the development of information science and encouragement of liver allograft transplantation[3]. The key reason hepatectomy is not applied globally is the high incidence of postoperative complications and high operative mortality[4]. Appropriate preoperative prevention strategies should, therefore, be considered to reduce the risk of postoperative complications. Predicting, evaluating, and intervening in surgical risk and preventing complications of liver surgery have become major clinical problems[5-7]. Postoperative pulmonary complications (PPCs) are important adverse events associated with surgery and anesthesia. The main PPCs include pulmonary insufflation, pneumonia, respiratory failure, and deterioration of potential pulmonary diseases. The treatment cost related to pulmonary complications is high and the average hospital stay is long. PPCs are a major cause of delayed recovery and worse outcomes after hepatectomy[8], their incidence is much higher than that of other important organ complications, and the associated complications can be life-threatening. Current clinical guidelines strongly recommend evaluation of the risk of PPCs. The prediction of PPCs enables individual application of preventive measures and perhaps even early treatment if a PPC eventually starts to develop[9]. Appropriate perioperative prevention strategies should be considered to reduce the risk of PPCs where possible. Since the 1970s, many risk assessment systems have been established and applied; however, these risk assessment systems still have many problems in guiding clinical practice. Currently, there is no perfect prediction and evaluation system for pulmonary complications in liver surgery. Although many factors have been implicated as predictors, few models have been developed using the rigorous methodology required for clinically useful tools[10]. Therefore, establishing a set of risk prediction and evaluation systems for perioperative pulmonary complications with strong clinical operability and improving the safety of liver surgery has become an urgent problem in the clinic.
In this study, perioperative risk factors for PPCs of liver surgery were screened and assessed according to the odds ratio (OR), and the total value of the perioperative risk factors for each patient was calculated. The results of the regression analysis will be used to create a scoring system for PPCs incidence and an associated cut-off value to make perioperative evaluation more intuitive.
Personal medical information files were established for patients undergoing perioperative liver surgery. The inclusion criteria were as follows: (1) Perioperative patients; (2) Complete medical records; and (3) Nonrecent secondary surgery. A total of 1633 cases were collected between January 1990 and December 2020 at the PLA General Hospital. Data were obtained from the medical records department of PLA General Hospital. Among these patients, 682 (41.76%) were diagnosed with benign hepatobiliary disease, including hepatolithiasis, and 951 (58.24%) were diagnosed with malignant hepatobiliary disease, mainly primary hepatocellular carcinoma and intrahepatic cholangiocarcinoma. The mean patient age was 47.80 ± 12.09 years old (range 2–83), with 1017 (62.28%) men and 616 (37.72%) women. After the evaluation formula was obtained, 100 consecutive patients were enrolled in the validation for verification.
Based on other commonly used surgical risk scoring systems and the project team's previous clinical research experience, the perioperative factors analyzed included the patient's basic information, diagnosis, laboratory examination, type of surgery, associated medical diseases, medication history, tumor position, and intraoperative variables (such as operative time, blood loss, blood transfusion). Postoperative conditions included complications and death.
The grouping variables were PPCs and the test variables were perioperative variables. The variables were set according to the grade for ordered classification variables, such as age and bilirubin level. The main risk factors and their relative risk values were determined using Pearson’s correlation analysis. All factors that were significantly correlated with postoperative adverse outcomes were included in the multivariate logistic regression analysis. A scoring system was introduced based on the OR values for these factors, which were rounded off to be clinically usable (the risk index was assigned according to the nearest integer for clinical application). The sum of the risk scores of all risk factors for a single patient was considered to be the patient’s total risk score for complications. The risk index for all patients with complications was calculated to establish the evaluation system for the risk of pulmonary complications: The liver operation pulmonary complication scoring system (LOPCSS). The cut-off value was used to determine the critical point of complications.
Receiver operating characteristic (ROC) curves were used to evaluate the resolution of the LOPCSS. The area under the curve (AUC) and cut-off values were calculated.
Statistical software (SPSS 25.0) was used for the data analysis. The measurement data are expressed as mean ± SD. Pearson’s correlation analysis was used to analyze the relationship between the complications and preoperative factors. Regression analysis was used to conduct a multivariate analysis of the factors affecting surgical complications, and P < 0.05 was considered statistically significant.
A total of 250 pulmonary complications were observed in 205 patients, of whom 26 patients had multiple complications, with an incidence of 12.55% (Table 1).
| Complication-pulmonary | n | Ratio (n/total number of patients), % |
| Pleural cavity infection | 1 | 0.06 |
| Respiratory tract infection | 3 | 0.18 |
| Pneumothorax | 3 | 0.18 |
| Respiratory insufficiency | 7 | 0.43 |
| Atelectasis | 22 | 1.35 |
| Pneumonia | 30 | 1.84 |
| Pleural effussion | 184 | 11.27 |
According to the univariate correlation analysis, the preoperative clinical risk factors for different levels of postoperative liver complications were age (P < 0.001), medical diseases requiring drug treatment (P < 0.001), Child-Pugh grade (P < 0.001), number of total liver segments to be removed (P < 0.001), blood transfusion (P < 0.001), blood loss (P < 0.001), operation duration (P < 0.001), adjacent organ invasion (P = 0.007), and preoperative hospital stay (P < 0.001) (Table 2).
| Variable | n | Pearson coefficient | P value1 |
| Age (years old) | 0.087 | 0.000 | |
| ≥ 65 | 147 | ||
| < 65 | 1486 | ||
| Medical diseases requiring drug treatment | 0.200 | < 0.001 | |
| Yes | 248 | ||
| No | 1385 | ||
| Child-pugh grade | 0.093 | < 0.001 | |
| A | 1463 | ||
| B, C | 170 | ||
| Number of segments resected | 0.124 | < 0.001 | |
| ≤ 2 segments resected | 1046 | ||
| ≥ 3 segments resected | 587 | ||
| Blood transfusion | 0.182 | 0.000 | |
| Yes | 689 | ||
| No | 944 | ||
| Blood loss (mL) | 0.103 | < 0.001 | |
| ≥ 800 | 204 | ||
| < 800 | 1429 | ||
| Operation duration (min) | 0.169 | 0.000 | |
| ≥ 180 | 922 | ||
| < 180 | 711 | ||
| Adjacent organ invasion | 0.066 | 0.007 | |
| Yes | 18 | ||
| No | 1615 | ||
| Preoperative hospital stay (days) | 0.098 | 0.000 | |
| ≤ 7 | 1142 | ||
| > 7 | 491 |
According to multivariate correlation analysis, the independent factors influencing postoperative complications of liver surgery were age, medical diseases requiring drug treatment, number of liver segments to be removed, operation duration, and blood transfusion, as shown in Table 3. A scoring system was introduced based on the OR values for these factors, which were rounded to improve the ease of applying the scale clinically, as shown in Table 4.
| Variable | Odds ratio | P value1 |
| χ1: Age (≥ 65 years old/< 65 years old) | 1.926 | 0.011 |
| χ2: Medical diseases requiring drug treatment (Yes/No) | 3.523 | < 0.001 |
| χ3: Number of segments resected (≥ 3/≤ 2) | 1.683 | 0.002 |
| χ4: Operation duration (≥ 180 min/< 180 min) | 1.896 | 0.004 |
| χ5: Blood transfusion (Yes/No) | 1.836 | 0.003 |
| Variable | Conditions | Scores |
| χ1: Age | < 65 years old | 0 |
| ≥ 65 years old | 2 | |
| χ2: Medical diseases requiring drug treatment | No | 0 |
| Yes | 4 | |
| χ3: Number of segments resected | ≤ 2 | 0 |
| ≥ 3 | 2 | |
| χ4: Operation duration | < 180 min | 0 |
| ≥ 180 min | 2 | |
| χ5: Blood transfusion | No | 0 |
| Yes | 2 |
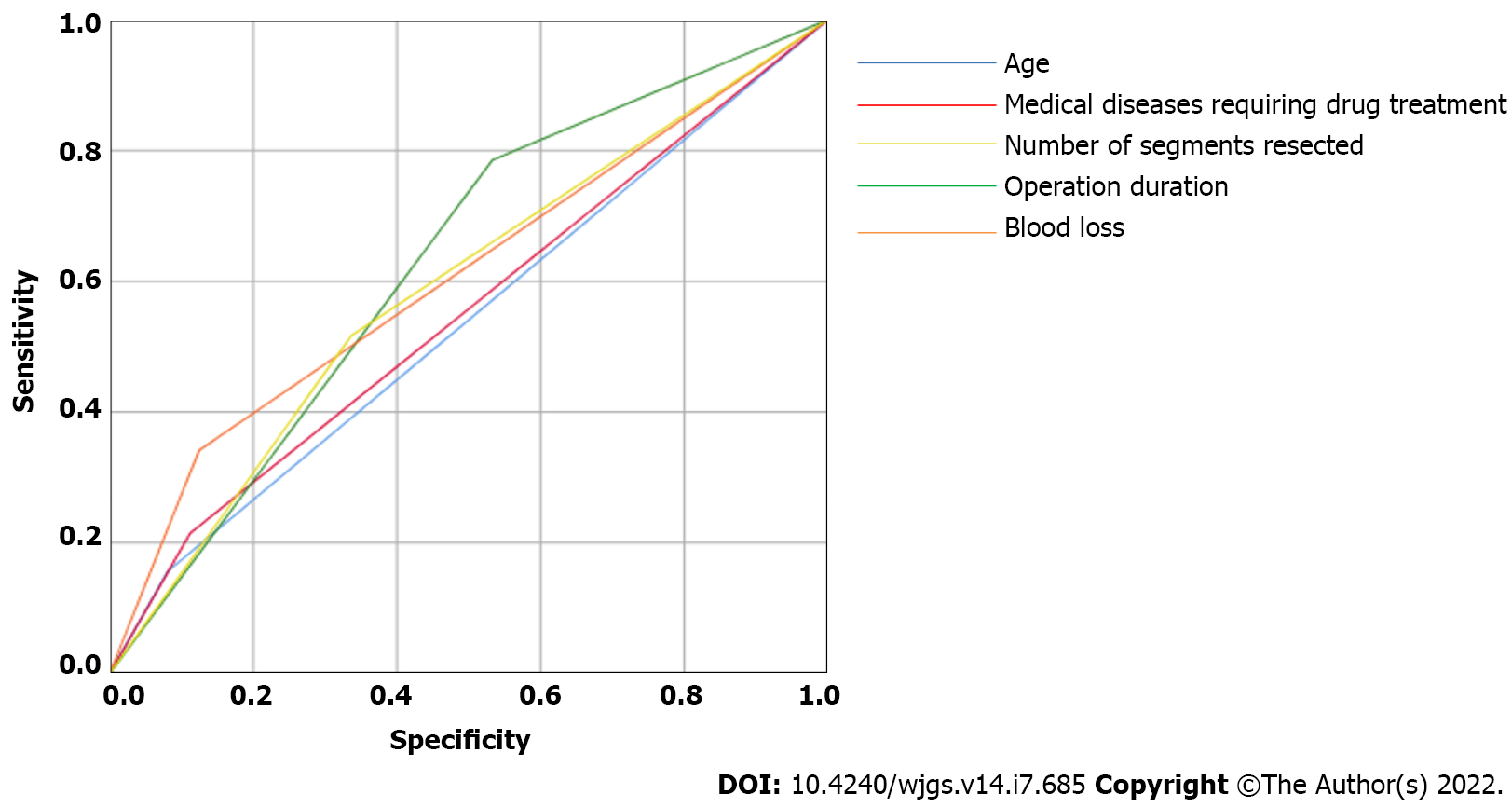
The ROC curves for each identified independent risk factors are plotted in Figure 1.
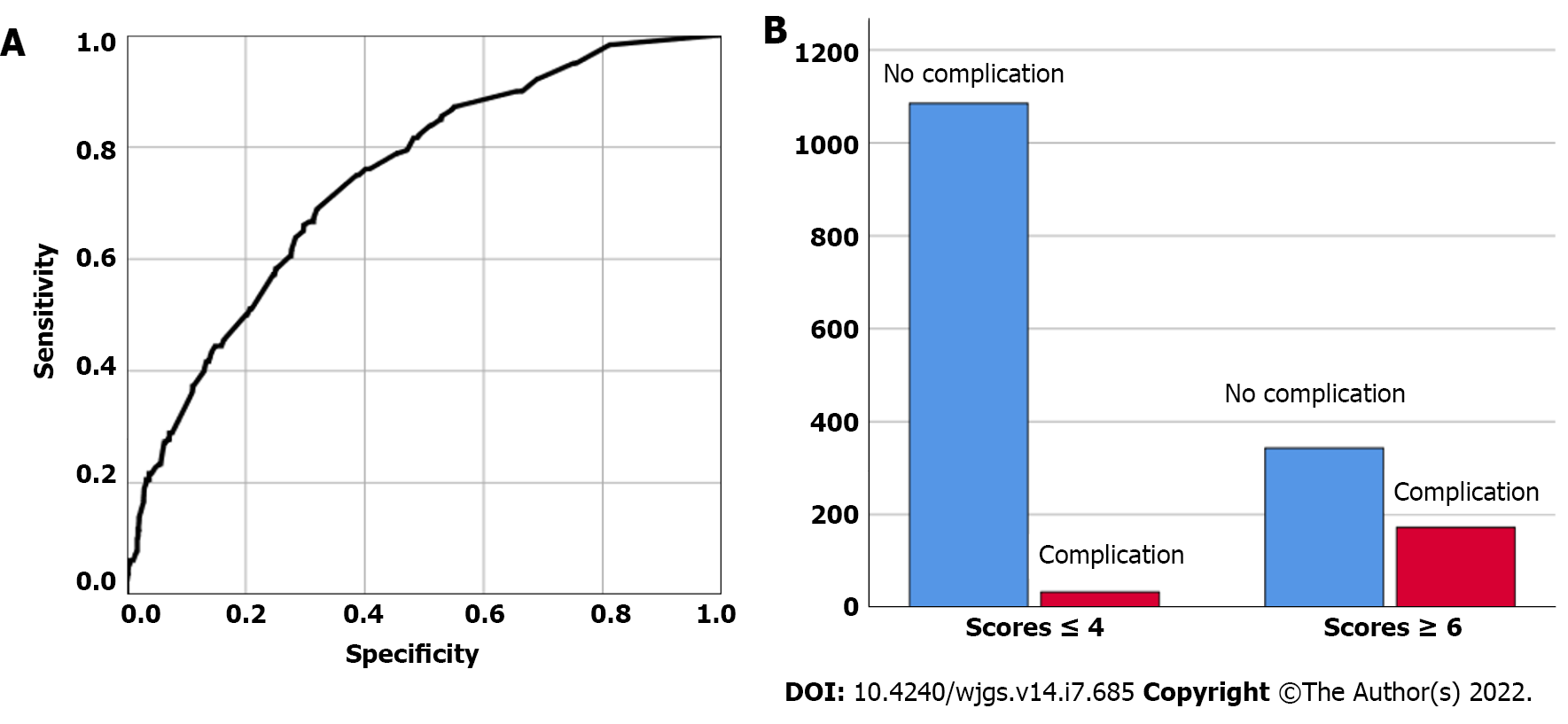
The ROC curves of the five combined variables are shown in Figure 2A. The AUC of the five combined variables was 0.742, and the corresponding standard error was 0.019. The cut-off value of the total score, calculated by adding the values of all risk factors, was 5. With this threshold, the incidence of pulmonary complications was 2.95% (33/1118) for patients with a score ≤ 4 and 33.40% (172/515) for patients with a score ≥ 6. The incidence of PPCs between patients with ≤ 4 points and ≥ 6 points was significantly different (χ2 = 297.731, P < 0.001), as shown in Figure 2B.
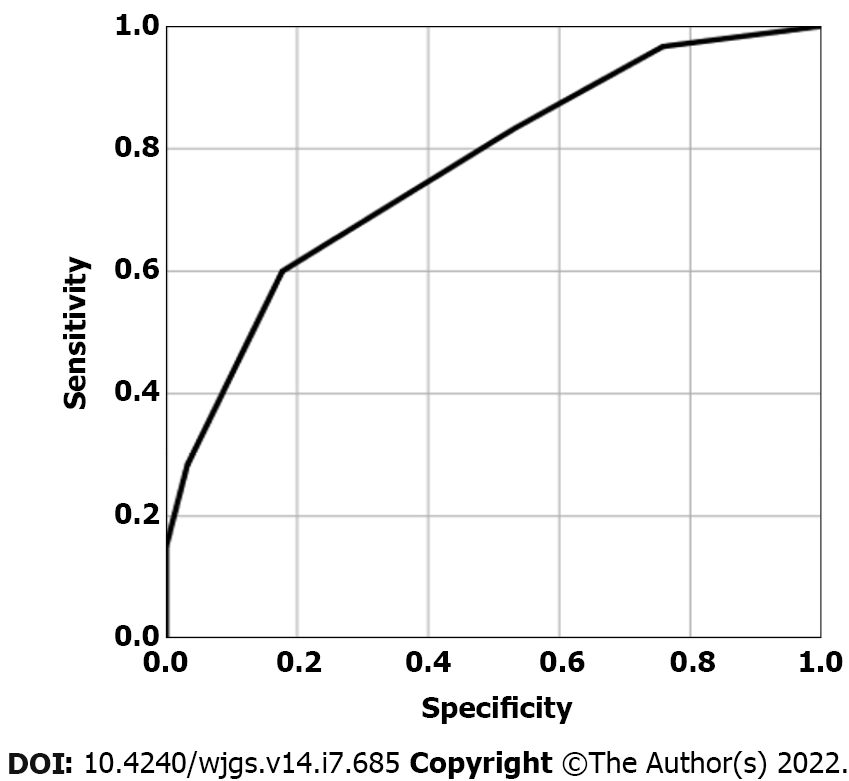
One hundred consecutive patients were enrolled in the validation group to verify LOPCSS. We analyzed the discrimination ability using ROC curves. The AUC of LOPCSS is 0.767, as shown in Figure 3.
Hepatectomy has always been characterized by complexity and a high incidence of complications and mortality. However, in recent years, the safety of hepatectomy has been significantly improved by optimizing the selection of surgical patients, anesthesia, and perioperative management, and especially with the establishment of hepatobiliary surgery as a specialty. For the past fifty years, the safety of hepatectomy has always been at the forefront of liver surgery[11]. With the rapid development of liver surgery, hepatectomy has changed from a risky procedure to a relatively safe one[12]. However, there is still a high incidence of complications and mortality with liver surgery, and appropriate preoperative prevention strategies must be considered to reduce the risk of postoperative complications[13]. However, a complete system for predicting complications of liver surgery based on perioperative factors remains unavailable[14]. Therefore, establishing a set of clinically applicable preoperative risk prediction and evaluation systems for surgical liver complications has become an urgent clinical problem[15,16].
Among the complications of liver surgery, the incidence of pulmonary complications is high[17]. This has a great impact on postoperative rehabilitation, so avoiding pulmonary complications should be considered as a priority by doctors. PPCs not only affect the recovery course and quality of life of patients, but also significantly increase the overall perioperative complication rate and mortality. Previous studies have reported that the incidence of PPCs was 2%–70%[18,19]. PPCs mainly include atelectasis, bronchitis, pneumonia, respiratory failure (postoperative mechanical ventilation time exceeding 48 h or unplanned reintubation), hypoxemia, COPD, or asthma attack. Various risk factors can increase the incidence of PPCs[20]. At present, the clear risk factors mainly include the operation site (such as the upper abdomen), emergency surgery, age > 65 years, duration of operation > 3 h, and poor overall health. Strengthening perioperative airway management, protecting pulmonary function, and reducing pulmonary complications are important to ensure the success of the operation and improve prognosis. In this study, a simplified prediction and evaluation system for PPCs of liver surgery which integrated multiple risk factors was established and verified, and is expected to provide new means for early intervention and treatment.
There are three major difficulties in performing surgery for elderly patients: (1) The decline in organ function and poor tolerance to the operation; (2) Elderly patients often have a variety of accompanying diseases; and (3) Elderly patients recover slowly after surgery. In this study, age was an independent risk factor for PPCs after liver surgery (≥ 65 years/< 65 years, OR = 1.926, P = 0.011). Elderly individuals are prone to pulmonary complications, such as pleural effusion and infection after surgery, and some elderly individuals also experience problems such as respiratory failure. This leads to high requirements for intraoperative and perioperative management. Therefore, perioperative management strategies should be improved.
Many patients who require surgery often have one or more other medical conditions or comorbidities[21], and this is more common in elderly patients[22]. The physiological function of elderly people decreases with age, and is evidenced by: Decreases in height and body surface area; muscle atrophy; decreases in the total number of metabolically active cells; and decreased function of the heart, blood vessels, respiration, kidney, and other organs. These changes in physiological function lowers the reserve ability to maintain the stability of the internal environment under stress. The stress of surgery increases the burden on the organ systems and oxygen consumption of the body, and myocardial oxygen consumption[23]. With the continuous breakthrough of the traditional surgical exclusion zone, a large number of high-risk surgery patients with liver, kidney, and lung insufficiency have been operated upon, and the number of surgical patients with diabetes, hypertension, heart disease, and other diseases has also increased rapidly. In these high-risk patients, perioperative comorbidities exist alone or in combination with several diseases, and are closely associated with postoperative complications and mortality. In this study, concomitant medical conditions requiring medication were independent risk factors for postoperative complications after liver surgery (yes/no, OR = 3.523, P < 0.001).
In recent years, due to the increasing maturity of liver surgery technology, the success rate of resection of giant liver tumors has increased[24], and postoperative complications and mortality have decreased greatly, such that large liver tumors that were considered inoperable in the past can now be safely resected. The main reasons for this are as follows: (1) The development of stereo positioning technology for liver tumors; (2) The development of liver bleeding, hemostasis, and blood transfusion technology; (3) More accurate liver and vascular surgery techniques; (4) Excellent anesthesia management; and (5) Advances in perioperative management. However, the amount of liver resected, and therefore the residual functional liver volume, remains the main factor affecting the curative effect of hepatectomy[25]. This study showed that the number of liver segments removed was an independent risk factor for complications after liver surgery (≥ 3/≤ 2, OR = 1.683, P = 0.002).
However, there are some limitations to measuring the scope of resection based on the number of liver segments. The volume of the left lobe of the liver is smaller than that of the right lobe. Consequently, resection of the two segments of the left lobe is not equivalent to resection of segments 6-7 or 7-8. There are also differences in the surgical difficulty and scope of resection. In this study, considering the complexity of liver anatomy and the possible infiltration of liver tumors into adjacent organs, three indicators (lesion size, number of liver segments removed, and presence of adjacent organ infiltration) were used to evaluate the scope of liver resection. Even with all of these considerations taken into account, the results of this study showed that the removal of > 2 liver segments was an independent risk factor for pulmonary complications.
The surgical duration has long attracted the attention of doctors as an important factor affecting rehabilitation after general anesthesia. The surgical duration mainly reflects the complexity of the operation. With the development of modern surgical medicine, operation durations are shorter than ever before; however, under existing conditions, the operation duration is still one of the main factors hindering rehabilitation after general anesthesia. The extension of the operation duration has a great impact on postoperative respiration, digestion, physiological response, and the recovery of autonomic function, and affects the quality of postoperative rehabilitation. Additionally, the operation duration can affect the occurrence of PPCs[26]. A longer duration of surgery has a significant impact on postoperative respiratory function. Owing to the residual effect of general anesthesia drugs, the respiratory center will be inhibited to varying degrees, resulting in a weakening of ventilation function, a reduction in tidal volume, and a change in respiratory rate. In addition, the residual effects of muscle relaxants can cause incomplete respiratory tract obstruction and insufficient ventilation. Simultaneously, long-term airway intubation can cause pulmonary infection, and the incidence of PPCs increases. Therefore, it is necessary to actively improve respiratory function. We should make preoperative and emergency plans, optimize the operation process, and shorten the operation time as much as possible. This study showed that the operation duration was an independent risk factor for complications after liver surgery (≥ 180 min/< 180 min, OR = 1.896, P = 0.004).
Blood transfusion is directly related to massive blood loss during surgery, which reflects a wider scope of resection. Because the estimation of intraoperative and postoperative acute bleeding is often inaccurate, the amount of blood transfused is often used as an alternative index of blood loss. As an effective treatment to correct intraoperative blood loss, blood transfusion is widely used in almost all hospitals; however, some negative effects can arise during its use, such as the spread of infectious diseases. In addition, blood transfusion also leads to some related complications[27], such as blood transfusion-related acute lung injury, blood transfusion-related graft-versus-host disease, blood transfusion-related circulatory overload, hemolytic reaction, and immunosuppression. Patients receiving blood transfusions tend to be older, have more complications, worse basic conditions, and more serious diseases. The adverse consequences of blood transfusion are related to factors such as blood transfusion-related immunosuppression, acute lung injury, changes in the coagulation cascade. Transfusion may cause infection and transfusion-related lung injury, which have an important impact on patient prognosis. Perioperative blood transfusions should be highly valued. Blood transfusions often lead to a significant increase in early mortality of the recipient and affects the prognosis. Attention should be paid to the risk factors for blood transfusions. For patients with risk factors, we should intervene as soon as possible, pay attention to the prevention and treatment of bleeding and blood transfusion-related complications, and prepare for blood transfusion when necessary. In this study, blood transfusion was an independent risk factor for PPCs after liver surgery (yes/no, OR = 1.836, P = 0.003).
Perioperative scoring systems have been developed to assess the risk of PPCs. An important example is the pulmonary complication risk score (PCRS) developed by the National Surgical Quality Improvement Program[28]. However, the PCRS also has limitations. The PCRS is a real-time network calculator based on big data that can only be used after registration with the model software on the internet. Although the prediction model comes from a large multicenter study, it has not been fully validated in countries outside the United States. Moreover, the surgical risk is different in China and the United States, and should be adjusted according to the actual situation in China.
In this study, a binomial logistic regression model was established to obtain the LOPCSS. The AUC of LOPCSS was 0.742 and the cut-off value of the expected score for complications was 5. Furthermore, in the validation dataset, the corresponding AUC of LOPCSS was 0.767. The scoring system has only five parameters, and the values are all integers (0-4); therefore, the calculation is simple to perform. If the patient’s score is higher than the cut-off value, the lung function of the patient should be fully adjusted before surgery to achieve the optimum conditions; if the lung function is poor and surgery is necessary, the surgical method should be adjusted to shorten the operation time as much as possible and reduce trauma to the patient.
This study has some limitations. Due to the limited number of cases with pulmonary complications, only internal validation was used in this study. Before the beginning of this study, considering that open liver surgery had more pulmonary complications than laparoscopic liver surgery, it was of great practical significance to study open liver surgery. Therefore, only cases of open liver surgery were included in the present study. At present, with the rapid growth in the number of cases of laparoscopic liver surgeries performed, the significance of studying the risk factors for complications of laparoscopic liver surgery is more prominent, and we plan to study this in future.
As a novel and simplified assessment system, the LOPCSS can effectively predict the PPCs of liver surgery through perioperative factors and can be used to evaluate the risk of pulmonary complications associated with liver surgery.
Predicting, evaluating, and intervening in surgical risk and preventing pulmonary complications of liver surgery have become major clinical problems.
Postoperative pulmonary complications (PPCs) are important adverse events associated with surgery and anesthesia. At present, there is no perfect system to evaluate the risk of pulmonary complications following liver surgery using perioperative variables.
This study aimed to design and verify a risk assessment system for predicting PPCs after hepatectomy based on perioperative variables.
A retrospective analysis was performed on 1633 patients undergoing liver surgery. All factors that were significantly correlated with postoperative adverse outcomes were included in the multivariate logistic regression analysis. A scoring system [the liver operation pulmonary complication scoring system (LOPCSS)] was introduced based on the odds ratio (OR) values for these factors. The sum of the risk scores of all risk factors for a single patient was the total risk score of the patient’s complications. The cut-off value was used to determine the critical point of complications.
The independent factors influencing PPCs of liver surgery were age (≥ 65 years old/< 65 years old, OR = 1.926, P = 0.011), medical diseases requiring drug treatment (yes/no, OR = 3.523, P < 0.001), number of liver segments to be removed (≥ 3/≤ 2, OR = 1.683, P = 0.002), operation duration (≥ 180 min/< 180 min, OR = 1.896, P = 0.004), and blood transfusion (yes/no, OR = 1.836, P = 0.003). The cut-off value of the expected score for complications was 5.
As a novel and simplified assessment system, the LOPCSS can effectively predict PPCs of liver surgery using perioperative variables.
We screened for perioperative risk factors associated with pulmonary complications in liver surgery and established a scoring system to predict the occurrence of complications.
We thank Mrs. Ai-Qun Zhang for her assistance with the data collection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cassese G, Italy; Karamarkovic AR, Serbia; Uhlmann D, Germany S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Agarwal V, Divatia JV. Enhanced recovery after surgery in liver resection: current concepts and controversies. Korean J Anesthesiol. 2019;72:119-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 62] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 2. | Glantzounis GK, Karampa A, Peristeri DV, Pappas-Gogos G, Tepelenis K, Tzimas P, Cyrochristos DJ. Recent advances in the surgical management of hepatocellular carcinoma. Ann Gastroenterol. 2021;34:453-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Marques HP, Barros I, Li J, Murad SD, di Benedetto F. Current update in domino liver transplantation. Int J Surg. 2020;82S:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Huang ZQ, Xu LN, Yang T, Zhang WZ, Huang XQ, Cai SW, Zhang AQ, Feng YQ, Zhou NX, Dong JH. Hepatic resection: an analysis of the impact of operative and perioperative factors on morbidity and mortality rates in 2008 consecutive hepatectomy cases. Chin Med J (Engl). 2009;122:2268-2277. [PubMed] |
| 5. | Nanashima A, Tobinaga S, Abo T, Nonaka T, Takeshita H, Hidaka S, Sawai T, Nagayasu T. Reducing the incidence of post-hepatectomy hepatic complications by preoperatively applying parameters predictive of liver function. J Hepatobiliary Pancreat Sci. 2010;17:871-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Chin KM, Allen JC, Teo JY, Kam JH, Tan EK, Koh Y, Goh KPB, Cheow PC, Raj P, Chow KHP, Chung YFA, Ooi LL, Chan CY, Lee SY. Predictors of post-hepatectomy liver failure in patients undergoing extensive liver resections for hepatocellular carcinoma. Ann Hepatobiliary Pancreat Surg. 2018;22:185-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Xu LN, Yang B, Li GP, Gao DW. Assessment of complications after liver surgery: Two novel grading systems applied to patients undergoing hepatectomy. J Huazhong Univ Sci Technolog Med Sci. 2017;37:352-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Soufi M, Flick KF, Ceppa DP, Blackwell MM, Mararu R, Nguyen TK, Schmidt CM, Nakeeb A, Zyromski N, House MG, Moszczynski Z, Ceppa EP. Investigating the incidence, impact, and severity of pulmonary complications after hepatectomy: A single institution experience. Surgery. 2022;171:643-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Nijbroek SG, Schultz MJ, Hemmes SNT. Prediction of postoperative pulmonary complications. Curr Opin Anaesthesiol. 2019;32:443-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Mazo V, Sabaté S, Canet J. How to optimize and use predictive models for postoperative pulmonary complications. Minerva Anestesiol. 2016;82:332-342. [PubMed] |
| 11. | Jackson NR, Hauch A, Hu T, Buell JF, Slakey DP, Kandil E. The safety and efficacy of approaches to liver resection: a meta-analysis. JSLS. 2015;19:e2014.00186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Yamazaki S, Takayama T. Current topics in liver surgery. Ann Gastroenterol Surg. 2019;3:146-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Xu LN, Xu YY, Gao DW. Impact of operative and peri-operative factors on the long-term prognosis of primary liver cancer patients undergoing hepatectomy. J Huazhong Univ Sci Technolog Med Sci. 2016;36:523-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Chen L, Wang YB, Zhang YH, Gong JF, Li Y. Effective prediction of postoperative complications for patients after open hepatectomy: a simplified scoring system based on perioperative parameters. BMC Surg. 2019;19:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Wang YK, Bi XY, Li ZY, Zhao H, Zhao JJ, Zhou JG, Huang Z, Zhang YF, Li MX, Chen X, Wu XL, Mao R, Hu XH, Hu HJ, Liu JM, Cai JQ. [A new prognostic score system of hepatocellular carcinoma following hepatectomy]. Zhonghua Zhong Liu Za Zhi. 2017;39:903-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Donadon M, Fontana A, Palmisano A, Viganò L, Procopio F, Cimino M, Del Fabbro D, Torzilli G. Individualized risk estimation for postoperative morbidity after hepatectomy: the Humanitas score. HPB (Oxford). 2017;19:910-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Jin S, Fu Q, Wuyun G, Wuyun T. Management of post-hepatectomy complications. World J Gastroenterol. 2013;19:7983-7991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 172] [Cited by in RCA: 164] [Article Influence: 13.7] [Reference Citation Analysis (3)] |
| 18. | Yang CK, Teng A, Lee DY, Rose K. Pulmonary complications after major abdominal surgery: National Surgical Quality Improvement Program analysis. J Surg Res. 2015;198:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 142] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 19. | Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Martinez Ruiz R, Lee JW, Henderson WG, Moss A, Mehdiratta N, Colwell MM, Bartels K, Kolodzie K, Giquel J, Vidal Melo MF. Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators. JAMA Surg. 2017;152:157-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 392] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 20. | Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118:317-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 435] [Article Influence: 54.4] [Reference Citation Analysis (0)] |
| 21. | Russell MC. Complications following hepatectomy. Surg Oncol Clin N Am. 2015;24:73-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Aucoin S, McIsaac DI. Emergency General Surgery in Older Adults: A Review. Anesthesiol Clin. 2019;37:493-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Gillis C, Carli F. Promoting Perioperative Metabolic and Nutritional Care. Anesthesiology. 2015;123:1455-1472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 197] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 24. | Liu X, Yang Z, Tan H, Liu L, Xu L, Sun Y, Si S, Huang J, Zhou W. Characteristics and operative treatment of extremely giant liver hemangioma >20 cm. Surgery. 2017;161:1514-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Khan AS, Garcia-Aroz S, Ansari MA, Atiq SM, Senter-Zapata M, Fowler K, Doyle MB, Chapman WC. Assessment and optimization of liver volume before major hepatic resection: Current guidelines and a narrative review. Int J Surg. 2018;52:74-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 26. | Sameed M, Choi H, Auron M, Mireles-Cabodevila E. Preoperative Pulmonary Risk Assessment. Respir Care. 2021;66:1150-1166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Kaufmann KB, Baar W, Glatz T, Hoeppner J, Buerkle H, Goebel U, Heinrich S. Epidural analgesia and avoidance of blood transfusion are associated with reduced mortality in patients with postoperative pulmonary complications following thoracotomic esophagectomy: a retrospective cohort study of 335 patients. BMC Anesthesiol. 2019;19:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 28. | Foster CA, Charles EJ, Turrentine FE, Sohn MW, Kron IL, Jones RS. Development and Validation of Procedure-Specific Risk Score for Predicting Postoperative Pulmonary Complication: A NSQIP Analysis. J Am Coll Surg. 2019;229:355-365.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |