Published online Jul 27, 2022. doi: 10.4240/wjgs.v14.i7.656
Peer-review started: August 17, 2021
First decision: September 12, 2021
Revised: September 21, 2021
Accepted: June 24, 2022
Article in press: June 24, 2022
Published online: July 27, 2022
Processing time: 344 Days and 5 Hours
In the past years, only a few studies with a limited number of adult patients analyzed clinical features of allied disorders of Hirschsprung’s disease (ADHD), most of which were individual case reports or lacked detailed clinical information. Although many studies have reported patients presenting to the emergency department (ED) with recurrent abdominal symptoms for a number of disorders, there are few data involving ADHD. However, owing to a lack of awareness of the disease, misdiagnoses and mistreatments are common. Severe complications such as perforation, bleeding, malabsorption, and even death in ADHD had been reported by many studies.
To assist ED clinicians in having a more comprehensive understanding of this disease and making an early suspected diagnosis of ADHD more effectively.
We enrolled 53 patients who visited the ED and were eventually diagnosed with ADHD over the past 11 years in our hospital. Their basic information, clinical manifestations, and imaging findings were analyzed. Blood indices were compared between the ADHD and irritable bowel syndrome (IBS) groups.
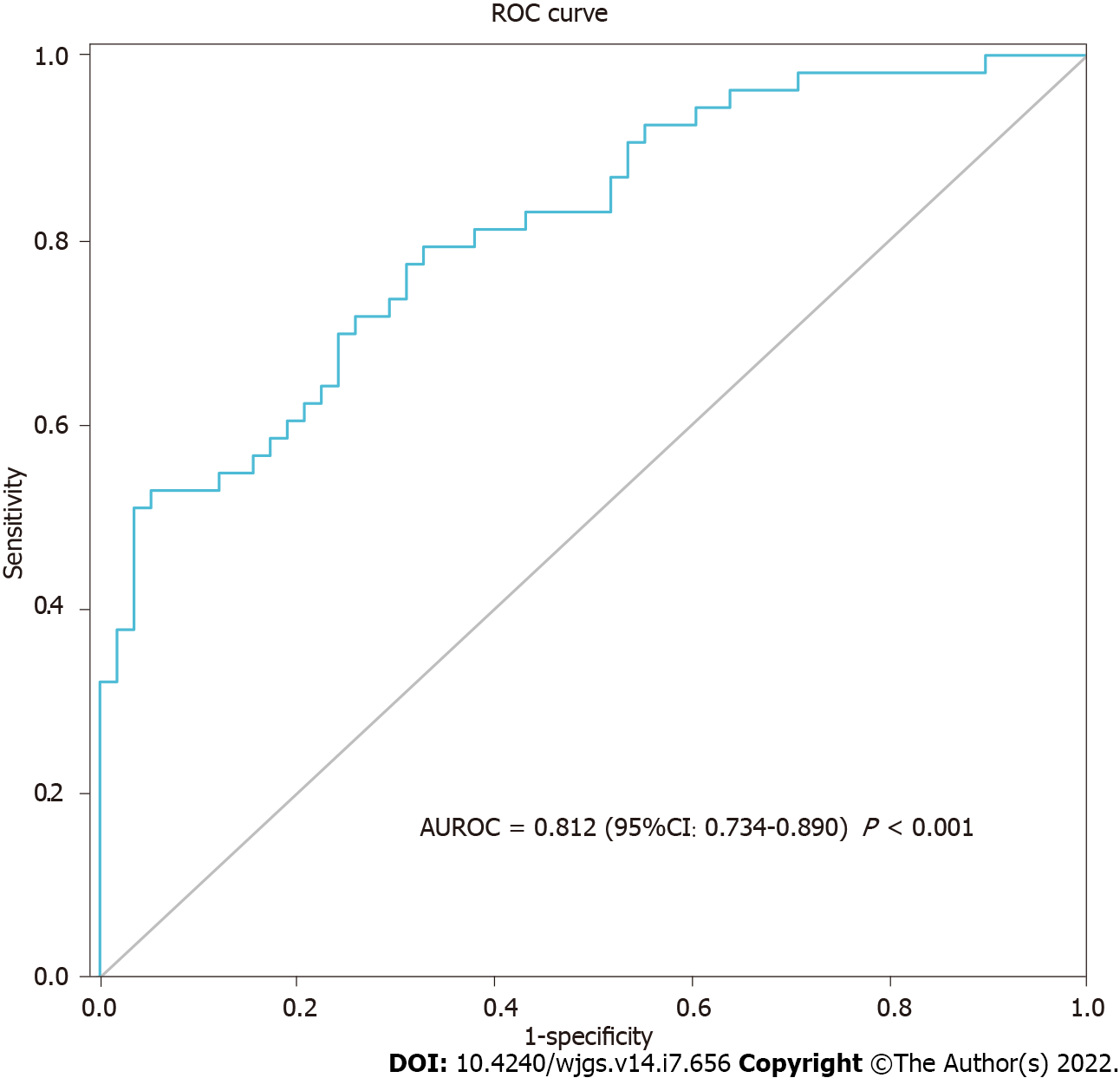
Adult patients with ADHD had a mean age of 48.8 ± 14.3 years, and 77.4% had been treated before admission. The transverse colon was the most common dilated part (73.6%), and constipation (67.9%) was the most common symptom. ADHD patients can present with uncommon symptoms and false-negative imaging findings. Logistic regression analysis indicated that body mass index (BMI) [odds ratio (OR) = 0.786, P = 0.013], cholinesterase (per 1000 units; OR = 0.693, P = 0.008), and blood chlorine (OR = 0.816, P = 0.022) were determined to be independent related factors between the ADHD and IBS groups. The area under the receiver operating characteristics curve of these three indices combined was 0.812 (P < 0.001).
Emergency physicians should be vigilant regarding patients with chronic constipation, abdominal pain, or abdominal distension, and consider the possibility of ADHD despite its rarity. Abdominal computed tomography examination is recommended as a useful tool in the suspected diagnosis of ADHD. BMI, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and IBS. The nutritional status of adult patients with ADHD is worthy of further attention. Surgical treatment for adult patients with ADHD is important and inevitable.
Core Tip: Emergency physicians should be vigilant regarding patients with chronic constipation, abdominal pain, or abdominal distension, especially those with recurrent and intolerable symptoms. Allied disorders of Hirschsprung’s disease (ADHD) should be considered in such cases despite its rarity. Abdominal computed tomography examination is recommended as a useful tool to make a suspected diagnosis of ADHD. Clinicians should also be wary of uncommon symptoms and false-negative imaging findings. Body mass index, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and irritable bowel syndrome. The nutritional status of adult patients with ADHD is worthy of further attention.
- Citation: Jiang S, Song CY, Feng MX, Lu YQ. Adult patients with allied disorders of Hirschsprung’s disease in emergency department: An 11-year retrospective study. World J Gastrointest Surg 2022; 14(7): 656-669
- URL: https://www.wjgnet.com/1948-9366/full/v14/i7/656.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i7.656
Patients with abdominal pain, abdominal distension, constipation, and intestinal obstruction in the emergency department (ED) are very common. However, during the follow-up of these patients over the years, we found that a small percentage were diagnosed with allied disorders of Hirschsprung’s disease (ADHD). We also noticed that they often visited the ED because of recurrent symptoms. It was reported that ADHD clinically resembled HD, despite the presence of ganglion cells in the rectum[1]. The first reported case was termed “pseudo Hirschsprung’s disease” by Ravitch[2] in 1958. In recent years, there have been many studies on the molecular mechanism, signaling pathway, and biomarkers associated with HD[3-5]. Researchers from Ireland reported that the diagnosis of ADHD is made after consideration of the presenting symptoms, radiographic findings, and histopathological examination[6]. Researchers from Japan have expounded on the specifics regarding the clinical symptoms, disease classification, and diagnostic criteria of ADHD[1,7,8]. According to their studies, ADHD can be classified into two categories: Diseases with intestinal ganglion cell abnormality (immature ganglia, isolated hypoganglionosis, and intestinal neuronal dysplasia) and diseases without intestinal ganglion cell abnormality (megacystis microcolon intestinal hypoperistalsis syndrome, segmental intestinal dilatation, internal anal sphincter achalasia, and chronic idiopathic intestinal pseudo-obstruction). All these studies have greatly increased our knowledge of ADHD. However, before a definite pathological diagnosis is made, making a suspected diagnosis of ADHD based on clinical manifestations alone is challenging because common intestinal disorders can present with these similarly[9]. Although many studies have reported patients presenting to the ED with recurrent abdominal symptoms for a number of disorders[10-13], there are few data involving ADHD. It is hard for most ED doctors to associate common abdominal symptoms with ADHD specifically. Consequently, potential diagnoses of ADHD are often missed or ignored in patients presenting with abdominal symptoms in the ED. Unfortunately, if the disease is not suspected, the subsequent treatment may be incorrect, and thus, further examination or targeted follow-up might not be implemented in such patients.
Owing to a lack of awareness of the disease, misdiagnoses and mistreatments are common. Severe complications such as perforation, bleeding, malabsorption, and even death in ADHD had been reported by many studies[14-18]. Moreover, we found that some patients repeatedly visited our ED or underwent one or more surgeries but still had recurrent symptoms. This prompted us to consider two important questions: What are the clinical characteristics of these patients? How can we make an early suspected diagnosis of ADHD more effectively?
However, the low prevalence of ADHD makes this difficult. A 10-years nationwide survey in Japan that included almost all ADHD cases from 2001 to 2010 showed that only 355 cases had a definite or suspicious diagnosis of ADHD[1]. Special attention should be given to addressing the difficulty of emergency clinicians in making a suspected diagnosis of ADHD. In past years, only a few studies with a limited number of adult patients analyzed its clinical features, most of which were individual case reports or lacked detailed clinical information. Herein, we performed a retrospective study to analyze the clinical manifestations, imaging findings, blood test indexes, treatment, and prognosis of adult ADHD patients. We hope to assist ED clinicians in having a more comprehensive understanding of this disease and making an early suspected diagnosis of ADHD more effectively.
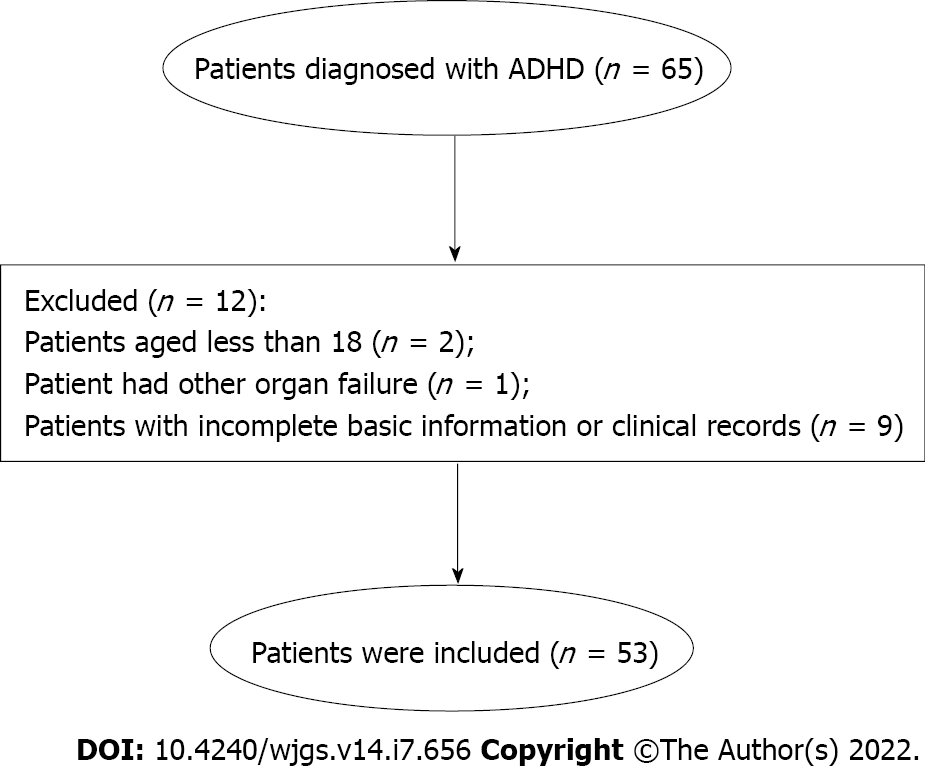
This single-center, retrospective observational study was carried out at the ED of the First Affiliated Hospital, School of Medicine, Zhejiang University. We enrolled patients from May 2009 to October 2020 who once visited the ED because of disease worsening and then, after receiving specialized treatment in our hospital, were finally diagnosed with ADHD. The diagnosis was consistent with existing guidelines and diagnostic criteria[1,7]. Figure 1 illustrates the specific screening procedure for ADHD patients. The patients were enrolled if they: (1) Were over 18 years old; and (2) Conformed to the diagnostic criteria for ADHD. The exclusion criteria included the following: (1) Patients who had missed important information; and (2) Patients who were suffering from heart, liver, brain, lung, kidney, or other vital organ failure. Finally, 53 patients with ADHD were included in this study, and among them, 39 had isolated hypoganglionosis and 14 had intestinal neuronal dysplasia on pathological analysis. Irritable bowel syndrome (IBS) is recognized as one of the most common functional gastrointestinal disorders presenting with abdominal pain and changes in bowel habits[19,20]. The diagnosis of IBS was in line with the Rome IV criteria[21]. To analyze blood indices in the adult ADHD patients, 58 patients diagnosed with IBS during the same period were included as a control group, who were all over 18 years and free of heart, liver, brain, lung, kidney, other vital organ failure and cachexia. This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (No. 2021271).
Data was collected from the electronic medical record system of the First Affiliated Hospital, School of Medicine, Zhejiang University. All 53 patients had confirmed pathology reports, and when they were finally diagnosed with ADHD at the specialty ward, the following data was recorded: Age, sex, hospital days, chief complaints, onset time, duration time, pre-hospitalization treatment, imaging findings, routine blood examination, biochemical test indexes, surgical procedures, and postoperative complications. The blood indices of both the ADHD and IBS groups were the first results on admission. The symptom duration was classified into the following: < 1 year, 1-5 years, 5-10 years, and > 10 years. We also identified the dilated sites of the bowel, if any (small intestine, transverse colon, ascending colon, descending colon, sigmoid colon, rectum, and no dilation) through radiological findings.
The data was analyzed using the SPSS statistical software package (version 23.0, SPSS Inc., IBM, Chicago, IL, United States). Continuous variables are described as the mean with standard deviation if they followed a normal distribution and median with interquartile range if they did not follow a normal distribution. Categorical variables are described as numbers (n) with percentage (%) in the group. The Kolmogorov-Smirnov normality test was used to determine if the quantitative variables had a normal distribution. The independent sample t-test or Mann-Whitney U test was used to evaluate continuous data, whereas the Chi-square test was used to analyze categorical variables. Variables with P < 0.05 in the univariate analysis were selected for the multivariate logistic regression to examine the independent related factors between ADHD and IBS. The stepwise procedure (forward: LR) was used to isolate the factors. Odds ratios (OR) and 95% confidence intervals (CI) were calculated, and a two-tailed P value < 0.05 was considered statistically significant. The area under the receiver operating characteristics curve (AUROC) was measured to evaluate the discriminative power of these blood test indices.
Among all 53 ADHD patients, the female-to-male ratio was 35:18 (35 females and 18 males) (Table 1). The mean age was 48.8 ± 14.3 years (range: 18-72 years), while the median length of hospital stay on first admission at our hospital was 14 d. Surgical history was classified into two categories: Abdominal (e.g., cesarean section, cholecystectomy, laparoscopic exploratory surgery, enterostomy, enterectomy, and inguinal hernia repair) and non-abdominal. Moreover, false negatives were found in 11 and 5 cases examined via enteroscopy and barium enema (BE), respectively. Lastly, all cases underwent either plain or contrast-enhanced abdominal computed tomography (CT) scans, and only one patient had a false-negative diagnosis.
| Basic characteristic | Data (n = 53) |
| Age (yr) | 48.8 ± 14.3 |
| Onset age (yr) | 42.8 ± 17.9 |
| Hospitalization days | 14.0 (10.0, 21.0) |
| Sex (n, %) | |
| Male | 18 (34.0) |
| Female | 35 (66.0) |
| Blood type (n, %) | |
| A | 10 (18.9) |
| B | 17 (32.1) |
| AB | 6 (11.3) |
| O | 19 (35.8) |
| Unknown | 1 (1.9) |
| All surgical history (n, %) | 25 (47.2) |
| Abdominal | 18 (34.2) |
| Non-abdominal | 7 (13.2) |
| Smoking (n, %) | |
| Yes | 5 (9.4) |
| No | 48 (90.6) |
| Drinking (n, %) | |
| Yes | 2 (3.8) |
| No | 51 (96.2) |
| Enteroscopy (n, %) | |
| Abnormality | 5 (9.4) |
| Non-abnormality | 11 (20.8) |
| Unexamined | 37 (69.8) |
| Barium enema (n, %) | |
| Intestinal dilation | 17 (32.1) |
| No abnormality | 5 (9.4) |
| Unexamined | 31 (58.5) |
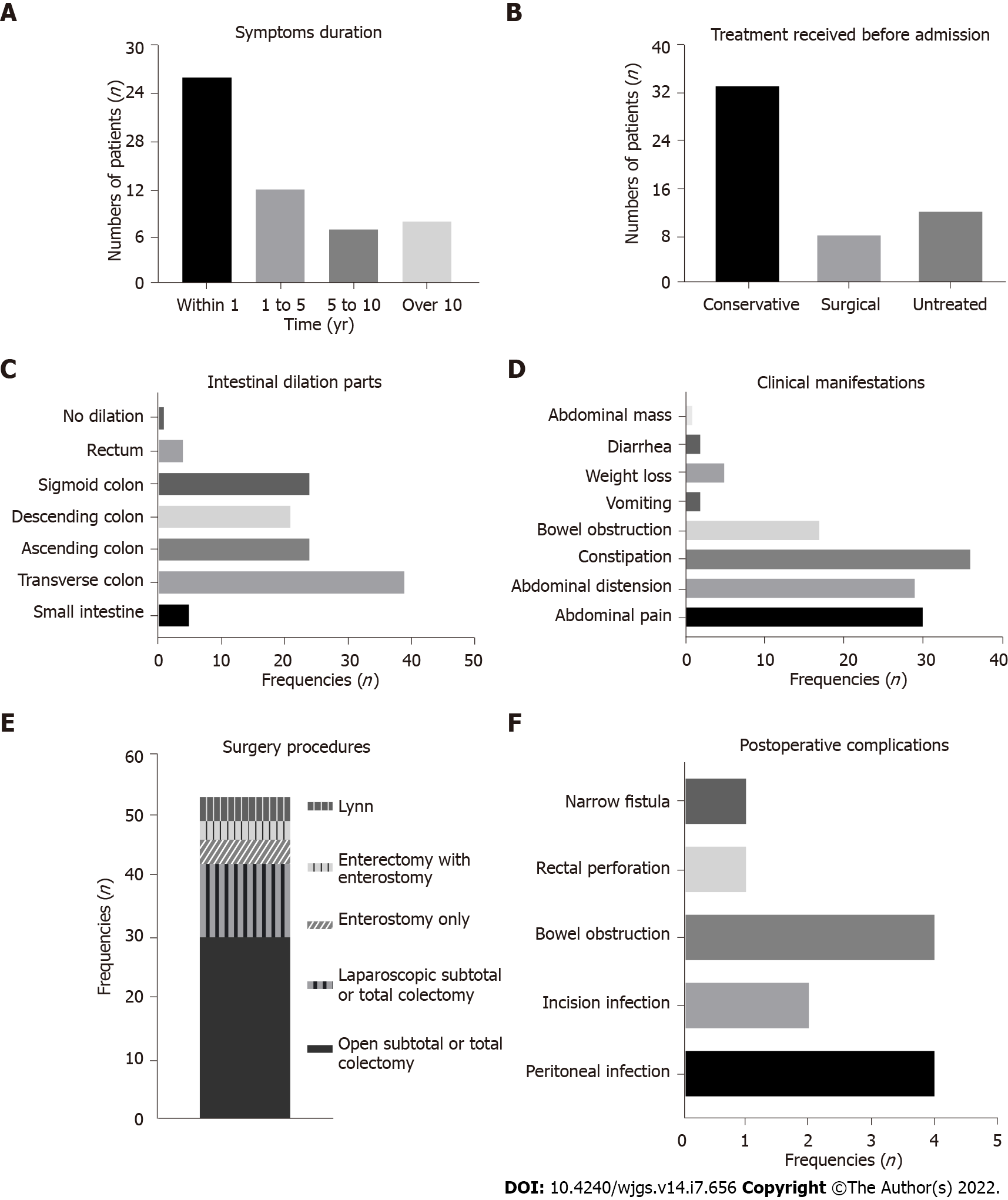
Among the 53 patients enrolled, 43 (81.1%) were either wrongly diagnosed or treated upon the first ED admission. On average, 17 mo passed from the first ED visit before arriving at the final diagnosis. The clinical information is presented in Figure 2. Notably, patients with < 1-year symptom duration were the most common. Furthermore, before a correct diagnosis was formulated, most patients were treated conservatively (i.e., medication, fasting, gastrointestinal decompression, or enema therapy). A total of 30 patients (56.6%) had a history of admission for abdominal symptoms; 22 cases were treated conservatively and 8 underwent enterectomy, including 3 cases who underwent bowel resection surgery twice in other hospitals. The transverse colon (73.6%) was the most involved dilated intestinal segment, while one case had no dilatations in the bowel. Abdominal pain, abdominal distension, constipation, and bowel obstruction were relatively common. Surprisingly, vomiting, weight loss, diarrhea, and abdominal mass were also found. Subtotal colectomy and total colectomy were the most common procedures, done in 42 cases (79.2%). Concomitant treatments mainly involved maintaining electrolyte balance, regulating intestinal flora, and symptomatic treatment. Postoperative complications were mainly bowel obstruction and infection.
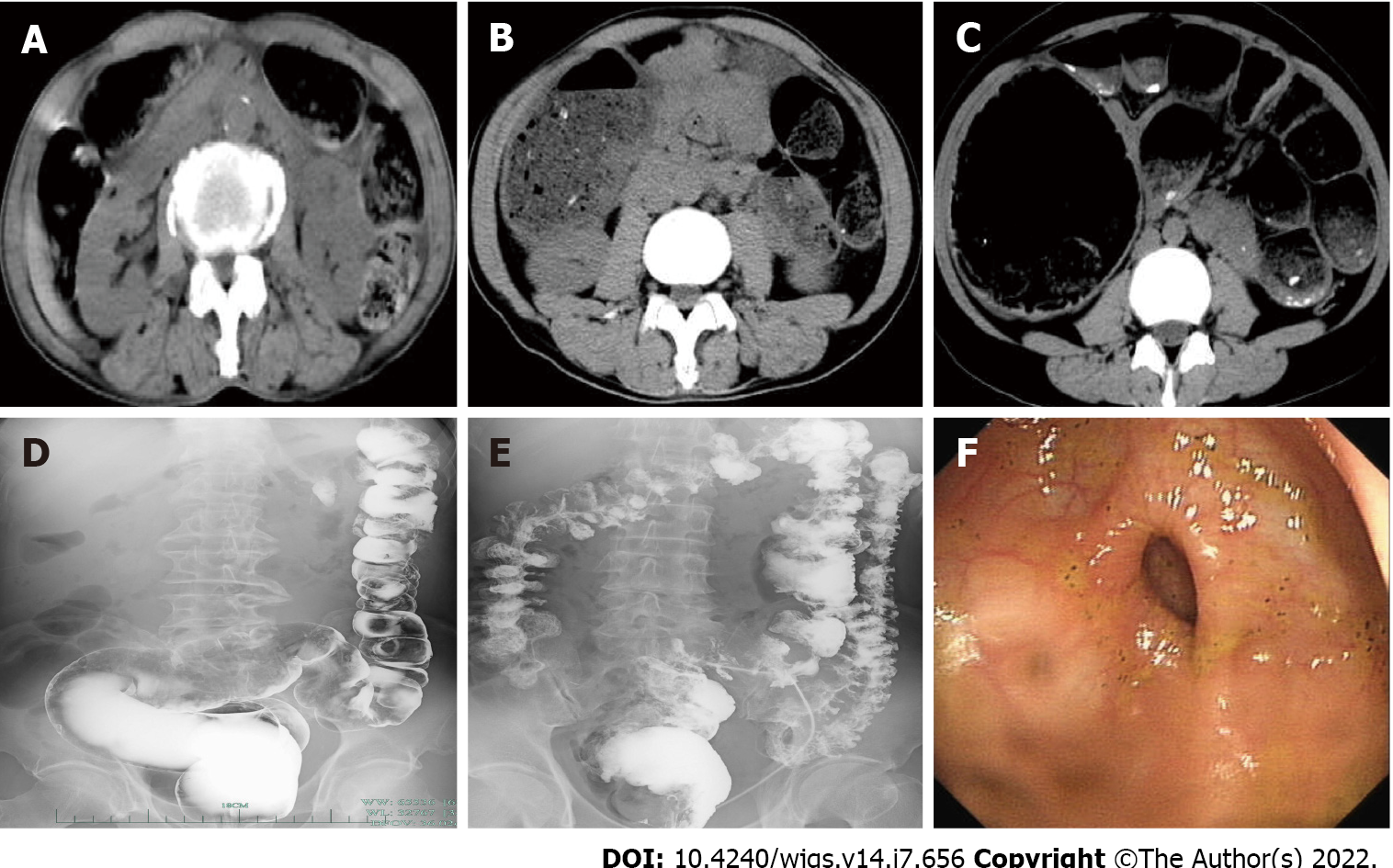
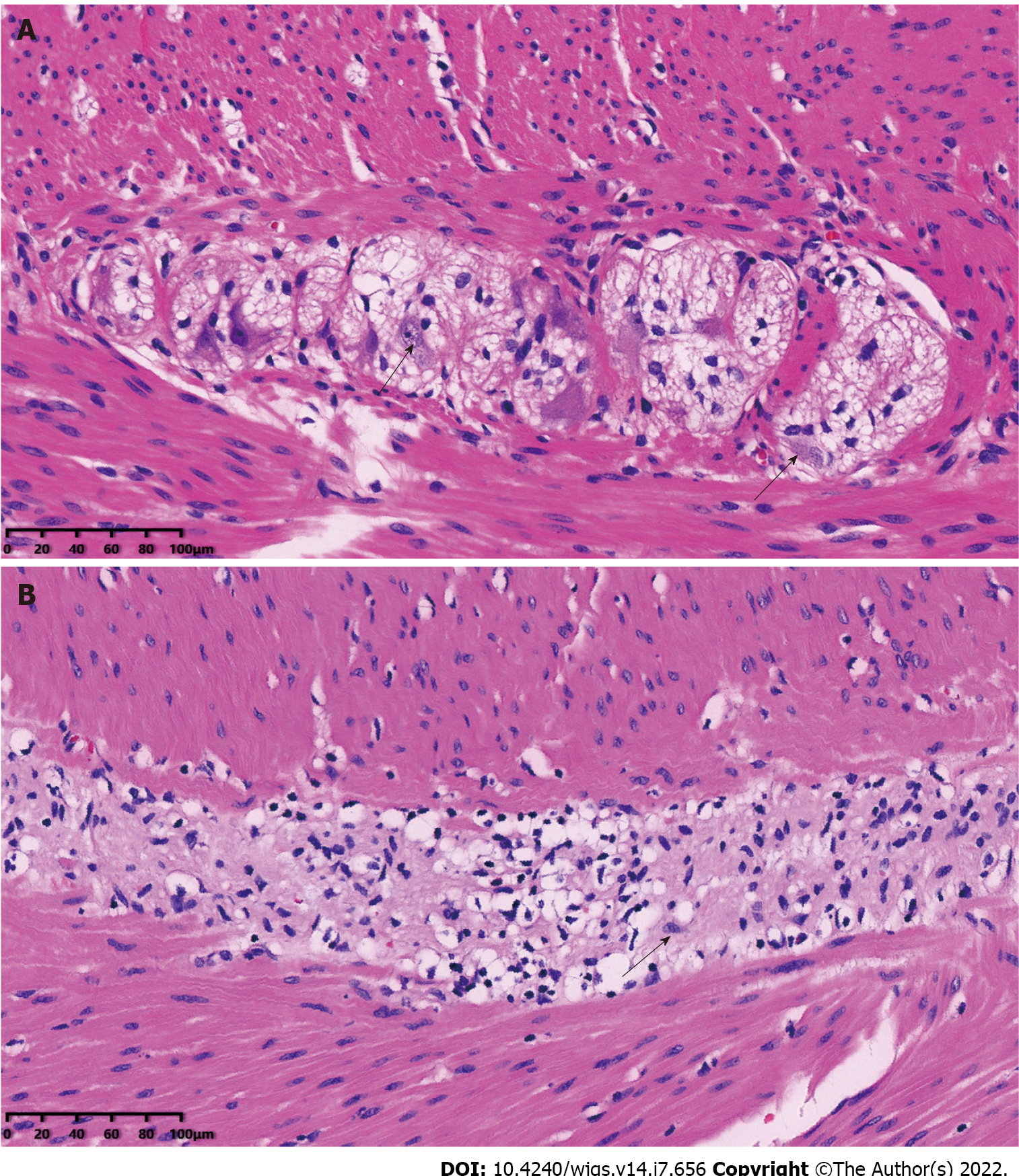
Typical radiographic images obtained from three cases are shown in Figure 3. Patient A was a 70-year-old man with chief complaints of intractable constipation, abdominal distension, and abdominal pain for 1 mo. Abdominal CT showed significant dilatation of gas in the colon (Figure 3A), whereas BE showed a dilated sigmoid colon and barium retention in the sigmoid colon and rectum (Figure 3D). Patient B was a 51-year-old man with intermittent lower abdominal pain and no defecation for 1 mo. Abdominal CT showed a dilated colon with a large amount of fecal content (Figure 3B), while BE showed a dilated middle and upper rectum and a narrow lower rectum (Figure 3E). Patient C was a 22-year-old girl with paroxysmal abdominal pain around the umbilicus and severe constipation for 2 mo. She was the only case that had marked narrowing of the intestinal lumen on enteroscopy. Abdominal CT showed that the whole colon was obviously distensible with gas accumulation and fecal retention (Figure 3C), while enteroscopy revealed significant narrowing of the intestine 40 cm from the anus, which could not be further examined (Figure 3F). The pathological sections of the normal intestinal ganglion and of the resected bowel of ADHD patients (hematoxylin-eosin staining) are shown in Figure 4, respectively. In Figure 4A, the black arrows indicate normal ganglion cells. In Figure 4B, the black arrow indicates the degenerated ganglion cell. The proliferation of nerve fibers and reduction of ganglion cells were also observed.
As shown in Table 2, there were no statistically significant differences in age or sex between the case and control groups (P > 0.05). ADHD patients had a significantly lower body mass index (BMI) than IBS patients (20.2 vs 22.6 kg/m2, P < 0.001). Similarly, cholinesterase and blood chlorine in ADHD patients were remarkably lower than those in IBS patients (P < 0.001). In addition, when compared with the control group, the case group had lower total protein and albumin levels (64.2 vs 69.3 g/L; and 41.2 vs 44.1 g/L, respectively, P < 0.05). Likewise, creatinine, triglyceride, total cholesterol, serum sodium, and blood calcium levels in the case group were distinctly lower than those in the control group (P < 0.05). No significant differences in other indices were found between the two groups (P > 0.05). After initial analysis, variables with a P value < 0.05 were selected and multivariate logistic regression analysis was performed. Since the values of cholinesterase varied widely (from 2020 U/L to 13252 U/L), we included it in the regression by dividing by 1000 according to the method of a previous study[22]. Logistic regression suggested that BMI (OR = 0.786, P = 0.013), cholinesterase (per 1000 units; OR = 0.693, P = 0.008), and blood chlorine (OR = 0.816, P = 0.022) were determined to be independent related factors between ADHD and IBS (Table 3). The AUROC of these three indices combined was 0.812 (95%CI: 0.734-0.890, P < 0.001) (Figure 5). The optimal cutoff value was 0.488 (sensitivity 71.7%, specificity 74.1%, and Euclidean index 0.491). These findings imply that BMI, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and IBS.
| Parameter | Case group (n = 53) | Control group (n = 58) | P value |
| Age (yr) | 48.8 ± 14.3 | 49.8 ± 14.5 | 0.715 |
| Male (n, %) | 18 (34.0%) | 24 (41.4%) | 0.421 |
| Body mass index (kg/m2) | 20.2 (18.8, 21.6) | 22.6 (20.3, 25.0) | < 0.001c |
| White blood cells (× 109/L) | 5.4 (3.9, 6.8) | 5.4 (4.7, 6.4) | 0.512 |
| Neutrocyte proportion (%) | 61.0 ± 14.5 | 57.9 ± 10.0 | 0.190 |
| Lymphocyte proportion (%) | 30.0 ± 14.2 | 32.1 ± 9.5 | 0.371 |
| Red blood cells (× 1012/L) | 4.3 (4.0, 4.6) | 4.4 (4.0, 4.8) | 0.064 |
| Hemoglobin (g/L) | 128.5 ± 16.2 | 133.9 ± 21.9 | 0.141 |
| Platelet count (× 109/L) | 214.0 (171.0, 260.5) | 213.0 (161.8, 245.0) | 0.445 |
| Total protein (g/L) | 64.2 ± 9.6 | 69.3 ± 5.7 | 0.001b |
| Albumin (g/L) | 41.2 ± 7.1 | 44.1 ± 4.3 | 0.014a |
| Alanine aminotransferase (U/L) | 13.0 (9.5, 19.0) | 17.0 (10.8, 27.3) | 0.061 |
| Aspartate aminotransferase (U/L) | 14.0 (17.0, 21.5) | 19.0 (15.0, 26.0) | 0.090 |
| Cholinesterase (U/L) | 6331.0 (4900.5, 7575.0) | 7534.0 (6877.8, 9216.8) | < 0.001c |
| Creatinine (μmol/L) | 61.0 ± 14.2 | 67.2 ± 13.3 | 0.018a |
| Triglyceride (mmol/L) | 1.0 (0.7, 1.3) | 1.2 (0.9, 1.7) | 0.013a |
| Total cholesterol (mmol/L) | 3.9 ± 1.0 | 4.3 ± 0.9 | 0.013a |
| Fasting blood glucose (mmol/L) | 4.8 (4.3, 5.8) | 4.8 (4.0, 5.2) | 0.225 |
| Serum potassium (mmol/L) | 4.0 ± 0.5 | 4.1 ± 0.4 | 0.139 |
| Serum sodium (mmol/L) | 141.0 (139.0, 142.0) | 142.0 (140.0, 143.0) | 0.011a |
| Blood chlorine (mmol/L) | 103.0 (101.0, 105.0) | 104.0 (103.0, 106.0) | 0.009b |
| Blood calcium (mmol/L) | 2.2 (2.1, 2.3) | 2.2 (2.1, 2.3) | 0.254 |
| Serum phosphorus (mmol/L) | 1.1 ± 0.3 | 1.2 ± 0.2 | 0.327 |
| Value | P value | OR | 95%CI |
| Body mass index | 0.013 | 0.786 | 0.649-0.951 |
| Cholinesterase, per 1000 units | 0.008 | 0.693 | 0.527-0.910 |
| Blood chlorine | 0.022 | 0.816 | 0.686-0.971 |
The rarity of ADHD makes it difficult to respond to its clinical features and suspect its diagnosis. To our best of knowledge, our study on the clinical characteristics of adults with ADHD has the largest sample in China, as well as more detailed clinical information about the subjects than previous studies. Our analysis was also from an ED perspective, thus enabling other ED physicians to have a more systematic and comprehensive understanding of the characteristics of ADHD patients. Moreover, we found that the atypical symptoms and negative radiological outcomes of ADHD could also make it more difficult to suspect its diagnosis. Another novel finding was that BMI, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and IBS. We believe that our findings could be helpful for emergency clinicians to lessen the chance of misdiagnosis and mistreatment of adult patients with ADHD.
It is known that 80%-90% of HD patients with delayed passage of meconium and abdominal distension or serious chronic constipation are diagnosed in the neonatal period[23]. Conversely, adult ADHD patients usually have mild symptoms with later onset that are hard to associate with ADHD, thus causing delayed treatment. Many previous studies have described the clinical manifestations of patients with ADHD[24,25], which are in line with the most common symptoms that we found in our study (i.e., abdominal pain, abdominal distension, and constipation). However, we also found uncommon symptoms. We found a right abdominal mass that was caused by dilation of the intestinal cavity in one patient who had difficulty in defecation for a long time. Two cases also presented with severe diarrhea, but their onset symptoms were abdominal distension. This might be related to the progression of the disease; however, these atypical symptoms could also be accidental and concomitant. Nevertheless, this means that the emergency doctor should not only focus on the common symptoms but also be aware of the uncommon ones that may mislead the diagnosis. Notably, 43.4% of the patients had a symptom duration of over 5 years. However, chronic constipation or abdominal distension due to ADHD can be life-threatening. In Japan, an adult female with ADHD died of circulatory failure due to the megacolon compressing the heart, lungs, and inferior vena cava[15]. Another study reported an adult male with ADHD who died of shock caused by intestinal necrosis due to extremely high intra-intestinal pressure[16]. Similarly, both cases had chronic onset at the beginning and also had a long history of intractable constipation, showing no improvements or recurrent attacks after conservative treatment, without further clinical visits or examination. We speculated that these mortalities were due to the late diagnosis and incorrect treatment. Thus, emergency physicians should consider the medical history of ADHD patients, especially those with chronic symptoms who showed no improvement or relapsed despite medication. Further examinations or targeted follow-ups are recommended for patients suspected of having ADHD.
Previous studies have also recommended imaging examinations to make a diagnosis. BE has been effectively used for preoperative evaluation to identify the extent of bowel disease in ADHD[26]. In our study, 17 out of 22 cases examined via BE presented with intestinal dilation and barium retention, while the rest had normal findings. Similar false-negative results were also reported by others in an approximate proportion compared to our study[27,28]. We believe that this could be another reason related to the progression of disease. Although BE has its limitations as a diagnostic tool, it should not be ignored because it can assess both dilated bowels and intestinal motility. Nowadays, enteroscopy has been widely used as the standard procedure for the diagnosis, screening, treatment, and follow-up of many colorectal diseases[29]. This was used in 16 cases in our study, but a large proportion presented with normal results. Only one case had a notably narrow lumen, while a small number of cases had intestinal mucosal abnormalities. Thus, we suggest that the role of colonoscopy in ADHD still needs to be verified in larger samples. In addition, researchers from New York University reported that CT could be used to identify bowel obstruction, with a sensitivity of 94% and specificity of 96%, revealing the correct cause of obstruction in 73% of cases[30]. Rubin[31] also pointed out that, as a key means of examination, CT provides great support for the diagnosis of abdominal diseases. Likewise, Wang et al[32] reported that coronal images on CT scans of the abdomen and pelvis may provide a complete assessment of the overall diameter of the colon. In our study, almost all patients had severe multistage intestinal dilatation, but surprisingly, there was one patient without intestinal dilatation. Thus, emergency clinicians need to be aware that not all adult ADHD patients present with intestinal dilation. Nevertheless, CT can detect sites of intestinal dilatation or stenosis with higher sensitivity and specificity than abdominal radiography[33]. Therefore, we strongly recommend that CT be used to identify ADHD, but if a patient suspected of ADHD has negative results on plain or enhanced CT, the suspicion cannot be ruled out. According to the patient’s medical history and features of symptoms, seeking specialty consultation was conducive, and further examinations were needed in our cases. However, it is also very possible that IBS might be considered by doctors, because IBS would be suspected in a patient with negative imaging examinations combined with obvious abdominal symptoms. Intestinal disorders similar to IBS have also been reported in patients who had previously undergone bowel resection[34]. All patients in our study had undergone enterectomy, implying that some patients may return to the hospital because of such symptoms even after being discharged.
To date, no specific blood index has been reported to identify ADHD. Our regression model showed that BMI, cholinesterase, and blood chlorine have good discrimination between ADHD and IBS (AUROC = 0.812). BMI was recognized as the most popular and common method for nutritional status assessment[35]. It was worth noting that BMI in the case group was significantly influenced by ADHD. There are a few possible reasons for this. First, ADHD patients are more likely to reduce food intake owing to difficulties in smooth defecation, which would result in a lower BMI. Second, ADHD patients usually take laxatives. Regular use of laxatives can give rise to electrolyte loss, steatorrhea, and kidney disturbances including hypokalemia and volume depletion[36]. IBS may also have those problems, but we considered that these behaviors may vary in degree. Meanwhile, ADHD patients had significantly lower levels of cholinesterase. It was reported that cholinesterase could be used as a biomarker of malnutrition[37]. In addition, acetylcholinesterase controls cholinergic nerve and chemical transmission by hydrolyzing the neurotransmitter acetylcholine[38], a major excitatory neuromodulator in the intestinal nervous system[39]. It was also reported that malnourishment caused by chronic obstruction associated with HD can affect the digestion and absorption of nutrients including iron and other blood-forming materials, leading to intractable anemia[40]. Considering all of the above, we concluded that patients with ADHD had worse nutritional status than patients with IBS. The nutritional status of adult patients with ADHD is worthy of further attention. On the other hand, our regression model has good power of discrimination between ADHD and IBS. Further studies are required to evaluate the impact of ADHD on malnourishment.
It was reported that suction rectal biopsy could be used to identify ADHD[41]. However, the procedure is controversial because it collects less amount of mucosa and submucosa, which carries a risk of producing false negatives[42]. Wedel et al[43] also reported that superficial submucous biopsies were not suitable for the diagnosis of hypoganglionosis and its severity. Since it is conducted 2 and 5 cm above the dentate line, this method is effective only if the distance from the lesion is within reach. Meanwhile, biopsy-related complications including perforation, bleeding, and infection were also reported[44]. Full-thickness pathological examination is the gold standard for the diagnosis of ADHD[45]. Immunohistochemistry was widely used in the histopathological diagnosis of ADHD[46]. Currently, hematoxylin and eosin staining, acetylcholinesterase staining, Hu C/D, CD56, S-100 protein, and SOX10 are all used by investigators for diagnosing ADHD[47]. However, full-thickness histopathological examination undoubtedly means that the definitive diagnosis depends on surgical resection of the intestine, which creates a confusing paradox between diagnosis and surgery.
No global consensus has been reached on whether an adult ADHD patient should undergo surgical therapy. For emergency clinicians, understanding the ultimate treatment of this disease can help patients get timely specialist treatment. It was reported that surgical treatment is only appropriate for patients whose symptoms have not improved after at least 6 mo of conservative treatment[8]. In contrast, many studies indicated that pharmaceutic therapy could not fundamentally relieve constipation and abdominal distension in ADHD and that surgical treatment is unavoidable[7,26,48]. In our study, we confirmed that surgical intervention is indeed necessary. All 53 of our patients underwent surgical treatment, and most of them who underwent radical surgery obtained a good prognosis. However, the surgical preference of an ADHD patient is also a factor that should be not ignored. It was reported that a 24-year-old woman underwent subtotal colectomy with a postoperative pathological diagnosis of ADHD, owing to her third recurrence of abdominal pain and no bowel movements for 4 d. The patient had a history of two episodes of bowel obstruction and was planning a second pregnancy; she was worried that such obstruction would probably occur again[49]. Postoperatively, it is important for emergency clinicians to know the possibilities and reasons for recurrence. In our study, three patients had recurrent episodes of constipation and had previously undergone intestinal resection surgery twice before admission. Consequently, two of them developed a peritoneal infection after the third operation. The occurrence of infection might be related to the multiple operations. However, based on the pathological reports of the third operation, they were diagnosed with ADHD, and thus, the infections may have been due to the progression of the disease. However, the possibility of insufficient resection of diseased intestinal segments in previous surgeries also exists. In HD surgery, Kapur et al[50] strongly recommended using intraoperative multipoint frozen rapid examination to ensure that the preserved intestine had a reasonable number of normal ganglion cells. The ganglia-to-nerve fiber ratio could be used in the decision of ADHD surgery[48]. Zhang et al[26] pointed out that the resection range of the bowel could be estimated using BE and 24-h delayed X-ray findings, though unavoidable false negatives may mislead the outcomes. Thus, a surgeon needs to ensure a complete resection of the diseased bowel in ADHD patients.
There were some limitations in our study. First, we enrolled patients who met our inclusion criteria as much as possible, but the sample size was still not large enough, which may result in sampling bias. An additional limitation was that our cases were limited to those diagnosed with ADHD pathologically. Second, as this is a retrospective study, we were limited in our ability to gather detailed outcome data after hospital discharge. Finally, this was a single-center study in a single institution. We intend to conduct a multicenter prospective study to validate our results.
In conclusion, emergency physicians should be vigilant regarding patients with chronic constipation, abdominal pain, or abdominal distension, especially those with recurrent and intolerable symptoms. ADHD should be considered in such cases despite its rarity. Abdominal CT examination is recommended as a useful tool to make a suspected diagnosis of ADHD. Clinicians should also be wary of uncommon symptoms and false-negative imaging findings. BMI, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and IBS. The nutritional status of adult patients with ADHD is worthy of further attention. Surgical treatment for adult patients with ADHD is important and inevitable.
We believe that these findings are beneficial for emergency clinicians to make appropriate suspected diagnoses earlier and reduce misdiagnosis and mistreatment of adult patients with ADHD. In the future, a large-scale study will be used to verify our results and discover more powerful models for ADHD. In addition, we will follow up with the patients for a longer period, including postoperative quality of life, and comparison of nutritional status before and after surgery. Future work requires more in-depth research on the molecular mechanisms, signal pathways, and biomarkers of ADHD.
In the past years, only a few studies with a limited number of adult patients analyzed the clinical features of allied disorders of Hirschsprung’s disease (ADHD).
Although many studies have reported patients presenting to the emergency department (ED) with recurrent abdominal symptoms for a number of disorders, there are few data involving ADHD. It is hard for most ED doctors to associate common abdominal symptoms with ADHD specifically.
To assist ED clinicians in having a more comprehensive understanding of this disease and making an early suspected diagnosis of ADHD more effectively.
We enrolled 53 patients who visited the ED and were eventually diagnosed with ADHD over the past 11 years in our hospital. Their basic information, clinical manifestations, and imaging findings were analyzed. Blood indices were compared between the ADHD and irritable bowel syndrome (IBS) groups.
About 77.4% of adult patients with ADHD had been treated before admission. The transverse colon was the most common dilated part (73.6%), and constipation (67.9%) was the most common symptom. ADHD patients can present with uncommon symptoms and false-negative imaging findings. Logistic regression analysis indicated that body mass index (BMI), cholinesterase, and blood chlorine were determined to be independent related factors between ADHD and IBS.
Emergency physicians should be vigilant regarding patients with chronic constipation, abdominal pain, or abdominal distension, and consider the possibility of ADHD despite its rarity. Abdominal computed tomography examination is recommended as a useful tool in the suspected diagnosis of ADHD. BMI, cholinesterase, and blood chlorine have good discriminative abilities between ADHD and IBS. The nutritional status of adult patients with ADHD is worthy of further attention. Surgical treatment for adult patients with ADHD is important and inevitable.
Large samples will be used to verify our results and discover more powerful models for ADHD. In addition, we will follow up with the patients for a longer period, including postoperative quality of life, and comparison of nutritional status before and after surgery. Future work requires more in-depth research on the molecular mechanisms, signal pathways, and biomarkers of ADHD.
We thank Wen Fang (the First Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou, China) for providing assistance with language editing.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Apiratwarakul K, Thailand; Cabezuelo AS, Spain S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Taguchi T, Ieiri S, Miyoshi K, Kohashi K, Oda Y, Kubota A, Watanabe Y, Matsufuji H, Fukuzawa M, Tomomasa T. The incidence and outcome of allied disorders of Hirschsprung's disease in Japan: Results from a nationwide survey. Asian J Surg. 2017;40:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Fu AX, Lui KN, Tang CS, Ng RK, Lai FP, Lau ST, Li Z, Garcia-Barcelo MM, Sham PC, Tam PK, Ngan ES, Yip KY. Whole-genome analysis of noncoding genetic variations identifies multiscale regulatory element perturbations associated with Hirschsprung disease. Genome Res. 2020;30:1618-1632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Torroglosa A, Villalba-Benito L, Fernández RM, Luzón-Toro B, Moya-Jiménez MJ, Antiñolo G, Borrego S. Identification of New Potential LncRNA Biomarkers in Hirschsprung Disease. Int J Mol Sci. 2020;21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Gershon MD. Hirschsprung disease and more: dysregulation of ERBB2 and ERBB3. J Clin Invest. 2021;131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Friedmacher F, Puri P. Classification and diagnostic criteria of variants of Hirschsprung's disease. Pediatr Surg Int. 2013;29:855-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 7. | Muto M, Matsufuji H, Taguchi T, Tomomasa T, Nio M, Tamai H, Tamura M, Sago H, Toki A, Nosaka S, Kuroda T, Yoshida M, Nakajima A, Kobayashi H, Sou H, Masumoto K, Watanabe Y, Kanamori Y, Hamada Y, Yamataka A, Shimojima N, Kubota A, Ushijima K, Haruma K, Fukudo S, Araki Y, Kudo T, Obata S, Sumita W, Watanabe T, Fukahori S, Fujii Y, Yamada Y, Jimbo K, Kawai F, Fukuoka T, Onuma S, Morizane T, Ieiri S, Esumi G, Jimbo T, Yamasaki T. Japanese clinical practice guidelines for allied disorders of Hirschsprung's disease, 2017. Pediatr Int. 2018;60:400-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Taguchi T, Kobayashi H, Kanamori Y, Segawa O, Yamataka A, Sugiyama M, Iwanaka T, Shimojima N, Kuroda T, Nakazawa A, Oda Y, Miyoshi K, Ieiri S. Isolated intestinal neuronal dysplasia Type B (IND-B) in Japan: results from a nationwide survey. Pediatr Surg Int. 2014;30:815-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Knowles CH, De Giorgio R, Kapur RP, Bruder E, Farrugia G, Geboes K, Lindberg G, Martin JE, Meier-Ruge WA, Milla PJ, Smith VV, Vandervinden JM, Veress B, Wedel T. The London Classification of gastrointestinal neuromuscular pathology: report on behalf of the Gastro 2009 International Working Group. Gut. 2010;59:882-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 192] [Article Influence: 12.8] [Reference Citation Analysis (1)] |
| 10. | Noh CK, Lee KJ. Fecal Microbiota Alterations and Small Intestinal Bacterial Overgrowth in Functional Abdominal Bloating/Distention. J Neurogastroenterol Motil. 2020;26:539-549. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Daniels J, Griffiths M, Fisher E. Assessment and management of recurrent abdominal pain in the emergency department. Emerg Med J. 2020;37:515-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Hakimian D, Benson AA, Khoury T, Massarwa M, Israel S, Salameh S, Gershinsky Y, Shapira B, Muszkat M. Gastrointestinal manifestations of synthetic cannabinoids: a retrospective cohort study. BMC Gastroenterol. 2021;21:274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Pararas N, Rajendiran S, Taha I, Powar RR, Holguera C, Tadros E. Spontaneous Rupture of a Huge Splenic Artery Aneurysm: A Case Report. Am J Case Rep. 2020;21:e919956. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Aldossary MY, Privitera A, Elzamzami O, Alturki N, Sabr K. A Rare Case of Adult-Onset Rectosigmoid Hypoganglionosis. Am J Case Rep. 2018;19:557-561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Nishijima A, Shiotani S, Hayakawa H, Nishijima H. Pseudo-Hirschsprung's disease with rectal hypoganglionosis: an autopsied case of circulatory failure due to severe constipation. Leg Med (Tokyo). 2015;17:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Ito T, Kimura T, Yagami T, Maeda N, Komura M, Ohnishi N, Fujita N, Arai K, Tomioka H, Miyatake S, Kobayashi K. Megacolon in an adult case of hypoganglionosis, a pseudo-Hirschsprung's disease: an autopsy study. Intern Med. 2008;47:421-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Komuro H, Urita Y, Hori T, Hirai M, Kudou S, Gotoh C, Kawakami H, Kaneko M. Perforation of the colon in neonates. J Pediatr Surg. 2005;40:1916-1919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Mecklenburg I, Leibig M, Weber C, Schmidbauer S, Folwaczny C. Recurrent severe gastrointestinal bleeding and malabsorption due to extensive habitual megacolon. World J Gastroenterol. 2005;11:7686-7687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Fournier A, Mondillon L, Luminet O, Canini F, Mathieu N, Gauchez AS, Dantzer C, Bonaz B, Pellissier S. Interoceptive Abilities in Inflammatory Bowel Diseases and Irritable Bowel Syndrome. Front Psychiatry. 2020;11:229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Salari-Moghaddam A, Keshteli AH, Esmaillzadeh A, Adibi P. Adherence to the pro-inflammatory diet in relation to prevalence of irritable bowel syndrome. Nutr J. 2019;18:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Drossman DA, Hasler WL. Rome IV-Functional GI Disorders: Disorders of Gut-Brain Interaction. Gastroenterology. 2016;150:1257-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 731] [Cited by in RCA: 1033] [Article Influence: 114.8] [Reference Citation Analysis (0)] |
| 22. | Keteyian SJ, Patel M, Kraus WE, Brawner CA, McConnell TR, Piña IL, Leifer ES, Fleg JL, Blackburn G, Fonarow GC, Chase PJ, Piner L, Vest M, O'Connor CM, Ehrman JK, Walsh MN, Ewald G, Bensimhon D, Russell SD; HF-ACTION Investigators. Variables Measured During Cardiopulmonary Exercise Testing as Predictors of Mortality in Chronic Systolic Heart Failure. J Am Coll Cardiol. 2016;67:780-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 23. | Dingemann J, Puri P. Isolated hypoganglionosis: systematic review of a rare intestinal innervation defect. Pediatr Surg Int. 2010;26:1111-1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Dunzendorfer T, Lee VW, Levine S, Morenas AD, Beazley RM, Chipkin S. Refractory constipation and megacolon in MEN 2b. Dig Dis Sci. 1996;41:2233-2237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Smith VV, Eng C, Milla PJ. Intestinal ganglioneuromatosis and multiple endocrine neoplasia type 2B: implications for treatment. Gut. 1999;45:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 63] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Zhang HY, Feng JX, Huang L, Wang G, Wei MF, Weng YZ. Diagnosis and surgical treatment of isolated hypoganglionosis. World J Pediatr. 2008;4:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Swenson O, Sherman JO, Fisher JH. Diagnosis of congenital megacolon: an analysis of 501 patients. J Pediatr Surg. 1973;8:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 127] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Taxman TL, Yulish BS, Rothstein FC. How useful is the barium enema in the diagnosis of infantile Hirschsprung's disease? Am J Dis Child. 1986;140:881-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Xu BB, Zhao XL, Xu GP. Clinical study of anesthetization by dezocine combined with propofol for indolent colonoscopy. World J Gastroenterol. 2016;22:5609-5615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Rubesin SE, Herlinger H. CT evaluation of bowel obstruction: a landmark article--implications for the future. Radiology. 1991;180:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Rubin GD. Computed tomography: revolutionizing the practice of medicine for 40 years. Radiology. 2014;273:S45-S74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 32. | Wang XJ, Camilleri M. Chronic Megacolon Presenting in Adolescents or Adults: Clinical Manifestations, Diagnosis, and Genetic Associations. Dig Dis Sci. 2019;64:2750-2756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Jaffe T, Thompson WM. Large-Bowel Obstruction in the Adult: Classic Radiographic and CT Findings, Etiology, and Mimics. Radiology. 2015;275:651-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 34. | Park IJ, Lee JH, Kye BH, Oh HK, Cho YB, Kim YT, Kim JY, Sung NY, Kang SB, Seo JM, Sim JH, Lee JL, Lee IK. Effects of PrObiotics on the Symptoms and Surgical ouTComes after Anterior REsection of Colon Cancer (POSTCARE): A Randomized, Double-Blind, Placebo-Controlled Trial. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Słowik J, Grochowska-Niedworok E, Maciejewska-Paszek I, Kardas M, Niewiadomska E, Szostak-Trybuś M, Palka-Słowik M, Irzyniec T. Nutritional Status Assessment in Children and Adolescents with Various Levels of Physical Activity in Aspect of Obesity. Obes Facts. 2019;12:554-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Roerig JL, Steffen KJ, Mitchell JE, Zunker C. Laxative abuse: epidemiology, diagnosis and management. Drugs. 2010;70:1487-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 105] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 37. | Seo M, Yamada T, Tamaki S, Hikoso S, Yasumura Y, Higuchi Y, Nakagawa Y, Uematsu M, Abe H, Fuji H, Mano T, Nakatani D, Fukunami M, Sakata Y. Prognostic Significance of Serum Cholinesterase Level in Patients With Acute Decompensated Heart Failure With Preserved Ejection Fraction: Insights From the PURSUIT-HFpEF Registry. J Am Heart Assoc. 2020;9:e014100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 38. | Rusu ME, Fizesan I, Pop A, Mocan A, Gheldiu AM, Babota M, Vodnar DC, Jurj A, Berindan-Neagoe I, Vlase L, Popa DS. Walnut (Juglans regia L.) Septum: Assessment of Bioactive Molecules and In Vitro Biological Effects. Molecules. 2020;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 39. | Schacht S, Masood F, Catmull S, Dolan R, Altabtabaee R, Grow W, Al-Nakkash L. Dietary Genistein Influences Number of Acetylcholine Receptors in Female Diabetic Jejunum. J Diabetes Res. 2017;2017:3568146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Sun X, Chu J, Li C, Deng Z. Hirschsprung's disease presenting as intractable anemia: a report of two cases and review of the literature. BMC Pediatr. 2020;20:525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 41. | Wu XJ, Zhang HY, Li N, Yan MS, Wei J, Yu DH, Feng JX. A new diagnostic scoring system to differentiate Hirschsprung's disease from Hirschsprung's disease-allied disorders in patients with suspected intestinal dysganglionosis. Int J Colorectal Dis. 2013;28:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 42. | Meier-Ruge WA, Brönnimann PB, Gambazzi F, Schmid PC, Schmidt CP, Stoss F. Histopathological criteria for intestinal neuronal dysplasia of the submucosal plexus (type B). Virchows Arch. 1995;426:549-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 43. | Wedel T, Roblick UJ, Ott V, Eggers R, Schiedeck TH, Krammer HJ, Bruch HP. Oligoneuronal hypoganglionosis in patients with idiopathic slow-transit constipation. Dis Colon Rectum. 2002;45:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 44. | Watanabe Y, Ito F, Ando H, Seo T, Kaneko K, Harada T, Iino S. Morphological investigation of the enteric nervous system in Hirschsprung's disease and hypoganglionosis using whole-mount colon preparation. J Pediatr Surg. 1999;34:445-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 45. | Feichter S, Meier-Ruge WA, Bruder E. The histopathology of gastrointestinal motility disorders in children. Semin Pediatr Surg. 2009;18:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Park SH, Min H, Chi JG, Park KW, Yang HR, Seo JK. Immunohistochemical studies of pediatric intestinal pseudo-obstruction: bcl2, a valuable biomarker to detect immature enteric ganglion cells. Am J Surg Pathol. 2005;29:1017-1024. [PubMed] |
| 47. | Yoshimaru K, Taguchi T, Obata S, Takemoto J, Takahashi Y, Iwanaka T, Yanagi Y, Kuda M, Miyoshi K, Matsuura T, Kinoshita Y, Yoshioka T, Nakazawa A, Oda Y. Immunostaining for Hu C/D and CD56 is useful for a definitive histopathological diagnosis of congenital and acquired isolated hypoganglionosis. Virchows Arch. 2017;470:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 48. | Gasparovic I, Kovac D, Persic M, Slavic I, Nikolic H, Jonjic N. Ganglia/nerve fibers ratio correlates with the need for surgery in patients diagnosed with Hirschsprung's disease allied disorder (HAD). Fetal Pediatr Pathol. 2011;30:405-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Qiu J, Yang G, Lin A. Allied disorders of Hirschsprung's disease. Tech Coloproctol. 2019;23:509-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Kapur RP. Histology of the Transition Zone in Hirschsprung Disease. Am J Surg Pathol. 2016;40:1637-1646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |