Published online Jun 27, 2022. doi: 10.4240/wjgs.v14.i6.621
Peer-review started: November 25, 2021
First decision: January 8, 2022
Revised: January 23, 2022
Accepted: May 16, 2022
Article in press: May 16, 2022
Published online: June 27, 2022
Processing time: 213 Days and 18.2 Hours
In adults, bowel intussusception is a rare diagnosis and is mostly due to an organic bowel disorder. In rare cases, this is a complication of a percutaneously placed endoscopic gastro (jejunostomy) catheter.
We describe a case of a 73-year-old patient with a history of myocardial infarction, chronic idiopathic constipation and Parkinson’s disease. For the admission of his Parkinson’s medication, a percutaneous endoscopic gastrostomy with jejunal extension (PEG-J) was placed. The patient presented three times at the emergency department of the hospital with intermittent abdominal pain with nausea and vomiting. There were no distinctive abnormalities from the physical and laboratory examinations. An abdominal computed tomography scan showed a small bowel intussusception. By push endoscopy, a jejunal bezoar at the tip of the PEG-J catheter was found to be the cause of small bowel intussusception. The intussusception was resolved after removing the bezoar during push enteroscopy.
Endoscopic treatment of bowel intussusception caused by PEG-J catheter bezoar.
Core Tip: In patients with a proximal feeding catheter and complaints of acute or intermittent abdominal pain, intussusception must be considered. An abdominal computed tomography scan is recommended for additional investigation. If small bowel intussusception is present/suspected, we recommend first investigating the cause via gastroscopy/push enteroscopy and, if possible, treating it endoscopically immediately so that surgery can be prevented.
- Citation: Winters MW, Kramer S, Mazairac AH, Jutte EH, van Putten PG. Bowel intussusception caused by a percutaneously placed endoscopic gastrojejunostomy catheter: A case report. World J Gastrointest Surg 2022; 14(6): 621-625
- URL: https://www.wjgnet.com/1948-9366/full/v14/i6/621.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i6.621
If normal oral intake of food or medication is insufficient or poorly tolerated for a longer period of time, an endoscopically placed percutaneous gastric tube (PEG) can be considered. PEG can be extended to the jejunum (PEG-J) or placed directly in the jejunum (PEJ). These procedures are considered to be safe[1-3]. Common complications of a PEG are a clogged or dislocated PEG catheter, pain at the insertion site, infection and peristomal leakage. Severe complications are rare, including bleeding, perforation, buried bumper syndrome, necrotizing fasciitis and metastatic spread[1,2]. In this case, we describe proximal intussusception of the small intestine as a rare complication of a PEG-J catheter.
The patient was a 73-year-old man who visited the emergency care centre on three occasions in three weeks with intermittent epigastric and lower thoracic pain accompanied by nausea and vomiting.
At the first two presentations, no clear leads were found in anamnesis, physical examination or exploratory additional examinations. No abnormalities were found on point-of-care ultrasound of the abdominal wall or abdomen. Additionally, no anomaly of the PEG-J catheter was found. There were no signs of myocardial ischaemia, as indicated by a normal electrocardiogram (ECG) and troponins. Gastroscopy showed candida oesophagitis, for which fluconazole was prescribed. Due to chronic constipation, laxatives were also started. During the last presentation, the stool pattern had improved, and defecation was daily and of normal consistency.
The patient had a history of myocardial infarction, chronic idiopathic constipation and Parkinson’s disease. PEG-J (AbbVie PEG 15 Fr; J extension 9 Fr) was placed 1.5 years ago for the administration of Parkinson medication (levodopa/carbidopa).
The patient has no personal and family history.
On physical examination, the patient was damp and sweaty, with normal vitals: Heart rate (67/min), blood pressure (141/80 mmHg) and temperature (36.6 °C). Auscultation of the heart and lungs showed a regular heart rhythm without murmur and clear lung sounds. During abdominal examination, sparse, normal-sounding peristalsis was heard. Palpation gave severe pressure pain in the upper left abdomen and in the epigastrio, without rebound pain. No rigidity or guarding was observed. The insertion of the PEG catheter appeared normal without redness, bleeding or hard subcutaneous swelling. PEG-J was open and well situated against the abdominal wall and easy to submerge and reapply.
The laboratory examinations showed (normal values in parentheses) mildly elevated C-reactive protein of 39 mg/L (< 5), normal lipase of 14 U/L (< 60) and a stable troponin-T of 16 ng/L compared to three days prior (< 14). Renal and liver function were normal. Remarkably, an elevated creatine kinase of 366 U/L (< 200) and a mildly elevated lactate of 2.2 mmol/L (0.5-1.6) were detected. The ECG showed a sinus rhythm of 68/min, with no ST-T abnormalities.
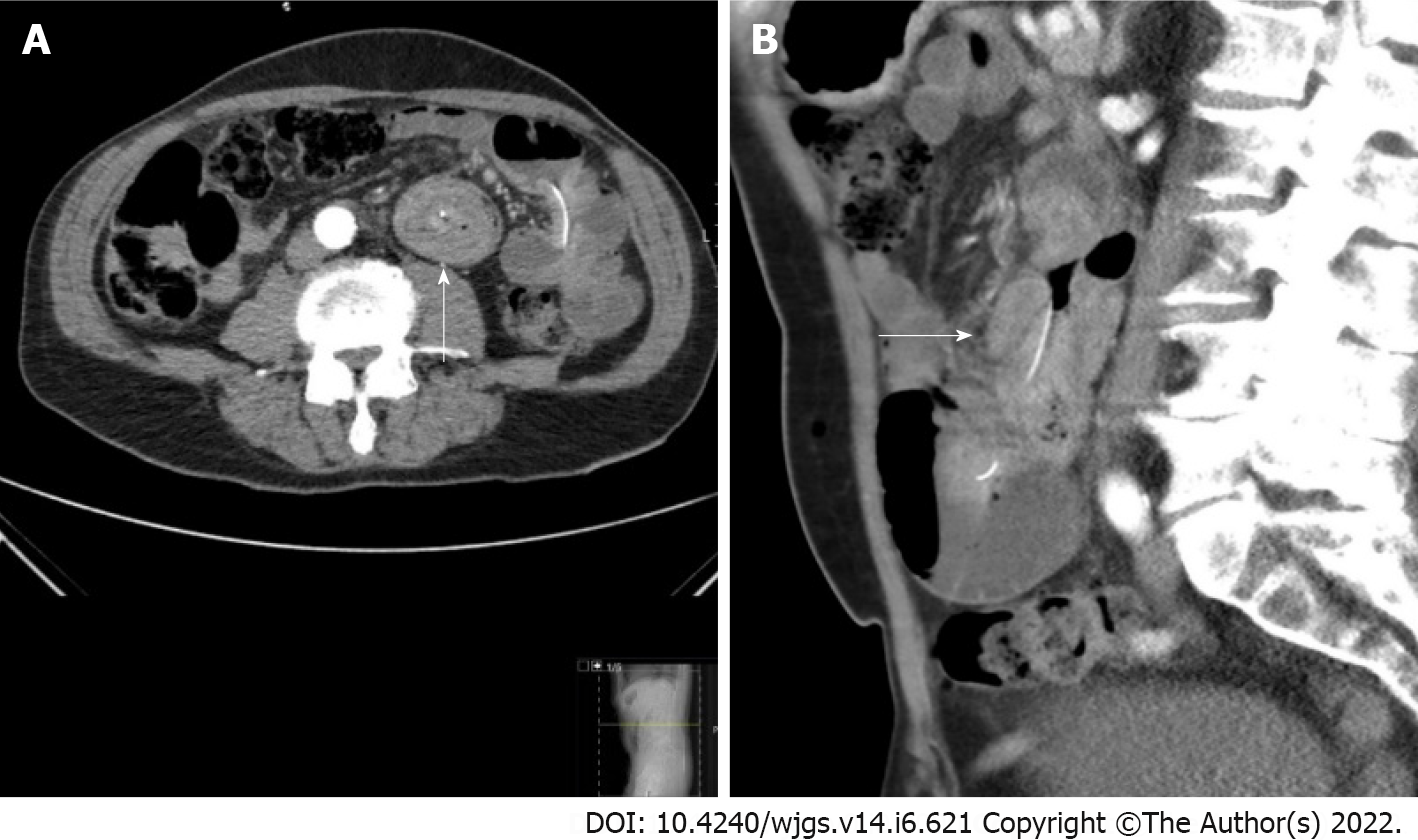
In the differential diagnosis of peptic/duodenal ulcer disease, cholecystitis, perforation, constipation due to bowel mobility problems in Parkinson’s disease, intestinal ischaemia and a complication of PEG-J were considered. Due to these considerations, abdominal computed tomography (CT) scans were performed with intravenous contrast in the arterial and portal venous phases (Figure 1), which showed intussusception at the duodenojejunal junction. There was no evident leadpoint for intussusception, and the intestinal loops proximal to intussusception were not dilated.
Small bowel intussusception.
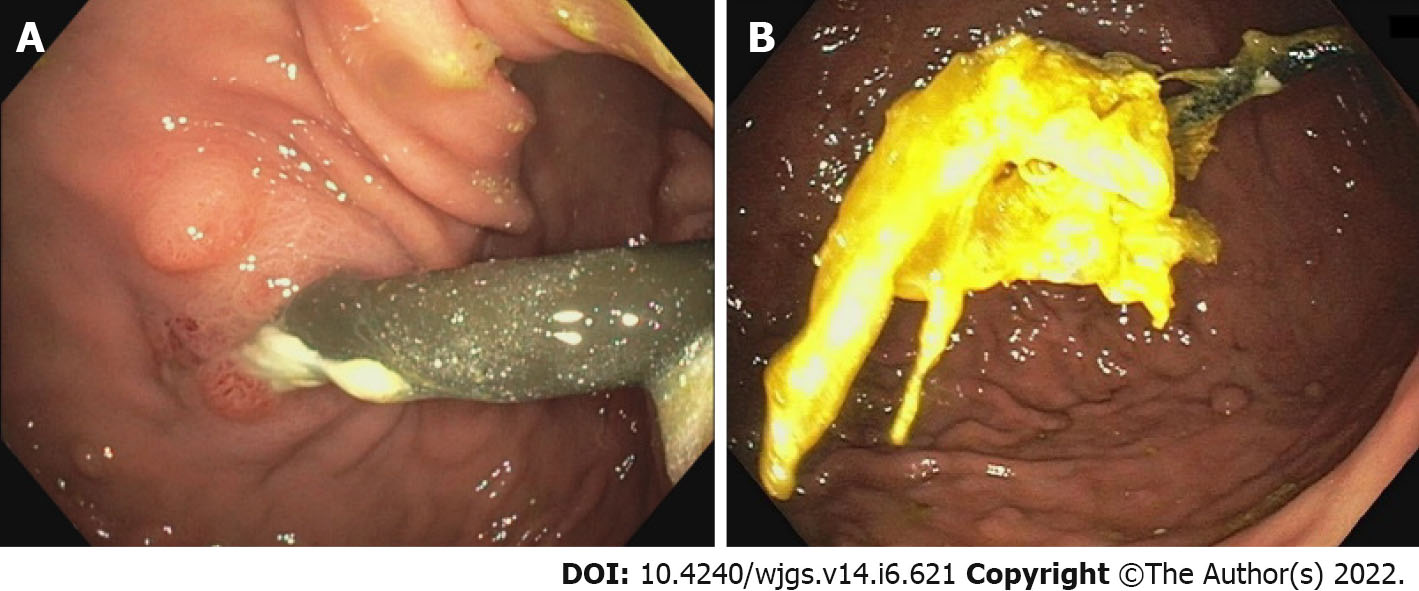
Proximal push enteroscopy was performed on suspicion of an intussusception possibly caused by PEG-J, a malignant or benign tumor. The button of the PEG was not situated against the stomach wall, and there was traction at the jejunum extension (Figure 2A). A lumen-filling bezoar, i.e., a stony mass, was found in the small intestine at the distal part of the jejunum extension. The bezoar was reduced endoscopically, after which the jejunal extension luxated and returned to the stomach with the remnant of the bezoar (Figure 2B). The jejunum extension was replaced, and the patient was discharged in good condition.
On the first outpatient revision, the patient had no complaints.
Bowel intussusception, in which a part of the intestine slides into the next part of the intestine (“telescoping”), is rare in adults. In adults, 1%-5% of intestinal obstructions are caused by intussusception. Most cases (90%) are due to an organic condition, such as inflammatory bowel disease, postoperative adhesions, (Meckel’s) diverticula, polyps or carcinoma. An iatrogenic factor is sometimes the cause of intussusception, such as after bariatric surgery or in the presence of intestinal feeding probes[4].
The use of PEG catheters is increasing in popularity because it is considered to be a safe method for the administration of nutrition and medication[1]. Severe complications of a PEG-J catheter are rare, and few case reports have described intussusception after the placement of PEG catheters (PEG/PEG-J/PEJ)[5-8]. Only one similar case has been described in the literature, in which a bezoar was attached to the distal end of a jejunum extension of a PEG[5]. The most likely mechanism causing intussusception in our case was the formation of a bezoar at the jejunum extension and the migration of this bezoar distally through the small intestine by intestinal peristalsis. This served as a lead point, causing intussusception.
Symptoms of intussusception in adults are often nonspecific and can be both acute or chronic. The most common symptom is abdominal pain. Other complaints include nausea, vomiting, gastrointestinal bleeding, abdominal distension and constipation[4,9]. Other PEG complications that can cause similar nonspecific symptoms include, i.e., malpositioning of the PEG, gastric/bowel perforation, or migration of the PEG catheter balloon into the pylorus or duodenum[1,10,11].
If a complication of PEG is suspected, a CT scan should be considered to differentiate between the complications of PEG. In adults, a CT abdomen is preferred in the diagnosis of intussusception because of its 90%-100% accuracy. A “target sign”, “sausage sign” or oedematous wall thickening will be observed. Comparatively, ultrasounds have an accuracy of 50%-60%, while X-rays are not sensitive[9,12]. As intussusception in adults is often caused by organic abnormalities, surgery is the most common intervention[12].
Our case illustrates that PEG can be complicated by proximal intussusception of the small intestine. Our advice is to perform imaging for intussusception when a patient with a PEG catheter has acute or intermittent abdominal pain. In addition, when intussusception is diagnosed, a patient should first undergo endoscopic exploration while being treated, if possible, to avoid more invasive surgical treatment.
Intussusception is a rare complication of a PEG catheter, with nonspecific clinical presentation. In patients with a PEG catheter complaining of acute or chronic abdominal pain with nausea, vomiting or obstipation, intussusception should be considered. The most accurate diagnostic tool is a CT scan. In cases of intussusception of the small intestine, we recommend immediately exploring and if possible, treating the intussusception endoscopically, to prevent surgical intervention.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Netherlands
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sato Y, Japan; Zharikov YO, Russia A-Editor: Yang YZ S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014;20:7739-7751. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 416] [Cited by in RCA: 340] [Article Influence: 30.9] [Reference Citation Analysis (8)] |
| 2. | Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014;20:8505-8524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 325] [Cited by in RCA: 269] [Article Influence: 24.5] [Reference Citation Analysis (10)] |
| 3. | Chang FC, Kwan V, van der Poorten D, Mahant N, Wolfe N, Ha AD, Griffith JM, Tsui D, Kim SD, Fung VS. Intraduodenal levodopa-carbidopa intestinal gel infusion improves both motor performance and quality of life in advanced Parkinson's disease. J Clin Neurosci. 2016;25:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 507] [Article Influence: 31.7] [Reference Citation Analysis (2)] |
| 5. | Dixon R, Burton S, Taylor LJ, Richeson BL, Fang JC. Bezoar formation on percutaneous endoscopic gastrojejunostomy tube causing gastric outlet obstruction and small-intestinal intussusception. VideoGIE. 2019;4:416-417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Kakiuchi T, Nakayama A, Nojiri J, Yamanouchi T, Matsuo M. Jejuno-jejunal intussusception caused by a percutaneous endoscopic gastrojejunostomy tube in a pediatric patient: A case report. Medicine (Baltimore). 2020;99:e19888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ibegbu E, Relan M, Vega KJ. Retrograde jejunoduodenogastric intussusception due to a replacement percutaneous gastrostomy tube presenting as upper gastrointestinal bleeding. World J Gastroenterol. 2007;13:5282-5284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Satoh T, Sawada K, Satoh M, Yohko K, Yamada M, Zaitsu M, Osada T, Sawaya R, Nata T, Ueno N, Moriichi K, Ikuta K, Mizukami Y, Watari J, Fujiya M, Kohgo Y. Small intestinal intussusceptions due to the placement of a percutaneous endoscopic jejunostomy tube. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Honjo H, Mike M, Kusanagi H, Kano N. Adult intussusception: a retrospective review. World J Surg. 2015;39:134-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 170] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | Shah J, Sunkara T, Yarlagadda KS, Rawla P, Gaduputi V. Gastric Outlet and Duodenal Obstruction as a Complication of Migrated Gastrostomy Tube: Report of Two Cases and Literature Review. Gastroenterology Res. 2018;11:71-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Becker BA, Walker TC. Gastric Outlet Obstruction Due to Malposition of Replacement Gastrostomy Tube. Clin Pract Cases Emerg Med. 2019;3:442-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303-3308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 142] [Cited by in RCA: 153] [Article Influence: 9.6] [Reference Citation Analysis (0)] |