Published online Mar 27, 2022. doi: 10.4240/wjgs.v14.i3.247
Peer-review started: September 27, 2021
First decision: December 4, 2021
Revised: December 9, 2021
Accepted: February 16, 2022
Article in press: February 16, 2022
Published online: March 27, 2022
Processing time: 179 Days and 0.9 Hours
Peroral endoscopic myotomy (POEM) has been demonstrated to be safe and effective in the treatment of achalasia. Longer myotomy is the standard POEM procedure for achalasia but when compared with shorter myotomy, its effectiveness is not as well known.
To compare the clinical effectiveness of longer and shorter myotomy.
PubMed, EmBase, Cochrane Library, web of science and clinicaltrials.gov were queried for studies comparing shorter and longer POEM for achalasia treatment. The primary outcome was clinical success rate. Secondary outcomes comprised of operative time, adverse events (AEs) rate, gastroesophageal reflux disease (GERD) and procedure-related parameters. The Mantel-Haenszel fixed-effects model was primarily used for the analysis. Publication bias was assessed.
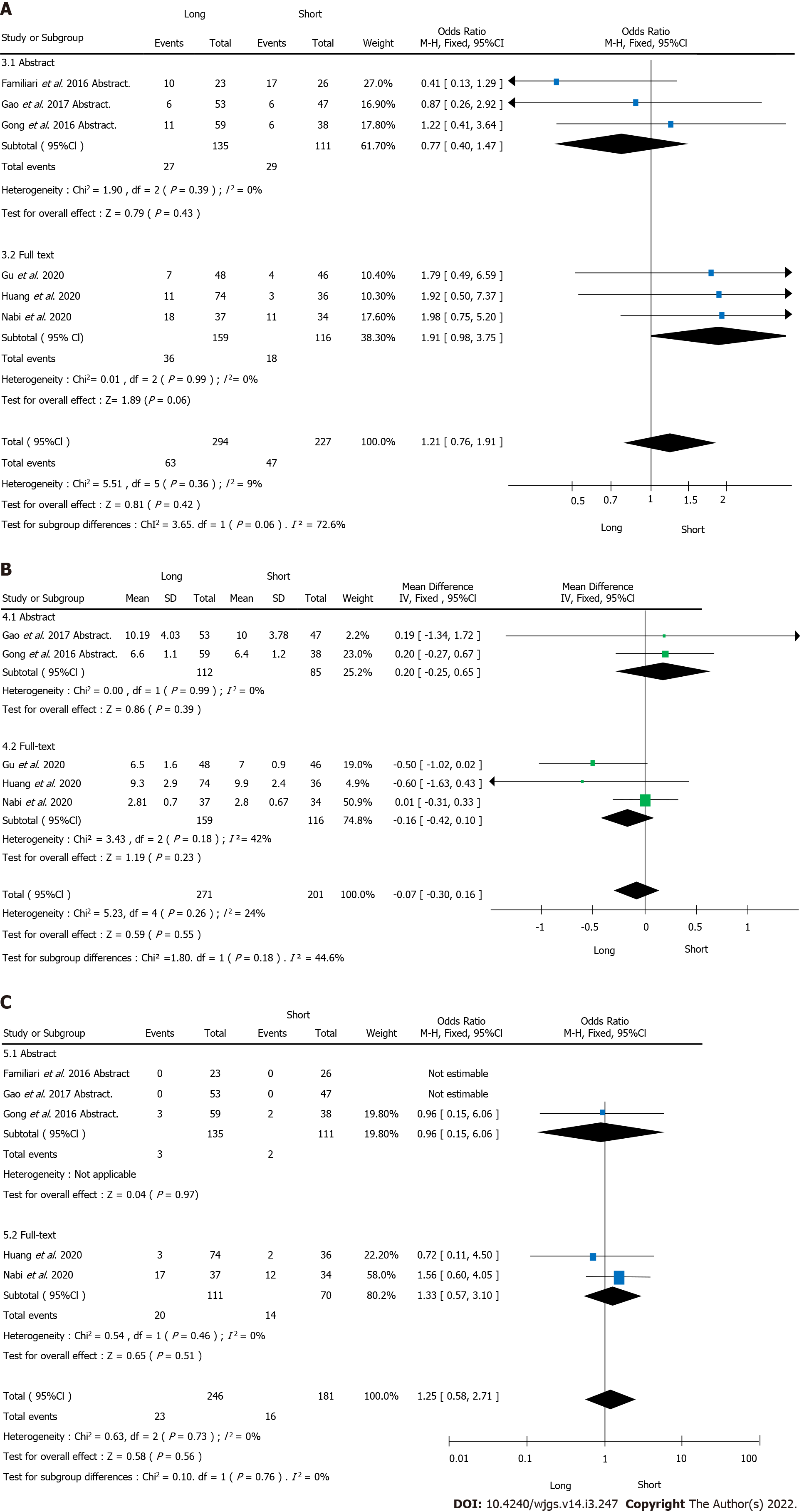
Six studies were included in this analysis with a total of 514 participants. During the follow-up period of 1-28.7 mo, longer and shorter myotomy in treating achalasia showed similar excellent effectiveness [overall clinical success (OR = 1, 95%CI: 0.46-2.17, P = 1, I2: 0%; subgroup of abstract (OR = 1.19, 95%CI: 0.38 to 3.73; P = 0.76; I2: 0%); subgroup of full text (OR = 0.86 95%CI: 0.30 to 2.49; P = 0.78; I2: 0%)]. Shorter myotomy had significantly reduced mean operative time compared with the longer procedure. There were no statistically significant differences in AEs rates, including GERD (overall OR = 1.21, 95%CI: 0.76-1.91; P = 0.42; I2: 9%; subgroup of abstract OR = 0.77, 95%CI: 0.40-1.47; P = 0.43; I2: 0%; subgroup of full text OR = 1.91, 95%CI: 0.98-3.75; P = 0.06; I2: 0%), hospital stay (overall MD = -0.07, 95%CI: -0.30 to 0.16; P = 0.55;
POEM was effective in treating achalasia. Shorter and longer myotomy procedures provided similar therapeutic effects in terms of long-term effectiveness. In addition, shorter myotomy reduced the operative time.
Core Tip: We evaluated the peroral endoscopic longer vs shorter myotomy for achalasia treatment in our study. To our knowledge, this is the first meta-analysis aiming to compare longer and shorter myotomy during peroral endoscopic myotomy for the treatment of achalasia regarding clinical success, safety and procedure-related outcomes. Shorter and longer myotomy procedures showed similar therapeutic effects in terms of long-term effectiveness. In addition, shorter myotomy reduced the operative time.
- Citation: Weng CY, He CH, Zhuang MY, Xu JL, Lyu B. Peroral endoscopic longer vs shorter esophageal myotomy for achalasia treatment: A systematic review and meta-analysis. World J Gastrointest Surg 2022; 14(3): 247-259
- URL: https://www.wjgnet.com/1948-9366/full/v14/i3/247.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i3.247
Achalasia is a rare esophageal motor disease with a prevalence of approximately 1 case/100000 adults. The pathophysiology of achalasia disorder involves incomplete relaxation of the lower esophageal sphincter (LES) and impaired esophageal peristalsis[1]. Its clinical manifestations comprise dysphagia, regurgitation, chest pain and weight loss. Currently, endoscopic botulinum toxin injection or pneumatic dilation and laparoscopic Heller myotomy (LHM) are used to treat achalasia[2]. Inoue and colleagues[3] carried out the first peroral endoscopic myotomy (POEM) surgery to treat 17 achalasia patients in 2010 with 100% technical success. POEM is a novel, minimally invasive therapeutic modality for achalasia and related disorders, which was first reported by Inoue et al[3] in 2010. Since then, POEM has been widely used in the treatment of achalasia in many studies and achieves excellent efficacy[4-7].
However, the technique of POEM has changed very little since its introduction[3]. During POEM, the variable extent of gastric myotomy and esophageal myotomy range from 2 cm to 3 cm and 6 cm to 10 cm, respectively. Meanwhile, previous studies have demonstrated the significance of the extent of the myotomy on the gastric side[8,9]. However, the clinical relevance of myotomy length on the esophagus remains unknown. Some researchers have also adopted shorter myotomy in POEM and achieved similar efficacy in recent years[10].
The existing literature lacks high-quality evidence to compare the clinical outcomes of short-length and long-length POEM for achalasia treatment. Furthermore, for shorter or longer myotomy in POEM, which is more effective remains unknown. In this study, we compared the two myotomy modalities based on clinical outcomes and the incidence of postoperative adverse events.
The present systematic review and meta-analysis was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. PubMed, EmBase, Web of Science, Cochrane Library and clinicaltrials.gov databases were searched for relevant studies published from January 2010 to October 2020, because POEM was first reported in humans in 2010[3]. The searching language of publications was restricted to English. The Medical Subject Headings (MESH) terms employed included Achalasia’s, Esophageal OR Esophageal Achalasia’s OR Cardiospasm OR Cardiospasms OR Achalasia OR Achalasia’s OR Achalasia, Esophageal OR Megaesophagus OR Esophageal Achalasia AND POEM OR Peroral endoscopic myotomy OR esophageal myotomy OR Per-oral endoscopic myotomy AND shorter OR longer OR modified. The reference lists of eligible articles were further assessed for additional studies of interest. Two investigators independently performed the search and data extraction, assessed the quality of the articles and the discrepancies were resolved by consensual discussion. The third investigator reviewed the extracted data. Discussion with senior authors solved any arising issues. Randomized clinical trials (RCTs) and retrospective studies were qualified for the search.
Article title and abstract eligibility screening was performed in an independent way by two investigators. Open-label double-blinded RCTs, as well as retrospective trials evaluating patients and comparing peroral endoscopic shorter and longer myotomy for the treatment of achalasia were included. Exclusion criteria were: (1) Experimental studies; (2) Publication language other than English; and (3) An editorial, a case report, a review or case series.
The data parameters obtained from each study were: (1) Trial features such as study design, sample size, follow-up duration and publication year; (2) Primary outcome, i.e. clinical success; and (3) Secondary outcomes, including (i) operative time, (ii) GERD (the main indicator was endoscopic reflux esophagitis), (iii) total number of adverse events (AEs) such as major bleeding, and (iv) procedure-related parameters.
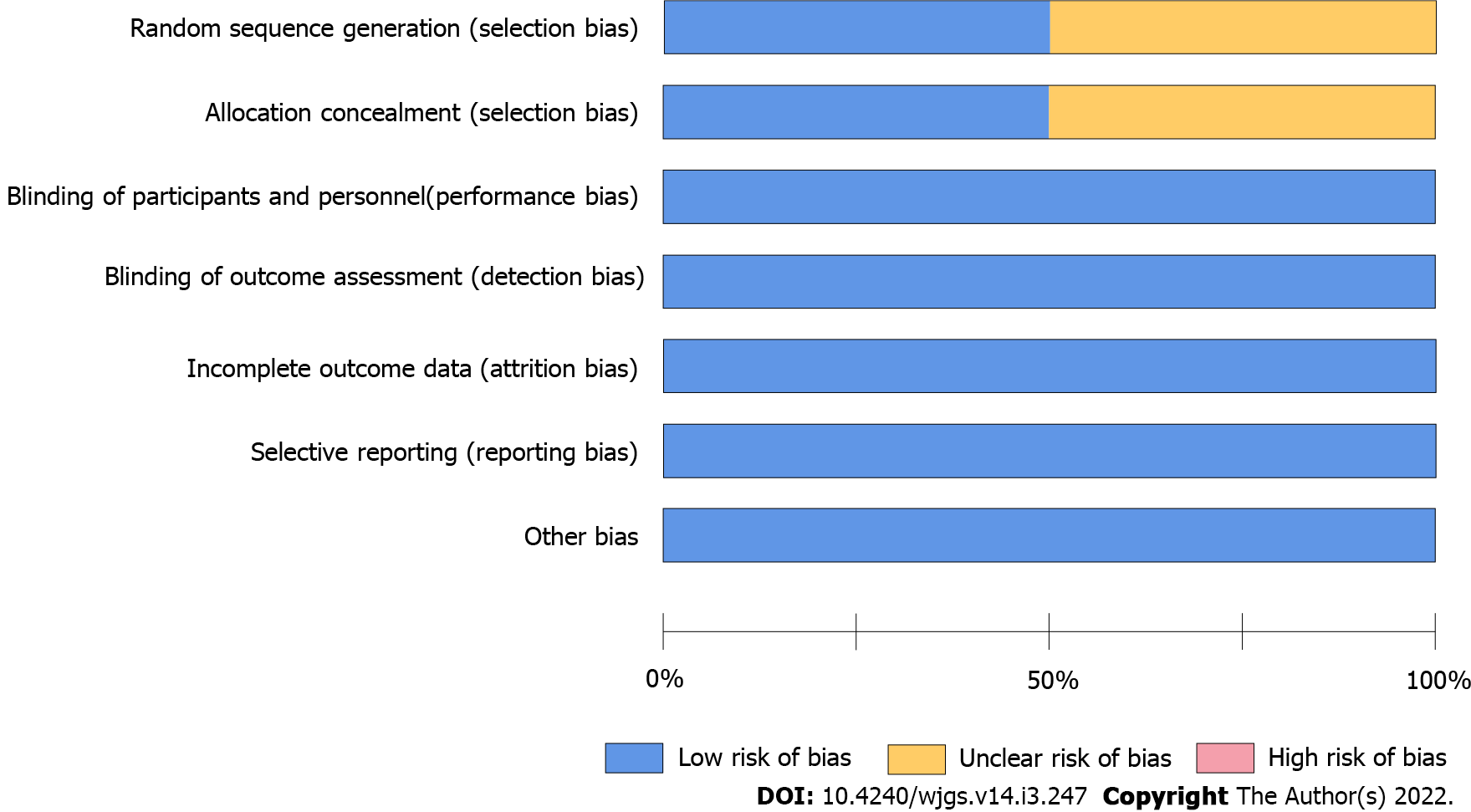
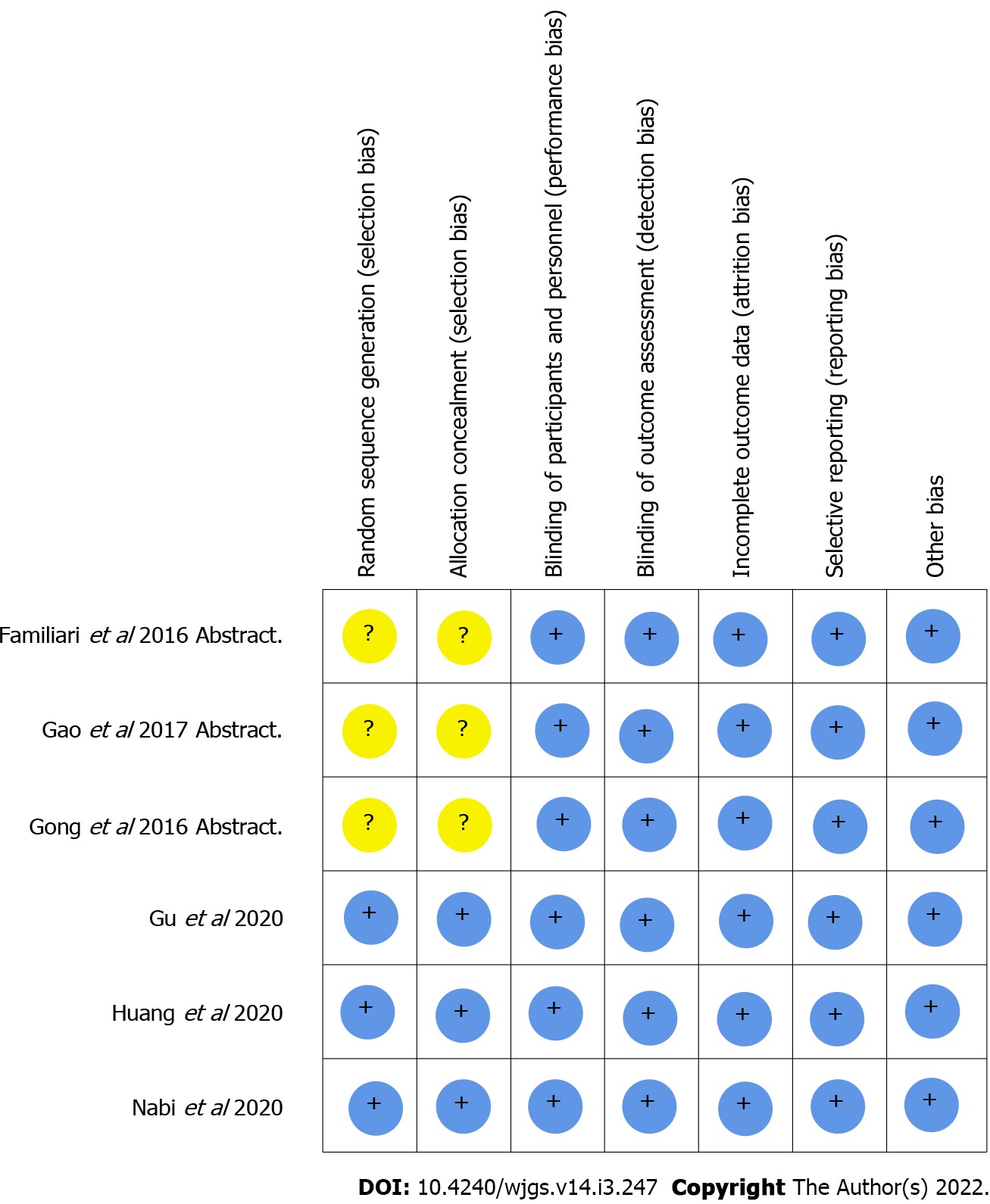
The Cochrane “risk of bias” tool and the Newcastle-Ottawa Scale (NOS) were employed for assessing methodological quality of included studies[11]. Discrepancies between the two investigators were resolved by consensual discussion.
Review Manager 5.3 (RevMan) was utilized to analyze the extracted data and determine odds ratios (ORs) and 95% confidence intervals (CIs). Heterogeneity was determined by inspection of forest plots, the Cochrane Q test, and the I² statistic. A Q test with P<0.10 was considered significant. According to the Cochrane Handbook for Systematic Reviews of Interventions (https://training.cochrane.org/handbook), I² values were categorized as: < 30%, low heterogeneity; 30%-50%, moderate heterogeneity; > 50%, substantial heterogeneity; > 75%, high heterogeneity.
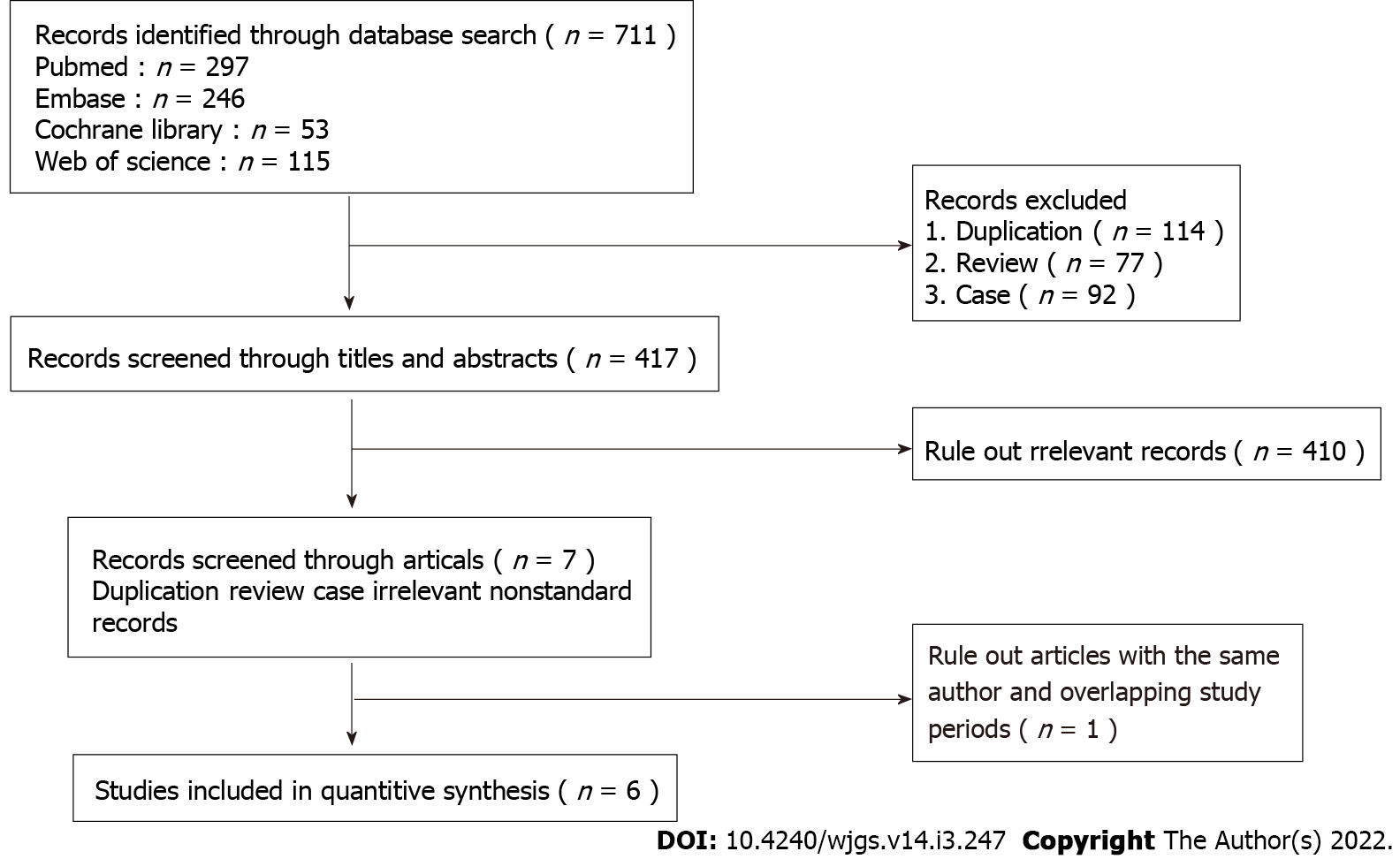
Details of the selection process were outlined in Figure 1. Overall, 711 articles were initially selected. After ruling out duplicates, reviews, case series, irrelevant and nonstandard records, 6 studies were included which involved 3RCTs and 3 retrospective trials[12-17] and covered 545 patients. Their features are summarized in Table 1. The quality assessment of the studies was depicted in Figure 2. No significant differences were found in age, sex, American Society of Anesthesiologists (ASA) classification and previous interventions[18]. The detailed study quality evaluation items were presented in Table 2. Compared with the long myotomy (LM) group, the length of esophageal myotomy in the short myotomy (SM) group was significantly reduced. The total incision range of the LM group was 8-25 cm, including 6-20 cm on the esophagus and 2-5 cm on the stomach. For the SM group, the cut range was 3-7cm, including 2-6 cm on the esophagus and 1-3 cm on the stomach.
| Ref. | Total sample | Sex, male/female, n | Age, yr | Symptoms duration, yr or mo | MBI | Classification, n (%) | Pre-ECK scores | LESP, mmHg | IRP, mmHg |
| Familiari et al[15], 2016 | LM: 38 | NA | NA | NA | NA | NA | NA | NA | NA |
| SM: 35 | |||||||||
| Gao et al[16], 2017 | LM: 53 | LM: 29/24; SM: 25/22 | LM: 37.83 ± 14.36 | LM: 5.23 ± 5.87 | LM: 19.76 ± 3.07 | NA | LM: 6.75 ± 1.86 | LM: 43.03 ± 13.73 | NA |
| SM: 47 | SM: 43.96 ± 11.69 | SM: 5.30 ± 4.87 | SM: 20.25 ± 2.97 | SM: 6.34 ± 1.74 | SM: 41.93 ± 14.93 | ||||
| Gong et al[17], 2016 | LM: 59; SM: 38 | Female; LM: 29; SM: 19 | LM: 39.8 ± 12.4; SM: 41.5 ± 7.2 | LM: 6.5 ± 5.5; SM: 7.9 ± 4.3 | LM: 20.7 ± 2.6; SM: 20.1 ± 3.2 | ASAC I: LM: 47; SM: 29; II: LM: 11; SM: 7; III: LM: 1; SM: 2; CC I: LM: 21; SM: 12 II: LM: 38; SM: 26 | LM: 7.2 ± 2.4; SM: 6.8 ± 1.7 | LM: 42.1 ± 12.9; SM: 44.6 ± 13.2 | NA |
| Gu et al[14], 2020 | LM: 48; SM: 46 | LM: 23/25; SM: 21/25 | LM: 42.8 ± 10.2; SM: 43.6 ± 11.4 | LM: 4.1(0.3~31.0); SM: 5.0(0.3~34.0) | NA | CC II: LM: 48; SM: 46 | LM: 7.1 ± 1.6; SM: 7.5 ± 1.5 | LM: 32.4 ± 5.3; SM: 33.5 ± 5.0 | LM: 21.5 ± 4.6; SM: 23.2 ± 4.8 |
| Huang et al[13], 2020 | LM: 74; SM: 36 | Female; LM: 34; SM: 17 | LM: 37.7 ± 13.0; SM: 40.8 ± 11.1 | LM: 8.9 ± 5.8; SM: 8.8 ± 5.5 | LM: 19.4 ± 3.1; SM: 20.3 ± 2.6 | ASAC I: LM: 58; SM: 33; II: LM: 15; SM: 2; III: LM: 1; SM: 1; CC I: LM: 26; SM: 12; II: LM: 48; SM: 24 | LM: 7.5 ± 1.9; SM: 7.1 ± 1.6 | LM: 39.8 ± 13.7; SM: 41.8 ± 14.3 | NA |
| Nabi et al[12],2020 | LM: 37; SM: 34 | LM: 24/13; SM: 18/16 | LM: 41.3 ± 14.4; SM: 40.1 ± 16.8 | LM: 3;SM: 3 | NA | ASAC I: LM: 13; SM: 12; II: LM: 24; SM: 22 | LM: 6.75 ± 1.32; SM: 6.02 ± 1.33 | NA | LM: 28.50 ± 11.01; SM: 26.40 ± 13.9 |
| Ref. | Follow-up sample | Length of the myotomy, cm | Operative time, min | Myotomy length, cm | Follow-up time, mo | Clinical success | GERD, % | LESP, mmHg | HRM, mmHg | Post-ECK scores | Adverse events |
| Familiari et al[15], 2016 | LM: 23 SM: 26 | LM: 13 SM: 8 | LM: 59.2 ± 16.7 SM: 47.7 ± 13.2 | ES: LM: 8.42 ± 2.13 SM: 3.87 ± 0.61 ST: LM: 2.49 ± 0.70 SM: 2.21 ± 0.41 TO: LM: 10.94 ± 2.11 SM: 6.04 ± 0.69 | 8 | LM: 100% SM: 100% | LM: 42.9% SM: 65% | LM: 17 ± 9.7 SM: 11.4 ± 6.5 | LM: 8.6 ± 4.9 SM: 5.9 ± 5.0 | LM: 0.5 ± 0.8 SM: 0.5 ± 0.8 | No |
| Gao et al[16], 2017 | LM: 53 SM: 47 | LM: > 7 SM: ≤7 | LM: 63.13 ± 26.5 SM: 50.62 ± 20.02 | NA | 3,6,12 | LM: 96.2% SM: 93.6% | LM: 11.3% SM: 12.8% | LM: 16.51 ± 5.01 SM: 17.41 ± 3.69 | NA | LM: 0.98 ± 1.14 SM: 1.06 ± 1.42 | MB: LM: 0, SM: 0 MP: LM: 1; SM: 0 HS: LM: 10.19 ± 4.03 SM: 10.21 ± 3.78 |
| Gong et al[17], 2016 | LM: 59 SM: 38 | LM: > 7 SM: ≤7 | LM: 68.5 ± 23.2 SM: 44.2 ± 16.3 | ES: LM: 8.5 ± 2.6 SM: 4.0 ± 0.9 ST: LM: 3.2 ± 1.4 SM: 2.1+0.3 TO: LM: 11.7 ± 2.4 SM: 6.1 ± 0.5 | NA | LM: 91.5% SM: 92.1% | LM: 18.6% SM: 15.8% | LM: 19.3 ± 8.5 SM: 16.7 ± 4.3 | NA | LM: 1.2 ± 1.2 SM: 1.0 ± 0.9 | MB: LM: 3; SM: 2 MP: LM: 1; SM: 0 HS: LM: 6.6 ± 1.1 SM: 6.4 ± 1.2 |
| Gu et al[14], 2020 | LM: 48 SM: 46 | LM: 7-8 SM: 3-4 | LM: 45.6 ± 16.2 SM: 31.2 ± 15.3 | ES: LM: 10.14 ± 0.54 SM: 5.66 ± 0.14 | 1,3,6,12 | LM: 93.8% SM: 95.7% | LM: 22.9% SM: 15.2% | LM: 12.1 ± 3.9 SM: 11.8 ± 4.4 | LM: 9.7 ± 2.6 SM: 10.1 ± 2.4 | LM: 0.72 ± 0.42 SM: 0.76 ± 0.51 | HS: LM: 6: 5 ± 1.6 SM: 7.0 ± 0.9 |
| Huang et al[13], 2020 | LM: 74 SM: 36 | LM > 7 SM≤ 7 | LM: 62.1 ± 25.2 SM: 46.6 ± 18.5 | ES: LM: 8.2 ± 2.7 SM: 4.0 ± 0.7 ST: LM: 3.2 ± 1.2 SM: 3.2 ± 1.2 TO: LM: 11.5 ± 3.1 SM: 6.0 ± 0.6 | 28.7 | LM: 91.9% SM: 94.4% | LM: 14.9% SM: 8.3% | LM: 13.3 ± 5.7 SM: 15.9 ± 3.2 | NA | LM: 1.6 ± 1.3 SM: 1.3 ± 1.2 | MB: LM: 3; SM: 2 MP: LM: 1; SM: 0 HS: LM: 9.3 ± 2.9 SM: 9.9 ± 2.4 |
| Nabi et al[12], 2020 | LM: 37 SM: 34 | LM: ≥ 6 SM: ≤ 3 | LM: 72.43 ± 27.28 SM: 44.03 ± 13.78 | ES: LM: 7.97 ± 2.40 SM: 2.76 ± 0.41 ST: LM: 2.84 ± 0.63 SM: 2.70 ± 0.73 | 12 | LM: 96.97% SM: 93.55% | LM: 56.67%SM: 44.4% | NA | LM: 7.44 ± 4.30 SM: 8.60 ± 1.30 | LM: 0.818 ± 0.983 SM: 0.935 ± 0.929 | MB: LM: 17; SM: 12 HS: LM: 2.81 ± 0.70 SM: 2.82 ± 0.67 |
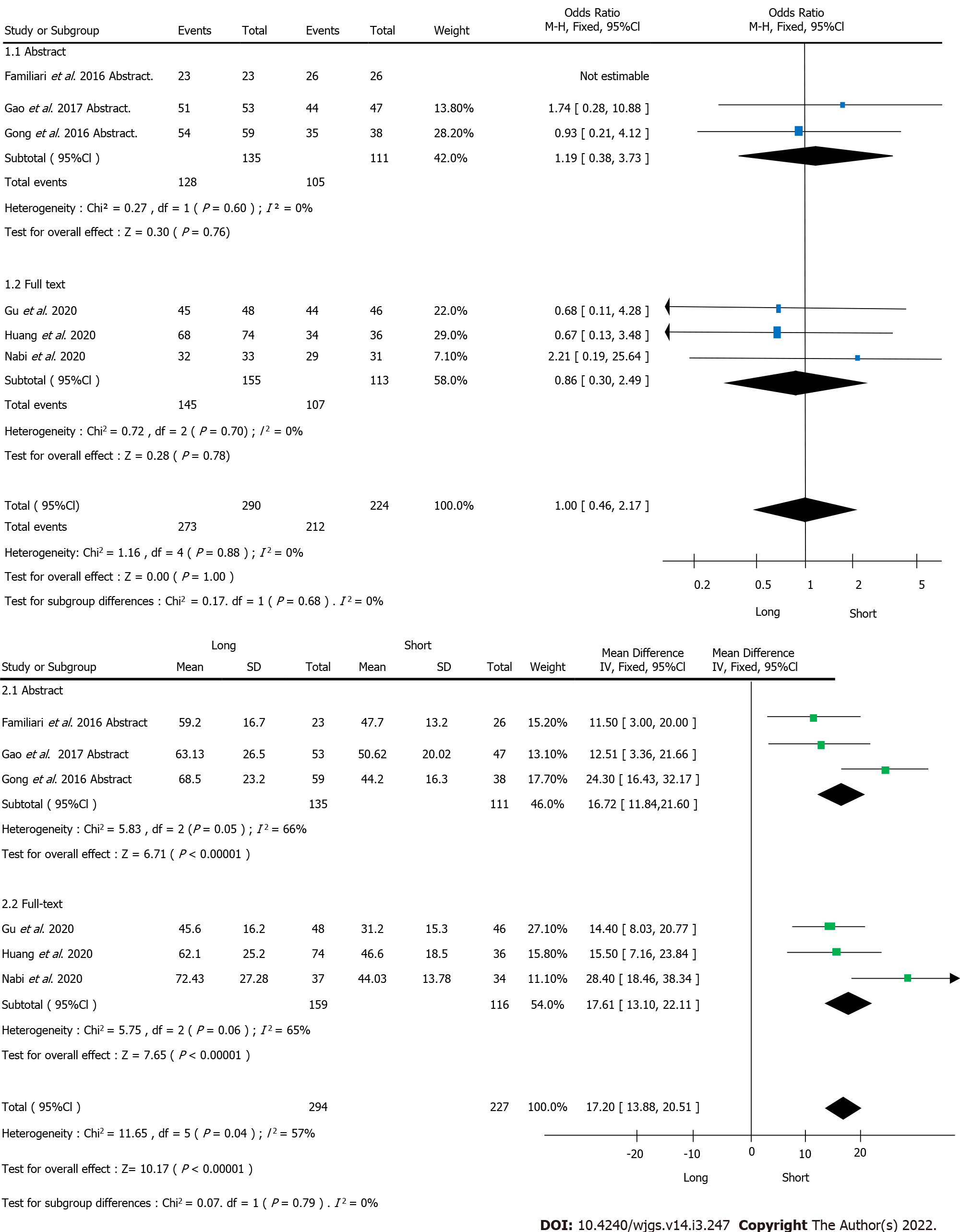
All patients were followed up for clinical success rate and Eckardt score. Data on clinical success after POEM were available in six studies (Figure 3) [overall clinical success (OR = 1, 95%CI: 0.46-2.17, P = 1, I2: 0%; subgroup of abstract (OR = 1.19, 95%CI: 0.38 to 3.73; P = 0.76; I2: 0%); subgroup of full text (OR = 0.86 95%CI: 0.30 to 2.49; P = 0.78; I2: 0%)]. Therefore, clinical success of POEM showed no statistically significant difference between the two groups.
Five studies presented pre-POEM Eckardt score as a quantitative variable. The score was 6.75 ± 1.86, 7.2 ± 2.4, 7.1 ± 1.6, 7.5 ± 1.9, 6.75 ± 1.32 in the LM group, respectively. In the SM group, the score was 6.34 ± 1.74, 6.8 ± 1.7, 7.5 ± 1.5, 7.1 ± 1.6 and 6.02 ± 1.33, respectively. Six studies provided postoperative Eckardt scores, which were also comparable between the LM and SM group. The postoperative Eckardt score in the LM group was 0.5 ± 0.8; 0.98 ± 1.14; 1.2 ± 1.2; 0.72 ± 0.42; 1.6 ± 1.3; 0.818 ± 0.983, respectively. Similarly, the score in the SM group was 0.5 ± 0.8; 1.06 ± 1.42; 1.0 ± 0.9; 0.76 ± 0.51; 1.3 ± 1.2 and 0.935 ± 0.929, respectively.
Operative time: Total procedure duration was available in all six articles including a total of 521 patients. The operative time in the LM group was 59.2 ± 16.7, 63.13 ± 26.50, 68.5 ± 23.2, 45.6 ± 16.2, 62.1 ± 25.2 and 72.43 ± 27.28, respectively. For the SM group, the time was 47.7 ± 13.2, 50.62 ± 20.02, 44.2 ± 16.3, 31.2 ± 15.3, 46.6 ± 18.5 and 44.03 ± 13.78, respectively. Obviously, the operative times in the SM group were shorter than that in the LM group (Figure 4).
Length of myotomy: A total of 3 RCTs and 2 retrospective studies involving 421 cases were meta-analyzed, with 180 cases in the SM group and 241 cases in the LM group. Myotomy length in POEM included the span of esophageal and gastric myotomy. The total length of myotomy in the LM group was 11.10 ± 2.0, 11.5 ± 3.1 and 11.7 ± 2.4 cm, respectively. Among them, the esophageal myotomy length was 8.42 ± 2.13, 8.2 ± 2.7, 10.14 ± 0.54, 7.97 ± 2.40 and 8.5 ± 2.6 cm, respectively, and the gastromyotomy length was 2.49 ± 0.70, 3.2 ± 1.4, 3.2 ± 1.2 and 2.84 ± 0.63 cm, respectively. The following myotomy values were obtained in the SM group of six studies: total length in three studies, 6.04 ± 0.69, 6.1 ± 0.5 and 6.0 ± 0.6 cm, respectively; esophageal length in five studies, 3.87 ± 0.61, 4.0 ± 0.9, 5.66 ± 0.14, 4.0 ± 0.7 and 2.76 ± 0.41 cm, respectively; and gastric length in four studies, 2.21 ± 0.41, 2.1 ± 0.3, 3.2 ± 1.2 and 2.70 ± 0.73 cm, respectively.
Manometry outcomes: Preoperative LES pressure in POEM was available in four articles with a total of 401 patients, and five articles including 450 individuals assessed postoperative LES pressure. The level of preoperative LES pressure in the LM group was 43.03 ± 13.73, 42.1 ± 12.9, 32.4 ± 5.3 and 39.8 ± 13.7 mmHg respectively, and the value was 41.93 ± 14.93, 44.6 ± 13.2, 33.5 ± 5.0 and 41.8 ± 14.3 mmHg, respectively, in the SM group. Postoperative LES pressure level in the LM group was 17 ± 9.7, 16.51 ± 5.01, 19.3 ± 8.5, 12.1 ± 3.9 and 13.3 ± 5.7 mmHg, respectively, and the pressure level was 11.4 ± 6.5, 17.41 ± 3.69, 16.7 ± 4.3, 11.8 ± 4.4 and 15.9 ± 3.2 mmHg, respectively, in the SM group.
Integrated relaxation pressure: Preoperative integrated relaxation pressure (IRP) in POEM was available in two articles with a total of 165 patients, and three articles including 214 individuals assessed postoperative IRP pressure. The levels of preoperative IRP in the LM group were 21.5 ± 4.6 mmHg and 28.50 ± 11.01 mmHg, and in the SM group, the values were 23.2 ± 4.8 mmHg and 26.40 ± 13.9 mmHg. Postoperative IRP level in the LM group was 8.6 ± 4.9, 9.7 ± 2.6, and 7.44 ± 4.30 mmHg, respectively, and this pressure level was 5.9 ± 5.0, 10.1 ± 2.4 and 8.60 ± 1.30 mmHg, respectively, in the SM group.
Endoscopic reflux esophagitis: This meta-analysis found no difference in endoscopic reflux esophagitis between the two procedures (total OR = 1.21, 95%CI: 0.76-1.91; P = 0.42; I2: 9%; subgroup of abstract OR = 0.77, 95%CI: 0.40-1.47; P = 0.43; I2: 0%; subgroup of full text OR = 1.91, 95%CI: 0.98-3.75; P = 0.06; I2: 0%), with low heterogeneity found. Hence, random- and fixed-effects models yielded identical results (Figure 5A).
AEs: The incidence rates of AEs in different studies are detailed in Table 2. No procedure-related deaths were recorded. The rate of hospitalization showed no difference between the two procedures (total MD = -0.07, 95%CI: -0.30 to 0.16; P = 0.55;
In this meta-analysis, we critically assessed the available RCTs and retrospective studies comparing SM and LM during POEM for the treatment of achalasia. Our main findings were that both approaches were equally effective yet the shorter procedure required reduced operation time. Heterogeneity across the studies was low and a comprehensive sensitivity analysis was consistent with our primary findings. No publication bias was detected.
The notion of endoscopic myotomy was first put forward by Ortega and collaborators[19], with an electrosurgical knife utilized for dissecting the lower esophageal rosette without manipulating the distal anti-reflux zone. Nevertheless, direct endoscopic myotomy has serious complications, and it has been abandoned. POEM was first reported by Pasricha and collaborators[20] in 2007 with pigs and utilized a submucosal tunnel for LES myotomy. In 2010, Inoue and collaborators[3] first applied POEM clinically using seven individuals who received a relatively shorter myotomy (mean length of 4.9 cm and 1.0 cm on the gastric side) but had worse clinical outcomes compared with the 10 cases undergoing a longer myotomy (mean length of 10.4 cm). With regard to myotomy length in POEM, Inoue and colleagues recommended to use a length of > 10 cm (average 13 cm) as the standard[21]. Since then, POEM has been considered as an emerging treatment modality and is the preferred therapeutic option for achalasia and has shown success in all age groups and different types and stages of achalasia[22]. In addition, POEM is promising in the treatment for spastic esophageal motility ailments. Avoiding abdominal incisions could reduce surgical invasiveness, improve cosmetic effects and shorten convalescence time[23]. Moreover, POEM has been widely used clinically due to its advantages over LHM[24] including no abdominal cut, faster recovery and the possibility of avoiding general anesthesia. In addition, unlike LHM, POEM does not involve GEJ dissection[25].
The major differences in the implementation of POEM worldwide include myotomy orientation (anterior or posterior), thickness (full or partial) and length (shorter and longer). With regard to myotomy length in POEM surgery, Von Renteln and colleagues (Germany), Costamagna and collaborators (Italy), Chiu and co-workers (Hong Kong, China) and Minami and colleagues (Japan), all performed LM to treat achalasia with a mean incision length of 12, 10, 10.8 or 14.4 cm, and promising efficacy and safety have been achieved[26-29]. However, these trials adopted the original LM POEM technique by Inoue et al[21], with a myotomy length of about 10 cm. Meanwhile, the average LES length was only 3.2 cm, ranging from 2.4 to 4.0 cm in healthy and achalasia individuals[30]. According to the guidelines of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), for cases of achalasia, esophageal myotomy length should be ≥ 4 cm and the gastromyotomy length should be 1-2 cm[31]. Therefore, it was hypothesized that a modified POEM procedure with a LM might be as effective as the LM procedure in achalasia treatment as it ensured sufficient LES cutting while ameliorating complications and decreasing operation time. To test this hypothesis, Wang et al[10] enrolled 46 patients who underwent modified POEM with shorter submucosal tunnel (average length 6.8 cm) and endoscopic myotomy of muscle bundles (total average length 5.4 cm). They reported that modified POEM with LM showed great safety and commendable short-term efficacy in treating achalasia. However, for patients with type I and II achalasia, a short esophageal myotomy may be sufficient[10].
The present analysis, which was based on RCTs and a retrospective study, confirmed that POEM offered excellent efficacy with a high clinical success rate. The treatment efficacy was similar between the SM and LM procedures, regardless of the definition used, length of myotomy, publication type and the statistical method employed to pool the data. The meta-analysis of manometric outcomes, where no significant disparities were detected, further endorsed the lack of clinical differences between LM and SM.
Another matter of debate is GERD after POEM[32]. Several technical refinements have been attempted to decrease the odds of post-POEM GERD, including a selective myotomy of the inner circular muscle[33], endoscopic fundoplication[34], or limiting the length of gastromyotomy[35]. The proper location of the gastroesophageal junction (GEJ) is critical in ensuring the procedure’s effectiveness and may have an impact on GERD[36,37]. Many reports showed a lower GERD incidence after POEM due to the preservation of the pharyngoesophageal ligament[38,39]. In the present meta-analysis, the incidence rate of GERD was similar between the SM and LM procedures.
Regarding POEM-related AEs, multicenter studies showed that the technique was associated with a low incidence of severe AEs (< 1%)[40,41]. Interestingly, we found that the total incidence rate of AEs, including hospitalization and major bleeding, were comparable between the two groups. Procedure-related outcomes were also evaluated. As expected from our clinical experience, the SM took much less time compared with the LM but the treatment effects were similar.
This meta-analysis had some limitations. First, the number of studies was very small and three RCTs were only retrieved as abstracts. Although we conducted subgroup analysis based on abstract and full-text, more studies were still needed to analyze the results. Second, only three articles evaluated IRP after POEM treatment. Third, a longer myotomy is thought to be more effective on controlling symptoms caused by the esophageal spasm of type III achalasia. However, in this meta-analysis, due to the small number of patients with type III achalasia and recent literature[18], our conclusions might not apply to type III achalasia treatment and a short myotomy could not be recommended. We expected more RCTs to examine the effect of shorter or longer in the treatment of type III achalasia. Due to the lack of relevant research articles, we did not evaluate the postoperative efficacy of POEM for achalasia subtypes. Fourth, the follow-up duration was relatively short so this study was unable to compare the long-term efficacy and AES between LM and SM procedures.
In conclusion, short myotomy has the advantage of reduced procedure time in the treatment of achalasia compared to long myotomy, but the clinical success rate, AEs, and reflux rate were comparable. Thus, peroral endoscopic shorter myotomy could have a great clinical application prospect. Our results are restricted by the small number of patients, short follow-up duration, and a lack of specific definition of short myotomy. Future studies with a larger sample size and longer follow-up duration are warranted to evaluate the long-term efficacy and safety of these two procedures in POEM.
For a long time, peroral endoscopic myotomy (POEM) has been demonstrated to be safe and effective in the treatment of achalasia.
Longer myotomy is the standard POEM procedure for achalasia, but its effectiveness compared with shorter myotomy is not well known. Thus, we want to provide an analysis to assess the clinical outcomes of shorter and longer myotomy.
To conduct a meta-analysis to compare the clinical effectiveness of the two procedures.
The PubMed, Web of Science, Cochrane Library, clinicaltrials.gov, and EMBASE databases were used to search for relevant studies to compare shorter and longer myotomy in POEM for achalasia treatment.
Longer and shorter myotomy groups in treating achalasia had similar excellent effectiveness. Shorter myotomy had significantly reduced mean operative time compared with the longer procedure. There were no statistically significant differences in AE’s rates, including gastroesophageal reflux diseases, hospital stay and major bleeding between the two procedures.
Short myotomy has the advantage of shorter procedure time in the treatment of achalasia compared to long myotomy, but the clinical success rate, adverse events , and reflux rate were comparable.
Future randomized clinical trials should determine whether the benefits remain comparable after years of follow-up.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Beraldo RF, Cabezuelo AS, Oda M S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wu RR
| 1. | Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 428] [Article Influence: 38.9] [Reference Citation Analysis (0)] |
| 2. | Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2020;115:1393-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 235] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 3. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1232] [Article Influence: 82.1] [Reference Citation Analysis (1)] |
| 4. | Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE. Per-Oral Endoscopic Myotomy: A Series of 500 Patients. J Am Coll Surg. 2015;221:256-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 346] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 5. | Nabi Z, Ramchandani M, Chavan R, Kalapala R, Darisetty S, Rao GV, Reddy N. Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open. 2017;5:E331-E339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Youn YH, Minami H, Chiu PW, Park H. Peroral Endoscopic Myotomy for Treating Achalasia and Esophageal Motility Disorders. J Neurogastroenterol Motil. 2016;22:14-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | He C, Li M, Lu B, Ying X, Gao C, Wang S, Ma C, Jin C. Long-Term Efficacy of Peroral Endoscopic Myotomy for Patients with Achalasia: Outcomes with a Median Follow-Up of 36 mo. Dig Dis Sci. 2019;64:803-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Inoue H, Shiwaku H, Kobayashi Y, Chiu PWY, Hawes RH, Neuhaus H, Costamagna G, Stavropoulos SN, Fukami N, Seewald S, Onimaru M, Minami H, Tanaka S, Shimamura Y, Santi EG, Grimes K, Tajiri H. Statement for gastroesophageal reflux disease after peroral endoscopic myotomy from an international multicenter experience. Esophagus. 2020;17:3-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 9. | Grimes KL, Bechara R, Shimamura Y, Ikeda H, Inoue H. Gastric myotomy length affects severity but not rate of post-procedure reflux: 3-year follow-up of a prospective randomized controlled trial of double-scope per-oral endoscopic myotomy (POEM) for esophageal achalasia. Surg Endosc. 2020;34:2963-2968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 10. | Wang J, Tan N, Xiao Y, Chen J, Chen B, Ma Z, Zhang D, Chen M, Cui Y. Safety and efficacy of the modified peroral endoscopic myotomy with shorter myotomy for achalasia patients: a prospective study. Dis Esophagus. 2015;28:720-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Cochrane Handbook for Systematic Reviews of Interventions [Internet]. [cited 20 July 2021]. Available from: https://training.cochrane.org/handbook. |
| 12. | Nabi Z, Ramchandani M, Sayyed M, Chavan R, Darisetty S, Goud R, Murthy HVV, Reddy DN. Comparison of Short Versus Long Esophageal Myotomy in Cases With Idiopathic Achalasia: A Randomized Controlled Trial. J Neurogastroenterol Motil. 2021;27:63-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 13. | Huang S, Ren Y, Peng W, Gao Q, Peng Y, Gong W, Tang X. Peroral endoscopic shorter versus longer myotomy for the treatment of achalasia: a comparative retrospective study. Esophagus. 2020;17:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 14. | Gu L, Ouyang Z, Lv L, Liang C, Zhu H, Liu D. Safety and efficacy of peroral endoscopic myotomy with standard myotomy versus short myotomy for treatment-naïve patients with type II achalasia: a prospective randomized trial. Gastrointest Endosc. 2021;93:1304-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 15. | Familiari Pietro, Anna Calì, Rosario Landi, Giovanni Gigante, Ivo Boskoski, Federico Barbaro, Andrea Tringali, Santiago Andrade Zurita, Vincenzo Perri, Guido Costamagna. Long vs Short POEM for the Treatment of Achalasia. Interim Analysis of a Randomized Controlled Trial. Gastrointestinal Endoscopy. 2016;83. |
| 16. | Gao QP, Tu SF, Tang XW, Huang SL, Gong W. Mid-term Outcomes of a Single Center Randomized Controlled Trial Comparing Peroral Endoscopic Short versus Long Myotomy for Achalasia in China. The American Journal of Gastroenterology. . |
| 17. | Gong W, Tang XW, Huang SL, Ren YT, Gao QP, Zhou JQ, Zhang XF, Bo Jiang. Peroral Endoscopic Shorter versus Longer Myotomy for the Treatment of Achalasia: A Comparative Study. The American Journal of Gastroenterology. . |
| 18. | Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, Shiwaku H, Kunda R, Chiu P, Saxena P, Messallam AA, Inoue H, Khashab MA. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endosc Int Open. 2015;3:E195-E201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 173] [Cited by in RCA: 189] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 19. | Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 101] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 20. | Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, Kalloo AN, Kantsevoy SV, Gostout CJ. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 360] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 21. | Inoue H, Santi EG, Onimaru M, Kudo SE. Submucosal endoscopy: from ESD to POEM and beyond. Gastrointest Endosc Clin N Am. 2014;24:257-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | NOSCAR POEM White Paper Committee. , Stavropoulos SN, Desilets DJ, Fuchs KH, Gostout CJ, Haber G, Inoue H, Kochman ML, Modayil R, Savides T, Scott DJ, Swanstrom LL, Vassiliou MC. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 23. | Cho YK, Kim SH. Current Status of Peroral Endoscopic Myotomy. Clin Endosc. 2018;51:13-18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Ponds FA, Fockens P, Lei A, Neuhaus H, Beyna T, Kandler J, Frieling T, Chiu PWY, Wu JCY, Wong VWY, Costamagna G, Familiari P, Kahrilas PJ, Pandolfino JE, Smout AJPM, Bredenoord AJ. Effect of Peroral Endoscopic Myotomy vs Pneumatic Dilation on Symptom Severity and Treatment Outcomes Among Treatment-Naive Patients With Achalasia: A Randomized Clinical Trial. JAMA. 2019;322:134-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 256] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 25. | Kahrilas PJ, Katzka D, Richter JE. Clinical Practice Update: The Use of Per-Oral Endoscopic Myotomy in Achalasia: Expert Review and Best Practice Advice From the AGA Institute. Gastroenterology. 2017;153:1205-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 26. | von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, Fuchs KH, Rösch T. Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol. 2012;107:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 27. | Costamagna G, Marchese M, Familiari P, Tringali A, Inoue H, Perri V. Peroral endoscopic myotomy (POEM) for oesophageal achalasia: preliminary results in humans. Dig Liver Dis. 2012;44:827-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 28. | Chiu PW, Wu JC, Teoh AY, Chan Y, Wong SK, Liu SY, Yung MY, Lam CC, Sung JJ, Chan FK, Lau JY, Ng EK. Peroral endoscopic myotomy for treatment of achalasia: from bench to bedside (with video). Gastrointest Endosc. 2013;77:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 88] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 29. | Minami H, Isomoto H, Yamaguchi N, Matsushima K, Akazawa Y, Ohnita K, Takeshima F, Inoue H, Nakao K. Peroral endoscopic myotomy for esophageal achalasia: clinical impact of 28 cases. Dig Endosc. 2014;26:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 30. | Shi Y, Xiao Y, Peng S, Lin J, Xiong L, Chen M. Normative data of high-resolution impedance manometry in the Chinese population. J Gastroenterol Hepatol. 2013;28:1611-1615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 31. | Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD; Society of American Gastrointestinal and Endoscopic Surgeons. SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc. 2012;26:296-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 138] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 32. | Rösch T, Repici A, Boeckxstaens G. Will Reflux Kill POEM? Endoscopy. 2017;49:625-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Wang XH, Tan YY, Zhu HY, Li CJ, Liu DL. Full-thickness myotomy is associated with higher rate of postoperative gastroesophageal reflux disease. World J Gastroenterol. 2016;22:9419-9426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 64] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 34. | Tyberg A, Choi A, Gaidhane M, Kahaleh M. Transoral incisional fundoplication for reflux after peroral endoscopic myotomy: a crucial addition to our arsenal. Endosc Int Open. 2018;6:E549-E552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 35. | Inoue H, Shiwaku H, Iwakiri K, Onimaru M, Kobayashi Y, Minami H, Sato H, Kitano S, Iwakiri R, Omura N, Murakami K, Fukami N, Fujimoto K, Tajiri H. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30:563-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 126] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 36. | Teitelbaum EN, Sternbach JM, El Khoury R, Soper NJ, Pandolfino JE, Kahrilas PJ, Lin Z, Hungness ES. The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc. 2016;30:745-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 37. | Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodème F, Lin Z, Hungness ES. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 2015;29:522-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 38. | Awaiz A, Yunus RM, Khan S, Memon B, Memon MA. Systematic Review and Meta-Analysis of Perioperative Outcomes of Peroral Endoscopic Myotomy (POEM) and Laparoscopic Heller Myotomy (LHM) for Achalasia. Surg Laparosc Endosc Percutan Tech. 2017;27:123-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 39. | Schneider AM, Louie BE, Warren HF, Farivar AS, Schembre DB, Aye RW. A Matched Comparison of Per Oral Endoscopic Myotomy to Laparoscopic Heller Myotomy in the Treatment of Achalasia. J Gastrointest Surg. 2016;20:1789-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 40. | Haito-Chavez Y, Inoue H, Beard KW, Draganov PV, Ujiki M, Rahden BHA, Desai PN, Pioche M, Hayee B, Haji A, Saxena P, Reavis K, Onimaru M, Balassone V, Nakamura J, Hata Y, Yang D, Pannu D, Abbas A, Perbtani YB, Patel LY, Filser J, Roman S, Rivory J, Mion F, Ponchon T, Perretta S, Wong V, Maselli R, Ngamruengphong S, Chen YI, Bukhari M, Hajiyeva G, Ismail A, Pieratti R, Kumbhari V, Galdos-Cardenas G, Repici A, Khashab MA. Comprehensive Analysis of Adverse Events Associated With Per Oral Endoscopic Myotomy in 1826 Patients: An International Multicenter Study. Am J Gastroenterol. 2017;112:1267-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 146] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 41. | Werner YB, von Renteln D, Noder T, Schachschal G, Denzer UW, Groth S, Nast JF, Kersten JF, Petzoldt M, Adam G, Mann O, Repici A, Hassan C, Rösch T. Early adverse events of per-oral endoscopic myotomy. Gastrointest Endosc. 2017;85:708-718.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 60] [Article Influence: 7.5] [Reference Citation Analysis (0)] |