Published online Mar 27, 2022. doi: 10.4240/wjgs.v14.i3.236
Peer-review started: November 1, 2021
First decision: December 4, 2021
Revised: December 12, 2021
Accepted: March 6, 2022
Article in press: March 6, 2022
Published online: March 27, 2022
Processing time: 144 Days and 2.6 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is the primary treatment for removing common bile duct (CBD) stones. The risk factors for CBD stone recurrence after ERCP have been discussed for many years. However, the influence of CBD morphology has never been noticed.
To evaluate CBD morphology and other predictors affecting CBD stone recurrence in average patients.
A retrospective analysis of 502 CBD stone patients who underwent successful therapeutic ERCP for stone extraction at our centre from February 2020 to January 2021 was conducted. CBD morphology and other predictors affecting CBD stone recurrence were examined by univariate analysis and multivariate logistic regression analysis.
CBD morphology (P < 0.01), CBD diameter ≥ 1.5 cm [odds ratio (OR) = 2.20, 95%CI: 1.08-4.46, P = 0.03], and endoscopic biliary sphincterotomy with balloon dilation (ESBD) (OR = 0.35, 95%CI: 0.17-0.75, P < 0.01) are three independent risk factors for CBD stone recurrence. Furthermore, the recurrence rate of patients with the S type was 6.61-fold that of patients with the straight type (OR = 6.61, 95%CI: 2.61-16.77, P < 0.01). The recurrence rate of patients with the polyline type was 2.45-fold that of patients with the straight type (OR = 2.45, 95%CI: 1.14-5.26, P = 0.02). The recurrence rate of S type patients was 2.70-fold that of patients with the polyline type (OR = 2.70, 95%CI: 1.08-6.73, P = 0.03). Compared with no-ESBD, ESBD could decrease the risk of recurrence.
CBD diameter ≥ 1.5 cm and CBD morphology, especially S type and polyline type, were associated with increased recurrence of CBD stones. In addition, ESBD was related to decreased recurrence. Patients with these risk factors should undergo periodic surveillance and standard prophylactic therapy.
Core Tip: Endoscopic retrograde cholangiopancreatography (ERCP) is the primary treatment for removing common bile duct (CBD) stones. The risk factors for CBD stone recurrence after ERCP have been discussed for many years. However, the influence of CBD morphology has never been reported. We demonstrate that CBD morphology was an independent risk factor for CBD stone recurrence in patients. Furthermore, the S type and polyline type were associated with an increased risk of recurrent CBD stones. This information represents a new perspective by defining the shape of the common bile duct on cholangiograms, which could redefine the risk factors and models of recurrence and predict periodic follow-up.
- Citation: Ji X, Yang Z, Ma SR, Jia W, Zhao Q, Xu L, Kan Y, Cao Y, Wang Y, Fan BJ. New common bile duct morphological subtypes: Risk predictors of common bile duct stone recurrence. World J Gastrointest Surg 2022; 14(3): 236-246
- URL: https://www.wjgnet.com/1948-9366/full/v14/i3/236.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i3.236
As a minimally invasive endoscopic procedure, endoscopic retrograde cholangiopancreatography (ERCP) is widely performed to treat common bile duct (CBD) stones. However, challenging problems, such as patients with gastrectomy who require multiple procedures and post ERCP complications, are typically encountered[1]. Choledocholithiasis recurrence is a long-term complication[2-5], and the recurrence rate after therapeutic ERCP was 2%-22% in the literature[6-9]. My previous studies reported that CBD morphology in Billroth II anatomy patients is an independent risk factor for CBD stone recurrence[10]. Therefore, we also aim to investigate CBD morphology in average patients with or without gastrectomy and clarify the association between CBD morphology and stone recurrence.
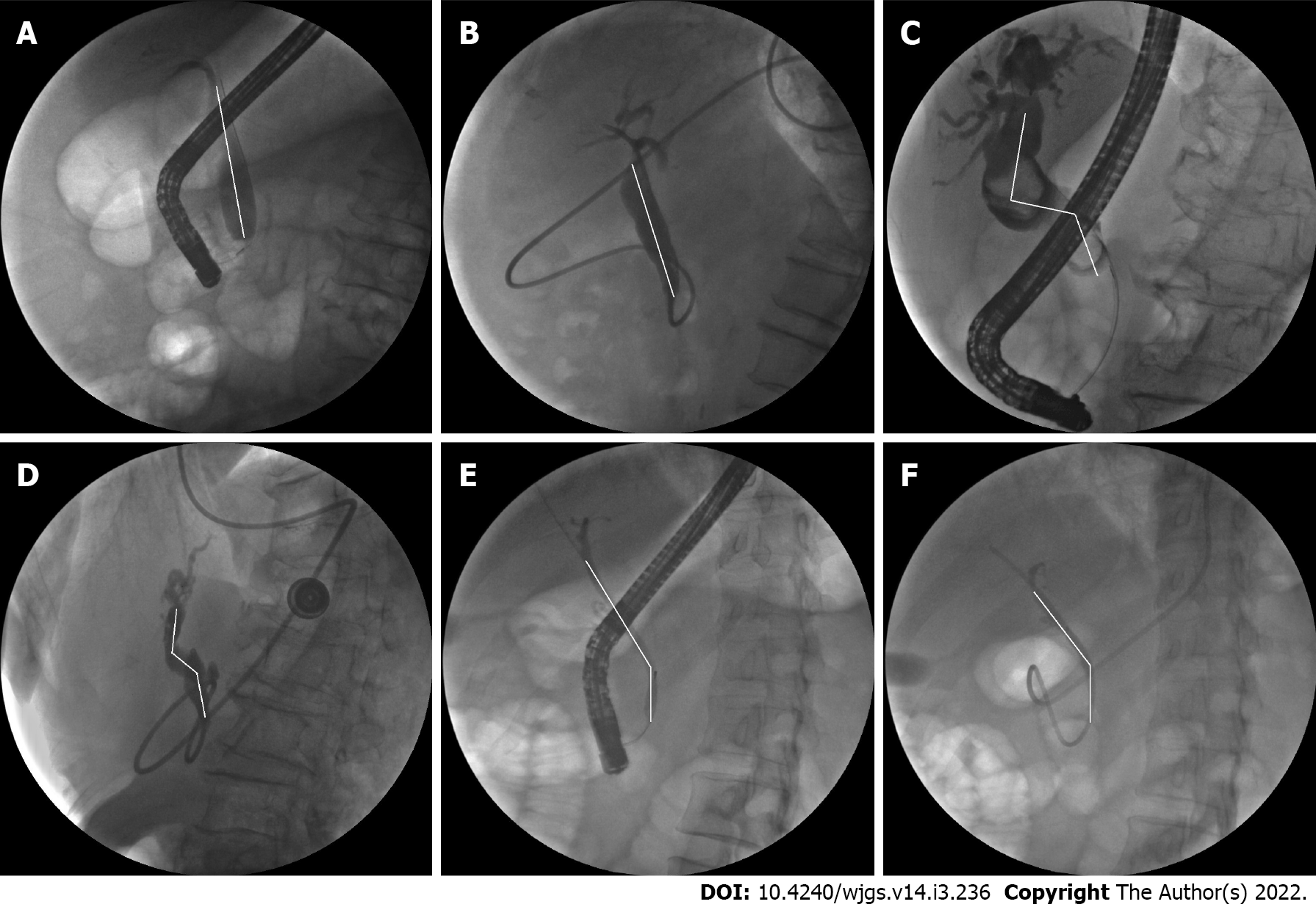
To date, there are a wide range of risk factors for recurrent CBD stones, and the most common predictors are operative related factors, such as age[11], periampullary diverticulum (PAD)[12,13], CBD diameter[14,15], CBD stone diameter[11,16], multiple CBD stones[12,17], endoscopic biliary sphincterotomy (EST)[11,16,18], endoscopic papillary balloon dilation (EPBD)[11], endoscopic papillary large balloon dilation (EPLBD)[19,20], EST with balloon dilation (ESBD)[15,21,22], cholecystectomy[23], gastrectomy[24,25], and CBD angulation[26-28]. However, there have been no reports concerning CBD morphology before my previous study. This is also the first study to report the best evidence regarding CBD morphology in average patients. In the present study, CBD morphology was defined as cholangiogram morphology from the confluence of the left and right hepatic ducts to the distal CBD entering the duodenum, including straight type, S type, and polyline type (Figure 1)[10].
From February 2020 to January 2021, 790 patients underwent ERCP at the General Hospital of Northern Theater Command, and 502 patients were included in this study. The exclusion criteria were as follows: (1) patients with tumours of the duodenal papilla, CBD, liver, or gallbladder; (2) patients without specific stones during ERCP; (3) patients who had not removed their stones completely after the first ERCP; and (4) patients with incomplete data. Stone recurrence was defined as the presence of CBD stones at least 6 mo after previous CBD stones were completely removed by ERCP. At least two stone recurrences were defined as multiple recurrences after the first ERCP[27]. Patients with CBD stones who visited our hospital were confirmed by abdominal computed tomography and ERCP.
All endoscopists performed the ERCP procedures with at least 500 cases of experience. In our institution, prophylactic antibiotics are used in patients without evidence of cholangitis before ERCP. Firstly, the patient was sedated in the left lateral decubitus position. Endoscopists used a side-viewing duodenoscope or a forward-viewing gastroscope (Olympus Medical, Tokyo, Japan) entering the stomach. The first step was to perform the wire-guided biliary cannulation. Precut sphincterotomy or the double-wire technique can be prepared after biliary cannulation failed. As selective biliary cannulation was achieved, depending on CBD stones, the operator executed the therapeutic intervention, which included EST, ESBD, EPBD, and EPLBD. After the therapeutic intervention, the operator chose to remove stones with a retrieval balloon and/or a retrieval basket with or without mechanical lithotripsy. After CBD stone removal, an endoscopic nasobiliary drainage (ENBD) tube was placed in all patients to determine the complete clearance of CBD stones. After 3-5 d of observation, endoscopists confirmed that no residual stones were present and identified the CBD morphology again by cholangiography.
Assessed factors, such as the CBD morphology, the largest stone, and the diameter of the CBD, were measured with the patient placed in the left lateral decubitus position during the operation. Furthermore, cholangiography was performed to determine the CBD morphology and the clearance of CBD stones through an ENBD tube before the tube was removed. CBD morphology was identified by at least two experienced endoscopists with operative and postoperative cholangiograms. The definition of CBD morphology was cholangiogram morphology from the confluence of the left and right hepatic ducts to the distal CBD entering the duodenum. We classified the CBD morphology as follows: straight type, the CBD was straight without bending; S type, the CBD was S-shaped with two bends; and polyline type, the CBD had one bend.
Statistical analyses were performed with SPSS 26.0. Univariate analysis was performed using Student’s t test, Fisher’s exact test and χ2 test. Independent risk factors were analyzed by multivariate logistic regression analysis with a backwards likelihood ratio. A value of P < 0.05 was considered statistically significant.
A total of 502 patients with CBD stones were retrospectively identified from the collected database. The average follow-up was 19 mo. Among the 502 patients, recurrence was detected in 43 patients, and multiple recurrences were detected in 9 patients. The rates of recurrence and multiple recurrences were 8.6% (43/502) and 1.8% (9/502), respectively. No statistically significant differences in patient characteristics, such as sex, PAD, CBD diameter, largest CBD stone diameter ≥ 1.5 cm, CBD stone number ≥ 2, muddy stones, initial ampullary intervention (EST), cholecystectomy, and procedure time, were observed between the recurrence group and nonrecurrence groups (Table 1 and Table 2).
| Characteristics | n (%) |
| Patients | 502 |
| Recurrence | 43 (8.6) |
| Multiple recurrences | 9 (1.8) |
| Male | 287 (57.2) |
| Age (mean ± SD, yr) | 65.2 ± 15.6 |
| Age 70 yr | 201 (40.0) |
| PAD | 243 (48.4) |
| CBD diameter (mean ± SD, cm) | 1.3 ± 0.7 |
| CBD diameter 1.5 cm | 160 (31.9) |
| Largest CBD stone diameter 1.5 cm | 83 (16.3) |
| CBD stone number 2 | 189 (37.6) |
| Muddy stones | 131 (26.1) |
| Initial ampullary intervention | |
| EST | 141 (28.1) |
| EPBD/EPLBD | 31 (6.2) |
| ESBD | 315 (62.7) |
| CBD morphology | |
| Straight type | 289 (57.6) |
| S type | 45 (9.0) |
| Polyline type | 168 (33.5) |
| Cholecystectomy | 26 (5.2) |
| Gastrectomy | 9 (1.8) |
| Procedure time (mean ± SD, min) | 20.0 ± 13.7 |
| Characteristics | Recurrence (n = 43) | Nonrecurrence (n = 459) | P value |
| Sex (male/female) | 23/20 | 264/195 | 0.61 |
| Age ≥ 70 yr | 25 (58.1) | 176 (38.3) | 0.01 |
| PAD | 23 (53.5) | 220 (47.9) | 0.49 |
| CBD diameter (mean ± SD, cm) | 1.5 ± 0.5 | 1.3 ± 0.7 | 0.06 |
| CBD diameter ≥ 1.5 cm | 23 (53.5) | 137 (29.8) | < 0.01 |
| Largest CBD stone diameter ≥ 1.5 cm | 11 (25.6) | 71 (15.5) | 0.09 |
| CBD stone number ≥ 2 | 15 (34.9) | 174 (37.9) | 0.70 |
| Muddy stones | 12 (27.9) | 119 (25.9) | 0.78 |
| Initial ampullary intervention | |||
| EST | 13 (30.2) | 128 (27.9) | 0.74 |
| EPBD/EPLBD | 9 (20.9) | 22 (4.8) | < 0.01 |
| ESBD | 17 (39.5) | 298 (64.9) | < 0.01 |
| CBD morphology | < 0.01 | ||
| Straight type | 14 (32.6) | 275 (59.9) | |
| S type | 11 (25.6) | 34 (7.4) | |
| Polyline type | 18 (41.9) | 150 (32.7) | |
| Cholecystectomy | 5 (11.6) | 21 (4.6) | 0.06 |
| Procedure time (mean ± SD, min) | 19.3 ± 14.2 | 20.1 ± 13.6 | 0.71 |
| Gastrectomy | 3 (7.0) | 6 (1.3) | 0.03 |
As shown in Table 3, the presence of a CBD diameter ≥ 1.5 cm (P = 0.01) differed significantly among different CBD morphologies and was detected in 96 (33.2%), 22 (48.9%), and 42 (25.0%) patients with straight type, S type, and polyline type, respectively. The proportion of patients with a CBD diameter ≥ 1.5 cm in the straight type group was the highest of all the groups. Other factors showed no significant difference.
| Characteristics | Straight type (n = 289) | S type (n = 45) | Polyline type (n = 168) | P value |
| Sex (male/female) | 166/123 | 30/15 | 91/77 | 0.32 |
| Age ≥ 70 yr | 104 (36.0) | 20 (44.4) | 77 (45.8) | 0.10 |
| PAD | 136 (47.1) | 20 (44.4) | 87 (51.8) | 0.53 |
| CBD diameter (mean ± SD, cm) | 1.3 ± 0.4 | 1.5 ± 0.5 | 1.4 ± 0.9 | 0.14 |
| CBD diameter ≥ 1.5 cm | 96 (33.2) | 22 (48.9) | 42 (25.0) | 0.01 |
| Largest CBD stone diameter ≥ 1.5 cm | 42 (14.5) | 8 (17.8) | 32 (19.0) | 0.44 |
| CBD stone number ≥ 2 | 105 (36.3) | 17 (37.8) | 67 (39.9) | 0.75 |
| Muddy stones | 78 (27.0) | 11 (24.4) | 42 (25.0) | 0.87 |
| Initial ampullary intervention | ||||
| EST | 84 (29.1) | 11 (24.4) | 46 (27.4) | 0.79 |
| EPBD/EPLBD | 18 (6.2) | 3 (6.7) | 10 (6.0) | 0.98 |
| ESBD | 180 (62.3) | 30 (66.7) | 105 (62.5) | 0.85 |
| Cholecystectomy | 19 (6.6) | 2 (4.4) | 5 (3.0) | 0.24 |
| Procedure time (mean ± SD, min) | 19.8 ± 11.7 | 19.7 ± 13.1 | 20.6 ± 16.7 | 0.81 |
| Gastrectomy | 5 (1.7) | 0 (0.0) | 4 (2.4) | 0.38 |
Characteristics of patients with single recurrence and multiple recurrences are shown in Table 4. All factors were not related to multiple recurrences given that significant differences were noted (P > 0.05). The results regarding PAD (P = 0.06) and ESBD (P = 0.07) were probably limited by the small sample size.
| Characteristics | Single recurrence (n = 34) | Multiple recurrences (n = 9) | P value |
| Sex (male/female) | 19/15 | 4/5 | 0.71 |
| Age (mean ± SD, yr) | 71.3 ± 13.7 | 68.6 ± 12.2 | 0.59 |
| Age ≥ 70 yr | 21 (61.8) | 4 (44.4) | 0.46 |
| PAD | 21 (61.8) | 2 (22.2) | 0.06 |
| CBD diameter (mean ± SD, cm) | 1.5 ± 0.5 | 1.6 ± 0.6 | 0.43 |
| CBD diameter ≥ 1.5 cm | 18 (52.9) | 5 (55.6) | 1.00 |
| Largest CBD stone diameter ≥ 1.5 cm | 10 (29.4) | 1 (11.1) | 0.41 |
| CBD stone number ≥ 2 | 12 (35.3) | 3 (33.3) | 1.00 |
| Muddy stones | 10 (29.4) | 2 (22.2) | 1.00 |
| Initial ampullary intervention | |||
| EST | 10 (29.4) | 3 (33.3) | 1.00 |
| EPBD/EPLBD | 6 (17.6) | 3 (33.3) | 0.37 |
| ESBD | 16 (47.1) | 1 (11.1) | 0.07 |
| CBD morphology | 0.22 | ||
| straight type | 12 (35.3) | 2 (22.2) | |
| S type | 10 (29.4) | 1 (11.1) | |
| polyline type | 12 (35.3) | 6 (66.7) | |
| Cholecystectomy | 5 (14.7) | 0 (0.0) | 0.57 |
| Gastrectomy | 3 (8.8) | 0 (0.0) | 1.00 |
| Procedure time (mean ± SD, min) | 19.9 ± 15.7 | 17.0 ± 6.3 | 0.60 |
In univariate analysis, age ≥ 70 years (P = 0.01), CBD diameter ≥ 1.5 cm (P < 0.01), EPBD/EPLBD (P < 0.01), ESBD (P < 0.01), gastrectomy (P = 0.03), and CBD morphology (P < 0.01) were significant factors for CBD stone recurrence.
Multicollinearity analysis showed all the results were VIF < 5, which represented no relationship among age ≥ 70 years, CBD diameter ≥ 1.5 cm, EPBD/EPLBD, ESBD, gastrectomy, and CBD morphology.
In multivariate analysis, CBD morphology (P < 0.01), CBD diameter ≥ 1.5 cm [odds ratio (OR) = 2.20, 95%CI: 1.08-4.46, P = 0.03], and ESBD (OR = 0.35, 95%CI: 0.17-0.75, P < 0.01) were identified as independent risk factors. Moreover, the recurrence rate of patients with the S type was 6.61-fold that of patients with the straight type (OR = 6.61, 95%CI: 2.61-16.77, P < 0.01). The recurrence rate of patients with the polyline type was 2.45-fold that of patients with the straight type (OR = 2.45, 95%CI: 1.14-5.26, P = 0.02), and the recurrence rate of S type patients was 2.70-fold that of patients with the polyline type (OR = 2.70, 95%CI: 1.08-6.73, P = 0.03) (Table 5).
| Factor | B | OR (95%CI) | P value | B | OR (95%CI) | P value |
| Age ≥ 70yr | 0.69 | 1.99 (0.99-4.00) | 0.06 | |||
| CBD diameter ≥ 1.5 cm | 0.79 | 2.20 (1.08-4.46) | 0.03 | |||
| EPBD/EPLBD | 0.92 | 2.51 (0.89-7.06) | 0.08 | |||
| ESBD | -1.04 | 0.35 (0.17-0.75) | < 0.01 | |||
| Gastrectomy | 1.46 | 4.29 (0.84-21.83) | 0.08 | |||
| CBD morphology | < 0.01 | < 0.01 | ||||
| Straight type | Reference | -0.90 | 0.41 (0.19-0.88) | 0.02 | ||
| S type | 1.89 | 6.61 (2.61-16.77) | < 0.01 | 0.99 | 2.70 (1.08-6.73) | 0.03 |
| Polyline type | 0.90 | 2.45 (1.14-5.26) | 0.02 | Reference |
ERCP remains the primary choice to extract CBD stones given its minimally invasive nature. However, risk factors for recurrent CBD stones have not been thoroughly defined. In our previous study, we hypothesized that the altered anatomy that resulted from gastrectomy could affect the shape of the CBD. Therefore, we classified the CBD morphology into straight type, S type, and polyline type. The results showed that CBD morphology was related to CBD stone recurrence in gastrectomy patients[10]. As the present study shows, CBD morphology was also related to recurrence in patients without gastrectomy. This clinical observation assumed that the biliary system could undergo anatomic variations as it developed from the primitive midgut and was further changed by surgery, such as gastrectomy. The complexity of CBD development potentially influences its normal function[29,30].
The incidence of CBD stone recurrence in this study was 8.6% with a median 19-month follow-up, which is compatible with previous studies. In multivariate analysis, CBD morphology, CBD diameter ≥ 1.5 cm, and ESBD represent three independent risk factors. More specifically, the recurrence rate of patients with the S type was greater than that of patients with other types. As reported, bile stasis, duodenal-biliary reflux, and bacterial infection are essential factors in the pathogenesis of CBD stone recurrence[31,32]. Given the pathophysiology and the clinical significance of CBD morphology, we can assume the mechanism of recurrence caused by the S type and polyline type. First, a curved CBD is prone to bile stasis, which also predisposes patients to bacterial infection. Second, different shapes of the CBD enter the duodenum at different angles. S-type and polyline-type CBDs enter the duodenum at angles close to a right angle and are prone to intestinal fluid reflux. Duodenal-biliary reflux may cause changes in the bile duct loop and bacterial infection[33].
Our study demonstrated that a CBD diameter ≥ 1.5 cm was an independent risk factor for recurrence. However, the mechanism of CBD dilation is unclear. Some studies assumed that CBD dilation could lead to CBD stone formation[34-36]. The decreased hydrostatic force of bile and loss of normal CBD functional movement may predispose patients to stone reformation[37].
Some studies have shown that age ≥ 70 years is clinically significant for CBD stone recurrence[30,38]. However, this facto was significant in univariate analysis and insignificant in multivariate analysis in our study. Park et al[39] reported that cholecystectomy could be routinely recommended to prevent newly developed gallstones, but it should be considered carefully in patients ≥ 70 of age due to high surgical comorbidity. However, the differences in cholecystectomy were not statistically significant in our study, which was probably limited by the small sample size. Patients aged ≥ 70 years and without cholecystectomy were suggested to undergo careful follow-up for CBD stone recurrence.
Several studies have proposed that gastrectomy patients have an increased risk of cholelithiasis, and the incidence of CBD stones is 10%-25%[24,40-42]. However, gastrectomy did not reach a significant difference due to the small sample size in multivariate analysis. Sugiyama et al[43]. reported that patients with CBD stone recurrence were prone to subsequent recurrence. Our study showed that the subsequent recurrence rate in patients with recurrent CBD stones was greater than the CBD stone recurrence rate (20.9% vs 8.6%). However, significant differences between single recurrence and multiple recurrences were not observed in our study.
EST, EPLBD, EPBD, and ESBD are important ERCP techniques for stone removal. Dong et al[44] conducted a meta-analysis to demonstrate that ESBD exhibited better efficacy and fewer early complications than EST. Another network meta-analysis showed that pancreatitis among ESBD, EPBD and EST did not reach a statistically significant difference. The risk of bleeding in ESBD and EST was higher than that in EPBD[45]. However, neither of them investigated the influence of initial ampullary interventions on recurrent CBD stones. Furthermore, several studies reported that different interventions were unrelated to CBD stone recurrence[30,46,47]. However, our study presented the result that ESBD was an independent risk factor for stone recurrence. Compared with no-ESBD, ESBD decreased the risk of recurrence.
In some studies, the potential contributors influencing ERCP technical difficulty have included the size and number of CBD stones, tapering distal CBD, and the distal CBD arm and angulation[48-50]. However, CBD morphology has never been defined as an independent risk factor for technical difficulty. Prospective and multicentric clinical trials should be conducted to explore the influence of CBD morphology on the ERCP process. Information on CBD morphology should be reported by endoscopists to predict the efficacy of certain devices and therapeutic interventions for CBD stone removal by ERCP and to achieve complete stone clearance.
Ando et al[6] and Cheon et al[51] recommended specific periodic follow-up after therapeutic ERCP, but these authors were not focused on CBD morphology. The exploration of CBD morphology leads to an accurate understanding of potential contributors to recurrent CBD stones. Comprehensive risk factors and a model could provide specific guidance for endoscopists and patients.
To date, our research is the first to evaluate CBD morphology as a risk factor for CBD stone recurrence in average patients. By comparing operative cholangiograms and postoperative ENBD cholangiograms, our study implied that pulling the duodenoscope during the operation could affect CBD angulation and CBD morphology. Therefore, we identified CBD morphology using postoperative ENBD cholangiograms to eliminate bias. During cholangiography, patients were all placed in the left lateral decubitus position. Postoperative cholangiography with ENBD could improve the accuracy of CBD morphology assessment and determine the clearance of CBD stones.
There are several limitations to this study. First, this study was retrospective. Second, we did not evaluate stone components, and this information might have clinical significance for stone recurrence. Third, the follow-up period was short, and a prospective study with a long follow-up could be performed to explore CBD stone recurrence in the future.
In conclusion, CBD morphology was a unique risk factor, and CBD morphology, CBD diameter ≥ 1.5 cm, and ESBD represent three independent risk factors. Further study is needed to reveal the mechanism, predict the procedure difficulty, and instruct the postoperative follow-up.
Preventing recurrent common bile duct (CBD) stones is an indispensable study. However, the risk factors for CBD stone recurrence after Endoscopic retrograde cholangiopancreatography (ERCP) are unclear.
The CBD on the cholangiogram is common in every ERCP operations. But CBD morphology has never been classified and discussed.
The aim was to investigate the relationship between CBD morphology and recurrent CBD stones in patients after ERCP.
From February 2020 to January 2021, 502 patients after ERCP at our center were included in the retrospective case-control study. Univariate analysis and multivariate logistic regression analysis were performed to identify risk factors for CBD stone recurrence.
CBD morphology, CBD diameter ≥ 1.5 cm, and endoscopic biliary sphincterotomy with balloon dilation (ESBD) are three independent risk factors for CBD stone recurrence. Furthermore, CBD diameter ≥ 1.5 cm could increase the risk of recurrence and ESBD could decrease the risk of recurrence.
Of the three CBD morphology, patients with the S type had the highest risk of recurrent CBD stones, followed by those with the polyline type and the lowest were the straight type.
A large-scale prospective study should be performed to verified patients with above risk factors could prevent recurrence with medical treatment, such as Ursodeoxycholic acid. And the surveillance period needs further research.
The study was supported by the Digestive Endoscopy Centre at General Hospital of Northern Theater Command.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and Hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Awai K, Japan; Thacoor A, United Kingdom S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Fujita Y, Iwasaki A, Sato T, Fujisawa T, Sekino Y, Hosono K, Matsuhashi N, Sakamaki K, Nakajima A, Kubota K. Feasibility of Endoscopic Papillary Large Balloon Dilation in Patients with Difficult Bile Duct Stones without Dilatation of the Lower Part of the Extrahepatic Bile Duct. Gut Liver. 2017;11:149-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Osnes M, Rosseland AR, Aabakken L. Endoscopic retrograde cholangiography and endoscopic papillotomy in patients with a previous Billroth-II resection. Gut. 1986;27:1193-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ, Lande JD, Pheley AM. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1687] [Article Influence: 58.2] [Reference Citation Analysis (2)] |
| 5. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective "short" double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 6. | Ando T, Tsuyuguchi T, Okugawa T, Saito M, Ishihara T, Yamaguchi T, Saisho H. Risk factors for recurrent bile duct stones after endoscopic papillotomy. Gut. 2003;52:116-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 124] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Keizman D, Ish Shalom M, Konikoff FM. Recurrent symptomatic common bile duct stones after endoscopic stone extraction in elderly patients. Gastrointest Endosc. 2006;64:60-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Kim DI, Kim MH, Lee SK, Seo DW, Choi WB, Lee SS, Park HJ, Joo YH, Yoo KS, Kim HJ, Min YI. Risk factors for recurrence of primary bile duct stones after endoscopic biliary sphincterotomy. Gastrointest Endosc. 2001;54:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Sugiyama M, Atomi Y. Risk factors predictive of late complications after endoscopic sphincterotomy for bile duct stones: long-term (more than 10 years) follow-up study. Am J Gastroenterol. 2002;97:2763-2767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 99] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Ji X, Jia W, Zhao Q, Wang Y, Ma SR, Xu L, Kan Y, Cao Y, Fan BJ, Yang Z. Common bile duct morphology is associated with recurrence of common bile duct stones in Billroth II anatomy patients. World J Clin Cases. 2021;9:7671-7681. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Deng F, Zhou M, Liu PP, Hong JB, Li GH, Zhou XJ, Chen YX. Causes associated with recurrent choledocholithiasis following therapeutic endoscopic retrograde cholangiopancreatography: A large sample sized retrospective study. World J Clin Cases. 2019;7:1028-1037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Oak JH, Paik CN, Chung WC, Lee KM, Yang JM. Risk factors for recurrence of symptomatic common bile duct stones after cholecystectomy. Gastroenterol Res Pract. 2012;2012:417821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Kim MH, Myung SJ, Seo DW, Lee SK, Kim YS, Lee MH, Yoo BM, Min MI. Association of periampullary diverticula with primary choledocholithiasis but not with secondary choledocholithiasis. Endoscopy. 1998;30:601-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Konstantakis C, Triantos C, Theopistos V, Theocharis G, Maroulis I, Diamantopoulou G, Thomopoulos K. Recurrence of choledocholithiasis following endoscopic bile duct clearance: Long term results and factors associated with recurrent bile duct stones. World J Gastrointest Endosc. 2017;9:26-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Paspatis GA, Paraskeva K, Vardas E, Papastergiou V, Tavernaraki A, Fragaki M, Theodoropoulou A, Chlouverakis G. Long-term recurrence of bile duct stones after endoscopic papillary large balloon dilation with sphincterotomy: 4-year extended follow-up of a randomized trial. Surg Endosc. 2017;31:650-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Mu H, Gao J, Kong Q, Jiang K, Wang C, Wang A, Zeng X, Li Y. Prognostic Factors and Postoperative Recurrence of Calculus Following Small-Incision Sphincterotomy with Papillary Balloon Dilation for the Treatment of Intractable Choledocholithiasis: A 72-Month Follow-Up Study. Dig Dis Sci. 2015;60:2144-2149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Kato S, Chinen K, Shinoura S, Kikuchi K. Predictors for bile duct stone recurrence after endoscopic extraction for naïve major duodenal papilla: A cohort study. PLoS One. 2017;12:e0180536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Nzenza TC, Al-Habbal Y, Guerra GR, Manolas S, Yong T, McQuillan T. Recurrent common bile duct stones as a late complication of endoscopic sphincterotomy. BMC Gastroenterol. 2018;18:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 19. | Zhao HC, He L, Zhou DC, Geng XP, Pan FM. Meta-analysis comparison of endoscopic papillary balloon dilatation and endoscopic sphincteropapillotomy. World J Gastroenterol. 2013;19:3883-3891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 20. | Kang DU, Choi Y, Lee HS, Lee HJ, Park SH, Yang DH, Yoon SM, Kim KJ, Ye BD, Myung SJ, Yang SK, Kim JH, Byeon JS. Endoscopic and Clinical Factors Affecting the Prognosis of Colorectal Endoscopic Submucosal Dissection-Related Perforation. Gut Liver. 2016;10:420-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Xu XD, Chen B, Dai JJ, Qian JQ, Xu CF. Minor endoscopic sphincterotomy followed by large balloon dilation for large choledocholith treatment. World J Gastroenterol. 2017;23:5739-5745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Guo SB, Meng H, Duan ZJ, Li CY. Small sphincterotomy combined with endoscopic papillary large balloon dilation vs sphincterotomy alone for removal of common bile duct stones. World J Gastroenterol. 2014;20:17962-17969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 366] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 24. | Bove V, Tringali A, Familiari P, Gigante G, Boškoski I, Perri V, Mutignani M, Costamagna G. ERCP in patients with prior Billroth II gastrectomy: report of 30 years' experience. Endoscopy. 2015;47:611-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 25. | Hashimoto M, Imamura T, Tamura T, Koyama R, Koizumi Y, Makuuchi M, Matsuda M, Watanabe G. Treatment of biliary tract stones after gastrectomy in the era of laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci. 2016;23:703-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Strnad P, von Figura G, Gruss R, Jareis KM, Stiehl A, Kulaksiz H. Oblique bile duct predisposes to the recurrence of bile duct stones. PLoS One. 2013;8:e54601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Zhang R, Luo H, Pan Y, Zhao L, Dong J, Liu Z, Wang X, Tao Q, Lu G, Guo X. Rate of duodenal-biliary reflux increases in patients with recurrent common bile duct stones: evidence from barium meal examination. Gastrointest Endosc. 2015;82:660-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Seo DB, Bang BW, Jeong S, Lee DH, Park SG, Jeon YS, Lee JI, Lee JW. Does the bile duct angulation affect recurrence of choledocholithiasis? World J Gastroenterol. 2011;17:4118-4123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Ando H. Embryology of the biliary tract. Dig Surg. 2010;27:87-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Choi SJ, Yoon JH, Koh DH, Lee HL, Jun DW, Choi HS. Low insertion of cystic duct increases risk for common bile duct stone recurrence. Surg Endosc. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 31. | Kullman E, Borch K, Lindström E, Anséhn S, Ihse I, Anderberg B. Bacteremia following diagnostic and therapeutic ERCP. Gastrointest Endosc. 1992;38:444-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Leung JW, Liu YL, Leung PS, Chan RC, Inciardi JF, Cheng AF. Expression of bacterial beta-glucuronidase in human bile: an in vitro study. Gastrointest Endosc. 2001;54:346-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Zhang Q, Ye M, Su W, Chen Y, Lou Y, Yang J, Ma T, Chen W, Gao S, Que R, Zhang B, Li H, Bai X, Liang T. Sphincter of Oddi laxity alters bile duct microbiota and contributes to the recurrence of choledocholithiasis. Ann Transl Med. 2020;8:1383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 34. | Kim KH, Rhu JH, Kim TN. Recurrence of bile duct stones after endoscopic papillary large balloon dilation combined with limited sphincterotomy: long-term follow-up study. Gut Liver. 2012;6:107-112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 35. | Costamagna G, Tringali A, Shah SK, Mutignani M, Zuccalà G, Perri V. Long-term follow-up of patients after endoscopic sphincterotomy for choledocholithiasis, and risk factors for recurrence. Endoscopy. 2002;34:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 109] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 36. | Ohashi A, Tamada K, Wada S, Hatanaka H, Tomiyama T, Tano S, Nakazawa K, Sugano K. Risk factors for recurrent bile duct stones after endoscopic papillary balloon dilation: long-term follow-up study. Dig Endosc. 2009;21:73-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 37. | Zhou XD, Chen QF, Zhang YY, Yu MJ, Zhong C, Liu ZJ, Li GH, Zhou XJ, Hong JB, Chen YX. Outcomes of endoscopic sphincterotomy vs open choledochotomy for common bile duct stones. World J Gastroenterol. 2019;25:485-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 38. | Kim KY, Han J, Kim HG, Kim BS, Jung JT, Kwon JG, Kim EY, Lee CH. Late Complications and Stone Recurrence Rates after Bile Duct Stone Removal by Endoscopic Sphincterotomy and Large Balloon Dilation are Similar to Those after Endoscopic Sphincterotomy Alone. Clin Endosc. 2013;46:637-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 39. | Park BK, Seo JH, Jeon HH, Choi JW, Won SY, Cho YS, Lee CK, Park H, Kim DW. A nationwide population-based study of common bile duct stone recurrence after endoscopic stone removal in Korea. J Gastroenterol. 2018;53:670-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Paik KH, Lee JC, Kim HW, Kang J, Lee YS, Hwang JH, Ahn SH, Park DJ, Kim HH, Kim J. Risk Factors for Gallstone Formation in Resected Gastric Cancer Patients. Medicine (Baltimore). 2016;95:e3157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 41. | Hosouchi Y, Nagamachi Y, Hara T. Evaluation of transverse colon interposition following total gastrectomy in patients with gastric carcinoma. Oncol Rep. 1998;5:87-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 42. | Hauters P, de Neve de Roden A, Pourbaix A, Aupaix F, Coumans P, Therasse G. Cholelithiasis: a serious complication after total gastrectomy. Br J Surg. 1988;75:899-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 43. | Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut. 2004;53:1856-1859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 44. | Dong SQ, Singh TP, Zhao Q, Li JJ, Wang HL. Sphincterotomy plus balloon dilation vs sphincterotomy alone for choledocholithiasis: a meta-analysis. Endoscopy. 2019;51:763-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Park CH, Jung JH, Nam E, Kim EH, Kim MG, Kim JH, Park SW. Comparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysis. Gastrointest Endosc. 2018;87:43-57.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 46. | Choe JW, Kim SY, Lee DW, Hyun JJ, Ahn KR, Yoon I, Jung SW, Jung YK, Koo JS, Yim HJ, Lee SW. Incidence and risk factors for postoperative common bile duct stones in patients undergoing endoscopic extraction and subsequent cholecystectomy. Gastrointest Endosc. 2021;93:608-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 47. | Chae MK, Lee SH, Joo KR. Assessment of the possible risk factors for primary common bile duct stone recurrence after cholecystectomy. Surg Endosc. 2021;35:6497-6504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 48. | Kim HJ, Choi HS, Park JH, Park DI, Cho YK, Sohn CI, Jeon WK, Kim BI, Choi SH. Factors influencing the technical difficulty of endoscopic clearance of bile duct stones. Gastrointest Endosc. 2007;66:1154-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 89] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 49. | Huang L, Lu X, Huang X, Zou X, Wu L, Zhou Z, Wu D, Tang D, Chen D, Wan X, Zhu Z, Deng T, Shen L, Liu J, Zhu Y, Gong D, Zhong Y, Liu F, Yu H. Intelligent difficulty scoring and assistance system for endoscopic extraction of common bile duct stones based on deep learning: multicenter study. Endoscopy. 2021;53:491-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 50. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Moon JH, Park SH, Itoi T, Isayama H, Kogure H, Lee SJ, Jung KT, Lee HS, Baron TH, Lee DK. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 51. | Cheon YK, Lehman GA. Identification of risk factors for stone recurrence after endoscopic treatment of bile duct stones. Eur J Gastroenterol Hepatol. 2006;18:461-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |