Published online Dec 27, 2022. doi: 10.4240/wjgs.v14.i12.1432
Peer-review started: September 15, 2022
First decision: October 21, 2022
Revised: October 28, 2022
Accepted: November 22, 2022
Article in press: November 22, 2022
Published online: December 27, 2022
Processing time: 103 Days and 7.3 Hours
Common diseases after radical gastrectomy include cholecystitis and pancreatitis, but the sudden onset of acute appendicitis in a short period following radical gastrectomy is very rare, and its clinical symptoms are easily misdiagnosed as duodenal stump leakage.
This is a case report of a 77-year-old woman with lower right abdominal pain 14 d after radical resection of gastric cancer. Her pain was not relieved by conservative treatment, and her inflammatory markers were elevated. Computed tomography showed effusion in the perihepatic and hepatorenal spaces, right paracolic sulcus and pelvis, as well as exudative changes in the right iliac fossa. Ultrasound-guided puncture revealed a slightly turbid yellow-green fluid. Laparoscopic exploration showed a swollen appendix with surrounding pus moss and no abnormalities of the digestive anastomosis or stump; thus, laparoscopic app
Acute appendicitis in the short term after radical gastrectomy needs to be differentiated from duodenal stump leakage, and early diagnosis and surgery are the most important means of treatment.
Core Tip: Common forms of abdominal inflammation occurring after radical gastrectomy are cholecystitis and pancreatitis, of which cholecystitis has the highest incidence. In contrast, the incidence of appendicitis in the short term after radical gastrectomy is rare and has not been reported before. Herein, we present a case of acute appendicitis in the short term following radical total gastrectomy. We suggest that acute appendicitis in the short term after gastric cancer surgery needs to be differentiated from duodenal stump leakage and that early diagnosis and surgery are the most important means of treatment.
- Citation: Ma J, Zha ZP, Zhou CP, Miao X, Duan SQ, Zhang YM. Acute appendicitis in the short term following radical total gastrectomy misdiagnosed as duodenal stump leakage: A case report. World J Gastrointest Surg 2022; 14(12): 1432-1437
- URL: https://www.wjgnet.com/1948-9366/full/v14/i12/1432.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i12.1432
Acute appendicitis is mainly caused by bacteria, fecal stones, and malformations, and the pathogenic condition must be mucosal damage and bacterial invasion[1]. Common forms of abdominal inflammation occurring after radical gastrectomy are cholecystitis and pancreatitis, of which cholecystitis has the highest incidence[2]. In contrast, the incidence of appendicitis in the short term after radical resection of gastric cancer is rare and has not been reported. The lack of typical symptoms of metastatic lower right abdominal pain is attributed to resection of the stomach and greater omentum. The symptoms mainly manifest as persistently aggravated right-sided abdominal pain and a high perforation rate; therefore, the inflammation is not easily confined, and the clinical symptoms are easily misdiagnosed as duodenal stump leakage.
Durative pain in the lower right abdomen 14 d after radical total gastrectomy.
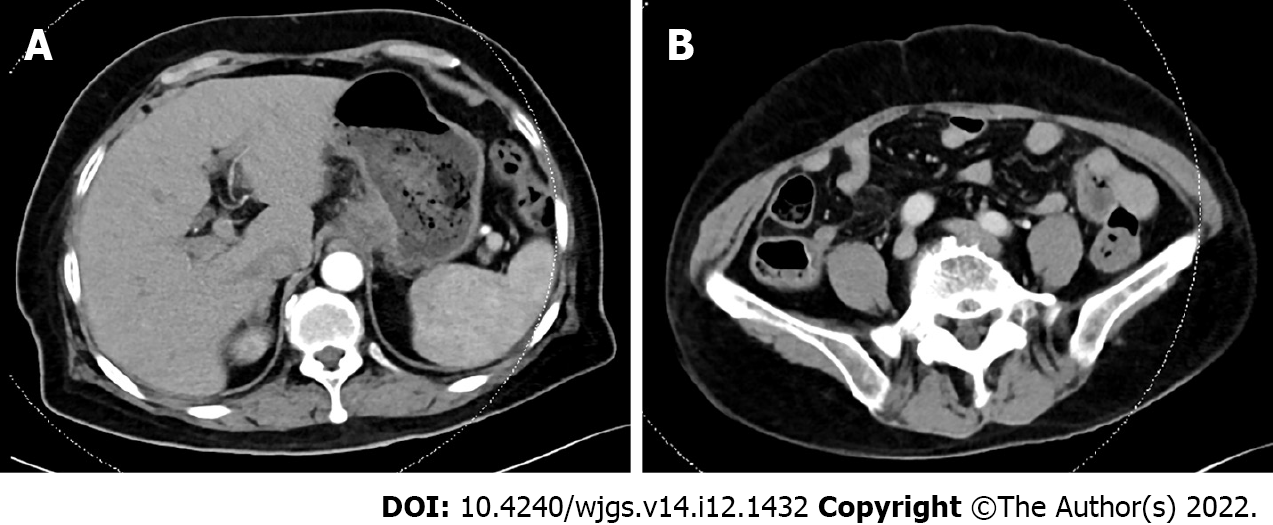
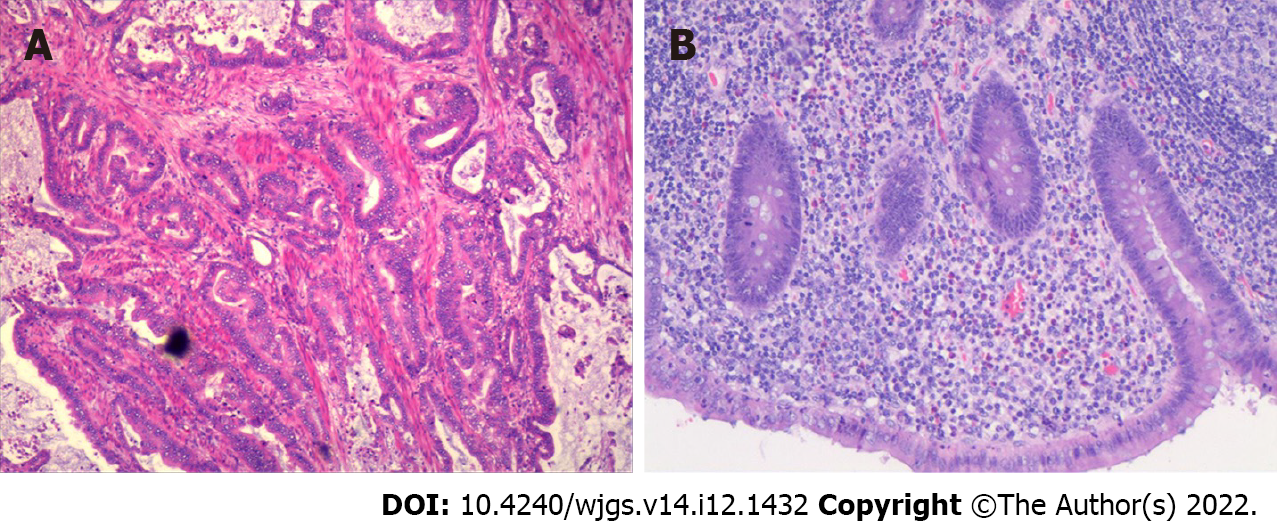
A 77-year-old woman was diagnosed with gastric cancer, and preoperative pathology showed adenocarcinoma, moderately differentiated, HP (-). On May 23, 2022, computed tomography (CT) showed that the cardia was thickened and reinforced (Figure 1A), and the appendix was normal (Figure 1B). Preoperative clinical staging showed cT4Nx; preoperative neoadjuvant therapy was recommended, but the patient refused due to advanced age, and "radical total gastrectomy (D2 lymph node dissection)" was performed under general anesthesia on May 26, 2022. Intraoperative exploration: The gallbladder had been removed; the omentum was adhered to the gallbladder bed, no ascites was seen, and no metastatic nodules were seen in the liver or peritoneum. Postoperative pathology indicated stage IIIB, moderately differentiated, intestinal-type adenocarcinoma with lymph node involvement (7/30) (Figure 2A). The resection margin was negative. The immunohistochemical marker results were as follows: CK (+), Her-2 (3+), MSH2 (+), MSH6 (+), PMS2 (+), MLH1 (+), and Ki-67 (approximately 70%).
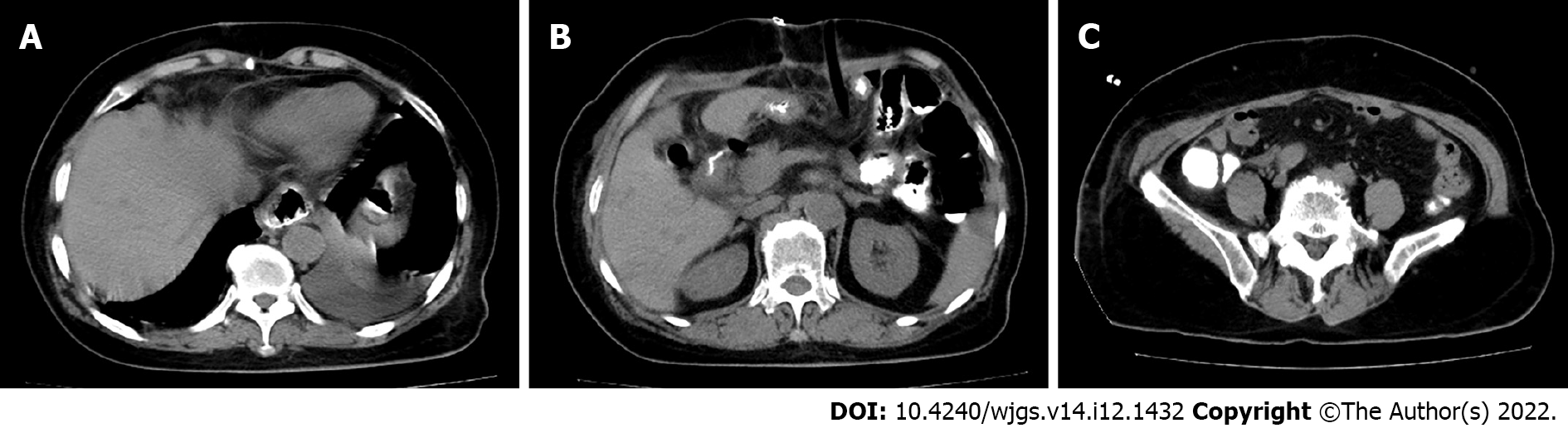
The patient recovered well after the operation; all inflammatory indexes gradually decreased, and her blood sugar was well controlled. On June 3, 2022, her D-dimer level was significantly elevated, and ultrasound showed intermuscular thrombosis located in the lower right extremity, which was treated with low-molecular-weight heparin. On June 4, 2022, CT showed no abnormalities around the anastomosis or stump, no leakage of oral pantothenic glucosamine into the abdominal cavity, no abnormalities in the ileocecal region or appendix, and no significant fluid accumulation in the abdominopelvic cavity (Figure 3). On June 8, 2022, her blood count, calcitonin and C-reactive protein (CRP) levels were normal, and she was ready to be discharged. However, during the night of June 9, 2022, the patient complained of persistent pain on the right side of the abdomen, and the abdominal pain became significantly worse on the morning of June 10, 2022.
The patient had a previous history of diabetes, hypertension, cholecystectomy and no history of chronic appendicitis.
There was no family history of tumors.
On June 6, the abdominal incision was healing well, and the patient reported tenderness in the lower right abdomen, muscle tension and rebound pain.
The patient’s leukocyte level was 17.18 × 109/L; neutrophil ratio, 88.4%; calcitonin level, 0.19 ng/mL; and CRP level, 65.20 mg/L.
On June 10, 2022, CT showed effusion in the perihepatic and hepatorenal spaces, right paracolic sulcus and pelvis and exudative changes in the right iliac fossa (Figure 4). Subsequent ultrasound-guided puncture revealed a slightly turbid yellow-green fluid.
Acute suppurative appendicitis after radical gastrectomy.
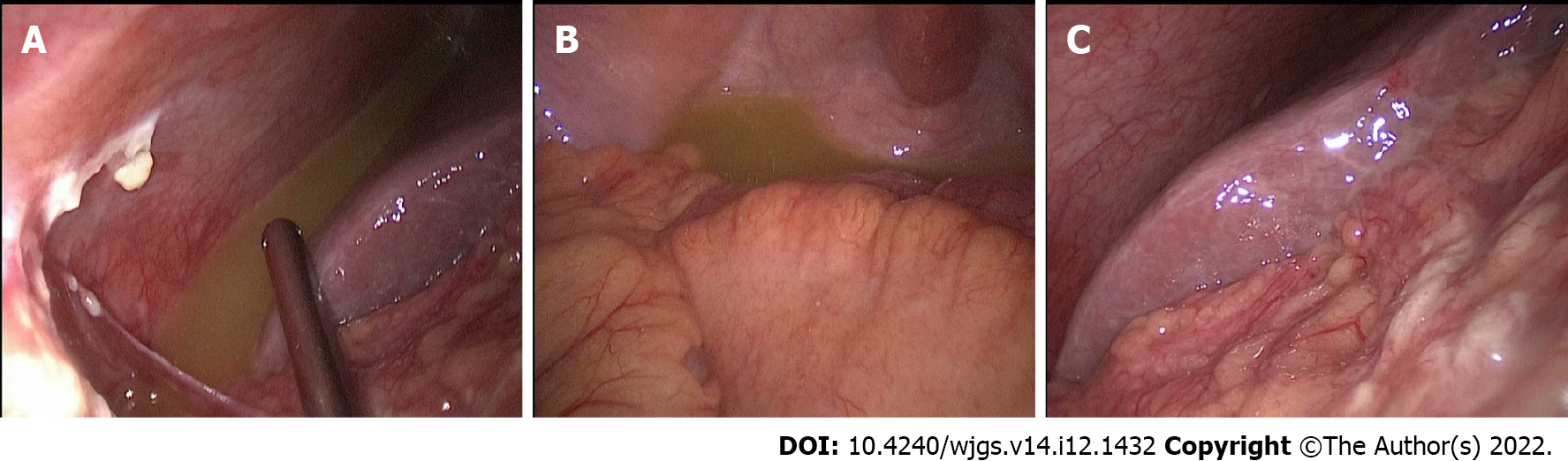
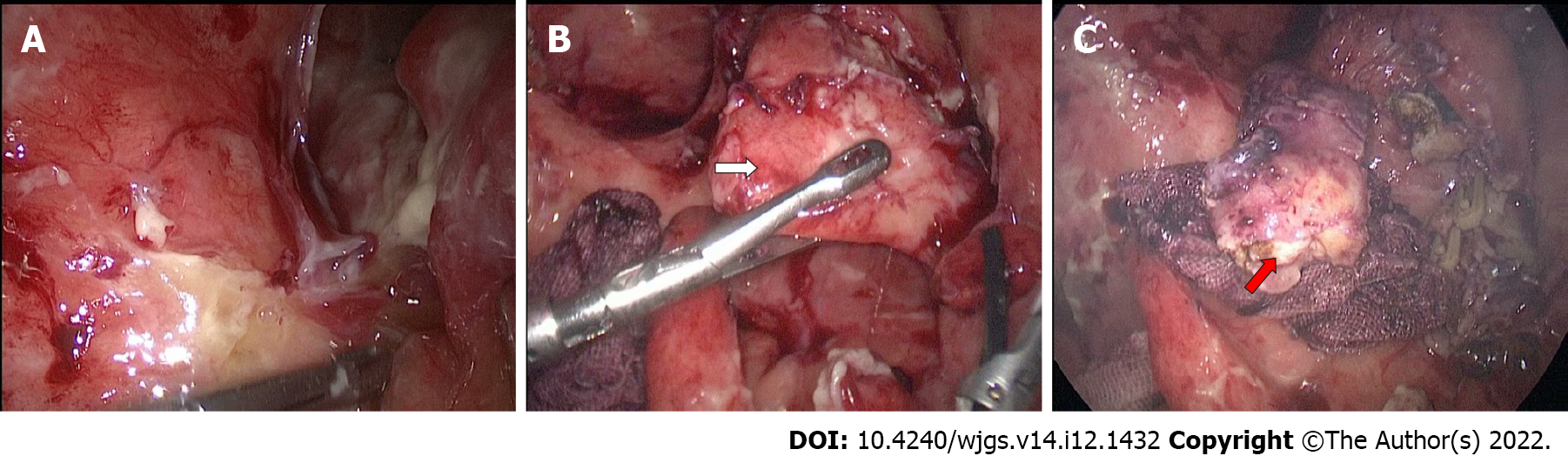
On June 10, 2022, laparoscopic exploration revealed yellow-green fluid in the perihepatic and pelvic cavities (Figure 5A and B); the duodenal stump was wrapped in tissue and did not show leakage (Figure 5C), and there were no abnormalities in the esophageal-jejunal anastomosis or jejunal-jejunal anastomosis. A large amount of pus moss was seen in the ileocecal region, and the terminal ileum wrapped around the appendix (Figure 6A). A septic and swollen appendix was seen after careful laparoscopic separation of the adhesions (Figure 6B). The appendiceal mesentery was treated with harmonic scissors and absorbable clips, the root of the appendix was ligated with thread, and the appendiceal stump was cauterized (Figure 6C). A pelvic drainage tube was placed after aspiration of intra-abdominal fluid.
Postoperative pathology showed acute purulent appendicitis and periapical inflammation (Figure 2B). The patient recovered well after surgery and was successfully discharged two weeks later. Follow-up CT showed no significant abnormalities in the abdominal cavity (Figure 7). The patient continued adjuvant chemotherapy after surgery, completing three cycles of oxaliplatin and S-1 (SOX regimen).
Cholecystitis and pancreatitis are common diseases after radical resection of gastric cancer. Appendicitis occurs rarely, as early as several months later, and perioperative combined episodes of appendicitis are even rarer.
There were several reasons for misdiagnosis in this case. First, we usually used one etiology to explain all the symptoms of the patient; we would focus on postoperative complications but might ignore the possibility of common diseases. Second, the most common abdominal complication after radical gastrectomy is duodenal stump leakage[3]. The patient had a history of diabetes and presented with postoperative right abdominal pain. CT showed hepatorenal and pelvic effusion, and the puncture revealed yellow-green turbid fluid, which could not exclude the occurrence of duodenal stump leakage.
This is a successful case in which laparoscopic exploration was promptly performed to clarify the diagnosis. This case is enlightening for the following reasons: (1) For patients with a history of diabetes and postoperative lower right abdominal pain, the possibility of appendicitis must be considered, as diabetes is a high-risk factor for appendicitis[4]; (2) Patients with appendicitis following gastrectomy have atypical abdominal pain due to surgical removal of all or a large part of the stomach, and reconstruction of the digestive tract alters the original physiological structure; (3) The large omentum was removed and could no longer easily confine the acute inflammation of the appendix; thus, as the disease worsened, diffuse peritonitis developed; (4) The occurrence of appendicitis has been reported in conjunction with several other diseases, such as colon cancer, tuberculosis, herniation and gynecological diseases[5-8]; and (5) Gastric cancer combined with appendiceal metastasis would cause symptoms of acute appendicitis, but in this case, there was no peritoneal or appendiceal metastasis[9]. In conclusion, acute appendicitis occurring within a short period after radical gastrectomy has its own characteristics and is easily confused with postoperative complications of gastric cancer; thus, a clear diagnosis and early surgical treatment are needed.
Acute appendicitis in the short term after gastric cancer is rare and easily ignored clinically and needs to be differentiated from duodenal stump leakage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arigami T, Japan; Moshref RH, Saudi Arabia; Straksyte V, Lithuania S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 685] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 2. | Seo HS, Na Y, Jung J. Analysis of the Occurrence of Diseases Following Gastrectomy for Early Gastric Cancer: a Nationwide Claims Study. J Gastric Cancer. 2021;21:279-297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Ramos MFKP, Pereira MA, Barchi LC, Yagi OK, Dias AR, Szor DJ, Zilberstein B, Ribeiro-Júnior U, Cecconello I. Duodenal fistula: The most lethal surgical complication in a case series of radical gastrectomy. Int J Surg. 2018;53:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Tseng CH. Metformin use is associated with a reduced risk of acute appendicitis in Taiwanese patients with type 2 diabetes mellitus. Sci Rep. 2021;11:12400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Hajibandeh S, Hajibandeh S, Morgan R, Maw A. The incidence of right-sided colon cancer in patients aged over 40 years with acute appendicitis: A systematic review and meta-analysis. Int J Surg. 2020;79:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Chiș B, Dudric V, Fodor D. Tuberculous appendicitis. A case report. Med Ultrason. 2017;19:333-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Bettini A, Ulloa JG, Harris H. Appendicitis within Morgagni Hernia and simultaneous Paraesophageal Hernia. BMC Surg. 2015;15:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Noor M, Chen A, Gonzalez RS. Clinicopathologic findings in gynecologic proliferations of the appendix. Hum Pathol. 2019;92:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Wang W, Cui T, Mao W. Acute appendicitis caused by metastatic gastric adenocarcinoma: a case report and literature review. Ann Palliat Med. 2021;10:7132-7137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |