Published online Jan 27, 2022. doi: 10.4240/wjgs.v14.i1.56
Peer-review started: April 5, 2021
First decision: July 3, 2021
Revised: July 31, 2021
Accepted: January 13, 2022
Article in press: January 13, 2022
Published online: January 27, 2022
Processing time: 288 Days and 23 Hours
Biliary atresia (BA) is a rare pediatric disease.
To compare the outcomes of laparoscopic portoenterostomy (Lap-PE) with those of laparotomy (Open-PE) at a single institution.
The surgical outcomes of PE were retrospectively analyzed for patients with a non-correctable type of BA from 2003 to 2020.
Throughout the assessment period, 119 patients received PE for BA treatment, including 66 Open-PE and 53 Lap-PE cases. Although the operation duration was longer (medians: for Open-PE, 242 min; for Lap-PE, 341 min; P < 0.001), blood loss was considerably less (medians: for Open-PE, 52 mL; for Lap-PE, 24 mL; P < 0.001) in the Lap-PE group than in the Open-PE group. The postoperative recovery of the Lap-PE group was more favorable; specifically, both times to resume oral intake and drain removal were significantly shorter in the Lap-PE group. Complete resolution of jaundice was observed in 45 Open-PE cases and 42 Lap-PE cases, with no statistically significant difference (P = 0.176). Native liver survival rates were >80% for both groups for the first half year post surgery, followed by a gradual decrease with time; there were no statistically significant differences in the native liver survival rates for any durations assessed.
Lap-PE could be a standard therapy for BA.
Core Tip: The aim of this study was to compare the outcomes of laparoscopic portoenterostomy (Lap-PE) with those of laparotomy (Open-PE) at our single institution. Although the surgical operating time was longer, the lower blood loss and more favorable postsurgical recovery (shorter time to resume oral intake and time to drain removal as well as less postsurgical adhesion) were significant advantages of Lap-PE over Open-PE. There was no significant difference in native liver survival rates or short-term surgical outcomes between LapPE and OpenPE. Therefore, our study results support the efficacy of Lap-PE as a standard therapy.
- Citation: Shirota C, Hinoki A, Tainaka T, Sumida W, Kinoshita F, Yokota K, Makita S, Amano H, Nakagawa Y, Uchida H. Laparoscopic Kasai portoenterostomy can be a standard surgical procedure for treatment of biliary atresia. World J Gastrointest Surg 2022; 14(1): 56-63
- URL: https://www.wjgnet.com/1948-9366/full/v14/i1/56.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v14.i1.56
Although liver transplantation (LTx) is an established treatment for biliary atresia (BA), Kasai portoenterostomy (PE) is still the firstline standard treatment to maintain the native liver. However, the outcome of PE for treating BA has not improved over the past 20 years, and 35%–60% of the patients who have undergone PE eventually underwent LTx[1,2].
We followed a standard surgical protocol that involved minimally invasive therapies with a laparoscope or thoracoscope; this protocol had been initially established in adult surgeries and has been applied as a standard procedure in various pediatric surgeries. Even if PE for BA is successful, some patients subsequently need LTx. In comparison with OpenPE, LapPE is much less invasive, postsurgical recovery is favorable, and adhesions are minimal, which are significant advantages for patients who require LTx.
Laparoscopy in patients with BA has been studied previously. Evidence in favor of laparotomy (OpenPE) appeared to be stronger than that of LapPE[3-6]; however, the number of recent reports demonstrating favorable outcomes of LapPE comparable with those of OpenPE have been increasing[7]. Those studies supporting LapPE, however, were all small, and none of them had reasonable sample sizes at a single institution (i.e., ≥50 cases each of LapPE and OpenPE) for comparing the outcomes with reasonable statistical power. Postoperative management after BA surgeries is complicated and requires a centralized procedure for consistency. Thus, it is considered important to perform a large-scale assessment at a single facility with a centralized management procedure for adequate comparison in the outcomes between LapPE and OpenPE [8,9].
In the case of BA, however, evidence for the usefulness of laparoscopic PE (LapPE) as a treatment option for BA, which is a rare pediatric disease, is still being obtained and evaluated. Therefore, the application of LapPE as a treatment option for BA remains controversial.
At our institution, we have made efforts to apply LapPE and improve our surgical technique and patient outcomes to increase the success rate of PE. The study aim was to compare the outcomes of LapPE at our single institution with those of OpenPE.
We obtained approval from our institutional ethics board for a retrospective review of the medical records of patients diagnosed with BA at our institution (approval number: 2020-0593).
The surgical outcomes of PE were retrospectively analyzed for patients with a noncorrectable type of BA who underwent PE at our institution from January 2003 to December 2020. The cases of correctable types of BA were excluded from the assessment. BA was diagnosed on the basis of a combination of radiographic findings, surgical findings of uncorrectable types, and liver histology. Complete resolution of jaundice was determined when the total bilirubin value was decreased by ≤ 1.2 mg/dL. Survival with the native liver was defined as the time when the liver functioned without LTx.
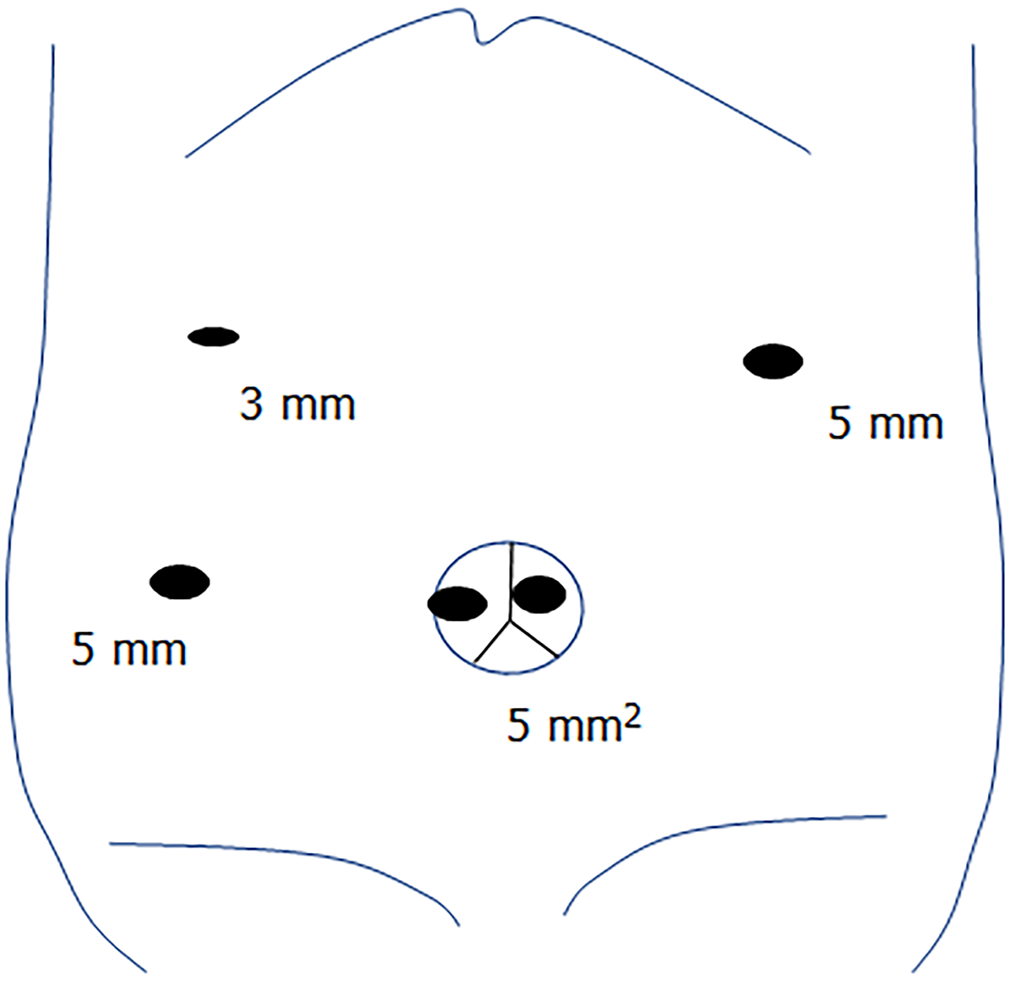
Although there was a difference between laparotomy and laparoscopy, the operative procedure did not drastically change during the study period. In laparoscopic surgery, the ports were placed as shown in Figure 1. Intraoperative cholangiography was performed in all cases, during both laparotomy and laparoscopy, to confirm the presence of bile ducts. We used 5-0 monofilament absorbable sutures for portoenterostomy in both open and laparoscopic surgeries. One of the most important points is that the fibrous tissue in the hilar plate is dissected just before baring the liver parenchyma; it is not completely resected. Then, the area between the right porta hepatic, in which the right anterior branch of the hepatic artery and portal vein enter the hepatic parenchyma, and the left porta hepatic, in which the left branch of the portal vein enters the parenchyma, should be dissected for anastomosis. In our study, all patients were treated by the same team at a single institution, thereby minimizing any differences in surgical procedure or postoperative management.
Data were statistically analyzed by performing the chi-squared test and Wilcoxon rank-sum test, with a P value of < 0.05 taken to be indicative of statistical significance except for native liver survival rates, which were analyzed by performing Kaplan-Meier method and the log-rank test. We used JMP Pro 15 (SAS Institute Inc., NC, United States) statistical software for statistical analyses.
Throughout the assessment period, 119 patients received PE for the treatment of a noncorrectable type of BA, including 66 OpenPE and 53 LapPE cases. No case was converted from laparoscopy to laparotomy. The median (range) values of key surgical parameters are shown by operation type (OpenPE group and LapPE group) in Table 1. The median age at surgery was significantly younger (P = 0.0018) in the LapPE (53 d) group than in the OpenPE group (66 d). Although the operation duration was longer in the Lap-PE group (median: 341 min) than in the Open-PE group (median: 271.5 min; P < 0.001), blood loss was significantly less in the Lap-PE group (median: 23.5 mL) than in the Open-PE group (52 mL; P < 0.001).
| Open-PE | Lap-PE | P value | |
| Number of patients | 66 | 53 | |
| Age at surgery | 66.0 (32.0-144.0) | 55.0 (23.0-116.0) | 0.0013 |
| Operation duration | 271.5 (167.0-390.0) | 341.0 (242.0-512.0) | < 0.0001 |
| Blood loss | 52.0 (5.0-363.0) | 23.5 (1.0-160.0) | < 0.0001 |
| Time to resume oral intake | 6.0 (3.0-14.0) | 3.0 (2.0-6.0) | < 0.0001 |
| Time to drain removal | 7.0 (3.0-15.0) | 6.0 (3.0-16.0) | 0.0004 |
| Complete resolution from jaundice case (%) | 45 (68.2%) | 42 (79.2%) | 0.176 |
The postoperative courses of recovery—specifically, both time to resume oral intake (medians: 3 and 6 postoperative days, respectively; P < 0.001) and time to drain removal (medians: 6 and 7 postoperative days, respectively; P < 0.001)—were significantly shorter in the Lap-PE group than in the Open-PE group. Complete resolution of jaundice was observed in 45 (68.2%) patients who underwent Open-PE and in 42 (79.3%) patients who underwent Lap-PE cases; the difference was not statistically significant (Table 1).
Forty-four patients underwent liver transplantation during the study period. The median duration from the Kasai operation to liver transplantation was 204 d (range: 54–1889 d) overall, with 156 d (range: 54–1889 d) for laparotomy and 249 d (range: 58–1479 d) for laparoscopy. Thirty-two patients did not achieve complete resolution from jaundice with the Kasai operation. Thirty of the 32 patients underwent liver transplantation, except for one patient who refused liver transplantation and one patient who died before the transplantation. The median duration between PE and liver transplantation was 156 d (range: 54–1889 d) after laparotomy and 127 d (range: 58–261 d) after laparoscopy. The remaining 14 patients underwent liver transplantation for the following reasons: Recurrent jaundice in 11 patients; hepatopulmonary syndrome, 1; repeated cholangitis, 1; and repeated melena, 1.
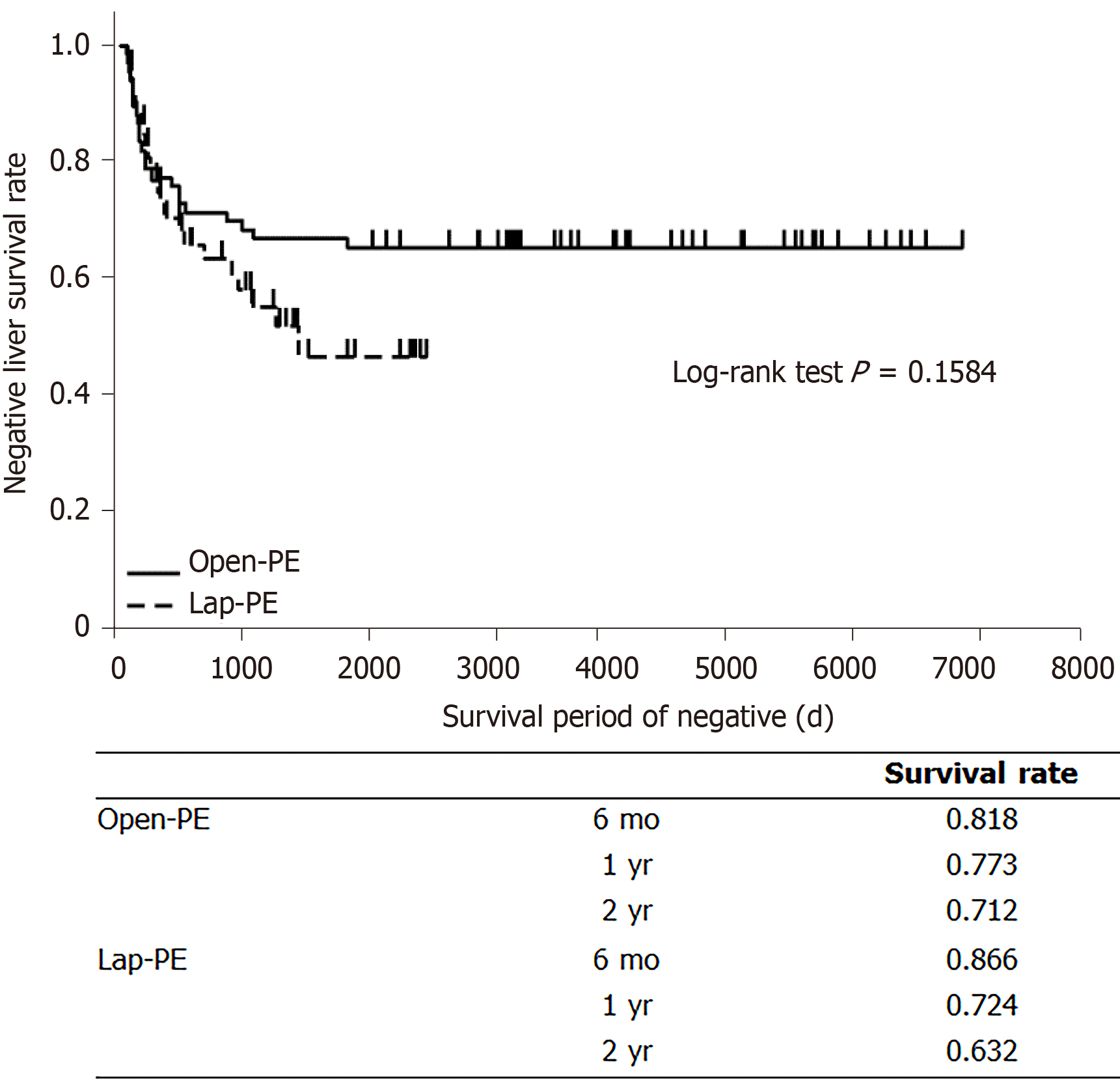
Native liver survival rates were > 80% for both groups for the first half year postsurgery, followed by a gradual decrease with time; there were no statistically significant differences in the native liver survival rates between the two groups for any durations assessed (log-rank test; P = 0.1584) (Figure 2).
During the study period, no intraoperative complications occurred in either open or laparoscopic procedures. Nine (13.6%) patients who underwent laparotomy and six (11.3%) who underwent laparoscopy were readmitted for cholangitis within 3 mo after surgery. Three patients underwent reoperation for bile stasis caused by adhesions of the Roux-en-Y anastomosis to the jejunum after laparotomy. Intestinal obstruction occurred after laparotomy in three patients and after laparoscopy in three patients. One patient underwent reoperation for anastomotic bleeding after laparoscopic surgery.
Operations by pediatric surgeons qualified by the Japanese Endoscopic Surgical Skill Qualification Committee were significantly shorter (P = 0.0314) than those performed by nonqualified surgeons, but neither intraoperative bleeding (P = 0.9704) nor the complete resolution rate (P = 0.9681) differed significantly (Table 2).
| Qualified | Non-qualified | P value | |
| Number of patients | 34 | 19 | |
| Operation duration (minutes) | 324.5 (242-483) | 390.0 (253-512) | 0.0314 |
| Blood loss (mL) | 25.5 (1-160) | 23.0 (3-122) | 0.9704 |
| Complete release from jaundice (case) | 27 (79.4%) | 15 (78.9%) | 0.9681 |
Our study, a comparison of 66 OpenPE cases with 53 LapPE cases, indicated no significant difference in native liver survival rates. In addition, although the LapPE procedure was longer than the Open-PE procedure, less blood loss and more favorable postoperative recovery, including shorter time to resume oral intake and shorter time to drain removal, were observed after LapPE than after Open-PE. The majority of earlier comparisons of the surgical outcomes after Open-PE and Lap-PE have indicated the superiority of OpenPE over LapPE[3,4,6,7,10]. On the basis of these results, LapPE is no longer performed in some institutions[10]. Conversely, Ji et al[11] reported a higher native liver survival rate after Lap-PE than after Open-PE in their shortterm assessment up to 3 years after the operation. A recent metaanalysis showed no significant difference in native liver survival rates between OpenPE and LapPE, and assessments in 2016 and after indicated a significantly higher rate of complete resolution of jaundice in the Lap-PE group than in the Open-PE group in the early phase[12]. However, Lap-PE outcomes were reported in only a single study, that of Ji et al[13], which had a sample size of > 50 and was performed at a single institution; the rarity of BA has limited study sample sizes. Ji et al[13] reported no significant difference in short and mediumterm outcomes after LapPE and OpenPE performed by skilled surgeons. In no study thus far have the surgical outcomes of LapPE and OpenPE been compared for a reasonably adequate sample size of > 50 cases.
The jaundicefree native liver survival rates after OpenPE for the treatment of BA have not changed for over 20 years, and 35%–60% of patients have eventually required LTx[1,2]. In a previous study, because Lap-PE produced fewer adhesions, the time until completion of hepatectomy and the duration of hospital stay were significantly shorter for patients who underwent liver transplantation after Lap-PE than for those who underwent Open-PE. Patients who underwent Lap-PE also tended to have less bleeding. These results suggested that Lap-PE before liver transplantation is advantageous[14]. Thus, if native liver survival rates are similar between LapPE and OpenPE, Lap-PE may be the more optimal option with greater advantage if LTx is eventually needed.
In this study, we compared the outcomes of surgeries performed from 2003 to 2020 between the OpenPE and LapPE groups. There was a significant difference in the patient age at the time of surgery between the two groups. This statistically significant difference can be explained by the difference in the year when the patients received either type of PE. Since 2011, stool color information has been added to the maternal handbooks in Japan for early detection of BA. This addition has enabled the mothers to visit hospitals earlier. We have applied LapPE as a standard procedure for the treatment of BA at our institution since December 2013; thus, LapPE has been performed for all BA cases since then, resulting in significantly younger age at the time of operation in the LapPE group than in the OpenPE group, which could be a potential confounding bias. However, according to a study of 3160 BA patients in Japan, the patient age at surgery is not a relevant confounding factor for surgical outcomes up to the age of 80 d[15]. Based on this published information, we performed an additional due diligence to compare the native liver survival rates between 47 patients in the Lap-PE group and 52 patients in the Open-PE group after excluding 20 patients who received PE at age ≥ 80 d, with similar results (P = 0.1516). The relationship between the timing of surgery and outcome has been studied, and the optimal age is still under debate[16-19]. Some authors have reported that the results are not good at 30–45 d of age. BA is a rare disease; thus, the number of cases is small, and because age is not correlated with surgical outcome, it is difficult to compare outcomes statistically when age is a confounding factor.
According to a report by Yang et al[13], surgeons need to maintain much higher technical skills for LapPE surgery than for OpenPE and require extensive experience with ≥ 50 surgeries. At our institution, we have not limited surgeons on the basis of their experience. In the present study, the surgery was significantly shorter when it was performed by qualified surgeons, which suggest that the time varies greatly depending on the skill of the surgeon. However, there was no statistically significant association between surgical operating time and surgical outcomes. Surgical outcomes were also not associated with the number of PE surgeries that a surgeon had previously performed. We have been making an effort to share the information on LapPE technical skills and surgical findings with all surgeons involved in PE surgeries at our institution. Thus, we believe that surgical outcomes were not affected by the experience of surgeons at our institution. This belief can be explained by the fact that younger surgeons can develop their skills through shared insights obtained during operations even though they are not assigned as the primary surgeons; thus, they may develop the knowledge and skills that can lead to surgical outcomes similar to those of more experienced surgeons. Pediatric surgeons need to perform surgeries for various rare pediatric diseases. Establishing surgical procedures enabling consistently favorable outcomes irrespective of the experience of surgeons should be a critical goal; therefore, LapPE is considered to be an adequate surgical procedure superior to conventional surgery.
This study has some limitations. This was a retrospective study, which could possibly introduce selection bias. Since LapPE has been introduced relatively recently, the followup period was limited, precluding the capability to evaluate potential longterm complications. The rate of complications did not differ significantly, but long-term survival rates may differ. Therefore, further studies with a larger study size, longterm follow-up, and thorough evaluations are warranted.
Complete resolution of jaundice was observed in 68.2% of patients who underwent Open-PE and 79.3% of those who underwent Lap-PE, but the difference was not statistically significant. Although the surgical operating time was longer, the lower blood loss and more favorable postsurgical recovery (shorter time to resume oral intake and time to drain removal as well as less postsurgical adhesion) were significant advantages of Lap-PE vs OpenPE. There was no significant difference in native liver survival rates or shortterm surgical outcomes between LapPE and OpenPE. Therefore, our study results support the efficacy of Lap-PE as a standard therapy.
The application of laparoscopic portoenterostomy (LapPE) as a treatment option for BA remains controversial.
Management after BA surgeries is complicated and requires a centralized procedure for consistency. Thus, it is considered important to perform a largescale assessment at a single facility with a centralized management procedure for adequate comparison in the outcomes between LapPE and OpenPE.
The aim of this study was to compare the outcomes of Lap-PE with those of laparotomy (Open-PE) at our single institution.
The surgical outcomes of PE were retrospectively analyzed for patients with a non-correctable type of BA from 2003 to 2020.
Throughout the assessment period, 119 patients received PE for BA treatment, including 66 Open-PE and 53 Lap-PE cases. Although the operation duration was longer (medians: for Open-PE, 242 min; for Lap-PE, 341 min; P < 0.001), blood loss was considerably less (medians: for Open-PE, 52 mL; for Lap-PE, 24 mL; P < 0.001) in the Lap-PE group than in the Open-PE group. Native liver survival rates were > 80% for both groups for the first half year post surgery, followed by a gradual decrease with time; there were no statistically significant differences in the native liver survival rates for any durations assessed.
Lap-PE could be a standard therapy for BA.
The rate of complications did not differ significantly, but long-term survival rates may differ. Therefore, further studies with a larger study size, longterm follow-up, and thorough evaluations are warranted.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Gunadi, Joshi D, Peruhova M S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Ibrahim M, Miyano T, Ohi R, Saeki M, Shiraki K, Tanaka K, Kamiyama T, Nio M. Japanese Biliary Atresia Registry, 1989 to 1994. Tohoku J Exp Med. 1997;181:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Nio M, Sasaki H, Wada M, Kazama T, Nishi K, Tanaka H. Impact of age at Kasai operation on short- and long-term outcomes of type III biliary atresia at a single institution. J Pediatr Surg. 2010;45:2361-2363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Hussain MH, Alizai N, Patel B. Outcomes of laparoscopic Kasai portoenterostomy for biliary atresia: A systematic review. J Pediatr Surg. 2017;52:264-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 4. | Lishuang M, Zhen C, Guoliang Q, Zhen Z, Chen W, Long L, Shuli L. Laparoscopic portoenterostomy versus open portoenterostomy for the treatment of biliary atresia: a systematic review and meta-analysis of comparative studies. Pediatr Surg Int. 2015;31:261-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Chan KW, Lee KH, Tsui SY, Wong YS, Pang KY, Mou JW, Tam YH. Laparoscopic versus open Kasai portoenterostomy in infant with biliary atresia: a retrospective review on the 5-year native liver survival. Pediatr Surg Int. 2012;28:1109-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Ure BM, Kuebler JF, Schukfeh N, Engelmann C, Dingemann J, Petersen C. Survival with the native liver after laparoscopic versus conventional kasai portoenterostomy in infants with biliary atresia: a prospective trial. Ann Surg. 2011;253:826-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Sun X, Diao M, Wu X, Cheng W, Ye M, Li L. A prospective study comparing laparoscopic and conventional Kasai portoenterostomy in children with biliary atresia. J Pediatr Surg. 2016;51:374-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Lampela H, Ritvanen A, Kosola S, Koivusalo A, Rintala R, Jalanko H, Pakarinen M. National centralization of biliary atresia care to an assigned multidisciplinary team provides high-quality outcomes. Scand J Gastroenterol. 2012;47:99-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 9. | Madadi-Sanjani O, Fortmann D, Rolle U, Rodeck B, Sturm E, Pfister ED, Kuebler JF, Baumann U, Schmittenbecher P, Petersen C. Centralization of Biliary Atresia: Has Germany Learned Its Lessons? Eur J Pediatr Surg. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Chan KW, Lee KH, Wong HY, Tsui SY, Wong YS, Pang KY, Mou JW, Tam YH. From laparoscopic to open Kasai portoenterostomy: the outcome after reintroduction of open Kasai portoenterostomy in infant with biliary atresia. Pediatr Surg Int. 2014;30:605-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Ji Y, Yang K, Zhang X, Jin S, Jiang X, Chen S, Xu Z. The short-term outcome of modified laparoscopic Kasai portoenterostomy for biliary atresia. Surg Endosc. 2021;35:1429-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Li Y, Gan J, Wang C, Xu Z, Zhao Y, Ji Y. Comparison of laparoscopic portoenterostomy and open portoenterostomy for the treatment of biliary atresia. Surg Endosc. 2019;33:3143-3152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Ji Y, Yang K, Zhang X, Chen S, Xu Z. Learning curve of laparoscopic Kasai portoenterostomy for biliary atresia: report of 100 cases. BMC Surg. 2018;18:107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Shirota C, Murase N, Tanaka Y, Ogura Y, Nakatochi M, Kamei H, Kurata N, Hinoki A, Tainaka T, Sumida W, Yokota K, Makita S, Oshima K, Uchida H. Laparoscopic Kasai portoenterostomy is advantageous over open Kasai portoenterostomy in subsequent liver transplantation. Surg Endosc. 2020;34:3375-3381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Nio M. Japanese Biliary Atresia Registry. Pediatr Surg Int. 2017;33:1319-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 16. | Okubo R, Nio M, Sasaki H; Japanese Biliary Atresia Society. Impacts of Early Kasai Portoenterostomy on Short-Term and Long-Term Outcomes of Biliary Atresia. Hepatol Commun. 2021;5:234-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 17. | Fawaz R, Baumann U, Ekong U, Fischler B, Hadzic N, Mack CL, McLin VA, Molleston JP, Neimark E, Ng VL, Karpen SJ. Guideline for the Evaluation of Cholestatic Jaundice in Infants: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2017;64:154-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 314] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 18. | Tessier MEM, Shneider BL. 60 Days in Biliary Atresia: A Historical Dogma Challenged. Clin Liver Dis (Hoboken). 2020;15:S3-S7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Sasaki H, Tanaka H, Wada M, Kazama T, Nakamura M, Kudo H, Okubo R, Sakurai T, Nio M. Analysis of the prognostic factors of long-term native liver survival in survivors of biliary atresia. Pediatr Surg Int. 2016;32:839-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |