Published online May 27, 2021. doi: 10.4240/wjgs.v13.i5.452
Peer-review started: November 2, 2020
First decision: November 30, 2020
Revised: December 10, 2020
Accepted: April 25, 2021
Article in press: April 25, 2021
Published online: May 27, 2021
Processing time: 199 Days and 14.7 Hours
Laparoscopic sleeve gastrectomy (LSG) is the most common bariatric surgical procedure. LSG is a restrictive procedure and in this operation stomach volume is greatly reduced. When the details of the procedure are examined, it is seen that there are many different methods surgery.
To analyze approaches of surgeons performing LSG.
A questionnaire consist of 44 questions was sent by e-mail to the surgeons performing bariatric surgery. Approaches of surgery about preoperative period, surgical techniques and postoperative period was questioned.
Different approaches about antibiotic prophylaxis, stapler line reinforcement utilization, application of intraoperative and postoperative leakage test, approach to the crus and hiatal hernia repair were detected. It was observed that a few partipicipants applied contrary to the guidelines of antibiotic prophlaxis and thromboembolism prophylaxis. Approaches about other subjects were generally similar.
In this study, approaches about LSG that most common bariatric surgical procedure in our country was learned. According to these results, knowing the approaches in our country will be beneficial in terms of determining the training programs in bariatric surgery, improving surgical results and reducing the complications.
Core Tip: The goal of laparoscopic sleeve gastrectomy is to limit the amount of food taken by reducing the stomach volume. When the surgical applications are examined, it is seen that although the surgical technique is similar in general terms, when the details of the technique are considered and the pre- and post-surgical applications are evaluated, there are very different applications. The aim of this study was to evaluate the clinical applications of laparoscopic sleeve gastrectomy surgeons.
- Citation: Mayir B. Practices concerning sleeve gastrectomy in Turkey: A survey of surgeons. World J Gastrointest Surg 2021; 13(5): 452-460
- URL: https://www.wjgnet.com/1948-9366/full/v13/i5/452.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i5.452
Obesity is an increasingly common health problem. According to 2012 data, the obesity rate in our country has been reported as 17.2%[1]. Today, surgical interventions are widely used in the treatment of morbid obesity. To date, various types of surgery have been described, including restrictive, malabsorptive or combined types. Among these different types of surgery, laparoscopic sleeve gastrectomy (LSG) is a restrictive operation and is considered an effective and safe procedure in the treatment of morbid obesity[2]. Since 2012, the American metabolic and bariatric surgery association has accepted LSG as the primary bariatric surgical procedure[3]. LSG is the most commonly performed bariatric surgical procedures in today in the world[4]. The goal of LSG is to limit the amount of food taken by reducing the stomach volume. When the surgical applications are examined, it is seen that although the surgical technique is similar in general terms, when the details of the technique are considered and the pre- and post-surgical applications are evaluated, there are very different applications[5]. The aim of this study was to evaluate the clinical applications of LSG surgeons in Turkey.
The study was designed as a questionnaire study. We gather names of doctors interested in bariatric surgery from the list of members of the obesity related associations in Turkey announced on the internet, authors of articles published in PubMed from Turkey regarding bariatric surgery, a variety of news and ads on social media. E-mail addresses of these names of surgeons were tried to be found on the internet. A questionnaire of 44 questions was sent to surgeons whose e-mail address could be reached. The questionnaire included descriptive questions about the demographic characteristics and surgical experience of the surgeons, examinations and applications before LSG, surgical techniques, postoperative follow-up and treatment process. Surgeons stating that they perform LSG at questionnaire were included in the study.
All results were recorded with SPSS 22 (IBM Corporation, Chicago, IL, United States) program and descriptive statistical calculations were performed.
Three hundred and sixty-six surgeons who were thought to be interested in bariatric surgery were sent a questionnaire. 63 (17.2%) of these surgeons answered the questionnaire.
Demographic characteristics and surgical experience of surgeons.
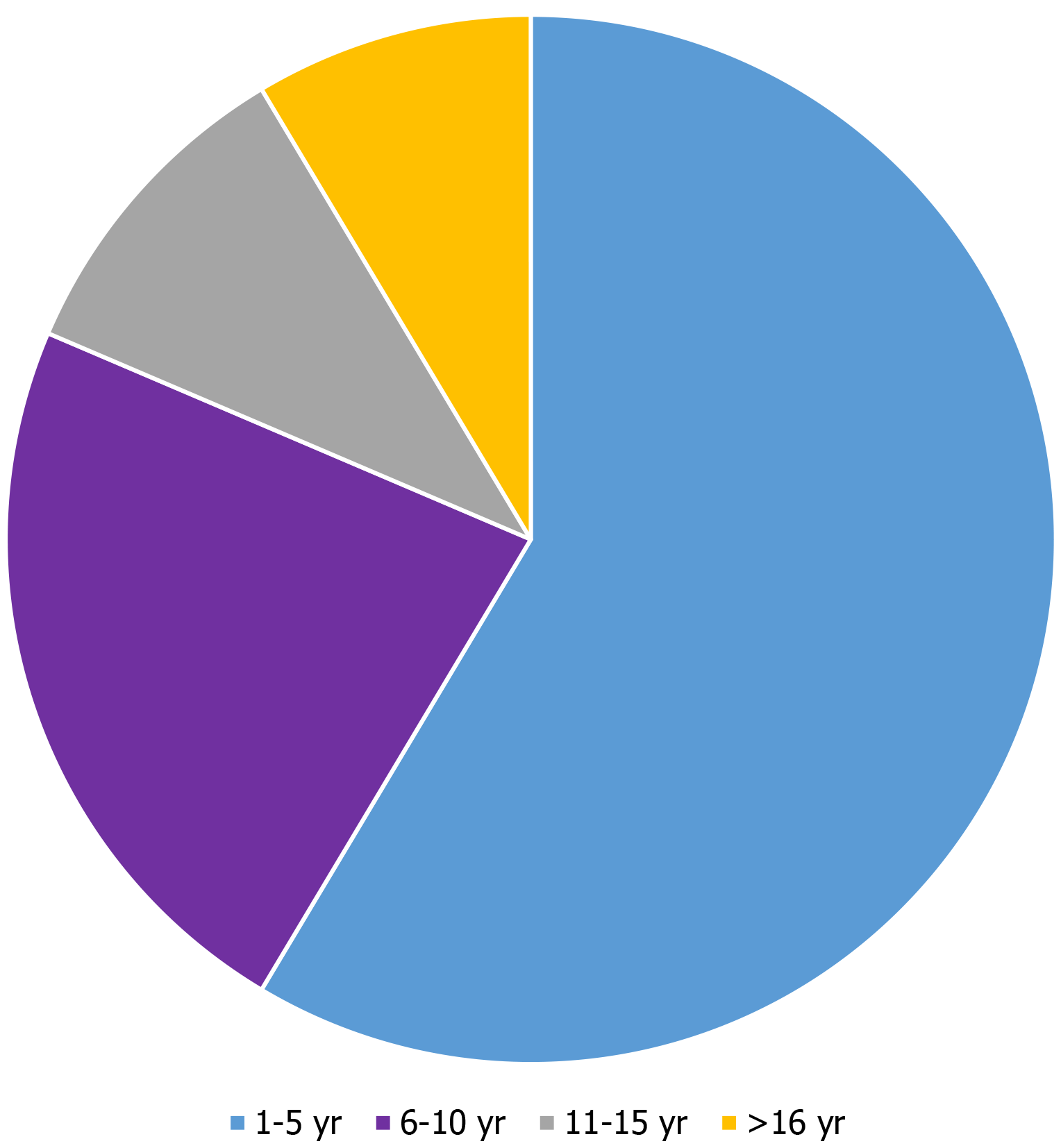
All participants were male. More than half of the participants performed operations at private health institutions (Table 1). When the expertise time of the physician's was examined, it was seen that 51% of the physicians were work as general surgeon for 6-11 years. It was seen that 51% of the physicians have been interested in bariatric surgery for 2-5 years. Only 16% of the participants are performing bariatric surgical procedures for more than 10 years (Figure 1).
| Institution | n | % |
| Private hospital | 26 | 41.3 |
| Training and research hospital | 15 | 23.8 |
| University hospital | 14 | 22.2 |
| University hospital/private hospital | 5 | 7.9 |
| Private clinic | 2 | 3.2 |
| State hospital | 1 | 1.6 |
While 10% of the participants reported that they could only perform sleeve gastrectomy, 90% reported that they could perform gastric bypass procedures in addition to LSG, and 25% reported that they could perform biliopancreatic diversion in addition to other procedures. 79% of the participants reported that they could perform revision bariatric surgical procedures. When amount of bariatric surgical procedures per month was considered, it was seen that 36% of the participants perform 1-5 operation per month and 21% perform more than 20 bariatric surgical procedures per month. 79% of the participants reported that they can perform endoscopic diagnostic procedures, and 60% reported that they perform stent or similar endoscopic procedures for treatment.
It was reported that at 13% of hospitals where participants work, stent or similar therapeutic endoscopic procedures could not be performed for patients in whom leakage was observed. 37.5% of these hospitals were private hospitals, 37.5% were education and research hospitals and 25% were university hospitals.
Preoperatively, 92% of the participants referred their patients to an internal medicine doctor or endocrinologist, 90% made routine upper gastrointestinal endoscopic examination of patients, 87% sent patients to routine abdominal ultrasonographic examination, 87% took psychiatric consultation and 63% made dexamethasone suppression test routinely.
It was observed that 52% of the participants recommend routine diet in the last week or the last few days before surgery, 87% applied low molecular weight heparin (LMWH) prophylaxis preoperatively, and 93% had wear preoperative socks for varicosis to their patients.
Presence of hiatal hernia is one of the factors affecting surgical approach at bariatric surgical interventions. In this group of patients, 60% of the participants added crus repair to LSG, 27% preferred gastric bypass procedures and 10% reported that only LSG was applied. One surgeon who stated that he can perform only sleeve gastrectomy as bariatric procedure reported that he referred patient to another center in the presence of hiatal hernia.
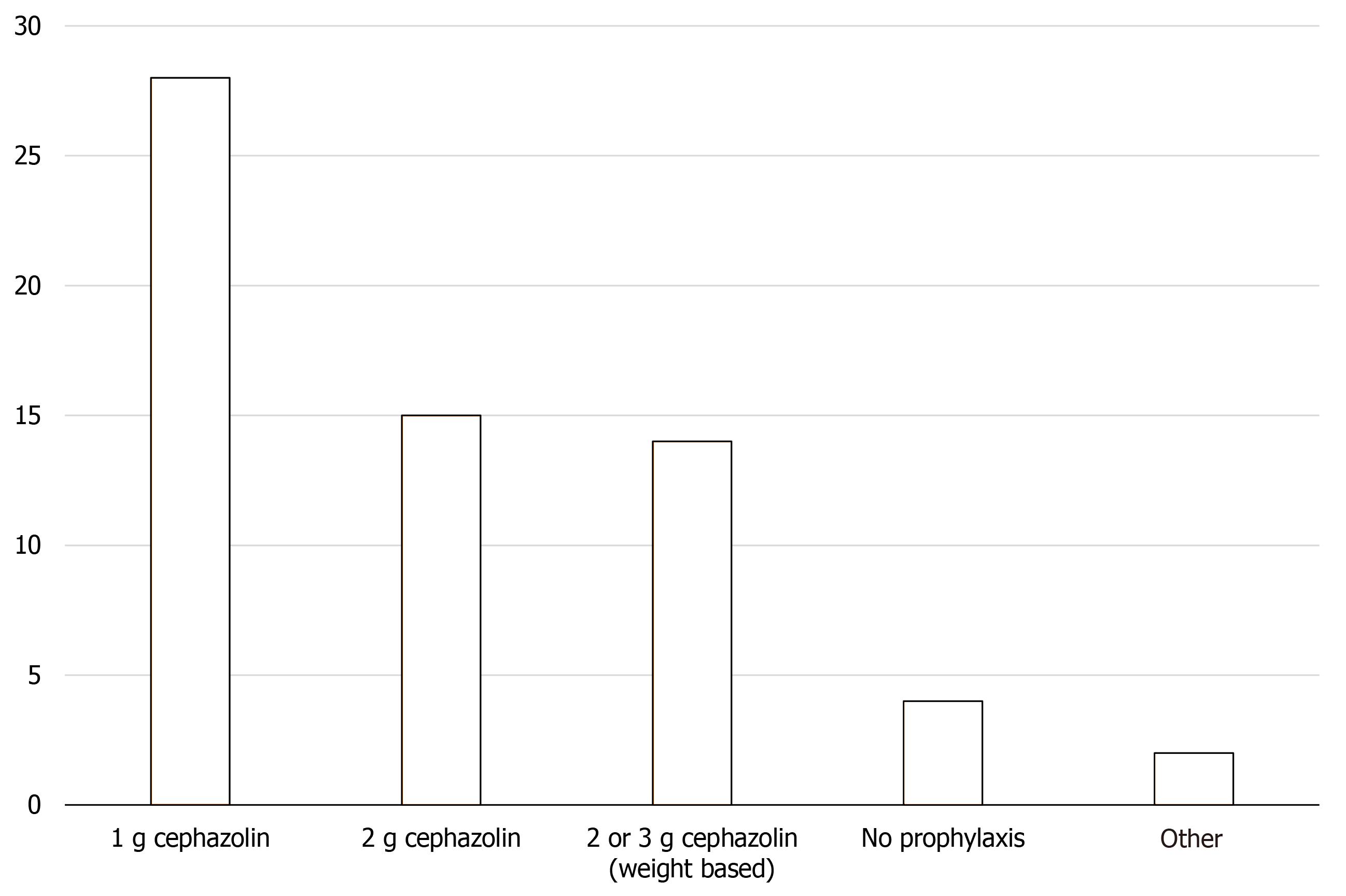
Ninety percent of the participants reported that they use cefazolin for preoperative antibiotic prophylaxis while 6% don’t use antibiotic prophylaxis (Figure 2).
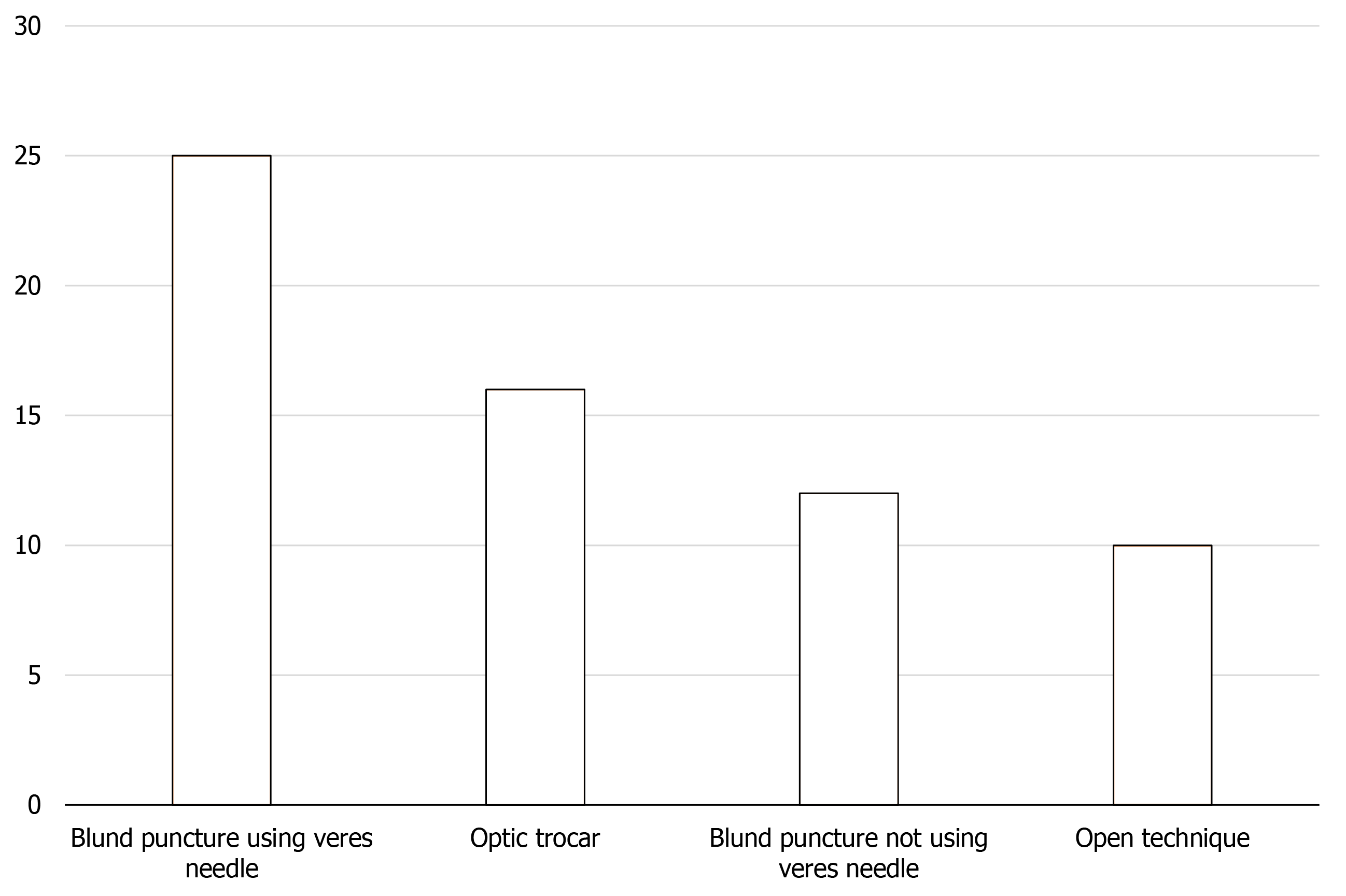
Although 43% of the participants think that the ideal method for first trochar insertions is the use of optical trocar, only 25% of perform the first trocar insertion with the optical trocar. The most common method for first trocar insertion was the introduction of a trocar after insufflation with a veres needle (40%) (Figure 3).
While 94% of the participants performed the surgery by 4 or 5 trocars, 81% reported that they used liver retractor routinely.
Eighty-three percent of participants reported that CO2 insufflation pressure was determined to be 12-15 mmHg, 10% of participants reported upper than 15 mm Hg, and 3% of participants reported lower than 12 mmHg.
Forty-eight percent of the participants reported that they routinely evaluate diaphragmatic cruses during surgery.
Some surgeons use intravenous hyoscine-n-butylbromide which they thought provides easier surgery technique and helps to remove more gastric tissue by losing stomach. It was seen that 52% of the participants did not never use intravenous hyoscine-n-butylbromide and 17% of them used it routinely.
The most commonly used bougie diameter was 36 F (37%) followed by, 39 F (24%) and 38 F (17%). 16% of the participants reported that they use 32 F and smaller diameter bougie.
There are many products to reinforce the stapler line for reducing the risk of leakage from the stapler line. In our study, the majority of the participants (56%) stated that they did not use any stapler line reinforcing products. 29% of the participants stated that they suture the stapler line in order to strengthen the stapler line and 11% of them apply fibrin tissue adhesive.
Seventy-one percent of the participants reported that they routinely performed intraoperative leakage test with methylene blue, 19% reported that they performed intraoperative leakage test with both methylene blue and air, and 3% reported that they performed intraoperative leakage test with only air.
Thirty-two percent of the participants reported that they sutured the fascia at all trocar incision of 10 mm and above, 29% sutured the fascia at the trocar region where only the stomach was taken out of the abdomen, 24% sutured the fascia at all trocar incisions 12 mm and above, and 16% reported that they don’t suture fascia at any trocar regions.
While 83% of the participants reported that they routinely place drains after surgery, 46% reported that they remove the drain within 3-4 d, 33% remove it within 1-2 d, and 5% remove it one week and after.
All participants reported that they mobilize patients within the first 24 h, 2% mobilize them within the first 1-4 h, and 60% mobilize them within 5-8 h.
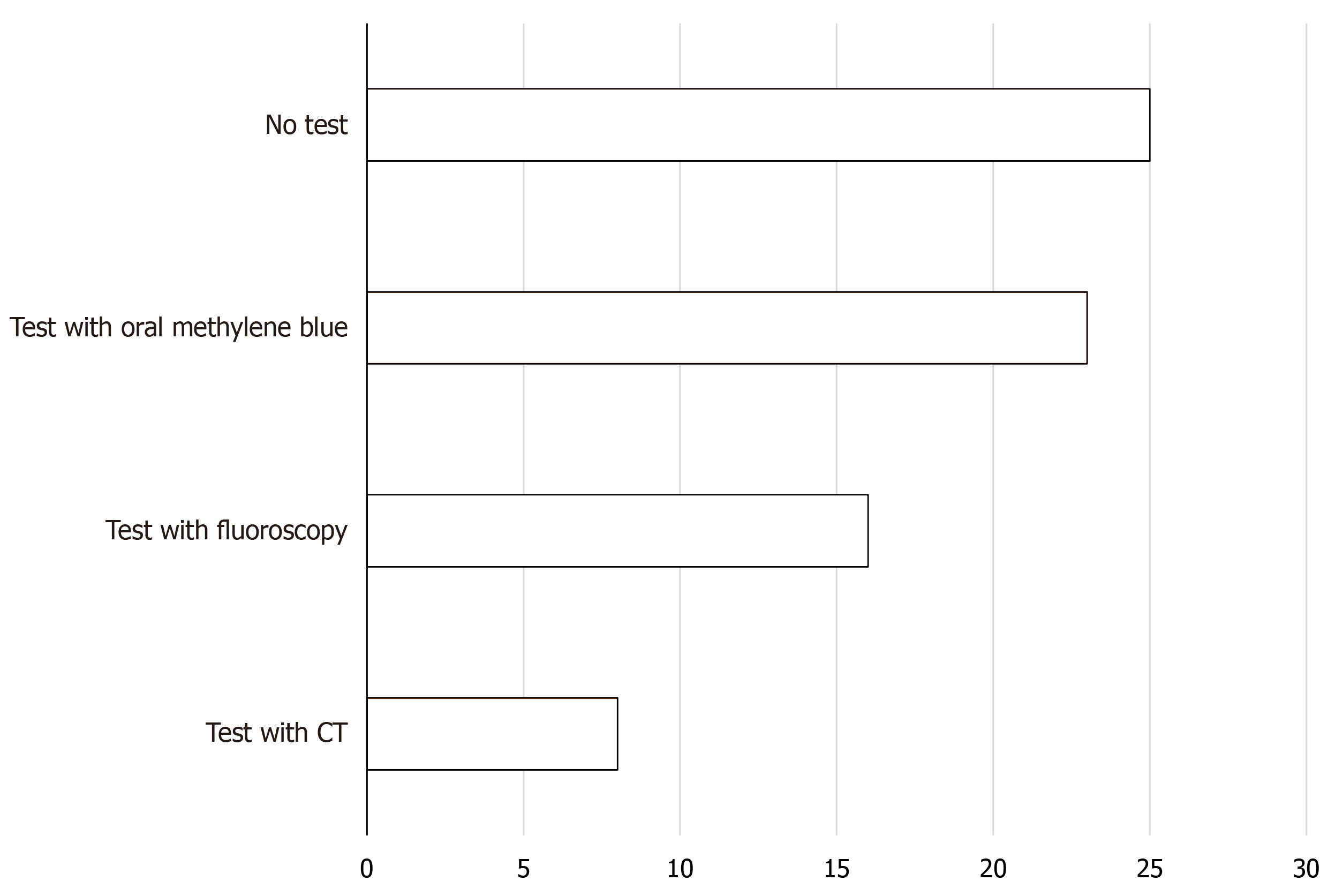
Forty percent of the participants stated that they did not perform postoperative leakage test, 22% made leakage test with oral methylene blue, 16% made leakage test with flouroscopy, 8% made leakage test with computerized tomography (CT), and 10% made leakage test with oral methylene blue and flouroscopy together, and 5% reported leakage test with oral methylene blue and CT together (Figure 4).
Forty one percent of the participants stated that they allow oral fluid intake in the first 24 h and 35% within 24-48 h. 52% of the participants stated that they discharge the patients on the 3rd day and 24% on the 2nd day.
Fifty two percent of the participants reported they follow-up postoperative hemogram levels routinely.
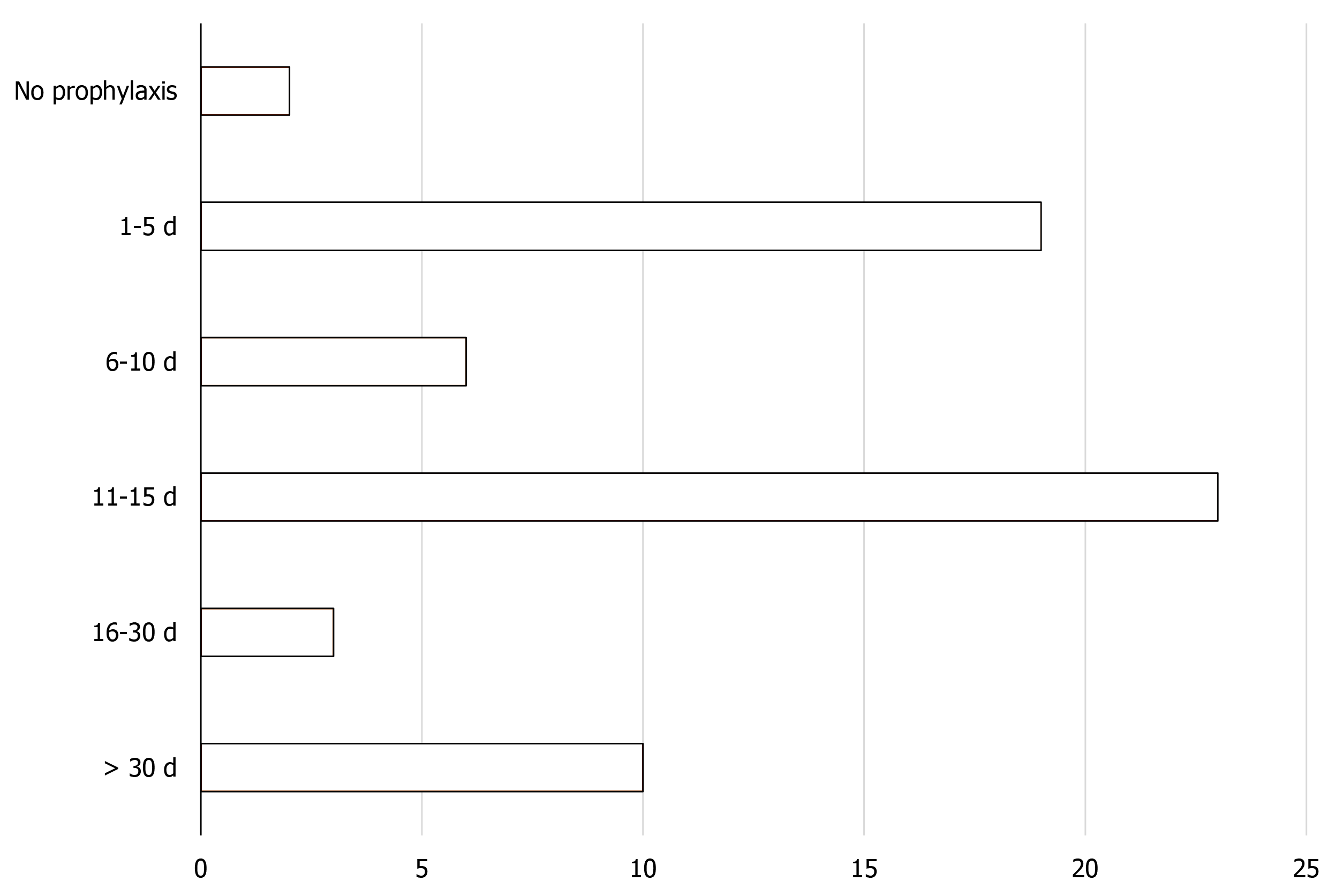
Sixteen percent of the participants reported that they did not perform routine LMWH prophylaxis for their patients after discharge (Figure 5).
While 75% of the participants refer their patients to the dietician while being discharge, 21% reported that they did not send their patients to the dietician and give recommendations by themselves and 4% of the participants did not refer their patients to the dietician.
Seventy-six percent of the participants stated that they routinely recommended multivitamin supplementation and 49% recommend non-dietary protein supplementation during discharge, 87% of the participants stated that they record patient data prospectively.
Bariatric surgery is currently considered to efficiently produce long-term weight loss, improve comorbidities and improve quality of life for the morbidly obese patient. Although consensus decisions have been reported in many subjects about to LSG, it is seen that there are no standards in some subjects and different applications performed in clinical practice. With this study, approaches of the surgeons performing LSG has learned and it is presented that there are different practices in some subjects related to LSG.
When the participant profile was examined in our study, it was seen that approximately half of the participants were 6-11 years general surgery specialist. These results indicate that surgeons with a certain experience interest in bariatric surgery rather than new specialists. In addition, when the participants' time to deal with bariatric surgery and the number of case per month and the types of primary or revision surgery considered, it is seen that a significant part of the participants have completed the learning curve and can be considered as experienced.
In our study, it was observed that preoperative evaluation is similar in general, but there were different approaches about applying to dexamethasone suppression test. When the literature is examined, it is seen that the necessity of Dexamethasone suppression test is controversial likewise in our study[6,7].
As there are standard indications for bariatric surgery according to World Health Organization, question about surgical indications did not asked to the surgeons, but because of being a controversial issue, there was a question about the approach in the presence of hiatal hernia in a patient undergoing LSG. It is generally accepted that LSG increases gastroesophageal reflux and that if the patient has hiatal hernia before LSG, reflux symptoms will worsen in the postoperative period[8,9]. In the presence of hiatal hernia, simultaneous diaphragmatic crus repairment or performing gastric bypass procedures are considered to be effective in preventing gastroesophageal reflux[10,11]. Although a significant portion of the participants have a tendency in this direction, 10% of the participants perform only LSG in presence of hiatal hernia indicating that the differences about approach in this subject in our country is likewise the world.
Although application of preoperative antibiotic prophylaxis is determined according to the guidelines, in our study it was observed that different applications were made in this regard. According to current guidelines, 2 or 3 g of cefazolin by weight was applied by 21% of the participants[12]. According to this result, it is necessary that current antibiotic prophylaxis applications should be reviewed by surgeons.
Obese individuals are at high risk group for thromboemboli. Complication about thromboembolism account for 50% of mortality after bariatric surgical procedures[13]. Many guidelines recommend preoperative mechanical prophylaxis and LMWH prophylaxis and postoperative LMWH prophylaxis in these patients[14]. In our study, in accordance with the suggestion of the guidelines, a significant number of participants performed prophylaxis with LMWH and stocking for varicosis for thromboembolism to their patients. However 13% of participants don’t perform preoperatively LMWH prophylaxis and 16% don’t advise LMWH prescribe at discharge, which was considered as important defect.
One of the most mortal complication after LSG is stapler line leakage[15]. To reduce the leakage rate, various applications are made to reinforce the stapler line. Although there are many new articles about this suject, effectiveness of stapler line reinforcing applications in meta-analyzes is not certain[16]. In the literature, usage of stapler line booster up to 80% has been reported[17]. The 44% of usage of stapler line booster rate in our country is below this rate. Although it has been observed that different applications have been tried to strengthen the stapler line in our country, the most common method was suturation of the stapler line.
One of the controversial issues regarding LSG is whether or not to perform leakage tests during or after surgery. Many studies have shown that leakage tests are ineffective, in some studies leakage risk is found to be increased due to testing and it is stated that routine testing is not necessary[18]. However, when the literature is examined, it is seen that leakage tests are still widely applied[19]. A similar result is found in our study and it is observed that the majority of the participants perform leakage tests routinely, only 26% did not perform leakage tests during the operation and 39% did not perform leakage tests post operatively.
Nowadays, by application of ERAS protocols in many surgical field significant decrease in morbidity and mortality was achieved[20]. The nutritional part of these protocols generally promotes the beginning of oral intake in the early period after gastrointestinal surgery. In the ERAS bariatric surgery guideline, it is stated that feeding with clear fluids can be started within a few hours after surgery. In the literature, it is generally reported that feeding with clear liquid can be started within the first 24 h after LSG. In our study, however, only 41% of the participants started oral feeding in the first 24 h.
The study has some limitations. First of all, this is a questionnaire study so results may not be as reliable as prospective or randomized studies. Another limitation is the small number of participants. 366 physicians were sent an e-mail questionnaire for the study, but 17% answered the questionnaire. If we look at the reasons for this; a portion of the mailing list consisted of corporate emails, and these corporate emails may not use actively. In addition, person is likely to use more than one e-mail and may questionnaire be sent to inactive e-mail address. Another reason may be that physicians receiving e-mails don’t want to participate the study. Some physicians have replied that they do not want to participate without an excuse. Although the number of participants is few, the participant profile is consisting of surgeons having experience in bariatric surgery that reinforces the results.
This study is first in our country about approaches of surgeons before, during and after LSG. Our study exactly demonstrated the attitudes of surgeons performing LSG. According to the results of the study, it is seen that approaches are generally appropriate with the guidelines, but it is seen in few subjects there are some applications not matching with general recommendations and guidelines. According to these results, it is important to inform surgeons through scientific meetings concerning up-to-date information on bariatric surgical procedures. In addition, similar studies on bariatric procedures other than LSG could make contribution to the literature.
Laparoscopic sleeve gastrectomy (LSG) is the most commonly performed bariatric surgical procedures in today in the world. When the surgical applications are examined, it is seen that although the surgical technique is similar in general terms, when the details of the technique are considered and the pre- and post-surgical applications are evaluated, there are very different applications.
The aim of this study was to evaluate the clinical applications of LSG surgeons in Turkey.
Knowing the different approaches will be benefical in terms of determining the training programs in bariatric surgery, improving surgical results and reducing the complications.
A questionnaire consist of 44 questions was sent by e-mail to the surgeons performing bariatric surgery. Approaches of surgery about preoperative period, surgical techniques and postoperative period was questioned.
Different approaches about antibiotic prophylaxis, stapler line reinforcement utilization, application of intraoperative and postoperative leakage test, approach to the crus and hiatal hernia repair were detected. It was observed that a few partipicipants applied contrary to the guidelines of antibiotic prophlaxis and thromboembolism prophylaxis. Approaches about other subjects were generally similar.
In this study, approaches about LSG that most common bariatric surgical procedure in our country was learned.
Approaches of the surgeons performing LSG has learned and it is presented that there are different practices in some subjects related to LSG.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tartaglia N S-Editor: Zhang L L-Editor: A P-Editor: Li JH
| 1. | TUİK Türkiye Saglik Arastirmasi 2012. Available from: http://www.tuik.gov.tr/PreHaberBultenleri.do?id=13490. |
| 2. | Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, Aminian A, Pothier CE, Kim ES, Nissen SE, Kashyap SR; STAMPEDE Investigators. Bariatric surgery vs intensive medical therapy for diabetes--3-year outcomes. N Engl J Med. 2014;370:2002-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1202] [Cited by in RCA: 1179] [Article Influence: 107.2] [Reference Citation Analysis (0)] |
| 3. | ASMBS Clinical Issues Committee. Updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis. 2012;8:e21-e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 116] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes Surg. 2018;28:3783-3794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 791] [Cited by in RCA: 727] [Article Influence: 103.9] [Reference Citation Analysis (0)] |
| 5. | Hans PK, Guan W, Lin S, Liang H. Long-term outcome of laparoscopic sleeve gastrectomy from a single center in mainland China. Asian J Surg. 2018;41:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Mechanick JI, Youdim A, Jones DB, Timothy Garvey W, Hurley DL, Molly McMahon M, Heinberg LJ, Kushner R, Adams TD, Shikora S, Dixon JB, Brethauer S. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9:159-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 446] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 7. | Alhambra Expósito MR, Tenorio Jiménez C, Molina Puerta MJ, Manzano García G, Prior Sánchez I, Muñoz Jiménez C, Gálvez Moreno MÁ. [Screening for Cushing's syndrome in obese patients; is it really necessary? Nutr Hosp. 2014;29:1020-1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Burgerhart JS, Schotborgh CA, Schoon EJ, Smulders JF, van de Meeberg PC, Siersema PD, Smout AJ. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes Surg. 2014;24:1436-1441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 9. | Carter PR, LeBlanc KA, Hausmann MG, Kleinpeter KP, deBarros SN, Jones SM. Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Ece I, Yilmaz H, Yormaz S, Çolak B, Acar F, Alptekin H, Sahin M. Comparison of mid-term clinical outcomes of laparoscopic partial cystectomy vs conventional partial cystectomy for the treatment of hepatic hydatid cyst. J Minim Access Surg. 2017;13:296-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Raj PP, Misra S, Bhattacharya S, Kumar SS, Kumar TSR, Khan MJ, Palanivelu C. Lower oesophageal peptic stricture after laparoscopic sleeve gastrectomy: World's first case report. J Minim Access Surg. 2020;16:282-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain D, Steinberg JP, Weinstein RA; American Society of Health-System Pharmacists (ASHP); Infectious Diseases Society of America (IDSA); Surgical Infection Society (SIS); Society for Healthcare Epidemiology of America (SHEA). Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 2013;14:73-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 599] [Cited by in RCA: 766] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 13. | Overby DW, Kohn GP, Cahan MA, Galanko JA, Colton K, Moll S, Farrell TM. Prevalence of thrombophilias in patients presenting for bariatric surgery. Obes Surg. 2009;19:1278-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Aminian A, Andalib A, Khorgami Z, Cetin D, Burguera B, Bartholomew J, Brethauer SA, Schauer PR. Who Should Get Extended Thromboprophylaxis After Bariatric Surgery? Ann Surg. 2017;265:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 15. | Iossa A, Abdelgawad M, Watkins BM, Silecchia G. Leaks after laparoscopic sleeve gastrectomy: overview of pathogenesis and risk factors. Langenbecks Arch Surg. 2016;401:757-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Chen B, Kiriakopoulos A, Tsakayannis D, Wachtel MS, Linos D, Frezza EE. Reinforcement does not necessarily reduce the rate of staple line leaks after sleeve gastrectomy. A review of the literature and clinical experiences. Obes Surg. 2009;19:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 121] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Cunningham-Hill M, Mazzei M, Zhao H, Lu X, Edwards MA. The Impact of Staple Line Reinforcement Utilization on Bleeding and Leak Rates Following Sleeve Gastrectomy for Severe Obesity: a Propensity and Case-Control Matched Analysis. Obes Surg. 2019;29:2449-2463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Kim J, Azagury D, Eisenberg D, DeMaria E, Campos GM; American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11:739-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 145] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 19. | Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1001] [Cited by in RCA: 1014] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 20. | Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg. 2016;40:2065-2083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 359] [Article Influence: 44.9] [Reference Citation Analysis (0)] |