Published online Mar 27, 2021. doi: 10.4240/wjgs.v13.i3.315
Peer-review started: October 3, 2020
First decision: December 4, 2020
Revised: December 17, 2020
Accepted: March 7, 2021
Article in press: March 7, 2021
Published online: March 27, 2021
Processing time: 165 Days and 18.2 Hours
Primary extra-gastrointestinal stromal tumors (E-GIST) of the liver are rare. The clinical presentation may range from asymptomatic to bleeding or manifestations of mass effect. Oncologic surgery followed by adjuvant therapy with imatinib is the standard of care. However, under specific circumstances, a cytoreductive approach may represent a therapeutic option. We describe herein the case of an 84-year-old woman who presented with a tender, protruding epigastric mass. Abdominal computed tomography scan revealed a large, heterogeneous mass located across segments III, IV, V, and VIII of the liver. The initial approach was transarterial embolization of the tumor, which elicited no appreciable response. Considering the large size and central location of the tumor and the advanced age of the patient, non-anatomic complete resection was indicated. Due to substantial intraoperative bleeding and hemodynamic instability, only a near-complete resection could be achieved. Histopathology and immunohistochemical staining confirmed the diagnosis of primary E-GIST of the liver. Considering the risk/benefit ratio for therapeutic options, debulking surgery may represent a strategy to control pain and prolong survival.
Here, we present a case report of a patient diagnosed with E-GIST primary of the liver, which was indicated a cytoreductive surgery and adjuvant therapy with imatinib.
E-GIST primary of the liver is a rare conditional, the treatment is with systemic therapy and total resection surgery. However, a cytoreductive surgery will be necessary when a complete resection is no possible.
Core Tip: Extra-gastrointestinal stromal tumor (E-GIST) of the liver is a rare condition, but the clinical presentation and treatment is similar to GIST of digestive tract. We present herein a case of giant hepatic E-GIST in an oldest person already reported and treated by cytoreductive surgery. This case highlights because it contributes to discussion of treatment approach, such as, the management of large hepatic masses, especially in GIST, and patient who would not tolerate major surgical resections.
- Citation: Fernandes MR, Ghezzi CLA, Grezzana-Filho TJ, Feier FH, Leipnitz I, Chedid AD, Cerski CTS, Chedid MF, Kruel CRP. Giant hepatic extra-gastrointestinal stromal tumor treated with cytoreductive surgery and adjuvant systemic therapy: A case report and review of literature. World J Gastrointest Surg 2021; 13(3): 315-322
- URL: https://www.wjgnet.com/1948-9366/full/v13/i3/315.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i3.315
Gastrointestinal (GI) stromal tumors (GISTs) arise from the interstitial cells of Cajal, located in the GI mesenchyme[1,2]. However, GISTs have also been also encountered in other sites that lack these cells, including the mesentery, omentum, and abdominal wall, suggesting that pluripotent mesenchymal stem cells are responsible for the development of GISTs outside the GI tract[3]. GISTs are currently classified according to histopathological and immunohistochemical criteria, based on expression of the tyrosine kinase KIT (CD117, c-Kit) by tumor cells[4,5]. GISTs located outside the GI tract are appropriately known as extra-GIST (E-GIST), and represent 1% of all GISTs[6,7]. Herein, we report the management of a very large symptomatic E-GIST of the liver in an older adult.
An 84-year-old woman, Caucasian, was admitted to our hospital with persistent upper abdominal pain.
An 84-year-old woman, Caucasian, was admitted to our hospital with 3-mo history right hypochondrium and epigastric pain. There was no history of fever, jaundice, coluria and acholia or unintentional weight loss.
The patient had no history of hepatic or GI diseases, malignancy, or previous surgeries.
Physical examination revealed a painful, protruding epigastric mass.
Liver function tests were within normal range, hemogram (hemoglobin 7.2 and hematocrit 24.7) and hepatitis B, hepatitis C, and human immunodeficiency virus serology were negative. Ca 19-9 levels were elevated (220 U/mL), while serum α-fetoprotein, CA-125, and carcinoembryonic antigen were within normal limits
A GI workup including endoscopy and colonoscopy did not show any significant abnormality.
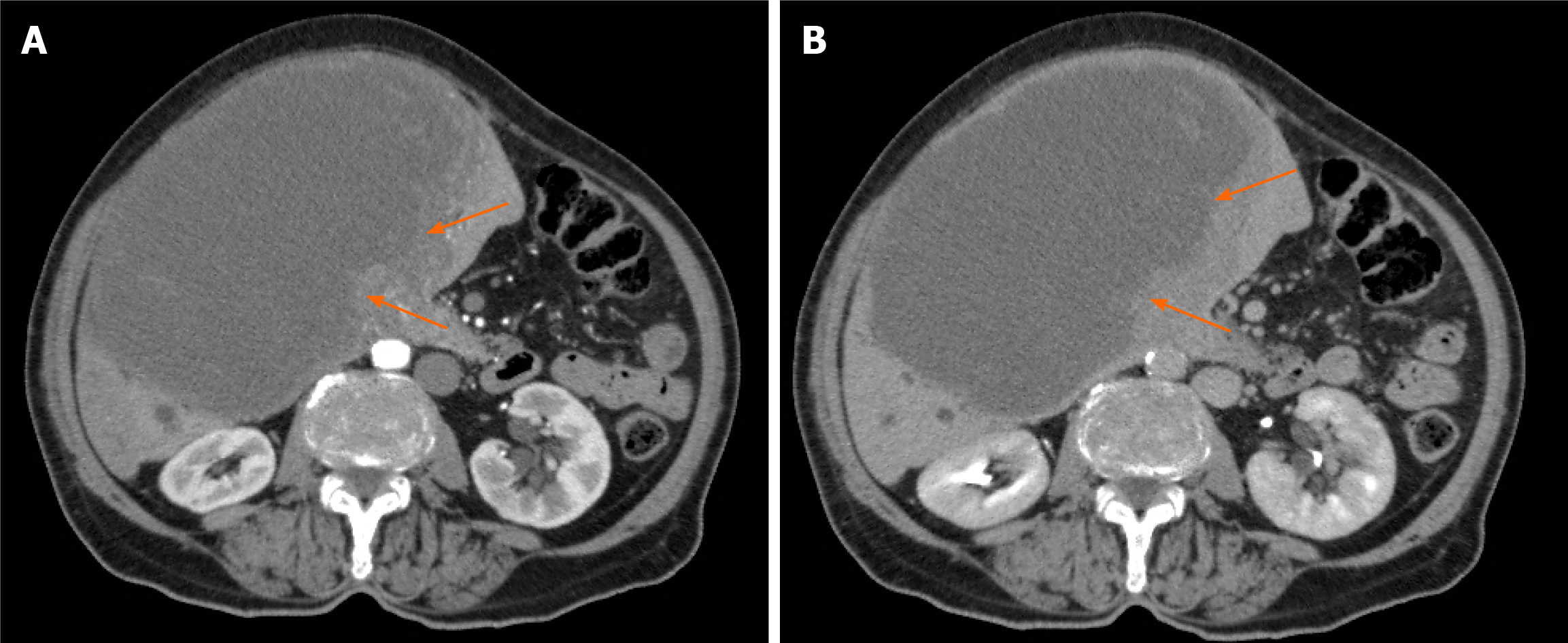
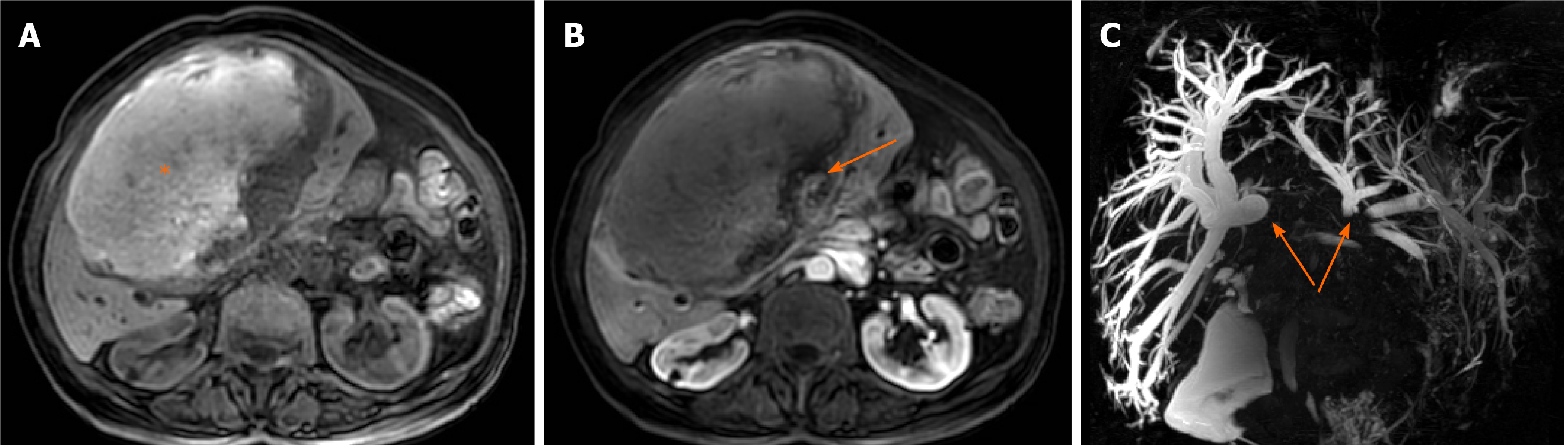
Computed tomography (CT) scan of the abdomen demonstrated a large (18.0 cm × 16.1 cm × 14.7 cm), heterogeneous hepatic mass, located in segments III, IV, V and VIII, with a solid peripheral component showing intense arterial enhancement and late-phase washout (Figure 1). Magnetic resonance imaging showed evidence of blood products within the liver mass. Dilation of the intra-hepatic bile ducts around the lesion was also observed (Figure 2).
A percutaneous tumor biopsy was performed. Histopathological analysis suggested an undifferentiated malignancy. Immunohistochemistry revealed liver cells with low mitotic index (10%). Thus, findings on imaging exams suggesting expansive tumor, well delimited and with preservation of vascular e biliary structures, despite the inconclusive biopsy, the hypothesis of GIST was considered. Pre-operative evaluation was performed according our protocol which was adapted from ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery.
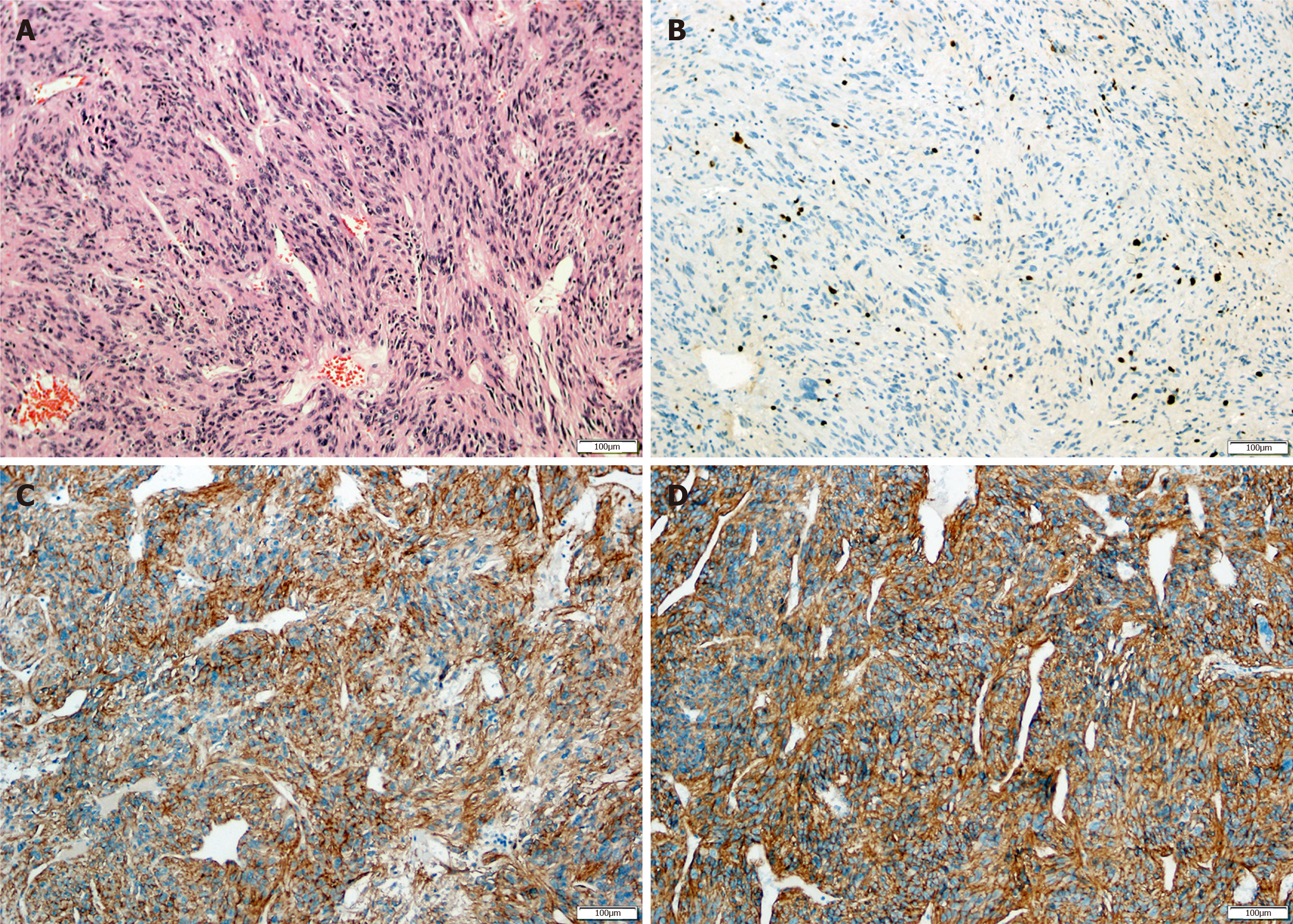
Histopathological analysis of the tumor showed a fusiform cell neoplasm positive for CD117, CD34 and DOG-1 and negative for spinal muscular atrophy and S-100 protein on immunohistochemical staining. The specimen presented a Ki67 index of 10%, which confirmed the diagnosis of primary E-GIST of the liver with intermediate-grade malignancy (Figure 3).
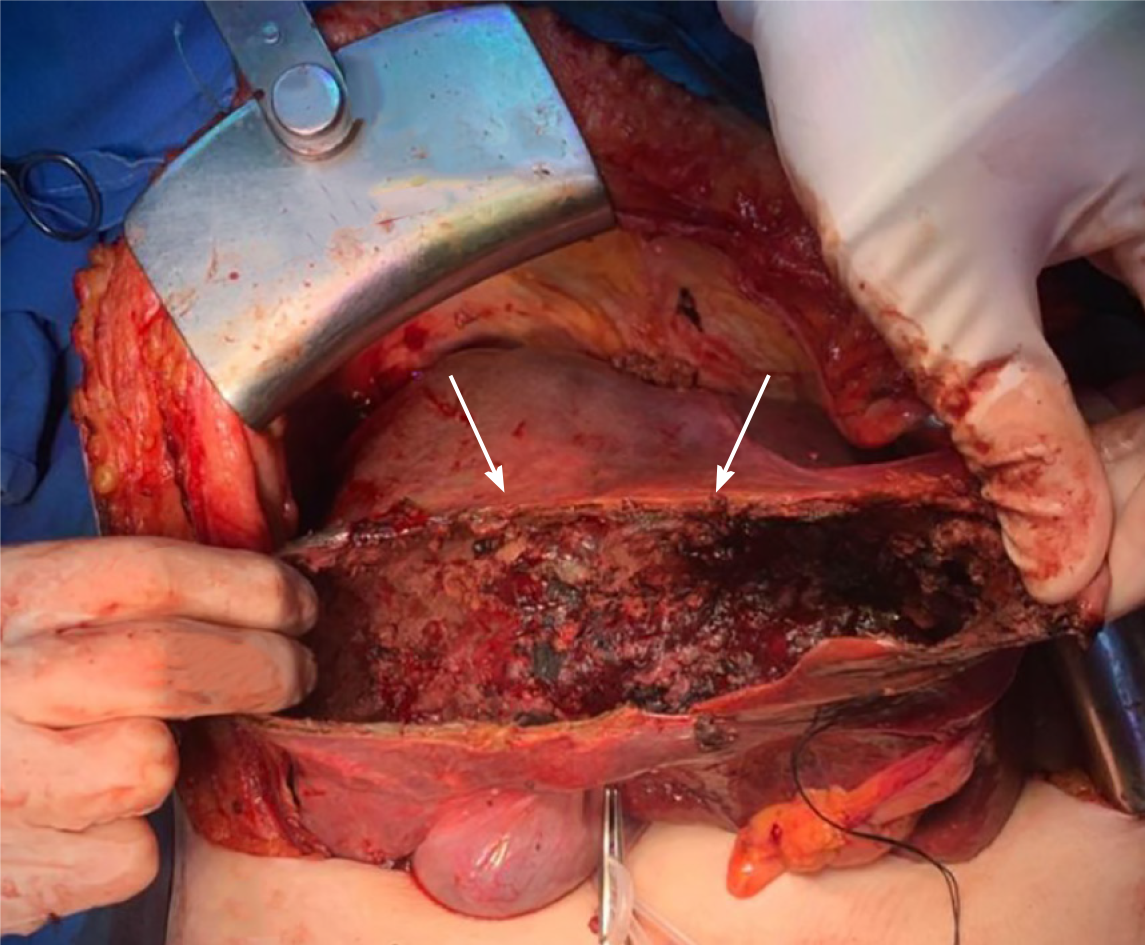
As the patient presented with progressive anemia and the lesion had a hemorrhagic component, the decision was made to perform transarterial embolization (TAE) of the tumor. There was no appreciable response, as well as mass effects symptoms were present, surgery was indicated. However, for complete resection of the tumor a left trissegmentectomy would be necessary. Considering the large size and central location of the lesion and advanced age of the patient, a non-anatomic complete resection was indicated. Ligation of the left hepatic artery was carried out. During tumor enucleation, the patient developed considerable bleeding and hemodynamic instability. Thus, a near-complete resection was performed (the posterior tumor capsule close to the raw surface of the liver was not removed) (Figure 4).
Postoperative follow-up was uneventful. After 6 mo, she remains asymptomatic and with no evidence of recurrent disease. An abdominal CT performed 6 mo after surgery demonstrated significant debulking of the mass (Figure 5).
GISTs are the most common mesenchymal neoplasm of the GI tract, representing 0.1%-0.3% of all malignancies; they are typically found in the stomach (60%-70%), small intestine (20%-30%), colorectum (5%), and esophagus (< 2%)[4,8-10]. However, GISTs have been identified outside of the GI tract (E-GISTs)[6,7]. Primary hepatic E-GISTs are very unusual, with only 22 cases reported in the literature up to 2019[1,5,11-29] (Table 1). No previous reports of cytoreductive surgery for primary E-GIST of the liver were found.
| Ref. | Year | Age/sex | Country | Presentation | Location | Size (cm) |
| Present | 2020 | 84/F | Brazil | Abdominal pain + mass | Bilobar (III/IV and V/VIII) | 16.2 |
| Hu et al[14] | 2019 | 79/F | China | Epigastric discomfort | RL | 3.2 |
| Joyon et al[15] | 2018 | 56/M | France | Abdominal pain | Bilobar (VII/VIII and LL) | 10 |
| 2018 | 59/F | France | Abdominal pain + weight loss | RL | 23 | |
| Carrillo et at[12] | 2017 | 41/M | Spain | Abdominal pain + weight loss | RL (V/VI) | 20 |
| Lok et al[19] | 2017 | 50/F | China | Abdominal pain | RL | 15 |
| Cheng et al[13] | 2016 | 63/M | China | No symptoms | RL | 15 |
| Nagai et al[28] | 2016 | 70/F | Japan | No symptoms | LL | 6 |
| Wang et al[29] | 2016 | 61/M | China | No symptoms | Caudate lobe | 7.3 |
| Liu et al[18] | 2016 | 56/F | China | No symptoms | LL + pancreas | 2.2 |
| Su et al[24] | 2015 | 65/M | Taiwan | Malaise, abdominal pain, loss of appetite | LL | 12 |
| Bhoy et al[11] | 2014 | 41/F | India | Abdominal pain, weight loss | RL (VI/VII) | 15 |
| Lin et al[17] | 2015 | 67/F | China | No symptoms | RL | 7.4 |
| Mao et al[22] | 2015 | 60/F | China | No symptoms | Bilobar (I, IV, V and VIII) | 12.8 |
| Kim et al[16] | 2014 | 71/M | South Korea | No symptoms | LL | 7 |
| Louis et al[20] | 2014 | 55/F | India | Abdominal pain, loss of appetite | Bilobar (II, III, VI and VIII) | 14.5 |
| Zhou et al[27] | 2014 | 56/M | China | No symptoms | RL | 10 |
| Li et al[37] | 2012 | 53/M | China | Abdominal discomfort | RL | 20 |
| Yamamoto et al[25] | 2010 | 70/M | Japan | Loss of appetite | LL | 20 |
| Luo et al[21] | 2009 | 17/M | China | No symptoms | RL | 5 |
| Ochiai et al[23] | 2009 | 30/M | Japan | Abdominal fullness | Bilobar | 27 |
| De Chiara et al[5] | 2006 | 37/M | Italy | No symptoms | RL (V) | 18 |
| Hu et al[1] | 2003 | 79/F | United States | Shortness of breath, pleuritic chest pain | RL | 15 |
GISTs presenting in the liver are usually metastatic until proven otherwise. There is no specific test able to define their primary or metastatic nature, and the diagnosis of primary hepatic E-GIST has to fulfill several conditions[15]. Endoscopic and imaging studies must show no evidence of GIST in the GI tract, absence of connection with the muscularis propria of the GI tract must be proven, and the patient must have no medical history suggesting resection of an overlooked or misdiagnosed GIST[3]. Diagnosis of a new GI tumor during the follow-up period also would preclude diagnosis of a primary GIST of the liver[15]. The patient reported in this paper has completed 6 mo of follow-up after surgery and, so far, all the aforementioned requirements for diagnosis of a primary hepatic E-GIST have been fulfilled.
The imaging picture of a primary E-GIST of the liver is a well-defined, heterogeneous, hypervascular lesion with areas of hemorrhage, necrosis, and/or cystic degeneration[30,31]. Thus, primary hepatic E-GISTs can be potentially misdiagnosed as other hepatic tumors, such as hypervascular metastasis, hepatocellular carcinoma and adenoma. Despite their rarity, primary hepatic E-GIST should be included in the differential diagnosis of primary liver lesions whenever a heterogeneous hypervascular liver mass is identified, especially in patients with no known primary neoplasia, no history of chronic liver disease, and no risk factors for adenoma[20].
Complete surgical resection followed by adjuvant therapy with imatinib is the standard of care for localized GIST, but other therapeutic options have been proposed, depending on the initial presentation and clinical context. Cytoreductive surgery has been used to prolong survival and improve quality of life for patients with metastatic neuroendocrine and ovarian cancer[32,33]. However, there is a scarcity of studies analyzing the impact of alternative treatments for advanced GIST, especially those cases in which complete R0 resection cannot be achieved. Recently, it has been demonstrated that debulking surgery combined with adjuvant drug therapy prolongs overall survival of patients with metastatic primary GIST when compared with imatinib alone[34]. TAE is also recommended as an option to impair stromal tumor progression[35].
In this case, a giant hepatic GIST was observed in a very frail 84-year-old woman. TAE was indicated to reduce tumor burden, an anatomic liver resection was avoided, and a tailored therapeutic approach was recommended. Despite the hypervascular nature of the tumor, there was no significant shrinkage after TAE. It was unlikely that pain and symptomatic relief would be achieved by systemic therapy alone, which also has been associated with GI and/or intra-abdominal bleeding due to tumor degeneration in approximately 5% of giant GISTs[36]. Therefore, considering the risk/benefit ratio, tumor debulking surgery was indicated as a strategy to control pain and improve patient quality of life while avoiding the morbidity and mortality associated with a major liver resection. Six months after adjuvant therapy with imatinib, she is asymptomatic with little residual tumor, as shown in the last abdominal CT scan (Figure 5).
E-GIST must be considered in the differential diagnosis of any large, hypervascular liver mass. Preoperative histopathological and immunohistochemical diagnosis is important to aid in therapeutic management. Aggressive strategies such as R0 surgical resection should always be the first choice, but a customized approach including a combination of TAE, cytoreductive surgery, and adjuvant or neoadjuvant systemic pharmacotherapy might be considered as an alternative, especially in high-risk patients.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kohno S S-Editor: Fan JR L-Editor: A P-Editor: Li JH
| 1. | Hu X, Forster J, Damjanov I. Primary malignant gastrointestinal stromal tumor of the liver. Arch Pathol Lab Med. 2003;127:1606-1608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Feng F, Tian Y, Liu Z, Xu G, Liu S, Guo M, Lian X, Fan D, Zhang H. Clinicopathologic Features and Clinical Outcomes of Esophageal Gastrointestinal Stromal Tumor: Evaluation of a Pooled Case Series. Medicine (Baltimore). 2016;95:e2446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (33)] |
| 3. | Vanel D, Albiter M, Shapeero L, Le Cesne A, Bonvalot S, Le Pechoux C, Terrier P, Petrow P, Caillet H, Dromain C. Role of computed tomography in the follow-up of hepatic and peritoneal metastases of GIST under imatinib mesylate treatment: a prospective study of 54 patients. Eur J Radiol. 2005;54:118-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti H, Rubin BP, Shmookler B, Sobin LH, Weiss SW. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002;33:459-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2231] [Cited by in RCA: 2149] [Article Influence: 93.4] [Reference Citation Analysis (1)] |
| 5. | De Chiara A, De Rosa V, Lastoria S, Franco R, Botti G, Iaffaioli VR, Apice G. Primary gastrointestinal stromal tumor of the liver with lung metastases successfully treated with STI-571 (imatinib mesylate). Front Biosci. 2006;11:498-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000;13:577-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 331] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 7. | Miettinen M, Lasota J. Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol. 2006;23:70-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1244] [Cited by in RCA: 1304] [Article Influence: 72.4] [Reference Citation Analysis (33)] |
| 8. | Sheppard K, Kinross KM, Solomon B, Pearson RB, Phillips WA. Targeting PI3 kinase/AKT/mTOR signaling in cancer. Crit Rev Oncog. 2012;17:69-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 183] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 9. | Sircar K, Hewlett BR, Huizinga JD, Chorneyko K, Berezin I, Riddell RH. Interstitial cells of Cajal as precursors of gastrointestinal stromal tumors. Am J Surg Pathol. 1999;23:377-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 337] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 10. | Miettinen M, Majidi M, Lasota J. Pathology and diagnostic criteria of gastrointestinal stromal tumors (GISTs): a review. Eur J Cancer. 2002;38 Suppl 5:S39-S51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 321] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 11. | Bhoy T, Lalwani S, Mistry J, Varma V, Kumaran V, Nundy S, Mehta N. Primary hepatic gastrointestinal stromal tumor. Trop Gastroenterol. 2014;35:252-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Carrillo Colmenero AM, Serradilla Martín M, Redondo Olmedilla MD, Ramos Pleguezuelos FM, López Leiva P. Giant primary extra gastrointestinal stromal tumor of the liver. Cir Esp. 2017;95:547-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Cheng X, Chen D, Chen W, Sheng Q. Primary gastrointestinal stromal tumor of the liver: A case report and review of the literature. Oncol Lett. 2016;12:2772-2776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Hu HJ, Fu YY, Li FY. Primary Gastrointestinal Stromal Tumor of the Liver. Clin Gastroenterol Hepatol. 2019;17:e106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Joyon N, Dumortier J, Aline-Fardin A, Caramella C, Valette PJ, Blay JY, Scoazec JY, Dartigues P. Gastrointestinal stromal tumors (GIST) presenting in the liver: Diagnostic, prognostic and therapeutic issues. Clin Res Hepatol Gastroenterol. 2018;42:e23-e28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Kim HO, Kim JE, Bae KS, Choi BH, Jeong CY, Lee JS. Imaging findings of primary malignant gastrointestinal stromal tumor of the liver. Jpn J Radiol. 2014;32:365-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Lin XK, Zhang Q, Yang WL, Shou CH, Liu XS, Sun JY, Yu JR. Primary gastrointestinal stromal tumor of the liver treated with sequential therapy. World J Gastroenterol. 2015;21:2573-2576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Liu L, Zhu Y, Wang D, Yang C, Zhang QI, Li X, Bai Y. Coexisting and possible primary extra-gastrointestinal stromal tumors of the pancreas and liver: A single case report. Oncol Lett. 2016;11:3303-3307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Lok HT, Chong CN, Chan AW, Fong KW, Cheung YS, Wong J, Lee KF, Lai PB. Primary hepatic gastrointestinal stromal tumor presented with rupture. Hepatobiliary Surg Nutr. 2017;6:65-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Louis AR, Singh S, Gupta SK, Sharma A. Primary GIST of the liver masquerading as primary intra-abdominal tumour: a rare extra-gastrointestinal stromal tumour (EGIST) of the liver. J Gastrointest Cancer. 2014;45:392-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 21. | Luo XL, Liu D, Yang JJ, Zheng MW, Zhang J, Zhou XD. Primary gastrointestinal stromal tumor of the liver: a case report. World J Gastroenterol. 2009;15:3704-3707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Mao L, Chen J, Liu Z, Liu CJ, Tang M, Qiu YD. Extracorporeal hepatic resection and autotransplantation for primary gastrointestinal stromal tumor of the liver. Transplant Proc. 2015;47:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Ochiai T, Sonoyama T, Kikuchi S, Ikoma H, Kubota T, Nakanishi M, Ichikawa D, Fujiwara H, Okamoto K, Sakakura C, Kokuba Y, Taniguchi H, Otsuji E. Primary large gastrointestinal stromal tumor of the liver: report of a case. Surg Today. 2009;39:633-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Su YY, Chiang NJ, Wu CC, Chen LT. Primary gastrointestinal stromal tumor of the liver in an anorectal melanoma survivor: A case report. Oncol Lett. 2015;10:2366-2370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Yamamoto H, Miyamoto Y, Nishihara Y, Kojima A, Imamura M, Kishikawa K, Takase Y, Ario K, Oda Y, Tsuneyoshi M. Primary gastrointestinal stromal tumor of the liver with PDGFRA gene mutation. Hum Pathol. 2010;41:605-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Zhao X, Yue C. Gastrointestinal stromal tumor. J Gastrointest Oncol. 2012;3:189-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 62] [Reference Citation Analysis (0)] |
| 27. | Zhou B, Zhang M, Yan S, Zheng S. Primary gastrointestinal stromal tumor of the liver: report of a case. Surg Today. 2014;44:1142-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Nagai T, Ueda K, Hakoda H, Okata S, Nakata S, Taira T, Aoki S, Mishima H, Sako A, Maruyama T, Okumura M. Primary gastrointestinal stromal tumor of the liver: a case report and review of the literature. Surg Case Rep. 2016;2:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Wang Y, Liu Y, Zhong Y, Ji B. Malignant extra-gastrointestinal stromal tumor of the liver: A case report. Oncol Lett. 2016;11:3929-3932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Yu MH, Lee JM, Baek JH, Han JK, Choi BI. MRI features of gastrointestinal stromal tumors. AJR Am J Roentgenol. 2014;203:980-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Ghanem N, Altehoefer C, Furtwängler A, Winterer J, Schäfer O, Springer O, Kotter E, Langer M. Computed tomography in gastrointestinal stromal tumors. Eur Radiol. 2003;13:1669-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 32. | Ejaz A, Reames BN, Maithel S, Poultsides GA, Bauer TW, Fields RC, Weiss MJ, Marques HP, Aldrighetti L, Pawlik TM. Cytoreductive debulking surgery among patients with neuroendocrine liver metastasis: a multi-institutional analysis. HPB (Oxford). 2018;20:277-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 33. | Griffiths CT. Surgical resection of tumor bulk in the primary treatment of ovarian carcinoma. Natl Cancer Inst Monogr. 1975;42:101-104. [PubMed] |
| 34. | Qiu HB, Zhou ZG, Feng XY, Liu XC, Guo J, Ma MZ, Chen YB, Sun XW, Zhou ZW. Advanced gastrointestinal stromal tumor patients benefit from palliative surgery after tyrosine kinase inhibitors therapy. Medicine (Baltimore). 2018;97:e9097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 35. | Tamura J, Nakayama Y, Kitaguchi K, Ura K, Taira K, Ooe H, Yoshikawa A, Ishigami S, Baba N. [A successfully resected case of liver metastasis of gastrointestinal stromal tumor responding to neoadjuvant chemotherapy with imatinib mesylate and interventional radiology]. Gan To Kagaku Ryoho. 2009;36:1769-1772. [PubMed] |
| 36. | Demetri GD, von Mehren M, Blanke CD, Van den Abbeele AD, Eisenberg B, Roberts PJ, Heinrich MC, Tuveson DA, Singer S, Janicek M, Fletcher JA, Silverman SG, Silberman SL, Capdeville R, Kiese B, Peng B, Dimitrijevic S, Druker BJ, Corless C, Fletcher CD, Joensuu H. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002;347:472-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3203] [Cited by in RCA: 3110] [Article Influence: 135.2] [Reference Citation Analysis (0)] |
| 37. | Li ZY, Liang QL, Chen GQ, Zhou Y, Liu QL. Extra-gastrointestinal stromal tumor of the liver diagnosed by ultrasound-guided fine needle aspiration cytology: a case report and review of the literature. Arch Med Sci. 2012;8:392-397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |