Published online Dec 27, 2021. doi: 10.4240/wjgs.v13.i12.1721
Peer-review started: March 30, 2021
First decision: May 13, 2021
Revised: May 28, 2021
Accepted: November 30, 2021
Article in press: November 30, 2021
Published online: December 27, 2021
Processing time: 268 Days and 19.4 Hours
Although the treatment guidelines for left sided diverticulitis are clear, the management of right colonic diverticulitis is not well established. This disease can no longer be ignored due to significant spread throughout Asia.
To analyse epidemiology, diagnosis and treatment of right-sided diverticulitis in western countries.
MEDLINE and PubMed searches were performed using the key words “right-sided diverticulitis’’, ‘‘right colon diverticulitis’’, ‘‘caecal diverticulitis’’, ‘‘ascending colon diverticulitis’’ and ‘‘caecum diverticula’’ in order to find relevant articles published until 2021.
A total of 18 studies with 422 patients were found. Correct diagnosis was made only in 32.2%, mostly intraoperatively or via CT scan. The main reason for misdiagnosis was a suspected acute appendicitis (56.8%). The treatment was a non-operative management (NOM) in 184 patients (43.6%) and surgical in 238 patients (56.4%), seven of which after NOM failure. Recurrence rate was low (5.45%), similar to eastern studies and inferior to left -sided diverticulitis. Recurrent patients were successfully conservatively retreated in most cases.
The management of right- sided diverticulitis is not well clarified in the western world and no selective guidelines have been considered even if principles are similar to those with left- sided diverticulitis. Wrong diagnosis is one of the most important problems and CT scan seems to be the best imaging modality. NOM offers a safe and effective treatment; surgery should be considered only in cases of complicated diverticulitis or if malignancy cannot be excluded. Further studies are needed to clarify the correct treatment.
Core Tip: This paper underlined the importance to collect more data on right-sided diverticulitis to understand if it is a more common condition than we thought, and if we really need more selective guidelines or we can simply apply the principles already proposed for left-sided diverticulitis.
- Citation: Epifani AG, Cassini D, Cirocchi R, Accardo C, Di Candido F, Ardu M, Baldazzi G. Right sided diverticulitis in western countries: A review. World J Gastrointest Surg 2021; 13(12): 1721-1735
- URL: https://www.wjgnet.com/1948-9366/full/v13/i12/1721.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i12.1721
Historically, diverticula in western countries are mostly located in sigmoid colon while right-sided diverticulosis (RSD) is rare. Conversely, colonic diverticula are mostly located on the right colon in eastern patients in contrast to those in Europe and the United States[1,2]. Recently several studies show an important spread of RSD in the world over Asia[3-5].
Regarding the diverticula of the right colon, we differentiate the diverticula of the cecum (solitary or multiple) and the ascending colon. In 1912, Potier[6] first described a case of cecum diverticulum. While the first case of diverticulitis in the ascending colon was described by Telling et al[7] in 1916, in this review we analyzed both subtypes.
The etiology and the real prevalence of this difference is still unclear. All studies about management of acute right-sided colonic diverticulitis (ARCD) are related to the Asian population and no specific guidelines are still available. The aim of the present study was to review epidemiology, diagnosis and treatment of ARCD to better analyze this disease in Western populations.
An extensive search for literature was carried out using MEDLINE (PubMed) and Cochrane Database of Collected Reviews for potentially relevant studies between January 1, 1990, and January 1, 2021.
The terms used for the search were: ‘‘right-sided diverticulitis’’, ‘‘right colon diverticulitis’’, ‘‘caecal diverticulitis’’, ‘‘ascending colon diverticulitis’’ and ‘‘caecum diverticula’’.
Exclusion criteria were studies based on the Asian population, left-sided diverticulitis, undefined laterality or both left-sided and right-sided diverticulitis, irrelevant publications, age < 18 years. Articles not written in English or full text not available as well as case reports and case series (< 5 patients), review articles and letters to the editor were excluded.
Right-sided laterality was defined as diverticulitis involving the cecum or the ascending colon until hepatic flexure.
“Correct diagnosis” was defined as radiologically confirmed diagnosis of diverticulitis, before any medical or surgical treatment.
“Presumptive diagnosis” was defined as diagnosis of diverticulitis deemed likely despite the absence of radiological confirmation, before any medical or surgical treatment.
“Diagnostic accuracy” was defined as the rate of correct diagnosis over the total number of patients analyzed.
“Non-operative management” was defined as any treatment not requiring surgery (e.g., bowel rest, antibiotics with or without percutaneous drainage).
Two reviewers (Epifani AG, Accardo C) will independently have screened titles and abstracts, evaluating the full text of potentially eligible studies. Any doubt or disagreements has been resolved by a third reviewer (Cassini D).
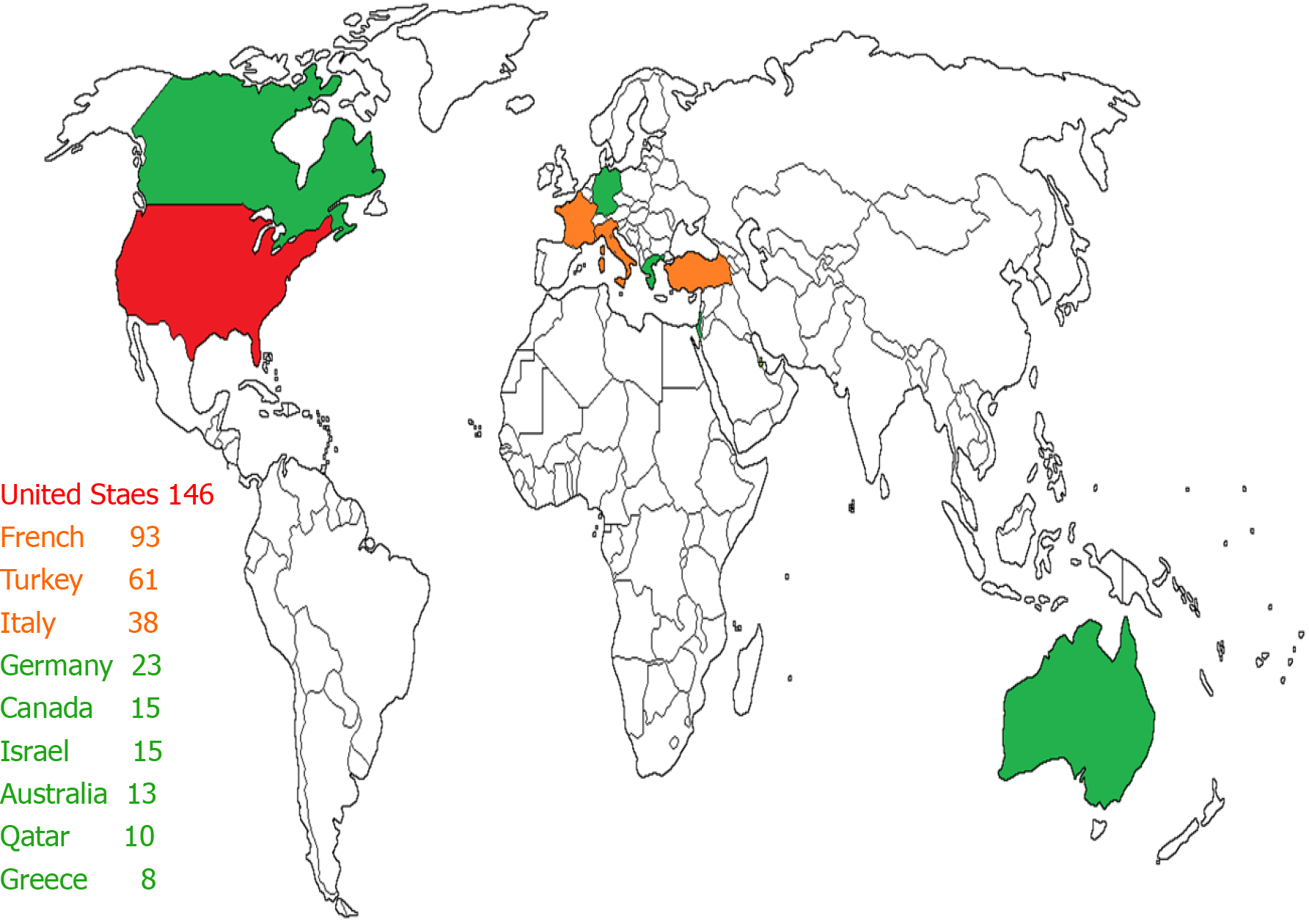
We included studies from Turkey because geopolitically it is also a European country and from Israel because most people are Caucasian with similar lifestyles to western countries and finally from Qatar because of their westernized diet and lifestyle.
We excluded the review by Schlussel et al[8] because their study included patients from the NIS database which is based on the international statistical classification of diseases and related health problems (ICD) coding method. By selecting the cases in this way it has not been possible to argue many of their results and we have not been able to do an adequate data extraction. Furthermore, lacking a specific code for coding ARCD, the low accuracy of this research method was also highlighted in another study in which the authors who had initially screened ARCD with ICD codes, found a high percentage of misdiagnosed cases (74%) when they subsequently analyzed every medical chart[9].
We analyzed data regarding study design, number of patients, demographic characteristics (age, sex), location of diverticula, diagnostic evaluation methods, misdiagnosis and modified Hinchey classification[10]. We also analysed data regarding the treatment distinguished between non-operative management (NOM) (every treatment not requiring surgery, e.g., bowel rest, antibiotic, percutaneous drainage) and surgery (reporting every procedure and relative approach). We therefore analysed short-term and long-term outcomes: length of stay, complications, reintervention, need for ostomy, death, recurrence (rate and type of treatment) and median follow-up. Data were analyzed with descriptive statistics.
Primary outcome was the analysis of short-term and long-term outcomes, especially regarding recurrence rate. The secondary outcome was the evaluation of diagnosis methods and percentage of misdiagnosis.
Quality of studies were evaluated by a methodological index for non-randomized studies (MINORS) score[11]. MINORS is a valid tool to easily assess the quality of non-randomized surgical studies both comparative or not (with a maximum score of 24 and 16, respectively). Of the 18 included studies, 16 had a retrospective cohort design and 2 had a retrospective cross-sectional design.
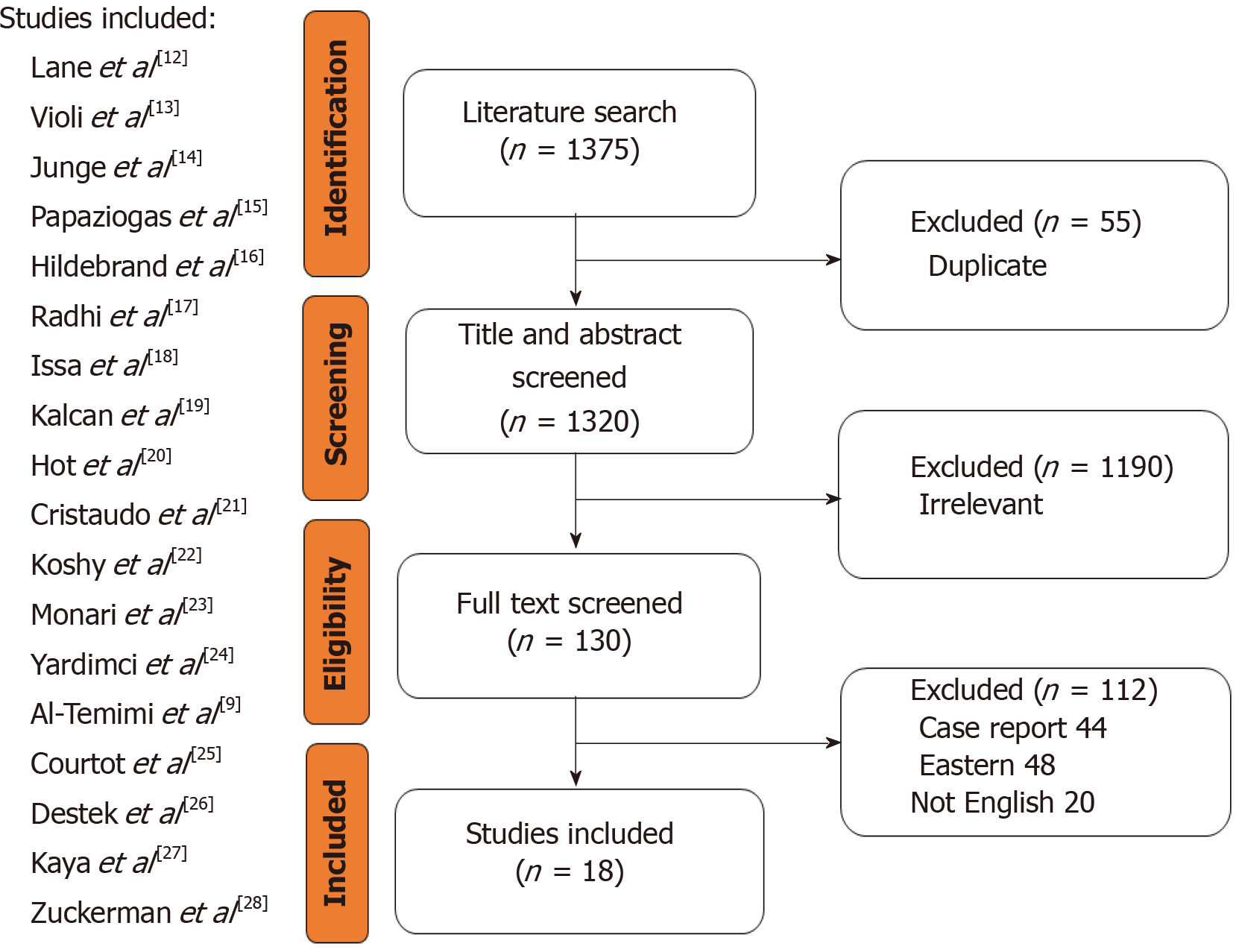
With our research we initially found 1375 articles. After removing 55 duplicates, we screened titles and abstracts excluding 1188 other articles. We therefore evaluated 130 full-text reviews and obtained 18 eligible studies. The entire process of screening is shown in Figure 1[9,12-28].
We analysed 18 studies, for a total of 422 patients. A summary of results is shown in Table 1, Table 2, Table 3, and Table 4[9,12-28] and in Figure 2. There were 212 females (50.2%) and 190 males (45%), however in 20 patients (4.7%) sex was not recorded. Mean patient age was 50.9 years (range: 30-65).
| Ref. | Year | Country | Numbers of patients | Minors | Follow-up (Mo) | Age | Male | Unc1 or Hinchey I/II | Hinchey III/IV | LOS2 (d) | Total recurrence (rate) |
| Lane et al[12] | 1999 | United States | 49 | 7 | 32 | 30 | 12.7 | 4 (8.16%) | |||
| Violi et al[13] | 2000 | Italy | 20 | 5 | 0 | ||||||
| Junge et al[14] | 2003 | Germany | 7 | 7 | 42 | 56 | 1 | ||||
| Papaziogas et al[15] | 2005 | Greece | 8 | 10 | 174 | 54.2 | 6 | 22 | 1 | ||
| Hildebrand et al[16] | 2007 | Germany | 16 | 16 | 60.9 | 4 | 11 | ||||
| Radhi et al[17] | 2011 | Canada | 15 | 7 | 65 | 6 | |||||
| Issa et al[18] | 2012 | Israel | 15 | 12 | 32 | 52 | 10 | 15 | 1 (6%) | ||
| Kalcan et al[19] | 2015 | Turkey | 6 | 8 | 6 | 34 | 4 | 4.5 | |||
| Hot et al[20] | 2015 | Turkey | 10 | 11 | 60 | 38.9 | 5 | 5 | |||
| Cristaudo et al[21] | 2015 | Australia | 13 | 11 | 12 | 44 | 8 | 4 | 0 | ||
| Koshy et al[22] | 2016 | Qatar | 10 | 11 | 18 | 30.4 | 9 | 0 | |||
| Monari et al[23] | 2017 | Italy | 18 | 11 | 29 | 50 | 10 | 0 | |||
| Yardimci et al[24] | 2017 | Turkey | 12 | 12 | 5.5 | 45 | 6 | 12 | 0 | ||
| Al-Temimi et al[9] | 2018 | United States | 33 | 17 | 56 | 13 | 20 | 9 | 7.6 | ||
| Courtot et al[25] | 2019 | France | 93 | 12 | 33 | 54 | 58 | 30 | 4 | 7 | |
| Destek et al[26] | 2019 | Turkey | 22 | 11 | 24 | 50.9 | 13 | 22 | 4 | ||
| Kaya et al[27] | 2020 | Turkey | 11 | 12 | 52 | 7 | 4.6 | 1 | |||
| Zuckerman et al[28] | 2020 | United States | 64 | 13 | 74.4 | 51.2 | 27 | 60 | 4 | 5 | 5 |
| Tot | 29 yr | 10 | 422 | 32 | 50.9 | 190 (45.2%) | 179 | 20 | 5 | 23 (5.45%) |
| Ref. | Year | Country | Numbers of patients | Diagnosis pre-op1 | Ultrasound | CT | Barium enema | Other | Diagn intra-op2 | Misdiagnosis (appendicitis) | Cecum (solitary) | Right | PAN-Div3 |
| Lane et al[12] | 1999 | United States | 49 | 3 | 2 | 1 | 41 | 46 (nr) | 49 (37) | 0 | |||
| Violi et al[13] | 2000 | Italy | 20 | 5 | 3 | 3 | 3 | 11 | |||||
| Junge et al[14] | 2003 | Germany | 7 | 2 | 2 | 7 | 5 (4) | 7 (6) | |||||
| Papaziogas et al[15] | 2005 | Greece | 8 | 0 | 7 (7) | 8 (nr) | 2 | ||||||
| Hildebrand et al[16] | 2007 | Germany | 16 | 7 | 9 (5) | ||||||||
| Radhi et al[17] | 2011 | Canada | 15 | ||||||||||
| Issa et al[18] | 2012 | Israel | 15 | 15 | 15 | 3 | 9 | 3 | |||||
| Kalcan et al[19] | 2015 | Turkey | 6 | 0 | 4 | 6 | 6 | ||||||
| Hot et al[20] | 2015 | Turkey | 10 | 1 | 10 | 9 (9) | 10 (10) | ||||||
| Cristaudo et al[21] | 2015 | Australia | 13 | 10 | 1 | 9 | 3 | 3 (3) | 13 | ||||
| Koshy et al[22] | 2016 | Qatar | 10 | 1 | 1 | 9 | 9 (9) | ||||||
| Monari et al[23] | 2017 | Italy | 18 | 9 | 1 | 6 | 1 | 1 XR 1 colon | 9 | 9 | 11 | 7 | |
| Yardimci et al[24] | 2017 | Turkey | 12 | 12 | 10 | 2 | |||||||
| Al-Temimi et al[9] | 2018 | United States | 33 | 13 | 20 (11) | ||||||||
| Courtot et al[25] | 2019 | France | 93 | 6 (6) | 49 | ||||||||
| Destek et al[26] | 2019 | Turkey | 22 | 2 (2) | 9 | 13 | |||||||
| Kaya et al[27] | 2020 | Turkey | 11 | 8 | 2 | 6 | 5 (5) | 6 | |||||
| Zuckerman et al[28] | 2020 | United States | 64 | 50 | 50 | 11 | 15 (10) | 33 | 22 | ||||
| Tot | 29 yr | 10 | 422 | 136 32.2% | 17 12.5% | 96 70.6% | 4 2.9% | 2 1.9% | 98 (23.2%) | 162 (92) 38.39% | 155 (97) 36.7% | 51 12% | 54 12.8% |
| Ref. | Year | Country | Numbers of patients | NOM | Surgery | Surgery after NOM | Complications | Re-intervention | Death | Recurr1 after NOM | Recurr1 after Surg2 | Recurr1 treatment |
| Lane et al[12] | 1999 | United States | 49 | 0 | 49 | 7 | 4 | 0 | 4 | 4 Surg2 | ||
| Violi et al[13] | 2000 | Italy | 20 | 0 | 20 | 0 | ||||||
| Junge et al[14] | 2003 | Germany | 7 | 0 | 7 | |||||||
| Papaziogas et al[15] | 2005 | Greece | 8 | 0 | 8 | 1 | 1 NOM | |||||
| Hildebrand et al[16] | 2007 | Germany | 16 | 16 | 0 | |||||||
| Radhi et al [17] | 2011 | Canada | 15 | 15 | ||||||||
| Issa et al[18] | 2012 | Israel | 15 | 15 | 1 | 1 NOM | ||||||
| Kalcan et al[19] | 2015 | Turkey | 6 | 6 | ||||||||
| Hot et al[20] | 2015 | Turkey | 10 | 10 | 0 | 0 | 0 | 0 | ||||
| Cristaudo et al[21] | 2015 | Australia | 13 | 10 | 3 | 0 | 0 | |||||
| Koshy et al[22] | 2016 | Qatar | 10 | 1 | 9 | 2 | 0 | |||||
| Monari et al[23] | 2017 | Italy | 18 | 18 | 3 | 0 | 0 | 0 | ||||
| Yardimci et al[24] | 2017 | Turkey | 12 | 12 | 0 | 0 | ||||||
| Al-Temimi et al[9] | 2018 | United States | 33 | 4 | 33 | 10 | ||||||
| Courtot et al[25] | 2019 | France | 93 | 68 | 25 | 6 | 19 | 1 | 0 | 6 | 1 | 5 NOM; 2 Surg |
| Destek et al[26] | 2019 | Turkey | 22 | 19 | 3 | 0 | 0 | 0 | 0 | 4 | 0 | 4 NOM |
| Kaya et al[27] | 2020 | Turkey | 11 | 6 | 5 | 2 | 1 | 1 NOM | ||||
| Zuckerman et al[28] | 2020 | United States | 64 | 49 | 15 | 1 | 2 | 5 | 0 | 4 NOM; 1 Surg | ||
| Tot | 29 yr | 10 | 422 | 184 (43.6%) | 238 (56.4%) | 7 (2.9%) | 45 (10.6%) | 6 (2.5%) | 0 | 17 (6%) | 6 (2.5%) | 16 NOM; 7 Surg |
| Ref. | Year | Country | Numbers of patients | DIV | AP | DIV + AP | ICR | Right colectomy | Ostomy | Open | VLS | Converted (rate) |
| Lane et al[12] | 1999 | United States | 49 | 7 | 3 | 39 | 1 | 49 | ||||
| Violi et al[13] | 2000 | Italy | 20 | 6 | 14 | |||||||
| Junge et al[14] | 2003 | Germany | 7 | 6 | 1 | 0 | ||||||
| Papaziogas et al[15] | 2005 | Greece | 8 | 6 | 0 | 2 | 0 | 8 | ||||
| Hildebrand et al[16] | 2007 | Germany | 16 | 3 | 16 | 0 | 15 | |||||
| Radhi et a [17] | 2011 | Canada | 15 | 15 | 15 | 1 (6%) | ||||||
| Issa et al[18] | 2012 | Israel | 15 | |||||||||
| Kalcan et al[19] | 2015 | Turkey | 6 | 5 | 1 | 4 | 2 | 2 (100%) | ||||
| Hot et al[20] | 2015 | Turkey | 10 | 1 | 9 | 0 | 10 | |||||
| Cristaudo et al[21] | 2015 | Australia | 13 | 2 | 1 | 3 | 1 (33.3%) | |||||
| Koshy et al[22] | 2016 | Qatar | 10 | 5 | 4 | 9 | 4 (44.4%) | |||||
| Monari et al[23] | 2017 | Italy | 18 | 5 | 4 | 9 | 0 | 4 | 14 | 5 (35.7%) | ||
| Yardimci et al[24] | 2017 | Turkey | 12 | |||||||||
| Al-Temimi et al[9] | 2018 | United States | 33 | 4 | 29 | 2 | 23 | 10 | 2 (20%) | |||
| Courtot et al[25] | 2019 | France | 93 | 1 | 2 | 6 | 16 | 2 | 9 | 16 | 5 (31%) | |
| Destek et al[26] | 2019 | Turkey | 22 | 2 | 1 | 0 | ||||||
| Kaya et al[27] | 2020 | Turkey | 11 | 2 | 2 | 1 | ||||||
| Zuckerman et al[28] | 2020 | United States | 64 | 6 | 8 | |||||||
| Tot | 29 yr | 10 | 422 | 30 12.6% | 16 6.7% | 17 7.1% | 31 13% | 151 63.4% | 5 2.1% | 122 63.5% | 70 36.5% | 20 28.6% |
The diagnosis was correctly achieved or presumed in 136 cases (32.2%), via CT scan in 96 cases (70.6%), by sonography in 17 cases (12.5%), and rarely by barium enema (4 cases, 2.9%), radiography or colonoscopy (one case each, accounting for 0.2%).
A correct diagnosis was achieved only intraoperatively in 98 cases (23%), while a misdiagnosis occurred in 162 cases (38.4%), 92 of which were suspected acute appendicitis.
Diverticula were caecal in 142 cases (33.6%), located in the right colon in 41 cases (12%), mixed in 3 cases and also 54 patients (12.8%) had left-sided diverticulosis (LSD). The exact location of right-sided diverticula (whether cecal or ascending) was not reported in 242 cases (57.3%). When reported, Hinchey classification was the most used scale (42%). They have reported 159 Hinchey I/II or uncomplicated diverticulitis, 17 Hinchey III and 3 Hinchey IV cases. Misdiagnosis occurred in 131 out of 219 patients (59.8%).
The treatment was NOM in 184 patients (median 43.6%) and surgery in 238 patients (56.4%), seven of which after NOM failure (2.94%). Surgical approach was open in 122 cases (51.2%) and laparoscopic in 70 patients (with a conversion rate of 28.6%).
Regarding surgical procedures: diverticulectomy in 30 patients; primary resection and anastomoses (PRA) in 182 patients (76.4%): when specified we found 31 ileocecal resections and 151 right hemicolectomies. In 33 cases an appendectomy was performed and 17 cases were associated with diverticulectomy.
Regarding post-operative complications, 45 adverse events were recorded (even if the surgical ones are not always differentiated) (10.7%), five diverting stoma were created (1.18%) and six reoperations were needed (2.5% of surgically treated patients). No deaths were reported. The mean length of hospital stay was 5 d (range: 4–22 d), and the median follow-up was 32.5 mo (range: 5–174 mo).
Recurrence occurred in 23 cases (5.45%), sixteen of which after NOM (3.8% of total, 5.98% of NOM cases), six after surgery (1.4% total, 2.5% of surgery cases) and in one case was not reported if recurrence occurred after NOM or surgery failure (treated with antibiotic). In the other cases, treatment after NOM was NOM again in 13 cases, while three patients underwent surgery; as well as two patients after surgery were treated via NOM and four patients underwent surgery again.
Diverticula presents as herniations of the bowel wall, mostly located in areas of structural weakness, such as the site of vessel penetrance. The bowel in diverticular disease patients appears shortened and shows thickened circular and longitudinal muscle layers due to elastosis. Patients with diverticular disease showed also irregular muscle bundle orientation, reduced myosin (MYH11) heavy chain gene expression, enhanced collagen crosslinking, which all contribute to the risk for bowel wall herniation[29-31].
Other relevant factors involved in the development of diverticular are abnormal bowel motility (due to altered enteric nervous system), gut microbiome, low fiber intake and western lifestyle[5-8].
Historically, RSD have been considered congenital and true (made of all layers) as opposed to LSD considered to be mostly acquired and false (made of mucosa and muscularis mucosa)[1,32,33]. Instead, according to further studies was found that most[34,35] or even all[36,37] of the cases of RSD were actually false, both solitary and multiple. This demonstrates that the underlying pathophysiology has not yet been fully clarified and that the etiology of diverticular disease on the right-side and left-side is probably more similar than we think.
The incidence of diverticular disease has been increasing in both Europe and the United States[3]. Although acute right-sided colonic diverticulitis (ARCD) is still considered a rare disease in the western world, the real incidence is not that rare[38] ranging from 5% to 20%[3,5,28,39].
Historically, a century ago it was seen in early studies that the prevalence of RSD was higher than expected (2%-5%)[40,41]. As early as 1961, Miangolarra[42] firstly describes the diverticulitis of the right colon as “an important surgical problem”.
Nevertheless, the evidence of ARCD is almost exclusively based on single-center or case reports. In fact, we found only 5 studies reporting more than 20 patients, demonstrating that it is not a widespread reality and that it is often managed according to individual surgeons[9,12,25,26,28].
In patients affected by ARCD we found that the median age was 50.9 years and was higher in patients with the Hinchey stage II than Hinchey I (45.7 vs 63, 57 years)[26]. Also, in comparison studies, we found an earlier onset than LSD (53 vs 64 years)[16,23,28].
Patients affected by ARCD typically presented at the emergency department with fever, pain in the right iliac fossa and often signs of peritoneal irritation. Blood tests show leukocytosis and increased C-reactive protein[12-15,18,19,24-27]. Similar symptoms and young age are confounding factors and they can be wrongly identified with the diagnosis of acute appendicitis in most of the cases described[14,15,17,22].
Recently Zuckerman et al[28] reported that 67% of patients underwent an operation for a misdiagnosis of appendicitis. This illustrates the importance of accurate diagnostic criteria to avoid unnecessary appendectomy or even a right hemicolectomy.
In fact, the diagnostic accuracy we calculate in all the studies is a poor 32.2%, when the reported misdiagnosis rate is 38.39% (162 cases), where 56.79% of the time (92 cases) diagnosis is clearly mistaken for acute appendicitis.
Effective diagnosis is therefore the main achilles heel of ARCD. In some studies, nuanced differences emerge in the clinical presentation that could help us in the differential diagnosis such as the longer duration of symptoms[26], the presence of diarrhea in the weeks preceding the pain[21] and the absence of nausea and vomiting[20,23]. Making the correct diagnosis can be very difficult relying only on the clinical evaluation especially if we consider that the Alvarado score shows a poor negative predicting value in distinguishing acute appendicitis from ARCD[23].
The awareness of this condition and the use of the correct imaging can help us to increase the rate of correct diagnosis. So, in the Kalcan study there was a 100% misdiagnosis rate because no physician did radiological investigations[19].
According to Wilson et al[43], it is possible to make an ultrasound diagnosis of diverticulitis when there are two of the following features: thickening of the wall (≥ 4 mm), diverticula with signs of inflammation, inflammatory modifications in the pericolic fat, pericolic or intramural inflammatory mass and intramural fistulas.
We know that in expert hands sonography may allow a correct diagnosis of ARCD, directly or suspected by indirect sign[15]. We also know that has a limited utility in obese patients and is user dependent[24,32,44]; and especially in emergency cases, diagnosis of ARCD can be even more difficult without more advanced and objective imaging exams such as CT scan[19]. Therefore, the ultrasound should not be the only imaging technique in a case of suspected diverticulitis and magnetic resonance imaging (MRI) might be useful when CT is contraindicated[45,46]. Nevertheless, MRI is not always available in the emergency setting and rarely used[47]. In particular, in patients presenting with right lower abdominal pain, thin-section helical CT scan may identify or exclude other clinical conditions[48].
For both sonography and CT there are very specific diagnostic criteria for ARCD such as colonic wall thickening and edema, pericolic fat infiltration or abscess and extraluminal air around the colon[24].
In our review only 12.5% of cases were diagnosed via sonography compared to 70.6% of correct CT-driven diagnosis; while other methods of diagnosis have rarely been effective.
The importance of tomography is clear in the article by Cristaudo et al[21] in which CT scan was necessary to detect the pathology in 90% of cases. Also, in the study of Kaya et al[27] in which CT scan recognized aggressive liver cancer domains (ALCDs) where the sonography failed. Moreover, the CT scan shows the exact extent of the degree of inflammation in order to be able to accurately plan any surgical intervention[16].
Certainly, the diffusion and accessibility of this imaging technique improved the diagnostic accuracy, as can be seen from the increase in the diagnosis rate in two periods, before and after 2007, in Zuckerman's study[28].
Finally, when surgical exploration may be the only way to obtain an effective diagnosis and allow the most adequate treatment then the minimally invasive approach may be the most suitable way to do it[23].
For the first time, in the latest WSES 2020 update for the management of acute colonic diverticulitis in the emergency setting, ARCD is defined as a distinct clinical entity and the principles of diagnosis and treatment are suggested to be similar to those in ALCD. However, patients with RCD require surgery less often than patients with ALCD, but their management is not well defined, and no unique guidelines have been proposed until now[49].
The correct diagnosis is very important because it allows a conservative management to successfully treat uncomplicated ARCD (uARCD)[21,24,25].
But historically the treatment of ARCD has been mostly surgical and it has always remained at the discretion of the surgeon since the first reported surgical treatment of acute right-side diverticulitis was made by an American surgeon in 1954[50].
As for surgical treatment, there are multiple options for complicated forms such as conservative (appendectomy), limited (diverticulectomy), or extensive (ileocecal resection or right hemicolectomy[12,32,51].
Mostly the indication for surgery was secondary to a wrong diagnosis, leading to the aggressive choice of surgical procedures based on the intraoperative findings[16,23,25]. Lane et al[12] for example advocated diverticulectomy in cases of a solitary diverticulum, and immediate right hemicolectomy in the case of cecal phlegmon or multiple diverticula.
Over the years, the interventions have been less and more reasoned. If the inflamed area was limited, then a narrow diverticulum resection has been proposed as a safe and effective technique[20,23]. And this attitude was confirmed after a 14-year follow-up study, with a unique case of recurrence 8 years after the reported episode[15].
Furthermore, removing the appendix was also useful for two reasons. First, there was a “contiguous appendicitis” secondary to diverticular inflammation[15,25] and second because the removal of the appendix would have allowed a simpler diagnosis in case of a new episode of pain in the right iliac fossa[19,22,27].
As much as 40% of ARCD patients underwent right hemicolectomy after finding a mass mimicking colon cancer[32]. It is also true that in some cases the histological analysis on the surgical specimen found the presence of adenocarcinoma of the cecum associated with multiple diverticula[17]. According to Radhi et al[17], single diverticula are more present in young patients and tend to be symptomatic, while multiple diverticula are incidental findings or associated with carcinoma in older patients.
Intraoperative findings of suspected tumors or complicated patients with significant extent of diverticulitis remained therefore the only reasons for extensive surgery[15,16,19,20] and could potentially avoid a formation of diverting stoma[9].
Analyzing our research, we found a very low number of stoma (1.18%) and reoperations needed (2.5%). Furthermore, our results agree with the recent studies which shows that need for ostomy was significantly less frequent in the ARCD group than ALCD (6.3% vs 62.5%) probably also due to the more favorable anatomical location of right colon (being retroperitoneal may limit the spread of inflammation in contrast to sigmoid colon) with ileocolic anastomosis burdened by a lower risk of leak compared to the colorectal ones[52].
Although the use of laparoscopy was often secondary to a wrong diagnosis of acute appendicitis[9], since the first laparoscopic diverticulectomy was performed in 1994[53], a more careful selection of patients allowed in experienced hands to perform even colonic resection with primary anastomosis with minimally invasive approach[16,23].
Conversion was mainly due to the detection of small bowel dilatation or difficult clinical picture such as free fluid or big abscess when laparoscopic approach was initially chosen to perform appendectomy instead[23].
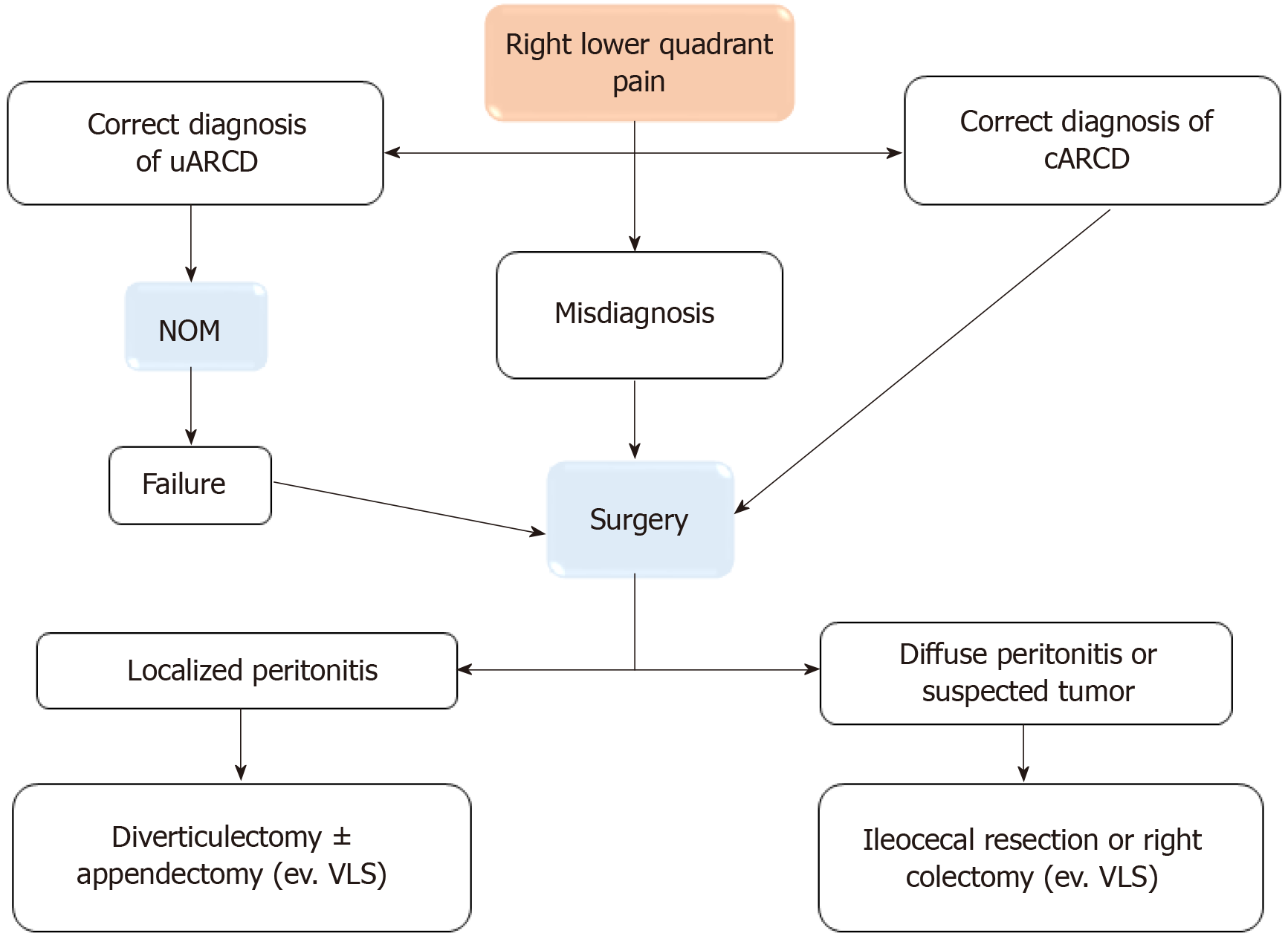
Finally, Hildebrand et al[16] stated that there was no big difference in the treatment of right-sided diverticulitis compared to left-sided diverticulitis. We confirm his conclusion, and we report in Figure 3 a synthesis of the therapeutic options highlighted in the therapeutic diagnostic algorithm inspired by the study of Kaya et al[27].
In our review we found a low recurrence rate (5.45%). Cristaudo et al[21] and Yardımcı et al[24] had no recurrence at all after NOM management, demonstrating the benign course of the disease. Other studies had a low range of recurrence (6%-21%). In fact, in the 23 cases of recurrence reported, 16 of which were successfully treated conservatively again[15,18,25-28]; seven cases of recurrence underwent surgery[12] and only two cases occurred after a previous NOM[25,28].
Eastern studies also show similar recurrence rate (1%-20.5%) after conservative management both for uncomplicated and recurrent RCD[54-56].
Zuckerman et al[28] also show a lower recurrence rate after ARCD compared with ALCD (4.1% vs 32.8%).
Furthermore, according to the analysis of Imaeda et al[1], there are fewer complicated RCDs than liver cancer domains (LCDs). In fact, the complication rate was also low (10.66%), with only 1.66% of major complications according to Clavien Dindo (CD) classifications (six reported CD 3 complications and only one CD4)[12,22,23,25].
A very important aspect was demonstrated by Courtot et al[25]as the recurrence rate was low and similar for both complicated and uncomplicated ARCD (6.8% and 8.8%, respectively) demonstrating the benign course of this condition.
Furthermore, in the Zuckerman et al[28] study it is shown that 5% of patients with an initial diagnosis of RCD subsequently developed colon cancer. And being a higher rate than average-risk[57], an endoscopic screening program for these patients could be scheduled.
Although the incidence of RSD is much higher in Asian countries, we have not found specific guidelines. Nonetheless, several authors have published studies showing their management for this condition.
For example, in two important studies the authors show that most cases of ARCD are uncomplicated (78.5% and 92.8%) and that they are successfully treated conservatively (reaching as much as 98% of cases)[58,59]. NOM is also effective in 41.7% of complicated ARCD (cARCD), reserving surgery only in the remaining cases and making it possible to convert an urgent intervention into an elective one.
In support of the efficacy of conservative treatment, two recent meta-analysis show similar results. In particular, they show a low recurrence rate after uncomplicated ARCD (10.9% and 12%). The first study[60] focused on the fact that only 4.4% of recurrences were complicated and there was only a 1.7% of re-recurrence rate. While the second[61] showed that only a small percentage of patients underwent surgery after recurrence (9.9% as urgent cases, 5.4% as elective cases). Both authors conclude that NOM is safe and feasible for Hinchey 1b-2 stages, similarly to the management of uncomplicated left-sided diverticulitis, while surgery should only be performed in selected cases.
The effectiveness of the NOM is even the background from which the authors started to design a prospective randomised controlled trial (RCT). Kim et al[62] compared the conservative treatment of uARCD with or without antibiotic obtaining similar results regarding to treatment failure rates (4.7% vs 1.6%), length of hospital stay and recurrence rate (7.8% vs 9.8%). Moreover, the group without antibiotics was burdened by a lower cost.
In the only recent study that defends the surgical approach, Luu et al[63] stated that laparoscopic diverticulectomy could be offered to selected patients (younger patients, who live in remote areas or with higher risks of recurrence). The author points out that, compared to conservative management, minimally invasive approach has similar outcomes in terms of complications (12.2% vs 8.6%) and treatment failure (13.5% vs 9.9%) and with a lower recurrence rate (0% vs 16.6%).
In this regard, there is some confusion on the main predictors of recurrence. In another study, multiple diverticula were found to be the main reason[64]. But this result seems to be disproved in the aforementioned RCT of Luu et al[63] in which fever and markers for inflammation were predictive, instead[62]. Other predictors were young age and longer duration of symptoms before hospital admission[65].
The management of ARCD remains a great challenge for surgeons. Although recent updates of WSES guidelines suggest that all the statements for ALCD may also apply to ARCD, several topics need to be investigated. Lack of diagnosis is the most important problem and CT scan seems to be the best imaging modality. NOM remains the preferred treatment in uncomplicated cases, whereas surgery should be considered in unstable patients or complicated disease. Laparoscopic approach should be offered whenever it is feasible. Further studies are needed in order to understand epide
This review underlines the importance to collect more data, especially in western countries, to understand if it’s a condition more common than we thought, and if we really need more selective guidelines or we can simply apply the principles already proposed for left side diverticulitis.
Right sided diverticulitis is very frequent in Asian countries, while in western countries it has always been considered very rare. On the other hand, in recent studies, the condition has been shown to be increasing in recent years.
Despite this rapid spread, there are no clear guidelines on the management of RSD. Until now, their management has been based on knowledge gained from left sided diverticulitis.
The authors therefore wanted to analyze the studies in the literature to have a broader and deeper point of view to understand what could be the correct management.
The authors analyzed the articles from western countries starting from 1990 in which the management and the subsequent outcome of right sided diverticulitis were shown.
The authors found that most cases of right colonic diverticulitis are treated effectively with non-operative management, reserving surgical treatment especially for complicated cases. Recurrences have a low rate and are also successfully treated conservatively.
Right sided diverticulitis has a similar management in both western and Asian countries.
Further studies will serve to identify more precisely which cases should be reserved for surgical treatment.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Preda SD, Sasaki Y S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Imaeda H, Hibi T. The Burden of Diverticular Disease and Its Complications: West vs East. Inflamm Intest Dis. 2018;3:61-68. [PubMed] [DOI] [Full Text] |
| 2. | Markham NI, Li AK. Diverticulitis of the right colon--experience from Hong Kong. Gut. 1992;33:547-549. [PubMed] [DOI] [Full Text] |
| 3. | Faucheron JL, Roblin X, Bichard P, Heluwaert F. The prevalence of right-sided colonic diverticulosis and diverticular haemorrhage. Colorectal Dis. 2013;15:e266-e270. [PubMed] [DOI] [Full Text] |
| 4. | Blachut K, Paradowski L, Garcarek J. Prevalence and distribution of the colonic diverticulosis. Review of 417 cases from Lower Silesia in Poland. Rom J Gastroenterol. 2004;13:281-285. [PubMed] |
| 5. | De Cecco CN, Ciolina M, Annibale B, Rengo M, Bellini D, Muscogiuri G, Maruotti A, Saba L, Iafrate F, Laghi A. Prevalence and distribution of colonic diverticula assessed with CT colonography (CTC). Eur Radiol. 2016;26:639-645. [PubMed] [DOI] [Full Text] |
| 6. | Potier F. Diverticulite et appendicite. Bulletins et Memoires de la Societe Anatomique de Paris. 1912;71:29-31. |
| 7. | Telling WHM, Gruner OC. Acquired diverticula, diverticulitis, and peridiverticulities of the large intestine. Br J Surg. 2006;4:468-530. [DOI] [Full Text] |
| 8. | Schlussel AT, Lustik MB, Cherng NB, Maykel JA, Hatch QM, Steele SR. Right-Sided Diverticulitis Requiring Colectomy: an Evolving Demographic? J Gastrointest Surg. 2016;20:1874-1885. [PubMed] [DOI] [Full Text] |
| 9. | Al-Temimi MH, Trujillo CN, Mahlberg S, Ruan J, Nguyen P, Yuhan R, Carmichael JC. Surgical Intervention for Right-Side Diverticulitis: A Case-Matched Comparison with Left-Side Diverticulitis. Am Surg. 2018;84:1608-1612. [PubMed] [DOI] [Full Text] |
| 10. | Wasvary H, Turfah F, Kadro O, Beauregard W. Same hospitalization resection for acute diverticulitis. Am Surg. 1999;65:632-5; discussion 636. [PubMed] |
| 11. | Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [PubMed] [DOI] [Full Text] |
| 12. | Lane JS, Sarkar R, Schmit PJ, Chandler CF, Thompson JE Jr. Surgical approach to cecal diverticulitis. J Am Coll Surg. 1999;188:629-34; discussion 634. [PubMed] [DOI] [Full Text] |
| 13. | Violi V, Roncoroni L, Boselli AS, Trivelli M, Peracchia A. Diverticulitis of the caecum and ascending colon: an unavoidable diagnostic pitfall? Int Surg. 2000;85:39-47. [PubMed] [DOI] [Full Text] |
| 14. | Junge K, Marx A, Peiper Ch, Klosterhalfen B, Schumpelick V. Caecal-diverticulitis: a rare differential diagnosis for right-sided lower abdominal pain. Colorectal Dis. 2003;5:241-245. [PubMed] [DOI] [Full Text] |
| 15. | Papaziogas B, Makris J, Koutelidakis I, Paraskevas G, Oikonomou B, Papadopoulos E, Atmatzidis K. Surgical management of cecal diverticulitis: is diverticulectomy enough? Int J Colorectal Dis. 2005;20:24-27. [PubMed] [DOI] [Full Text] |
| 16. | Hildebrand P, Kropp M, Stellmacher F, Roblick UJ, Bruch HP, Schwandner O. Surgery for right-sided colonic diverticulitis: results of a 10-year-observation period. Langenbecks Arch Surg. 2007;392:143-147. [PubMed] [DOI] [Full Text] |
| 17. | Radhi JM, Ramsay JA, Boutross-Tadross O. Diverticular disease of the right colon. BMC Res Notes. 2011;4:383. [PubMed] [DOI] [Full Text] |
| 18. | Issa N, Paran H, Yasin M, Neufeld D. Conservative treatment of right-sided colonic diverticulitis. Eur J Gastroenterol Hepatol. 2012;24:1254-1258. [PubMed] [DOI] [Full Text] |
| 19. | Kalcan S, Başak F, Hasbahçeci M, Kılıç A, Canbak T, Kudaş İ, Baş G, Alimoğlu O. Intraoperative diagnosis of cecal diverticulitis during surgery for acute appendicitis: Case series. Ulus Cerrahi Derg. 2016;32:54-57. [PubMed] [DOI] [Full Text] |
| 20. | Hot S, Eğin S, Gökçek B, Yeşiltaş M, Alemdar A, Akan A, Karahan SR. Solitary caecum diverticulitis mimicking acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2015;21:520-523. [PubMed] [DOI] [Full Text] |
| 21. | Cristaudo A, Pillay P, Naidu S. Caecal diverticulitis: Presentation and management. Ann Med Surg (Lond). 2015;4:72-75. [PubMed] [DOI] [Full Text] |
| 22. | Koshy RM, Abusabeib A, Al-Mudares S, Khairat M, Toro A, Di Carlo I. Intraoperative diagnosis of solitary cecal diverticulum not requiring surgery: is appendectomy indicated? World J Emerg Surg. 2016;11:1. [PubMed] [DOI] [Full Text] |
| 23. | Monari F, Cervellera M, Pirrera B, D'Errico U, Vaccari S, Alberici L, Tonini V. Right-sided acute diverticulitis: A single Western center experience. Int J Surg. 2017;44:128-131. [PubMed] [DOI] [Full Text] |
| 24. | Yardımcı E, Hasbahçeci M, İdiz UO, Atay M, Akbulut H. Is surgery necessary to confirm diagnosis of right-sided diverticulitis in spite of relevant clinical and radiological findings? Ulus Travma Acil Cerrahi Derg. 2017;23:61-65. [PubMed] [DOI] [Full Text] |
| 25. | Courtot L, Bridoux V, Lakkis Z, Piessen G, Manceau G, Mulliri A, Meurette G, Bouayed A, Vénara A, Blanc B, Tabchouri N, Salamé E, Ouaïssi M. Long-term outcome and management of right colonic diverticulitis in western countries: Multicentric Retrospective Study. J Visc Surg. 2019;156:296-304. [PubMed] [DOI] [Full Text] |
| 26. | Destek S, Gül VO. Effectiveness of conservative approach in right colon diverticulitis. Ulus Travma Acil Cerrahi Derg. 2019;25:396-402. [PubMed] [DOI] [Full Text] |
| 27. | Kaya C, Celayir MF, Bozkurt E, Omeroglu S, Guven O, Mihmanli M. Solitary caecal diverticulitis: Comparison of operative and non operative treatment. J Pak Med Assoc. 2020;70:1926-1929. [PubMed] [DOI] [Full Text] |
| 28. | Zuckerman J, Garfinkle R, Vasilevksy CA, Ghitulescu G, Faria J, Morin N, Boutros M. Short- and Long-Term Outcomes of Right-Sided Diverticulitis: Over 15 Years of North American Experience. World J Surg. 2020;44:1994-2001. [PubMed] [DOI] [Full Text] |
| 29. | Hellwig I, Böttner M, Barrenschee M, Harde J, Egberts JH, Becker T, Wedel T. Alterations of the enteric smooth musculature in diverticular disease. J Gastroenterol. 2014;49:1241-1252. [PubMed] [DOI] [Full Text] |
| 30. | Wess L, Eastwood MA, Wess TJ, Busuttil A, Miller A. Cross linking of collagen is increased in colonic diverticulosis. Gut. 1995;37:91-94. [PubMed] [DOI] [Full Text] |
| 31. | Hobson KG, Roberts PL. Etiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2004;17:147-153. [PubMed] [DOI] [Full Text] |
| 32. | Puylaert JB. Ultrasound of colon diverticulitis. Dig Dis. 2012;30:56-59. [PubMed] [DOI] [Full Text] |
| 33. | Hawkins AT, Wise PE, Chan T, Lee JT, Glyn T, Wood V, Eglinton T, Frizelle F, Khan A, Hall J, Ilyas MIM, Michailidou M, Nfonsam VN, Cowan ML, Williams J, Steele SR, Alavi K, Ellis CT, Collins D, Winter DC, Zaghiyan K, Gallo G, Carvello M, Spinelli A, Lightner AL. Diverticulitis: An update from the age old Paradigm. Curr Probl Surg. 2020;57:100863. [PubMed] [DOI] [Full Text] |
| 34. | Shukla HS. LE Hughes: watch him do it and you will learn it. J Surg Oncol. 2006;93:597-600. [PubMed] [DOI] [Full Text] |
| 35. | Pieterse AS, Rowland R, Miliauskas JR, Hoffmann DC. Right-sided diverticular disease of the colon: a morphological analysis of 16 cases. Aust N Z J Surg. 1986;56:471-475. [PubMed] [DOI] [Full Text] |
| 36. | Pace JL, Podestà MT. Diverticular Disease of Right Colon: Report of 7 Post-Mortem Cases. Proc R Soc Med. 1974;67:1044-1044. [PubMed] [DOI] [Full Text] |
| 37. | Lee YS. Diverticular disease of the large bowel in Singapore. An autopsy survey. Dis Colon Rectum. 1986;29:330-335. [PubMed] [DOI] [Full Text] |
| 38. | Golder M, Ster IC, Babu P, Sharma A, Bayat M, Farah A. Demographic determinants of risk, colon distribution and density scores of diverticular disease. World J Gastroenterol. 2011;17:1009-1017. [PubMed] [DOI] [Full Text] |
| 39. | Sharara AI, Ziade N, Shayto RH, Rustom LBO, Chehab H, Rimmani HH, Hanna K, Chalhoub JM, Sarkis FS, Rahal MA, Soweid A, Mourad FH, Barada K, Harb AH. The Natural History of Incidental Colonic Diverticulosis on Screening Colonoscopy. Can J Gastroenterol Hepatol. 2018;2018:3690202. [PubMed] [DOI] [Full Text] |
| 40. | Ochsner HC, Bargen JA. Diverticulosis of the Large Intestine; an Evaluation of Historical and Personal Observations. Ann Intern Med. 1935;9:282-296. [DOI] [Full Text] |
| 41. | Wilkinson SA. Diverticulosis and Diverticulitis of the Colon. N Engl J Med. 1933;209:197-202. [DOI] [Full Text] |
| 42. | Miangolarra CJ. Diverticulitis of the right colon: an important surgical problem. Ann Surg. 1961;153:861-870. [PubMed] [DOI] [Full Text] |
| 43. | Wilson SR, Toi A. The value of sonography in the diagnosis of acute diverticulitis of the colon. AJR Am J Roentgenol. 1990;154:1199-1202. [PubMed] [DOI] [Full Text] |
| 44. | Kameda T, Kawai F, Taniguchi N, Kobori Y. Usefulness of transabdominal ultrasonography in excluding adnexal disease. J Med Ultrason (2001). 2016;43:63-70. [PubMed] [DOI] [Full Text] |
| 45. | Nielsen K, Richir MC, Stolk TT, van der Ploeg T, Moormann GR, Wiarda BM, Schreurs WH. The limited role of ultrasound in the diagnostic process of colonic diverticulitis. World J Surg. 2014;38:1814-1818. [PubMed] [DOI] [Full Text] |
| 46. | Hall J, Hammerich K, Roberts P. New paradigms in the management of diverticular disease. Curr Probl Surg. 2010;47:680-735. [PubMed] [DOI] [Full Text] |
| 47. | Destigter KK, Keating DP. Imaging update: acute colonic diverticulitis. Clin Colon Rectal Surg. 2009;22:147-155. [PubMed] [DOI] [Full Text] |
| 48. | Jang HJ, Lim HK, Lee SJ, Lee WJ, Kim EY, Kim SH. Acute diverticulitis of the cecum and ascending colon: the value of thin-section helical CT findings in excluding colonic carcinoma. AJR Am J Roentgenol. 2000;174:1397-1402. [PubMed] [DOI] [Full Text] |
| 49. | Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R, Ceresoli M, Chiara O, Chiarugi M, Coimbra R, Cortese F, Cui Y, Damaskos D, De' Angelis GL, Delibegovic S, Demetrashvili Z, De Simone B, Di Marzo F, Di Saverio S, Duane TM, Faro MP, Fraga GP, Gkiokas G, Gomes CA, Hardcastle TC, Hecker A, Karamarkovic A, Kashuk J, Khokha V, Kirkpatrick AW, Kok KYY, Inaba K, Isik A, Labricciosa FM, Latifi R, Leppäniemi A, Litvin A, Mazuski JE, Maier RV, Marwah S, McFarlane M, Moore EE, Moore FA, Negoi I, Pagani L, Rasa K, Rubio-Perez I, Sakakushev B, Sato N, Sganga G, Siquini W, Tarasconi A, Tolonen M, Ulrych J, Zachariah SK, Catena F. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. [PubMed] [DOI] [Full Text] |
| 50. | Mears TW, Judd ES Jr, Martin J. Diverticulitis of the right side of the colon, with report of a case of diverticulitis of the hepatic flexure. Proc Staff Meet Mayo Clin. 1954;29:410-415. [PubMed] |
| 51. | Papapolychroniadis C, Kaimakis D, Fotiadis P, Karamanlis E, Stefopoulou M, Kouskouras K, Dimitriadis A, Harlaftis N. Perforated diverticulum of the caecum. A difficult preoperative diagnosis. Report of 2 cases and review of the literature. Tech Coloproctol. 2004;8 Suppl 1:s116-s118. [PubMed] [DOI] [Full Text] |
| 52. | Hyman N, Manchester TL, Osler T, Burns B, Cataldo PA. Anastomotic leaks after intestinal anastomosis: it's later than you think. Ann Surg. 2007;245:254-258. [PubMed] [DOI] [Full Text] |
| 53. | Rubio PA. Laparoscopic resection of a solitary cecal diverticulum. J Laparoendosc Surg. 1994;4:281-285. [PubMed] [DOI] [Full Text] |
| 54. | Park HC, Chang MY, Lee BH. Nonoperative management of right colonic diverticulitis using radiologic evaluation. Colorectal Dis. 2010;12:105-108. [PubMed] [DOI] [Full Text] |
| 55. | Komuta K, Yamanaka S, Okada K, Kamohara Y, Ueda T, Makimoto N, Shiogama T, Furui J, Kanematsu T. Toward therapeutic guidelines for patients with acute right colonic diverticulitis. Am J Surg. 2004;187:233-237. [PubMed] [DOI] [Full Text] |
| 56. | Yang HR, Huang HH, Wang YC, Hsieh CH, Chung PK, Jeng LB, Chen RJ. Management of right colon diverticulitis: a 10-year experience. World J Surg. 2006;30:1929-1934. [PubMed] [DOI] [Full Text] |
| 57. | Niv Y, Hazazi R, Levi Z, Fraser G. Screening colonoscopy for colorectal cancer in asymptomatic people: a meta-analysis. Dig Dis Sci. 2008;53:3049-3054. [PubMed] [DOI] [Full Text] |
| 58. | Chiu TC, Chou YH, Tiu CM, Chiou HJ, Wang HK, Lai YC, Chiou YY. Right-Sided Colonic Diverticulitis: Clinical Features, Sonographic Appearances, and Management. J Med Ultrasound. 2017;25:33-39. [PubMed] [DOI] [Full Text] |
| 59. | Chung BH, Ha GW, Lee MR, Kim JH. Management of Colonic Diverticulitis Tailored to Location and Severity: Comparison of the Right and the Left Colon. Ann Coloproctol. 2016;32:228-233. [PubMed] [DOI] [Full Text] |
| 60. | Lee JH, Ahn BK, Lee KH. Conservative treatment of uncomplicated right-sided diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2021;. [PubMed] [DOI] [Full Text] |
| 61. | Lee YF, Tang DD, Patel SH, Battaglia MA, Shanker BA, Cleary RK. Recurrence of Acute Right Colon Diverticulitis Following Nonoperative Management: A Systematic Review and Meta-analysis. Dis Colon Rectum. 2020;63:1466-1473. [PubMed] [DOI] [Full Text] |
| 62. | Kim JY, Park SG, Kang HJ, Lim YA, Pak KH, Yoo T, Cho WT, Shin DW, Kim JW. Prospective randomized clinical trial of uncomplicated right-sided colonic diverticulitis: antibiotics vs no antibiotics. Int J Colorectal Dis. 2019;34:1413-1420. [PubMed] [DOI] [Full Text] |
| 63. | Luu LH, Vuong NL, Yen VTH, Phuong DTT, Vu BK, Thanh NV, Khanh NT, Van Hai N. Laparoscopic diverticulectomy vs non-operative treatment for uncomplicated right colonic diverticulitis. Surg Endosc. 2020;34:2019-2027. [PubMed] [DOI] [Full Text] |