Published online Dec 27, 2021. doi: 10.4240/wjgs.v13.i12.1638
Peer-review started: March 27, 2021
First decision: June 14, 2021
Revised: June 21, 2021
Accepted: November 26, 2021
Article in press: November 26, 2021
Published online: December 27, 2021
Processing time: 271 Days and 6.7 Hours
Giant hiatal hernias still pose a major challenge to digestive surgeons, and their repair is sometimes a highly complex task. This is usually performed by laparoscopy, while the role of the thoracoscopic approach has yet to be clearly defined.
To preoperatively detect patients with a giant hiatal hernia in whom it would not be safe to perform laparoscopic surgery and who, therefore, would be candidates for a thoracoscopic approach.
In the present study, using imaging test we preoperatively simulate the field of vision of the camera and the working area (instrumental access) that can be obtained in each patient when the laparoscopic approach is used.
From data obtained, we can calculate the access angles that will be obtained in a preoperative computerised axial tomography coronal section, according to the location of the trocar. We also provide the formula for performing the angle calculations If the trocars are placed in loss common situations, thus enabling us to determine the visibility and manoeuvrability for any position of the trocars.
The working area determines the cases in which we can operate safely and those in which certain areas of the hernia cannot be accessed, which is when the thoracoscopic approach would be safer.
Core Tip: This study was conducted to determine the accessibility obtained when the laparoscopic approach is applied to the repair of a giant hiatal hernia. The main study aim is to detect cases in which full access to all areas of the hernial sac is not possible, and in which, therefore, the thoracoscopic approach would be safer.
- Citation: Lara FJP, Zubizarreta Jimenez R, Moya Donoso FJ, Hernández Gonzalez JM, Prieto-Puga Arjona T, del Rey Moreno A, Pitarch Martinez M. Preoperative calculation of angles of vision and working area in laparoscopic surgery to treat a giant hiatal hernia. World J Gastrointest Surg 2021; 13(12): 1638-1650
- URL: https://www.wjgnet.com/1948-9366/full/v13/i12/1638.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i12.1638
A hiatal hernia is the protrusion of abdominal contents into the mediastinum through the diaphragmatic hiatus. It is a common condition in the general population and, due to the progressive aging of the population, is expected to become more so[1].
Hiatal hernias are classified into four types according to their anatomical characteristics[2-7]. Type 1 ("Sliding"), the most common, is a herniation of the oesophagogastric junction above the diaphragm, propelling the stomach into the abdomen. Type 2 (“Pure para-oesophageal”) is the thoracic migration of the gastric fundus while the oesophagogastric junction remains in the correct position. Type 3 ("Mixed") combines the components of Types 1 and 2. Type 4 ("Giant"), occurs when the hernia affects the entire stomach and other abdominal viscera, including the colon, omentum, small intestine, liver and spleen[8].
However, the term "Giant para-oesophageal hernia" is imprecise. The term "giant" is subject to interpretation, and although there is no consensus as to what percentage of the stomach should rise into the thorax for the hernia to be defined as “giant”, most authors agree that this category represents 5%-10% of all hiatal hernias[9].
The standard treatment for a hiatal hernia is to reduce the capacity of the abdominal cavity, to close the defect and to perform an anti-reflux procedure, usually by means of 360º (Nissen) fundoplication.
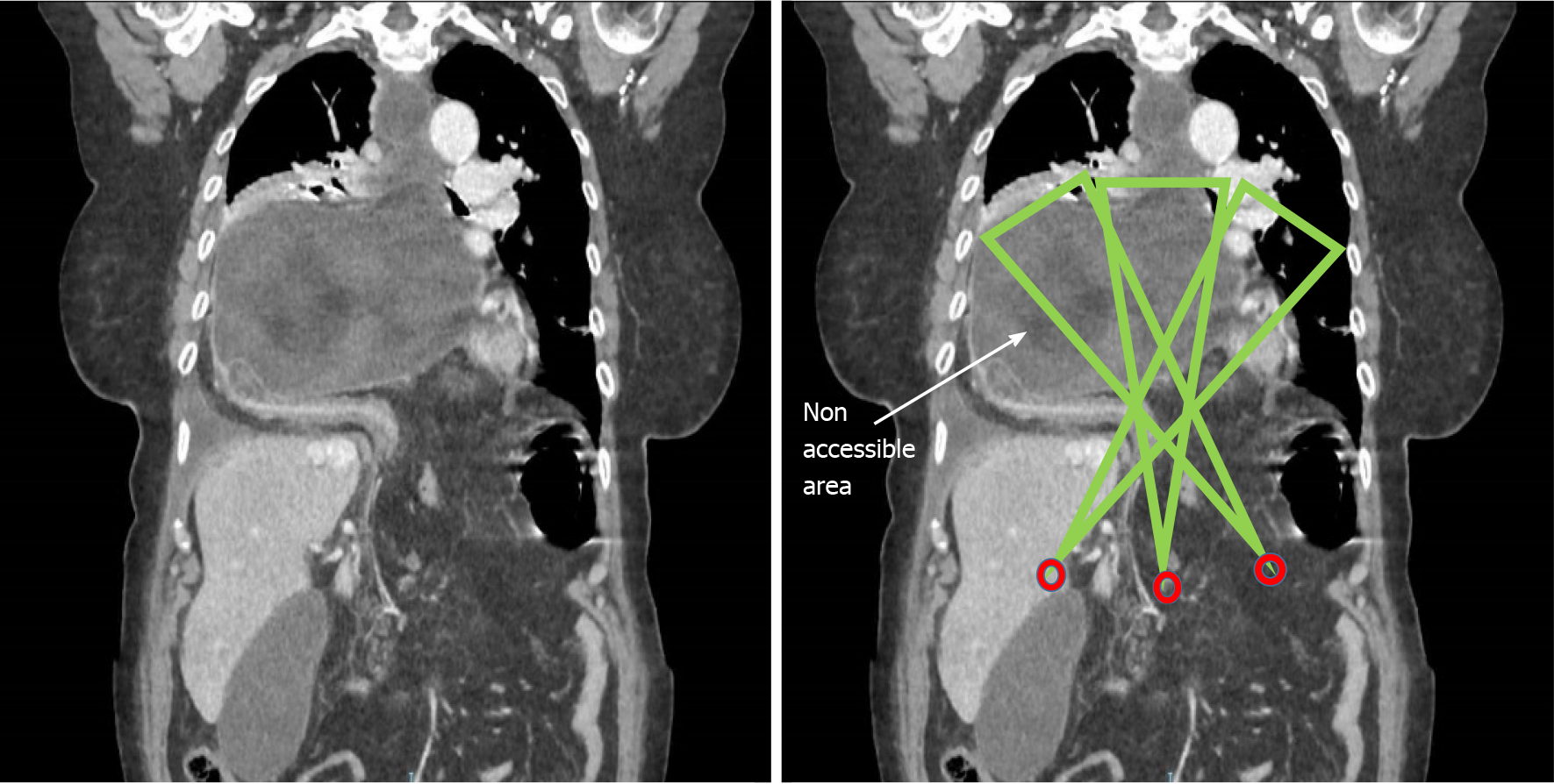
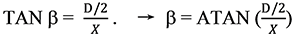
When the hernia is large, it is sometimes difficult to dissect the sac to reduce the hernia, and so ‘dark’ areas may remain, which cannot be accessed through the abdominal approach, due either to an insufficient angle of vision or to an insufficient instrument working angle (the apparatus cannot reach the operative site). In the present article, we derive the information necessary to assess visual (camera) and working (instrumental) access to all parts of the intrathoracic hernial sac, making it possible to confirm whether the laparoscopic approach is safe and reliable, or on the contrary, whether a thoracic approach would be necessary.
As observed above, with giant hernias, it is sometimes not possible to achieve full visibility of all areas of the sac using the laparoscopic approach. For this reason, we describe a procedure by which the angles of vision and the instrument working angle needed during the intervention can be preoperatively assessed by simulation in a computerised axial tomography (CAT) scan. The information thus obtained will reveal whether it is safe to use a laparoscopic approach or whether a thoracoscopic approach is needed.
By determining certain parameters – the camera angle aperture, the diameter of the hernial orifice and the positioning of the trocars with respect to this orifice – we can calculate the angle of vision and the instrument working angle available during the intervention. The angle of vision is defined as the visual field of the intrathoracic content into which the optical instrument must be inserted through the hernial orifice. The instrument working angle is the available access to the different parts of the intrathoracic hernial content by means of which the instruments can be delivered through the hiatal hernial orifice.
The procedure consists in performing a simulation with a preoperative thoraco-abdominal CAT scan of all patients with a giant hiatal hernia. In the coronal plane, we evaluate the angles of vision and the instrument working angles that will be obtained, according to where the trocars are located. This will reveal whether there are any hidden areas that are inaccessible visually or with surgical instruments.
The following methods are used to calculate these angles.
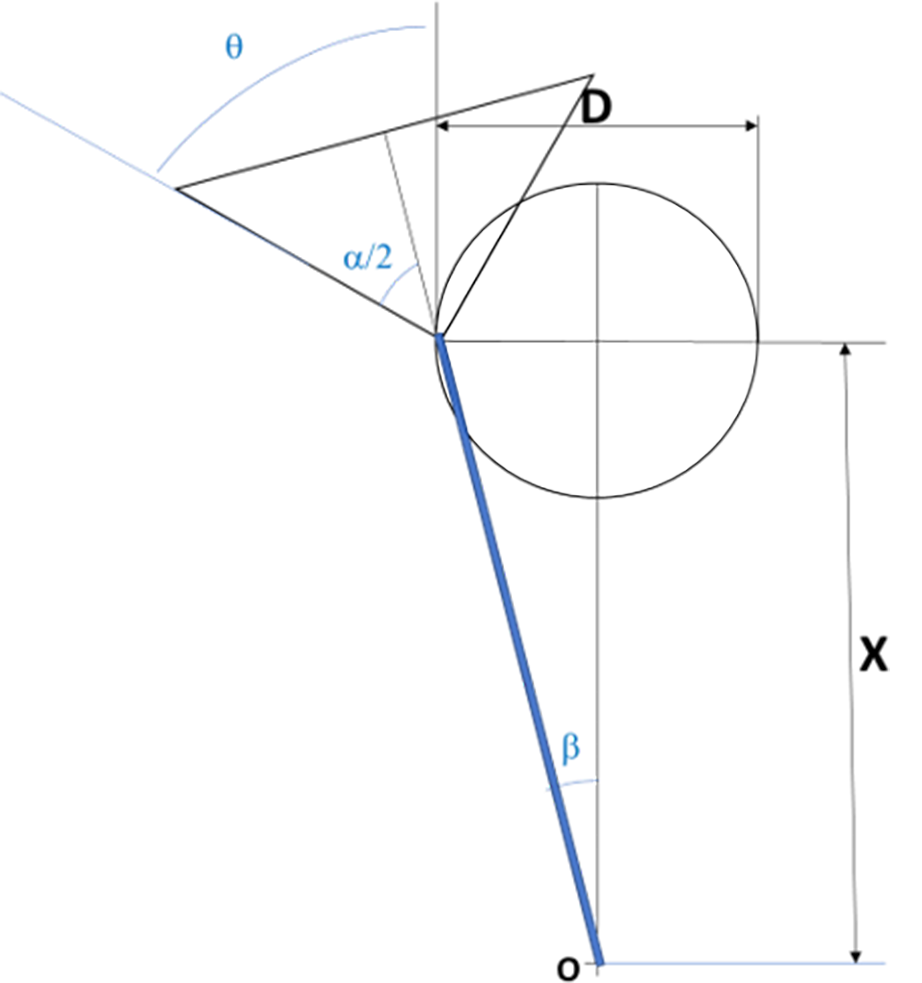
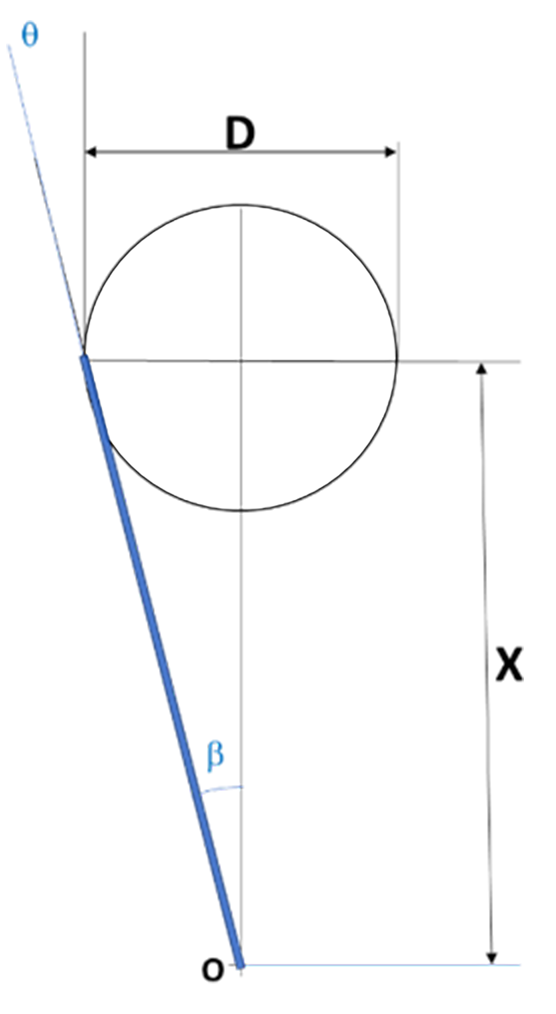
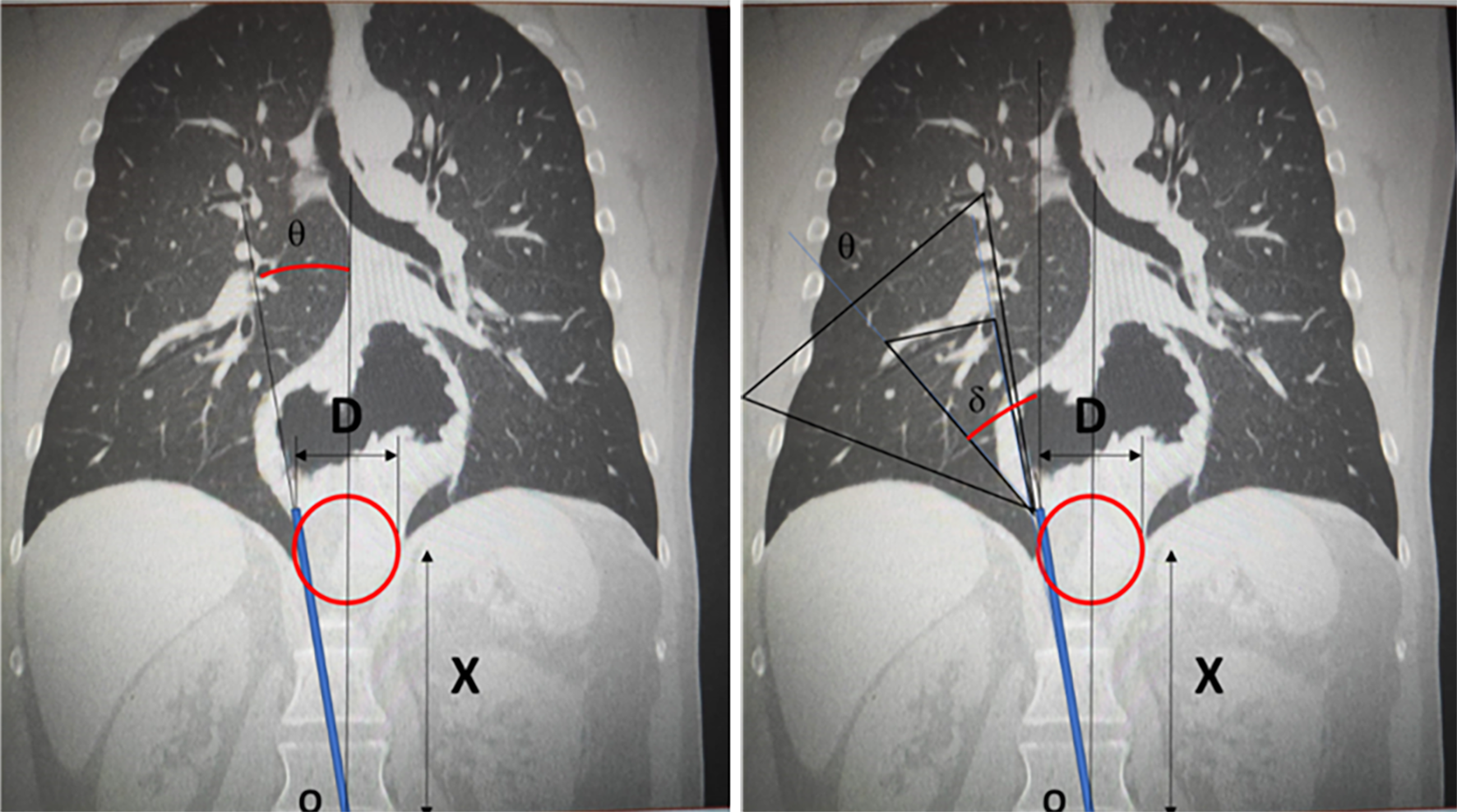
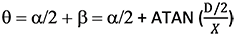
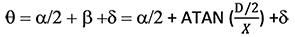
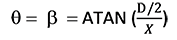
To evaluate the angle of vision, consider the geometry shown in Figure 1, regarding a laparoscopic intervention. The entry point for the instruments is marked with point O, which for simplicity is assumed to be centred with respect to the hernial orifice within the cavity, of diameter D. The distance between point O and the centre of the hernial orifice is labelled X, and b is the angle from the vertical, from point O to the maximum point of entry of the instruments.
The greatest angle of view that the camera can achieve is obtained when the camera inserted via the entry point reaches the hernial orifice. From here, the camera’s angle of vision (a) can be projected.
Considering the geometric relationship between the distances and the angles, the angle q can be calculated as follows, from the camera’s angle of vision (data supplied by the manufacturer), distance X and the diameter of circle D.
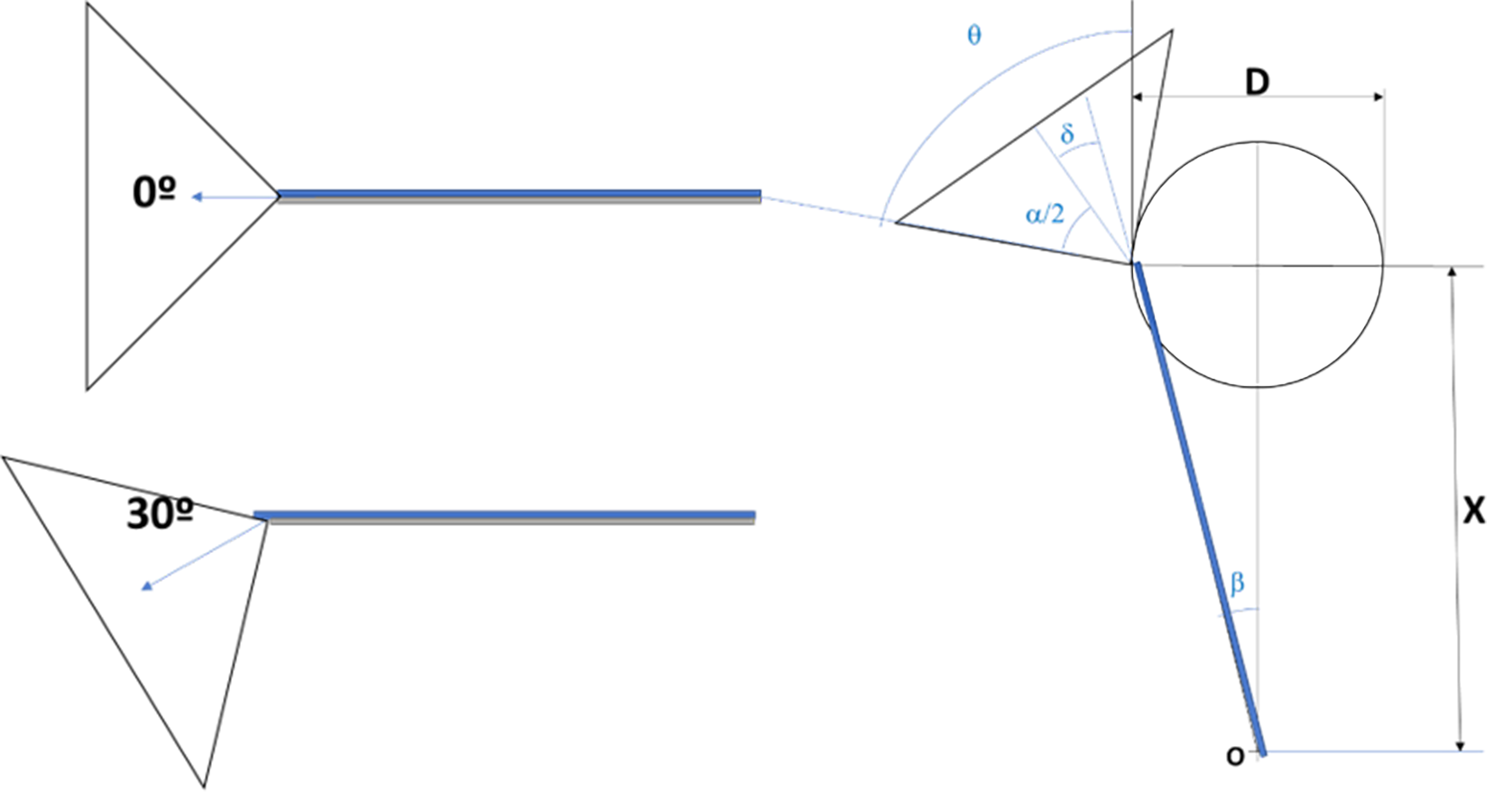
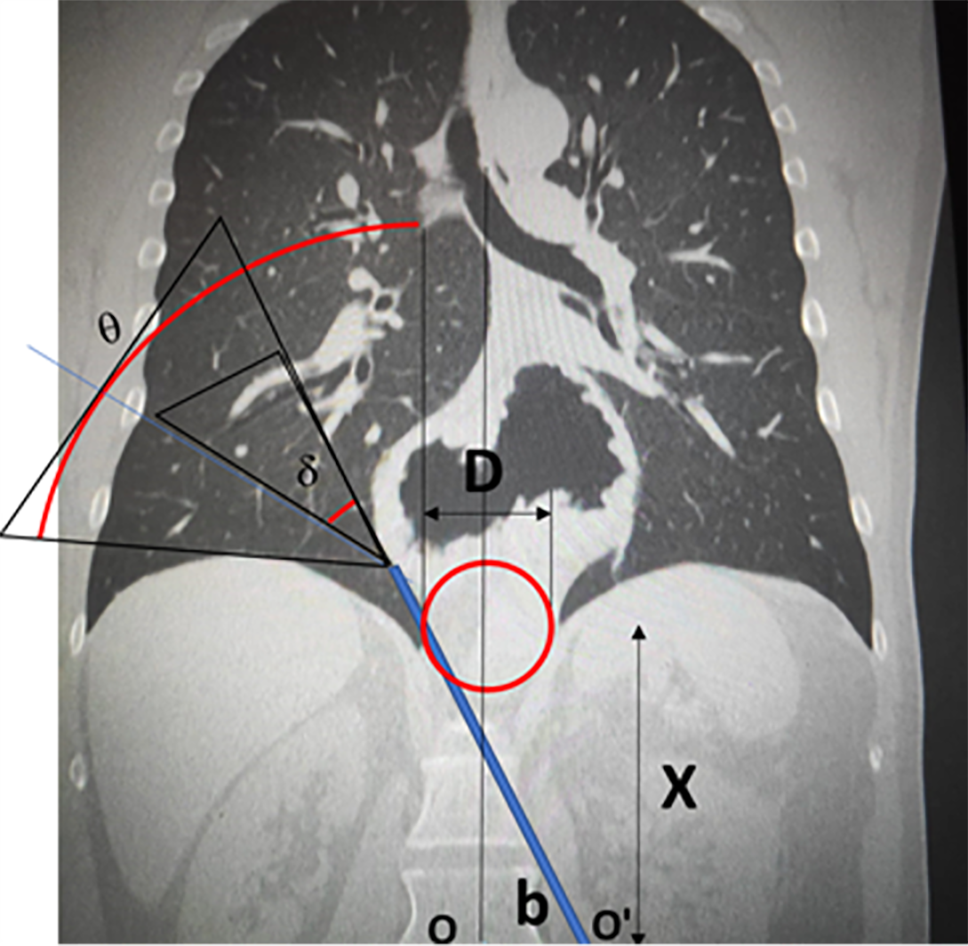
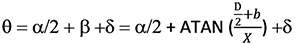
The camera can sometimes be bevelled to increase the angle of vision, rotating it through the angle d. Figure 2 shows how the bevel arrangement expands the angle of vision. When a bevel angle of d is introduced, the equation then becomes:
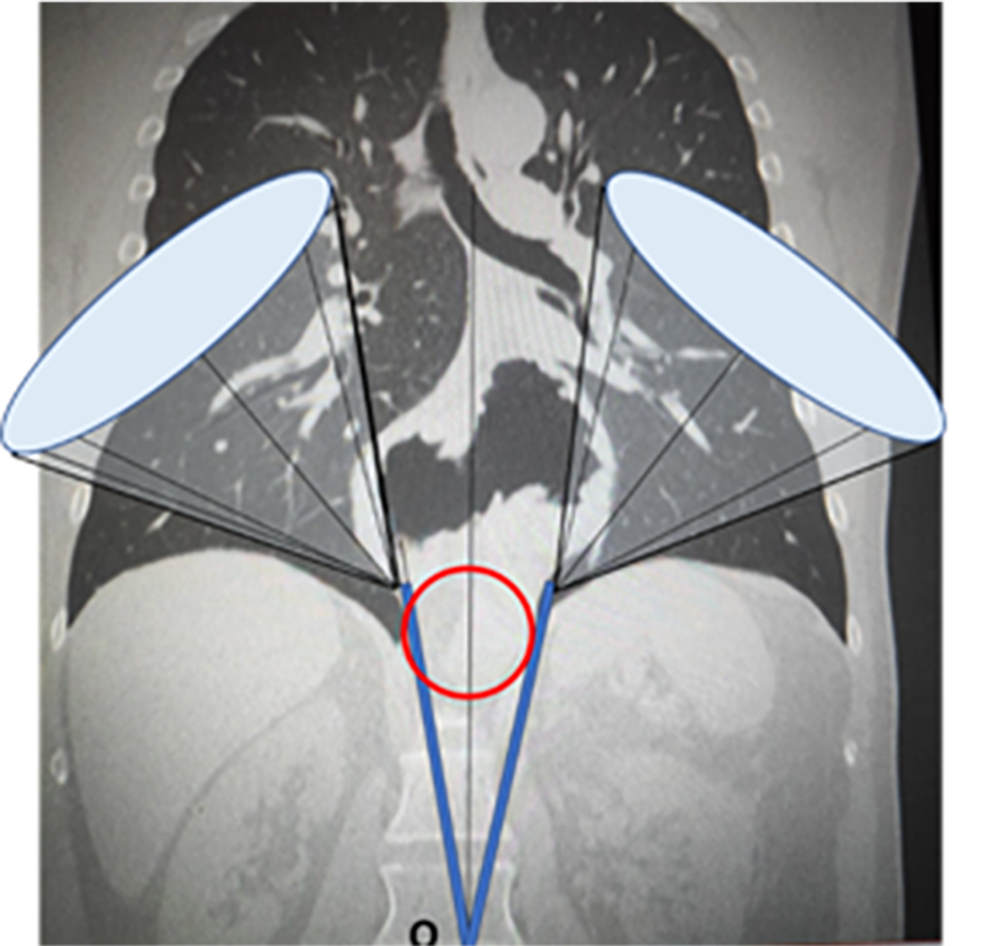
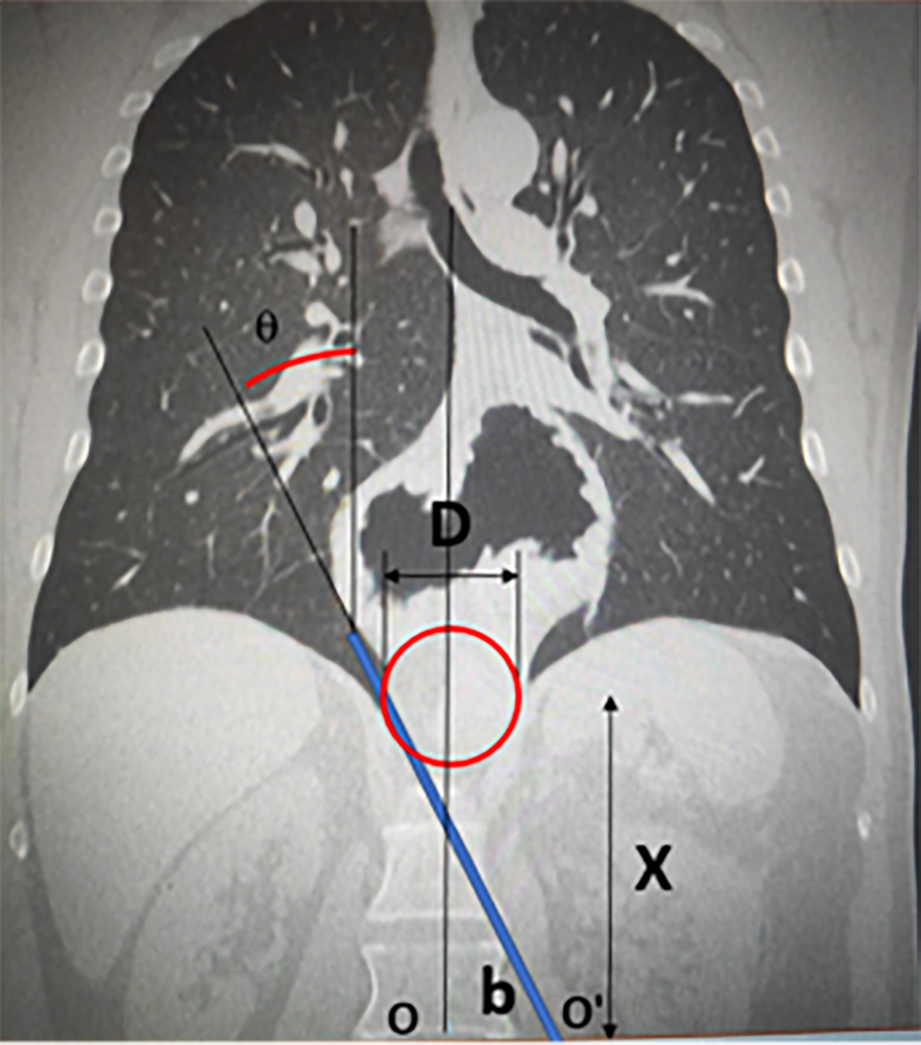
These expressions allow us to evaluate the cone of vision for the instrument working area. Figure 3 shows the projection of this cone on the CAT scan, to illustrate the geometric concept.
Figure 4 shows the geometric model for the laparoscopy instruments.
In this case, the additional angles a and d cannot be applied to the operating instruments since the heads cannot be rotated. The maximum angle that can be achieved with the stipulated geometry is then calculated as follows:
From the above expressions, the maximum viewing and working angles can be calculated, using the corresponding dimensions for each patient. By way of example, and to facilitate the evaluation, Figure 5 shows the CAT image, from which the dimensions for the D and X values can be taken to calculate the angle q.
Tables 1, 2 and 3 detail the values of angle q for the different geometric values observed in the intervention, with a camera angle of vision of a = 60º and a bevel angle d of 0º or 30º.
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 35.71 | 38.53 | 41.31 | 44.04 | 46.70 | 49.29 | 51.80 | 54.23 | 56.57 |
| 11 | 35.19 | 37.77 | 40.30 | 42.80 | 45.26 | 47.65 | 49.98 | 52.25 | 54.44 |
| 12 | 34.76 | 37.13 | 39.46 | 41.77 | 44.04 | 46.26 | 48.43 | 50.56 | 52.62 |
| 13 | 34.40 | 36.58 | 38.75 | 40.89 | 42.99 | 45.07 | 47.10 | 49.09 | 51.04 |
| 14 | 34.09 | 36.12 | 38.13 | 40.12 | 42.09 | 44.04 | 45.95 | 47.82 | 49.65 |
| 15 | 33.81 | 35.71 | 37.59 | 39.46 | 41.31 | 43.13 | 44.93 | 46.70 | 48.43 |
| 16 | 33.58 | 35.36 | 37.13 | 38.88 | 40.62 | 42.34 | 44.04 | 45.71 | 47.35 |
| 17 | 33.37 | 35.04 | 36.71 | 38.37 | 40.01 | 41.63 | 43.24 | 44.83 | 46.39 |
| 18 | 33.18 | 34.76 | 36.34 | 37.91 | 39.46 | 41.00 | 42.53 | 44.04 | 45.52 |
| 19 | 33.01 | 34.51 | 36.01 | 37.50 | 38.97 | 40.44 | 41.89 | 43.32 | 44.74 |
| 20 | 32.86 | 34.29 | 35.71 | 37.13 | 38.53 | 39.93 | 41.31 | 42.68 | 44.04 |
| 21 | 32.73 | 34.09 | 35.44 | 36.79 | 38.13 | 39.46 | 40.78 | 42.09 | 43.39 |
| 22 | 32.60 | 33.90 | 35.19 | 36.48 | 37.77 | 39.04 | 40.30 | 41.56 | 42.80 |
| 23 | 32.49 | 33.73 | 34.97 | 36.20 | 37.43 | 38.65 | 39.87 | 41.07 | 42.26 |
| 24 | 32.39 | 33.58 | 34.76 | 35.95 | 37.13 | 38.30 | 39.46 | 40.62 | 41.77 |
| 25 | 32.29 | 33.43 | 34.57 | 35.71 | 36.84 | 37.97 | 39.09 | 40.20 | 41.31 |
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 65.71 | 68.53 | 71.31 | 74.04 | 76.70 | 79.29 | 81.80 | 84.23 | 86.57 |
| 11 | 65.19 | 67.77 | 70.30 | 72.80 | 75.26 | 77.65 | 79.98 | 82.25 | 84.44 |
| 12 | 64.76 | 67.13 | 69.46 | 71.77 | 74.04 | 76.26 | 78.43 | 80.56 | 82.62 |
| 13 | 64.40 | 66.58 | 68.75 | 70.89 | 72.99 | 75.07 | 77.10 | 79.09 | 81.04 |
| 14 | 64.09 | 66.12 | 68.13 | 70.12 | 72.09 | 74.04 | 75.95 | 77.82 | 79.65 |
| 15 | 63.81 | 65.71 | 67.59 | 69.46 | 71.31 | 73.13 | 74.93 | 76.70 | 78.43 |
| 16 | 63.58 | 65.36 | 67.13 | 68.88 | 70.62 | 72.34 | 74.04 | 75.71 | 77.35 |
| 17 | 63.37 | 65.04 | 66.71 | 68.37 | 70.01 | 71.63 | 73.24 | 74.83 | 76.39 |
| 18 | 63.18 | 64.76 | 66.34 | 67.91 | 69.46 | 71.00 | 72.53 | 74.04 | 75.52 |
| 19 | 63.01 | 64.51 | 66.01 | 67.50 | 68.97 | 70.44 | 71.89 | 73.32 | 74.74 |
| 20 | 62.86 | 64.29 | 65.71 | 67.13 | 68.53 | 69.93 | 71.31 | 72.68 | 74.04 |
| 21 | 62.73 | 64.09 | 65.44 | 66.79 | 68.13 | 69.46 | 70.78 | 72.09 | 73.39 |
| 22 | 62.60 | 63.90 | 65.19 | 66.48 | 67.77 | 69.04 | 70.30 | 71.56 | 72.80 |
| 23 | 62.49 | 63.73 | 64.97 | 66.20 | 67.43 | 68.65 | 69.87 | 71.07 | 72.26 |
| 24 | 62.39 | 63.58 | 64.76 | 65.95 | 67.13 | 68.30 | 69.46 | 70.62 | 71.77 |
| 25 | 62.29 | 63.43 | 64.57 | 65.71 | 66.84 | 67.97 | 69.09 | 70.20 | 71.31 |
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 5.71 | 8.53 | 11.31 | 14.04 | 16.70 | 19.29 | 21.80 | 24.23 | 26.57 |
| 11 | 5.19 | 7.77 | 10.30 | 12.80 | 15.26 | 17.65 | 19.98 | 22.25 | 24.44 |
| 12 | 4.76 | 7.13 | 9.46 | 11.77 | 14.04 | 16.26 | 18.43 | 20.56 | 22.62 |
| 13 | 4.40 | 6.58 | 8.75 | 10.89 | 12.99 | 15.07 | 17.10 | 19.09 | 21.04 |
| 14 | 4.09 | 6.12 | 8.13 | 10.12 | 12.09 | 14.04 | 15.95 | 17.82 | 19.65 |
| 15 | 3.81 | 5.71 | 7.59 | 9.46 | 11.31 | 13.13 | 14.93 | 16.70 | 18.43 |
| 16 | 3.58 | 5.36 | 7.13 | 8.88 | 10.62 | 12.34 | 14.04 | 15.71 | 17.35 |
| 17 | 3.37 | 5.04 | 6.71 | 8.37 | 10.01 | 11.63 | 13.24 | 14.83 | 16.39 |
| 18 | 3.18 | 4.76 | 6.34 | 7.91 | 9.46 | 11.00 | 12.53 | 14.04 | 15.52 |
| 19 | 3.01 | 4.51 | 6.01 | 7.50 | 8.97 | 10.44 | 11.89 | 13.32 | 14.74 |
| 20 | 2.86 | 4.29 | 5.71 | 7.13 | 8.53 | 9.93 | 11.31 | 12.68 | 14.04 |
| 21 | 2.73 | 4.09 | 5.44 | 6.79 | 8.13 | 9.46 | 10.78 | 12.09 | 13.39 |
| 22 | 2.60 | 3.90 | 5.19 | 6.48 | 7.77 | 9.04 | 10.30 | 11.56 | 12.80 |
| 23 | 2.49 | 3.73 | 4.97 | 6.20 | 7.43 | 8.65 | 9.87 | 11.07 | 12.26 |
| 24 | 2.39 | 3.58 | 4.76 | 5.95 | 7.13 | 8.30 | 9.46 | 10.62 | 11.77 |
| 25 | 2.29 | 3.43 | 4.57 | 5.71 | 6.84 | 7.97 | 9.09 | 10.20 | 11.31 |
The lateral access trocars increase the instrument working angle, since they are located on either side of point O, thus forming a second entry point, called O'. This point is displaced by distance b from point O. Figure 6 shows the model overlain on the CAT scan.
The following equations are used to calculate the maximum instrument working angle:
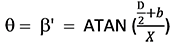
Table 4 shows the q (º) values for b = 6 cm, which is the estimated mean location of the lateral trocars normally employed for laparoscopic hiatal hernia surgery.
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 34.99 | 36.87 | 38.66 | 40.36 | 41.99 | 43.53 | 45.00 | 46.40 | 47.73 |
| 11 | 32.47 | 34.29 | 36.03 | 37.69 | 39.29 | 40.82 | 42.27 | 43.67 | 45.00 |
| 12 | 30.26 | 32.01 | 33.69 | 35.31 | 36.87 | 38.37 | 39.81 | 41.19 | 42.51 |
| 13 | 28.30 | 29.98 | 31.61 | 33.18 | 34.70 | 36.16 | 37.57 | 38.93 | 40.24 |
| 14 | 26.57 | 28.18 | 29.74 | 31.26 | 32.74 | 34.16 | 35.54 | 36.87 | 38.16 |
| 15 | 25.02 | 26.57 | 28.07 | 29.54 | 30.96 | 32.35 | 33.69 | 34.99 | 36.25 |
| 16 | 23.63 | 25.11 | 26.57 | 27.98 | 29.36 | 30.70 | 32.01 | 33.27 | 34.51 |
| 17 | 22.38 | 23.81 | 25.20 | 26.57 | 27.90 | 29.20 | 30.47 | 31.70 | 32.91 |
| 18 | 21.25 | 22.62 | 23.96 | 25.28 | 26.57 | 27.82 | 29.05 | 30.26 | 31.43 |
| 19 | 20.22 | 21.54 | 22.83 | 24.10 | 25.35 | 26.57 | 27.76 | 28.93 | 30.07 |
| 20 | 19.29 | 20.56 | 21.80 | 23.03 | 24.23 | 25.41 | 26.57 | 27.70 | 28.81 |
| 21 | 18.43 | 19.65 | 20.85 | 22.04 | 23.20 | 24.34 | 25.46 | 26.57 | 27.65 |
| 22 | 17.65 | 18.82 | 19.98 | 21.12 | 22.25 | 23.36 | 24.44 | 25.51 | 26.57 |
| 23 | 16.93 | 18.06 | 19.18 | 20.28 | 21.37 | 22.44 | 23.50 | 24.54 | 25.56 |
| 24 | 16.26 | 17.35 | 18.43 | 19.50 | 20.56 | 21.60 | 22.62 | 23.63 | 24.62 |
| 25 | 15.64 | 16.70 | 17.74 | 18.78 | 19.80 | 20.81 | 21.80 | 22.78 | 23.75 |
The field of vision can be expanded by inserting the camera through one of the trocars with lateral displacement (Figure 7). The resulting field of vision is then calculated by the following expression:
Tables 5 and 6 show the values obtained for the field of vision after applying the following values: lateral displacement, b = 6 cm; camera viewing angle = 60º; bevel angle d = 0º or 30º.
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 64.99 | 66.87 | 68.66 | 70.36 | 71.99 | 73.53 | 75.00 | 76.40 | 77.73 |
| 11 | 62.47 | 64.29 | 66.03 | 67.69 | 69.29 | 70.82 | 72.27 | 73.67 | 75.00 |
| 12 | 60.26 | 62.01 | 63.69 | 65.31 | 66.87 | 68.37 | 69.81 | 71.19 | 72.51 |
| 13 | 58.30 | 59.98 | 61.61 | 63.18 | 64.70 | 66.16 | 67.57 | 68.93 | 70.24 |
| 14 | 56.57 | 58.18 | 59.74 | 61.26 | 62.74 | 64.16 | 65.54 | 66.87 | 68.16 |
| 15 | 55.02 | 56.57 | 58.07 | 59.54 | 60.96 | 62.35 | 63.69 | 64.99 | 66.25 |
| 16 | 53.63 | 55.11 | 56.57 | 57.98 | 59.36 | 60.70 | 62.01 | 63.27 | 64.51 |
| 17 | 52.38 | 53.81 | 55.20 | 56.57 | 57.90 | 59.20 | 60.47 | 61.70 | 62.91 |
| 18 | 51.25 | 52.62 | 53.96 | 55.28 | 56.57 | 57.82 | 59.05 | 60.26 | 61.43 |
| 19 | 50.22 | 51.54 | 52.83 | 54.10 | 55.35 | 56.57 | 57.76 | 58.93 | 60.07 |
| 20 | 49.29 | 50.56 | 51.80 | 53.03 | 54.23 | 55.41 | 56.57 | 57.70 | 58.81 |
| 21 | 48.43 | 49.65 | 50.85 | 52.04 | 53.20 | 54.34 | 55.46 | 56.57 | 57.65 |
| 22 | 47.65 | 48.82 | 49.98 | 51.12 | 52.25 | 53.36 | 54.44 | 55.51 | 56.57 |
| 23 | 46.93 | 48.06 | 49.18 | 50.28 | 51.37 | 52.44 | 53.50 | 54.54 | 55.56 |
| 24 | 46.26 | 47.35 | 48.43 | 49.50 | 50.56 | 51.60 | 52.62 | 53.63 | 54.62 |
| 25 | 45.64 | 46.70 | 47.74 | 48.78 | 49.80 | 50.81 | 51.80 | 52.78 | 53.75 |
| D (cm) | |||||||||
| X (cm) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| 10 | 94.99 | 96.87 | 98.66 | 100.36 | 101.99 | 103.53 | 105.00 | 106.40 | 107.73 |
| 11 | 92.47 | 94.29 | 96.03 | 97.69 | 99.29 | 100.82 | 102.27 | 103.67 | 105.00 |
| 12 | 90.26 | 92.01 | 93.69 | 95.31 | 96.87 | 98.37 | 99.81 | 101.19 | 102.51 |
| 13 | 88.30 | 89.98 | 91.61 | 93.18 | 94.70 | 96.16 | 97.57 | 98.93 | 100.24 |
| 14 | 86.57 | 88.18 | 89.74 | 91.26 | 92.74 | 94.16 | 95.54 | 96.87 | 98.16 |
| 15 | 85.02 | 86.57 | 88.07 | 89.54 | 90.96 | 92.35 | 93.69 | 94.99 | 96.25 |
| 16 | 83.63 | 85.11 | 86.57 | 87.98 | 89.36 | 90.70 | 92.01 | 93.27 | 94.51 |
| 17 | 82.38 | 83.81 | 85.20 | 86.57 | 87.90 | 89.20 | 90.47 | 91.70 | 92.91 |
| 18 | 81.25 | 82.62 | 83.96 | 85.28 | 86.57 | 87.82 | 89.05 | 90.26 | 91.43 |
| 19 | 80.22 | 81.54 | 82.83 | 84.10 | 85.35 | 86.57 | 87.76 | 88.93 | 90.07 |
| 20 | 79.29 | 80.56 | 81.80 | 83.03 | 84.23 | 85.41 | 86.57 | 87.70 | 88.81 |
| 21 | 78.43 | 79.65 | 80.85 | 82.04 | 83.20 | 84.34 | 85.46 | 86.57 | 87.65 |
| 22 | 77.65 | 78.82 | 79.98 | 81.12 | 82.25 | 83.36 | 84.44 | 85.51 | 86.57 |
| 23 | 76.93 | 78.06 | 79.18 | 80.28 | 81.37 | 82.44 | 83.50 | 84.54 | 85.56 |
| 24 | 76.26 | 77.35 | 78.43 | 79.50 | 80.56 | 81.60 | 82.62 | 83.63 | 84.62 |
| 25 | 75.64 | 76.70 | 77.74 | 78.78 | 79.80 | 80.81 | 81.80 | 82.78 | 83.75 |
In 1919, Soresi performed the first operation to reduce a hiatal hernia and to achieve closure of the diaphragmatic pillars[10]. Since then, Skinner et al[2], Nissen[11], Collis[12], have advanced the state of the art with their conceptual and technical innovations. The first completely laparoscopic operation with Collis gastroplasty and Nissen fundoplication was described in 1998[13].
The essential steps of the procedure are the complete reduction of the hiatal hernia, excision of the hernial sac, extensive mediastinal mobilisation of the oesophagus, tension-free femoral closure and the construction of an anti-reflux mechanism. The first step is to reduce the hiatal hernia content by gentle traction of the hernial sac, gradually proceeding with extensive mediastinal mobilisation of the oesophagus (with blunt dissection) to obtain at least 2-2.5 cm of intra-abdominal oesophageal length[14]. During the dissection of the hernial sac, care must be taken to avoid lesions of the vagal nerves on the anterior and posterior surfaces of the oesophagus, the pleura and the adjacent vascular structures. Evidently, this manoeuvre could be very dangerous without visual control of certain areas of adhesions to the sac, or even with visual control if we cannot access the necessary areas with the laparoscopic instrument. These circumstances sometimes lead to blind dissections and traction that may damage vital structures[15].
The minimally invasive approach generally provides an excellent view of the hiatal region, far superior to that obtained by laparotomy, and is associated with low rates of morbidity and mortality, a short hospital stay and excellent patient compliance. From the technical point of view, during hernia reduction, the laparoscopic approach allows precise identification of the anatomical structure (vagus nerves, parietal pleura, distal oesophagus, etc.). Moreover, the dissection is facilitated by pneumoperitoneum[16-18].
Laparoscopic para-oesophageal hernia repair can be safely performed, by expert practitioners, with mortality rates of 1.3% in elective settings and 8% in emergencies[19,20]. However, major surgical complications can sometimes occur following iatrogenic lesions of the pleura, aorta or pericardium[21]. In addition, traction on the gastric fundus, the oesophagus-gastric junction and the lower oesophagus can provoke immediate or delayed visceral perforation, with life-threatening consequences[22].
These problems are usually due to a lack of direct vision of the working area. Moreover, in giant hernias the surgeon must overcome a ‘bottleneck’ effect; the hernial sac and content must be accessed through a relatively narrow hiatal hernial orifice, which limits the manoeuvrability of the instruments and the laparoscopic camera. With larger hernias, this situation can make it impossible to access certain areas of the intrathoracic hernial content.
Clearly, preoperative awareness of these circumstances is of great importance. If the field of vision or the instrument accessibility is limited, we could opt for a thoracic approach that would provide a good field of vision and an adequate working area in which to intervene safely.
The tables below show the angles of vision and the working angles obtained, according to the distance from the trocar to the hiatal orifice and according to its diameter. Tables 1, 2 and 3 show the results with the camera trocar in the usual, midline, position. Tables 4, 5 and 6 then show the angle of vision and the working angles obtained with the trocar located 6 cm to the left or right of the midline (the usual position for instrument trocars). From these data, we can calculate the access angles that will be obtained in a preoperative CAT coronal section, according to the location of the trocar. We also provide the formula for performing the angle calculations If the trocars are placed in less common situations, thus enabling us to determine the visibility and manoeuvrability for any position of the trocars.
From the study results obtained, it is apparent that the field of vision (with the 30º camera) spans almost all areas of expansion of a giant hiatal hernia. However, the working area is more limited and this factor, ultimately, determines the cases in which we can operate safely and those in which certain areas of the hernia cannot be accessed, which is when the thoracoscopic approach would be safer.
The optimal surgical approach for the repair of giant hiatal hernias has long been debated. Traditionally, this process required a laparotomy or thoracotomy, with their associated rates of morbidity. Conventional thinking used to be that the formation of adhesions, which often occur with laparotomy, might lessen the risk of hernia recurrence by helping retain the reduced structures within the abdomen.
However, the laparoscopic repair of hiatal hernias has provided a valuable surgical alternative since its introduction in 1992[23], in many cases offering better postoperative results and reducing costs[24,25]. For this reason, and especially since 2007, laparoscopic and thoracoscopic procedures have increasingly been employed to treat hiatal hernias.
To date, no randomised controlled trials have been performed to determine whether the thoracoscopic or laparoscopic approach is better, and so the choice remains highly dependent on the preferences and skills of the surgeon in question. Proponents of the laparoscopic approach refer to the easier manipulation of instruments and the ability to visualise the reduced viscera, thus avoiding inadvertent injury. On the other hand, supporters of the thoracoscopic method emphasise that it helps avoid adhesions (if there has been previous abdominal surgery) and that abdominal viscera are easily reduced with CO2 insufflated into the thorax[26].
Surgeons who advocate thoracoscopic repair point out that this method achieves a better visualisation of herniated structures, thus facilitating the dissection and resection of the sac. Accordingly, this approach would be indicated when preoperative simulation detects the presence of ‘dark’ areas that cannot be accessed visually or instrumentally via laparoscopy.
Nowadays, the vast majority of surgeons use the laparoscopic approach for hiatal hernias, and so laparoscopic fundoplication is performed almost universally[27].
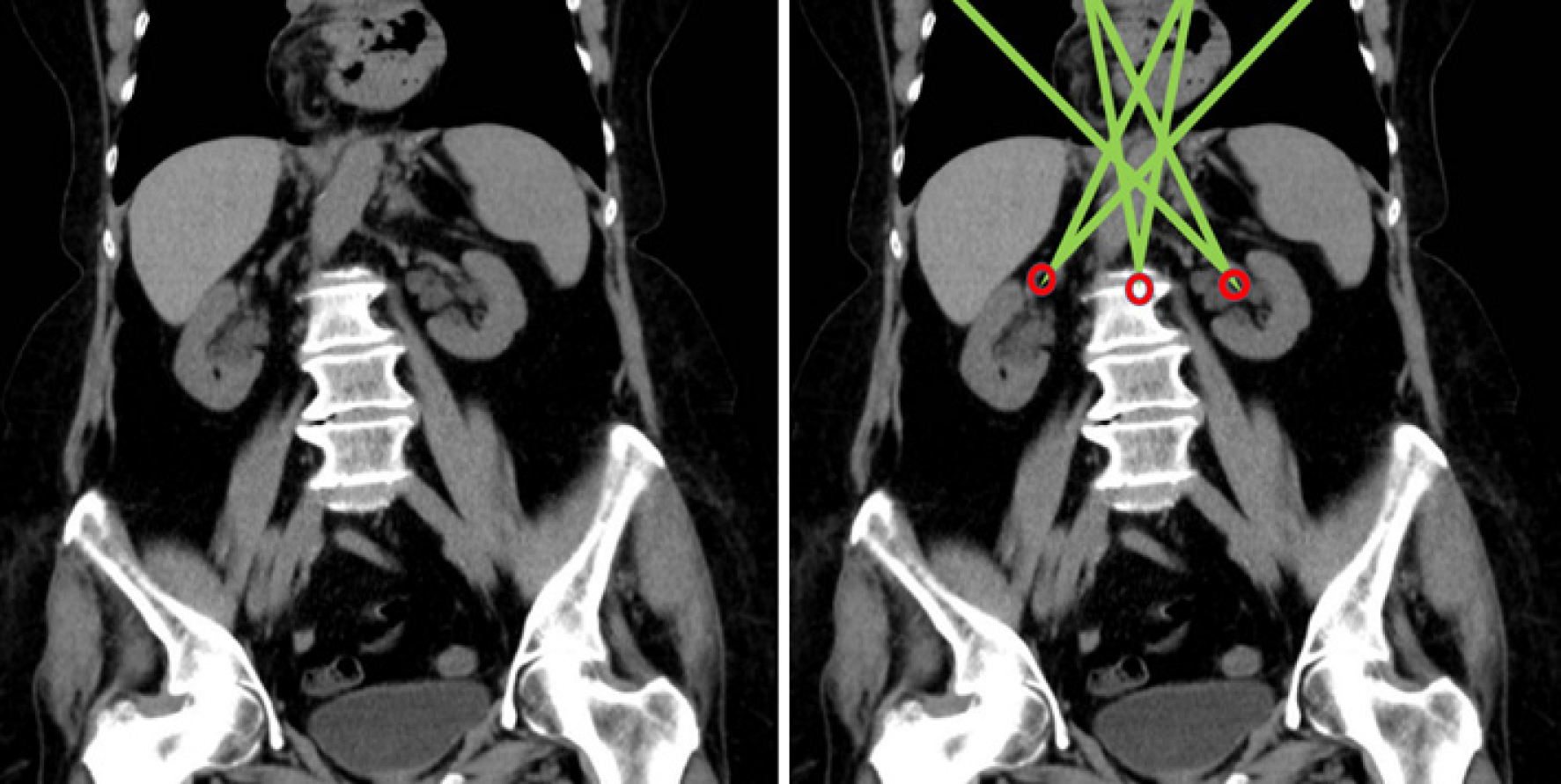
Recurrence rates after primary laparoscopic hiatal repair range from 1% to 7%, but can reach 50% with large hiatal hernias[28]. This increase is probably influenced by the fact that in these types of hernias there may be dark areas that cannot be accessed, which prevents the correct dissection of the sac (Figures 8 and 9). In fact, we performed a retrospective calculation of the angles of vision and the working angles in patients operated on with giant hernias, and found four cases in which the content of the hernia was not fully accessible. One of these cases could not be completed laparoscopically. Of the other three, two suffered a recurrence. For these patients, the outcomes would probably have been better if the thoracoscopic approach had been taken.
Despite its long history, the surgical management of giant hiatal hernias continues to evolve, and several questions remain to be clarified. For example, how should we define a giant hernia? Is mesh repair always appropriate? What are the indications determining the most suitable approach? Our study helps clarify the latter issue by providing objective data on visibility and manoeuvrability, thus informing the surgical team of the indications for the approach which is safest and produces the best results.
In short, we believe that full use should be made of the complementary imaging tests that are now available, so that before undertaking any laparoscopic intervention for a giant hiatal hernia we can calculate exactly what can be seen and how far we can go with the surgical instruments. This information, in turn, will enable the most suitable approach to be taken and thus optimise the results of the intervention.
This study was conducted to determine the accessibility obtained when the laparoscopic approach is applied to the repair of a giant hiatal hernia.
In patients with giant hernias, it is sometimes not possible to achieve full visibility of all areas of the sac using the laparoscopic approach.
The main study aim is to detect cases in which full access to all areas of the hernial sac is not possible, and so the thoracoscopic approach would be safer.
Our study helps clarify the latter issue by providing objective data on visibility and manoeuvrability, thus informing the surgical team of the indications for the approach which is safest and produces the best results.
Information of complementary imaging tests will enable us to adopt the most suitable approach and thus optimise the results of the intervention in patients with giant hiatal hernia.
From the study results obtained, the working area determines the cases in which we can operate safely and those in which certain areas of the hernia cannot be accessed, which is when the thoracoscopic approach would be safer.
By determining certain parameters – the camera angle aperture, the diameter of the hernial orifice and the positioning of the trocars with respect to this orifice – we can calculate the angle of vision and the instrument working angle available during the intervention.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shah OJ S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Davis SS Jr. Current controversies in paraesophageal hernia repair. Surg Clin North Am. 2008;88:959-978, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967;53:33-54. [PubMed] |
| 3. | Hill LD. Incarcerated paraesophageal hernia. A surgical emergency. Am J Surg. 1973;126:286-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 165] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Landreneau RJ, Hazelrigg SR, Johnson JA, Marshall JB, Gifford DL, Curtis JJ, Boley TM. The giant paraesophageal hernia: a particularly morbid condition of the esophageal hiatus. Mo Med. 1990;87:884-888. [PubMed] |
| 5. | Landreneau RJ, Johnson JA, Marshall JB, Hazelrigg SR, Boley TM, Curtis JJ. Clinical spectrum of paraesophageal herniation. Dig Dis Sci. 1992;37:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Mercer CD, Velasco N, Hill LD. Paraesophageal hernia. In: Hill L, Kozarek R, McCallum R, Mercer CD (eds). The esophagus: Medical and surgical management. Philadelphia: WB Saunders, 1998: 148–156. |
| 7. | Pearson FG, Cooper JD, Ilves R, Todd TR, Jamieson WR. Massive hiatal hernia with incarceration: a report of 53 cases. Ann Thorac Surg. 1983;35:45-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 104] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 330] [Cited by in RCA: 254] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 9. | Correa J, Morales CH, Toro JP. Laparoscopic repair of giant hiatal hernia: surgical technique, and clinical, endoscopic and radiological follow-up. Rev Colomb Cir. 2020;35:32-42. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Stylopoulos N, Rattner DW. The history of hiatal hernia surgery: from Bowditch to laparoscopy. Ann Surg. 2005;241:185-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 113] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | NISSEN R. [A simple operation for control of reflux esophagitis]. Schweiz Med Wochenschr. 1956;86:590-592. [PubMed] |
| 12. | COLLIS JL. An operation for hiatus hernia with short oesophagus. Thorax. 1957;12:181-188. [PubMed] |
| 13. | Johnson AB, Oddsdottir M, Hunter JG. Laparoscopic Collis gastroplasty and Nissen fundoplication. A new technique for the management of esophageal foreshortening. Surg Endosc. 1998;12:1055-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 88] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | O'Rourke RW, Khajanchee YS, Urbach DR, Lee NN, Lockhart B, Hansen PD, Swanstrom LL. Extended transmediastinal dissection: an alternative to gastroplasty for short esophagus. Arch Surg. 2003;138:735-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Oleynikov D, Jolley JM. Paraesophageal hernia. Surg Clin North Am. 2015;95:555-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Frantzides CT, Richards CG, Carlson MA. Laparoscopic repair of large hiatal hernia with polytetrafluoroethylene. Surg Endosc. 1999;13:906-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, Bremner CG. Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg. 2000;190:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 353] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 18. | Paul MG, DeRosa RP, Petrucci PE, Palmer ML, Danovitch SH. Laparoscopic tension-free repair of large paraesophageal hernias. Surg Endosc. 1997;11:303-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 57] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Ballian N, Luketich JD, Levy RM, Awais O, Winger D, Weksler B, Landreneau RJ, Nason KS. A clinical prediction rule for perioperative mortality and major morbidity after laparoscopic giant paraesophageal hernia repair. J Thorac Cardiovasc Surg. 2013;145:721-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Dallemagne B, Quero G, Lapergola A, Guerriero L, Fiorillo C, Perretta S. Treatment of giant paraesophageal hernia: pro laparoscopic approach. Hernia. 2018;22:909-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Çalıkoğlu İ, Özgen G, Toydemir T, Yerdel MA. Iatrogenic cardiac tamponade as a mortal complication of peri-hiatal surgery. Analysis of 30 published cases. Heliyon. 2019;5:e01537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Sihvo EI, Salo JA, Räsänen JV, Rantanen TK. Fatal complications of adult paraesophageal hernia: a population-based study. J Thorac Cardiovasc Surg. 2009;137:419-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 23. | Cuschieri A, Shimi S, Nathanson LK. Laparoscopic reduction, crural repair, and fundoplication of large hiatal hernia. Am J Surg. 1992;163:425-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 116] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Felix VN, Yogi I, Senday D, Coimbra FT, Martinez Faria KV, Belo Silva MF, Previero Elias da Silva G. Post-operative giant hiatal hernia: A single center experience. Medicine (Baltimore). 2019;98:e15834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Karmali S, McFadden S, Mitchell P, Graham A, Debru E, Gelfand G, Graham J, Martin S, Tiruta C, Grondin S. Primary laparoscopic and open repair of paraesophageal hernias: a comparison of short-term outcomes. Dis Esophagus. 2008;21:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Yang X, Hua R, He K, Shen Q, Yao Q. Laparoscopic hernioplasty of hiatal hernia. Ann Transl Med. 2016;4:343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Yun JS, Na KJ, Song SY, Kim S, Kim E, Jeong IS, Oh SG. Laparoscopic repair of hiatal hernia. J Thorac Dis. 2019;11:3903-3908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |