Published online Nov 27, 2021. doi: 10.4240/wjgs.v13.i11.1405
Peer-review started: April 6, 2021
First decision: May 13, 2021
Revised: July 3, 2021
Accepted: July 21, 2021
Article in press: July 21, 2021
Published online: November 27, 2021
Processing time: 234 Days and 7.5 Hours
As one of the major abdominal operations, pancreaticoduodenectomy (PD) involves many organs. The operation is complex, and the scope of the operation is large, which can cause significant trauma in patients. The operation has a high rate of complications. Pancreatic leakage is the main complication after PD. When pancreatic leakage occurs after PD, it can often lead to abdominal bleeding and infection, threatening the lives of patients. One study found that pancreatic leakage was affected by many factors including the choice of pancreaticojejunostomy method which can be well controlled.
To investigate the choice of operative methods for pancreaticojejunostomy and to conduct a multivariate study of pancreatic leakage in PD.
A total of 420 patients undergoing PD in our hospital from January 2014 to March 2019 were enrolled and divided into group A (n = 198) and group B (n = 222) according to the pancreatointestinal anastomosis method adopted during the operation. Duct-to-mucosa pancreatojejunostomy was performed in group A and bundled pancreaticojejunostomy was performed in group B. The operation time, intraoperative blood loss, and pancreatic leakage of the two groups were assessed. The occurrence of pancreatic leakage after the operation in different patients was analyzed.
The differences in operative time and intraoperative bleeding between groups A and B were not significant (P > 0.05). In group A, the time of pancreatojejunostomy was 26.03 ± 4.40 min and pancreatic duct diameter was 3.90 ± 1.10 mm. These measurements were significantly higher than those in group B (P < 0.05). The differences in the occurrence of pancreatic leakage, abdominal infection, abdominal hemorrhage and gastric retention between group A and group B were not significant (P > 0.05). The rates of pancreatic leakage in patients with preoperative albumin < 30 g/L, preoperative jaundice time ≥ 8 wk, and pancreatic duct diameter < 3 mm, were 23.33%, 33.96%, and 19.01%, respectively. These were significantly higher than those in patients with preoperative albumin ≥ 30 g/L, preoperative jaundice time < 8 wk, and pancreatic duct diameter ≥ 3 cm (P < 0.05). Logistic regression analysis showed that preoperative albumin < 30 g/L, preoperative jaundice time ≥ 8 wk, and pancreatic duct diameter < 3 mm were risk factors for pancreatic leakage after PD (odds ratio = 2.038, 2.416 and 2.670, P < 0.05).
The pancreatointestinal anastomosis method during PD has no significant effect on the occurrence of pancreatic leakage. The main risk factors for pancreatic leakage include preoperative albumin, preoperative jaundice time, and pancreatic duct diameter.
Core Tip: From retrospective studies, it was confirmed that the type of pancreaticojejunostomy during pancreaticoduodenectomy had no significant effect on the occurrence of postoperative pancreatic leakage. The main risk factors for pancreatic leakage include preoperative albumin, preoperative jaundice time and pancreatic duct diameter.
- Citation: Liang H, Wu JG, Wang F, Chen BX, Zou ST, Wang C, Luo SW. Choice of operative method for pancreaticojejunostomy and a multivariable study of pancreatic leakage in pancreaticoduodenectomy. World J Gastrointest Surg 2021; 13(11): 1405-1413
- URL: https://www.wjgnet.com/1948-9366/full/v13/i11/1405.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v13.i11.1405
As one of the major abdominal operations, pancreaticoduodenectomy (PD) involves many organs. The operation is complex, and the scope of the operation is large, which can cause significant trauma in patients. The operation has a high rate of complications. Pancreatic leakage is the main complication after PD[1-5]. When pancreatic leakage occurs after PD, it can often lead to abdominal bleeding and infection, threatening the lives of patients. One study found that pancreatic leakage was affected by many factors including the choice of pancreaticojejunostomy method, which can be well controlled. Due to the differences in the specific surgical mechanism of the two commonly used anastomosis methods after PD, duct-to-mucosa pancreatojejunostomy and bundled pancreaticojejunostomy, and the individual differences among patients, not all patients can undergo pancreaticojejunostomy. However, each method has advantages and disadvantages. There are still some differences regarding the type of pancreaticojejunostomy that is more favorable for patients[6]. Therefore, in this study, the curative effect of duct-to-mucosa pancreaticojejunostomy and binding pancreaticojejunostomy in PD was reviewed. Multiple factors of postoperative pancreatic leakage were analyzed.
A total of 420 patients undergoing PD in our hospital between January 2014 and March 2019 were selected. The inclusion criteria were as follows: (1) American Association of Anesthesiologists classification I–II; (2) Age > 18 years; and (3) Complete preservation of clinical variables. The exclusion criteria were abnormal coagulation function, blood system diseases, immune system diseases, and other basic diseases. These patients were divided into group A (n = 198) and group B (n = 222) according to the pancreatointestinal anastomosis method adopted during the operation. There was no significant difference in the general parameters between groups A and B (P > 0.05, Table 1).
| Group | Cases | Male/female | Age (yr) | Albumin(g/L) | Hemoglobin (g/L) | Disease types | |||
| Carcinoma of the head of the pancreas | Carcinoma of the ampulla | Carcinoma of the lower common bile duct | Duodenal carcinoma | ||||||
| A group | 198 | 110/88 | 60.33 ± 9.82 | 36.70 ± 4.40 | 110.02 ± 10.43 | 93 (46.97) | 52 (26.26) | 31 (15.66) | 22 (11.11) |
| B group | 222 | 132/90 | 59.81 ± 10.11 | 36.12 ± 5.53 | 109.82 ± 12.21 | 108 (48.65) | 72 (32.43) | 29 (13.06) | 13 (5.86) |
| t/χ2 | 0.653 | 0.533 | 1.180 | 0.179 | 5.372 | ||||
| P value | 0.419 | 0.594 | 0.239 | 0.858 | 0.146 | ||||
In PD, reconstruction of the digestive tract was in the order of pancreaticojejunostomy, choledochojejunostomy, and gastrojejunostomy to conduct Roux-Y anastomosis. Duct-to-mucosa pancreatojejunostomy was performed in group A. First, we sutured the jejunal seromuscular layer intermittently with the pancreatic tissue at the posterior edge of the pancreatic section. We cut a small hole in the jejunal wall corresponding to the pancreatic duct, then the posterior wall of the jejunum was sutured intermittently with the entire jejunum using three needles, and a silicone tube was inserted into the jejunum and beyond the bilioenterostomy. Next, the anterior wall of the pancreatic duct and the whole jejunum were sutured intermittently using three needles so that the pancreatic duct was placed into the jejunal mucosa as far as possible. We then sutured the anterior tissue of the pancreatic section and the jejunal seromuscular layer intermittently. If necessary, the jejunal seromuscular layer and pancreatic capsule were intermittently embedded and sutured.
Bundled pancreaticojejunostomy was performed in group B. A multifunctional surgical dissector was used to cut the pancreas at the neck, and scrape suction was used to bluntly separate the pancreas. The jejunum was cut near the terminal jejunal artery. The jejunum was turned over to 3 o’clock, so that the mucosal surface of the jejunum was outward. After that, we closed the pancreas and intestinal stump and sutured the two sides with silk thread as a single layer. The posterior lip was sutured first, and then the anterior lip was sutured. The two loose temporary ligation knots were cut off and the mucosal surface was destroyed. The jejunum was returned to its original position. A number 0 absorbable suture was passed through the mesenteric puncture hole between the two groups of blood vessels near the broken end of the jejunum to ligate the jejunum so that the jejunum and pancreas were closely attached. The tightness of ligation was such that the ligation coil could just extend into the small vascular clamp end.
The operative time, anastomotic time, intraoperative bleeding loss, and pancreatic duct diameter were compared between the two groups. The rates of pancreatic leakage, abdominal infection, abdominal hemorrhage, and gastric retention were recorded. The preoperative albumin, preoperative jaundice time, pancreatic duct diameter, and other important clinical variables were analyzed and compared.
SPSS 22.0 software was used for parameter statistics. The measurement data are expressed as mean ± SD. The differences between these two groups were compared by independent sample t-tests. Categorical variables are expressed as frequency or percentage, and the comparison between the two groups was performed using the χ2 test. Multivariate analysis adopted the logistic regression analysis, where α = 0.05 was the test level.
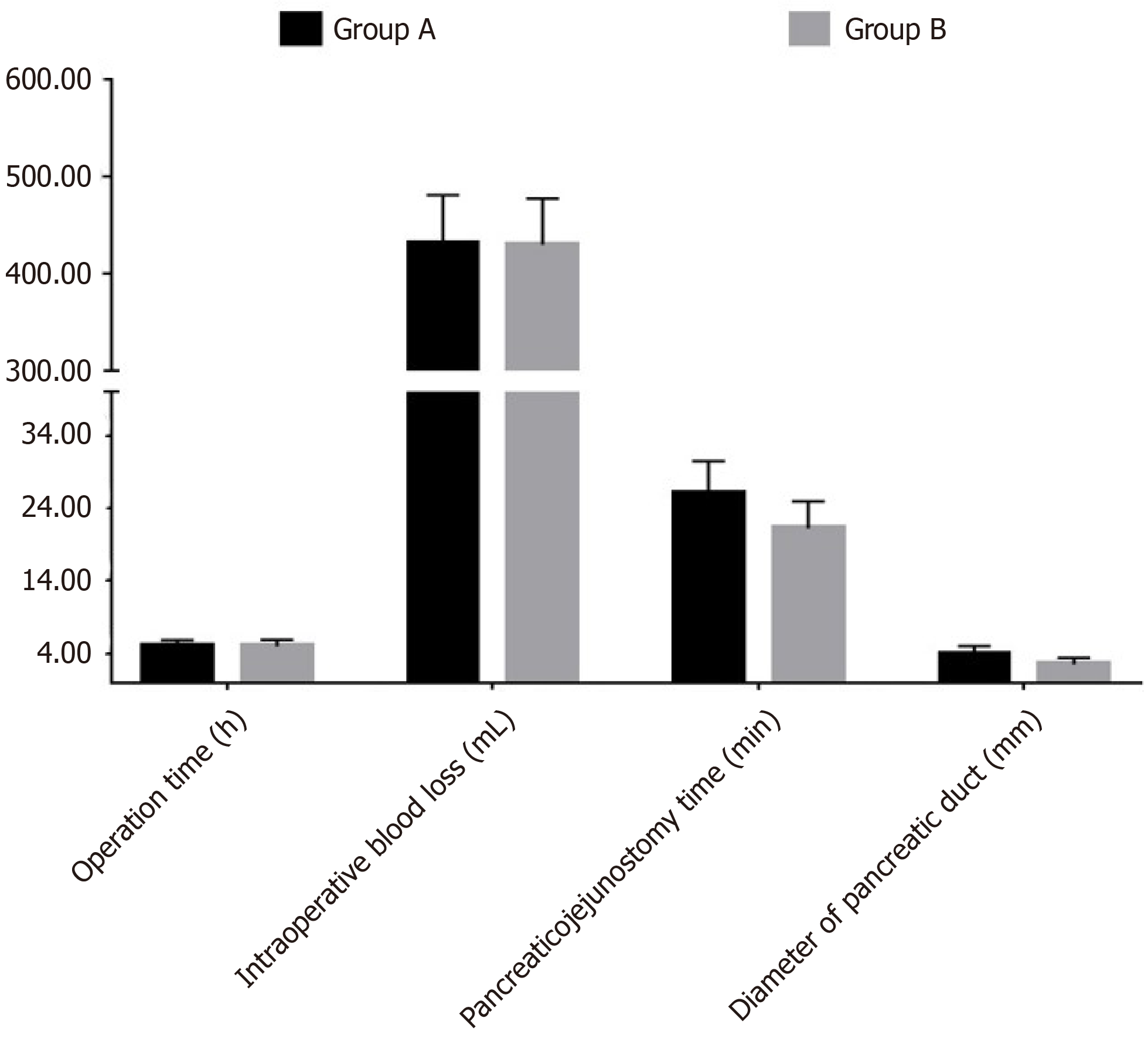
The differences in operative time and intraoperative bleeding between groups A and B were not significant (P > 0.05). The time of pancreatojejunostomy and pancreatic duct diameter in group A were significantly higher than those in group B (P < 0.05, Table 2 and Figure 1).
| Group | Cases | Operation time (h) | Intraoperative blood loss (mL) | Pancreaticojejunostomy time (min) | Diameter of pancreatic duct (mm) |
| A group | 198 | 5.02 ± 0.82 | 430.40 ± 50.03 | 26.03 ± 4.40 | 3.90 ± 1.10 |
| B group | 222 | 4.97 ± 0.90 | 429.28 ± 47.74 | 21.19 ± 3.77 | 2.50 ± 0.88 |
| t | 0.593 | 0.235 | 12.139 | 14.470 | |
| P value | 0.554 | 0.815 | 0.000 | 0.000 |
The differences in the occurrence of pancreatic leakage, abdominal infection, abdominal hemorrhage, and gastric retention between groups A and B were not significant (P > 0.05, Table 3).
| Group | Cases | Pancreatic leakage | Abdominal infection | Abdominal hemorrhage | Gastric retention |
| A group | 198 | 14 (7.07) | 8 (4.04) | 7 (3.54) | 7 (3.54) |
| B group | 222 | 21 (9.46) | 10 (4.50) | 9 (4.05) | 8 (3.60) |
| χ2 | 0.782 | 0.055 | 0.077 | 0.001 | |
| P value | 0.377 | 0.815 | 0.782 | 0.970 |
The rates of pancreatic leakage in patients with preoperative albumin < 30 g/L, preoperative jaundice time ≥ 8 wk, and pancreatic duct diameter < 3 mm were significantly higher than those in patients with preoperative albumin ≥ 30 g/L, preoperative jaundice time < 8 wk, and pancreatic duct diameter ≥ 3 cm (P < 0.05, Table 4).
| Index | Cases | Postoperative pancreatic leakage | χ2 | P value |
| Age (yr) | 0.072 | 0.789 | ||
| ≤ 60 | 243 | 21 (8.64) | ||
| > 60 | 177 | 14 (7.91) | ||
| Sex | 0.004 | 0.953 | ||
| Male | 242 | 20 (8.26) | ||
| Female | 178 | 15 (8.43) | ||
| Diabetes | 0.153 | 0.696 | ||
| Yes | 120 | 11 (9.17) | ||
| No | 300 | 24 (8.00) | ||
| Hypertension | 0.089 | 0.766 | ||
| Yes | 178 | 14 (7.87) | ||
| No | 242 | 21 (8.68) | ||
| Preoperative albumin | 33.739 | 0.000 | ||
| < 30 g/L | 90 | 21 (23.33) | ||
| ≥ 30 g/L | 330 | 14 (4.24) | ||
| Preoperative jaundice time | 52.154 | 0.000 | ||
| < 8 wk | 367 | 17 (4.63) | ||
| ≥ 8 wk | 53 | 18 (33.96) | ||
| Operation time | 0.022 | 0.883 | ||
| < 4 h | 209 | 17 (8.13) | ||
| ≥ 4 h | 211 | 18 (8.53) | ||
| Intraoperative blood loss | 0.087 | 0.768 | ||
| < 430 mL | 230 | 20 (8.70) | ||
| ≥ 430 mL | 190 | 15 (7.89) | ||
| Vascular resection and reconstruction | 0.000 | 1.000 | ||
| Yes | 60 | 5 (8.33) | ||
| No | 360 | 30 (8.33) | ||
| Pancreatic texture | 0.022 | 0.883 | ||
| Soft | 221 | 18 (8.14) | ||
| Hard | 199 | 17 (8.54) | ||
| Diameter of pancreatic duct | 25.355 | 0.000 | ||
| < 3 mm | 121 | 23 (19.01) | ||
| ≥ 3 mm | 299 | 12 (4.01) | ||
| Pancreaticojejunostomy time | 0.305 | 0.580 | ||
| < 30 min | 320 | 28 (8.75) | ||
| ≥ 30 min | 100 | 7 (7.00) | ||
| Pancreatic duct indwelling support tube | 0.162 | 0.687 | ||
| Yes | 335 | 27 (8.06) | ||
| No | 85 | 8 (9.41) | ||
| Disease types | 0.018 | 0.999 | ||
| Carcinoma of the head of the pancreas | 201 | 17 (8.46) | ||
| Carcinoma of the ampulla | 124 | 10 (8.06) | ||
| Carcinoma of the lower common bile duct | 60 | 5 (8.33) | ||
| Duodenal carcinoma | 35 | 3 (8.57) |
Logistic regression analysis showed that preoperative albumin < 30 g/L, preoperative jaundice time ≥ 8 wk, and pancreatic duct diameter < 3 mm were risk factors for pancreatic leakage after PD (odds ratio = 2.038, 2.416, and 2.670, P < 0.05, Table 5).
| Factor | β | SE | Walds | P value | Odds ratio (95%CI) |
| Preoperative albumin < 30 g/L | 0.712 | 0.202 | 12.424 | 0.000 | 2.038 (1.372-3.028) |
| Preoperative jaundice time ≥ 8 wk | 0.882 | 0.329 | 7.187 | 0.000 | 2.416 (1.268-4.604) |
| Diameter of pancreatic duct < 3 mm | 0.982 | 0.311 | 9.970 | 0.000 | 2.670 (1.451-4.911) |
The anatomical structures adjacent to the pancreas are relatively important; therefore, PD is a highly complex operation that involves many organs. The procedure can cause significant damage to the body, and the morbidity and mortality associated with postoperative complications are high[7]. Pancreatic leakage is the most dangerous complication of PD[8]. Preventing pancreatic leakage is key to the success of the operation, specifically with regard to selection of the procedure used for pancreaticojejunal anastomosis[9]. A previous study[10] found that different anastomosis methods have different effects in different patients. Therefore, clinical recommendations should be made according to the patient's condition, the surgical characteristics, and the selection of the appropriate pancreaticointestinal anastomosis method to improve the surgical effect.
Duct-to-mucosa pancreaticojejunostomy and bundled pancreaticojejunostomy are the most common procedures performed in PD. The results showed that there was no significant difference in operation time and intraoperative blood loss between groups A and B, but the pancreaticojejunostomy duration and pancreatic duct diameter in group A were significantly larger than those in group B. These results indicate that pancreaticojejunal mucosal anastomosis is slow and is mostly used for patients with larger pancreatic duct diameters. Pancreaticojejunostomy can ensure the continuity and patency of the jejunal mucosa and pancreatic duct, thus better maintaining the exocrine function of the pancreas and the patency of the anastomosis. Burying the pancreatic stump under the jejunal serosa can effectively protect the anastomosis and reduce bleeding caused by pancreatic juice eroding the pancreatic stump. However, the operation is relatively difficult, the technical requirements of the anastomosis are high, and they are mostly suitable for patients with large-diameter pancreatic ducts[11,12]. Bundled pancreaticojejunostomy can be used to avoid pinhole indwelling by ensuring the sealing of anastomosis via binding instead of suturing, thus reducing the incidence of pancreatic leakage. However, previous studies[13,14] have indicated that this method is not suitable for patients in whom the pancreatic stump is too thick, which must be addressed with certain surgical requirements.
Through further study, no significant differences in the occurrence of pancreatic leakage, abdominal infection, intraperitoneal hemorrhage, and gastric retention between groups A and B were found. These results indicate that the rates of pancreatic leakage and other complications after duct-to-mucosa pancreaticojejunostomy and bundled pancreaticojejunostomy were similar. At present, there is no consensus on which specific operation is best for digestive tract reconstruction in PD. Therefore, surgeons need to understand the specific indications for different anastomosis methods. With the development of clinical technology, more ideal pancreatic stump management methods are expected to be explored through large sample and prospective studies to reduce the rate of postoperative pancreatic leakage and improve the safety of the operation.
Analysis of the relationship between postoperative pancreatic leakage and clinical indicators showed that the rate of postoperative pancreatic leakage in patients with preoperative albumin < 30 g/L, preoperative jaundice duration ≥ 8 wk, and pancreatic duct diameter < 3 cm were significantly higher than those before the operation. Logistic regression showed that preoperative albumin < 30 g/L, preoperative jaundice duration ≥ 8 wk, and pancreatic duct diameter < 3 cm were risk factors for pancreatic leakage in patients with PD. These results indicate that preoperative albumin level, preoperative jaundice duration, and pancreatic duct diameter are the main risk factors for pancreatic leakage after PD. Therefore, patients with abnormal preoperative bilirubin and albumin levels and a long duration of jaundice need to be given special attention before the operation and should receive good perioperative supportive treatment to reduce the rate of postoperative pancreatic leakage. Pancreatic leakage is not only related to surgical and pancreatic factors but is also closely related to the basic state of the patient during the perioperative period. As the duration of jaundice increases, the decreased liver function in patients is gradually aggravated. Related studies[15-17] indicated that vitamin K1 could be used to improve coagulation function and jaundice symptoms, but the absorption of toxins in the body could lead to damage to multiple organs and the liver, inducing pancreatic leakage. Perioperative hypoproteinemia is another main cause of abdominal infection, wound infection, and pancreatic leakage. Patients with relatively poor nutritional status require timely supplementation with albumin and nutrients. A good visual field and pancreatic duct exposure are important factors for ensuring a successful pancreaticoenteric anastomosis; therefore, a large diameter is needed to suture the pancreaticoenteric anastomosis, which should then be left in place. The pinhole is an important cause of pancreatic leakage and requires special attention[18-20].
In summary, intraoperative pancreaticojejunostomy in PD had no significant effect on postoperative pancreatic leakage. The main risk factors for pancreatic leakage included preoperative albumin, preoperative jaundice time and pancreatic duct diameter.
Pancreaticoduodenectomy (PD) involves many organs, and the operation is complex and the scope of operation is large. The operation can cause significant trauma in patients and has a high rate of complications. Pancreatic leakage is the main complication after PD.
This study discussed the selection of surgical methods for pancreaticojejunostomy and pancreatic leakage during PD.
This study aimed to investigate the choice of operative methods for pancreaticojejunostomy and conduct a multivariate analysis of pancreatic leakage in PD.
A total of 420 patients undergoing PD were selected and divided into group A and group B according to the pancreatointestinal anastomosis method adopted during the operation. Duct-to-mucosa pancreatojejunostomy was performed in group A and bundled pancreaticojejunostomy was performed in group B. The operation time, intraoperative blood loss, and pancreatic leakage in the two groups were observed, and the occurrence of pancreatic leakage after the operation in different patients was analyzed.
The differences in operative time and intraoperative bleeding between groups A and B were not significant. In group A, the duration of pancreatojejunostomy was 26.03 ± 4.40 min and the pancreatic duct diameter was 3.90 ± 1.10 mm. These measurements were significantly higher than those in group B. The differences in the occurrence of pancreatic leakage, abdominal infection, abdominal hemorrhage, and gastric retention between group A and group B were not significant. The rates of pancreatic leakage in patients with preoperative albumin < 30 g/L, preoperative jaundice time ≥ 8 wk, and pancreatic duct diameter < 3 mm were 23.33%, 33.96%, and 19.01%, respectively.
The pancreatointestinal anastomosis method during PD has no significant effect on the occurrence of pancreatic leakage. The main risk factors for pancreatic leakage include preoperative albumin, preoperative jaundice time, and pancreatic duct diameter.
A more advantageous surgical method for pancreaticojejunostomy should be selected.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fukuta M, Honda M S-Editor: Wang JL L-Editor: Webster JR P-Editor: Li JH
| 1. | de Medeiros FS, Junior ESDM, França RL, Neto HCM, Santos JM, Júnior EAA, Júnior SODS, Tavares MHSMP, de Moura EGH. Preemptive endoluminal vacuum therapy after pancreaticoduodenectomy: A case report. World J Gastrointest Endosc. 2020;12:493-499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Qureshi S, Ghazanfar S, Quraishy MS, Rana R. Stented Pancreatico-duodenectomy: Does it lead to decreased pancreatic fistula rates? J Pak Med Assoc. 2018;68:348-352. [PubMed] |
| 3. | La Greca G, Primo S, Sofia M, Lombardo R, Puleo S, Russello D, Di Cataldo A. Combination of fibrin glue protection with microsurgical technique for duct-to-mucosa pancreatico-jejunostomy reduces the incidence of leakages after pancreaticoduodenectomy. Ann Ital Chir. 2014;85:490-494. [PubMed] |
| 4. | Cirocchi R, Partelli S, Castellani E, Renzi C, Parisi A, Noya G, Falconi M. Right hemicolectomy plus pancreaticoduodenectomy vs partial duodenectomy in treatment of locally advanced right colon cancer invading pancreas and/or only duodenum. Surg Oncol. 2014;23:92-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Choe YM, Lee KY, Oh CA, Lee JB, Choi SK, Hur YS, Kim SJ, Cho YU, Ahn SI, Hong KC, Shin SH, Kim KR. Risk factors affecting pancreatic fistulas after pancreaticoduodenectomy. World J Gastroenterol. 2008;14:6970-6974. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Song Y, Tieniber AD, Vollmer CM, Lee MK, Roses RE, Fraker DL, Kelz RR, Karakousis GC. Predictors and outcomes of jejunostomy tube placement at the time of pancreatoduodenectomy. Surgery. 2019;165:1136-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Zhang W, Huang Z, Zhang J, Che X. Safety and effectiveness of open pancreaticoduodenectomy in adults aged 70 or older: A meta-analysis. J Geriatr Oncol. 2021;12:1136-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Tuech JJ, Pessaux P, Duplessis R, Villapadierna F, Ronceray J, Arnaud JP. [Pancreatojejunal or pancreatogastric anastomosis after cephalic duodenopancreatectomy. A comparative retrospective study]. Chirurgie. 1998;123:450-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Zhang W, Huang Z, Zhang J, Che X. Safety and efficacy of robot-assisted versus open pancreaticoduodenectomy: a meta-analysis of multiple worldwide centers. Updates Surg. 2021;73:893-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Smits FJ, van Santvoort HC, Besselink MG, Boerma D, Busch OR, van Dam RM, van Eijck CH, Festen S, van der Harst E, de Hingh IH, de Jong KP, Borel Rinkes IH, Molenaar IQ; Dutch Pancreatic Cancer Group. Predicting Successful Catheter Drainage in Patients With Pancreatic Fistula After Pancreatoduodenectomy. Pancreas. 2019;48:811-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Yang H, Ren Y, Yu Z, Zhou H, Zhang S, Luo C, Jiao Z. Pancreatic fistula after pancreatoduodenectomy due to compression of the superior mesenteric vessels: a case report. BMC Surg. 2020;20:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Jester AL, Chung CW, Becerra DC, Molly Kilbane E, House MG, Zyromski NJ, Max Schmidt C, Nakeeb A, Ceppa EP. The Impact of Hepaticojejunostomy Leaks After Pancreatoduodenectomy: a Devastating Source of Morbidity and Mortality. J Gastrointest Surg. 2017;21:1017-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Ishiwatari H, Sato J, Kaneko J. Hepaticojejunostomy for the right hepatic bile duct using a forward-viewing echoendoscope in a patient after pancreatoduodenectomy. Dig Endosc. 2019;31:e82-e83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Khan AS, Williams G, Woolsey C, Liu J, Fields RC, Doyle MMB, Hawkins WG, Strasberg SM. Flange Gastroenterostomy Results in Reduction in Delayed Gastric Emptying after Standard Pancreaticoduodenectomy: A Prospective Cohort Study. J Am Coll Surg. 2017;225:498-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Yang JR, Xiao R, Zhou J, Wang L, Wang JX, Zhang Q, Niu JX, Wang ZF, Yang RF, Ren JJ. Establishment of a Canine Training Model for Digestive Tract Reconstruction after Pancreaticoduodenectomy. J Invest Surg. 2021;34:561-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Kang JS, Han Y, Kim H, Kwon W, Kim SW, Jang JY. Prevention of pancreatic fistula using polyethylene glycolic acid mesh reinforcement around pancreatojejunostomy: the propensity score-matched analysis. J Hepatobiliary Pancreat Sci. 2017;24:169-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Li Y, Liu XM, Zhang HK, Zhang XF, Tang B, Ma F, Lv Y. Magnetic Compression Anastomosis in Laparoscopic Pancreatoduodenectomy: A Preliminary Study. J Surg Res. 2021;258:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Morelli L, Di Franco G, Guadagni S, Palmeri M, Furbetta N, Gianardi D, Del Chiaro M, Di Candio G, Mosca F. Technical Details and Results of a Modified End-to-Side Technique of Pancreatojejunostomy: a Personal Series of 100 Patients. J Gastrointest Surg. 2017;21:2090-2099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Hayama S, Senmaru N, Hirano S. Delayed gastric emptying after pancreatoduodenectomy: comparison between invaginated pancreatogastrostomy and pancreatojejunostomy. BMC Surg. 2020;20:60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Pedrazzoli S. Pancreatoduodenectomy (PD) and postoperative pancreatic fistula (POPF): A systematic review and analysis of the POPF-related mortality rate in 60,739 patients retrieved from the English literature published between 1990 and 2015. Medicine (Baltimore). 2017;96:e6858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 155] [Article Influence: 19.4] [Reference Citation Analysis (0)] |