Published online Aug 27, 2020. doi: 10.4240/wjgs.v12.i8.346
Peer-review started: May 2, 2020
First decision: May 24, 2020
Revised: May 31, 2020
Accepted: July 26, 2020
Article in press: July 26, 2020
Published online: August 27, 2020
Processing time: 111 Days and 8.9 Hours
Laparoscopic distal gastrectomy (LDG) for gastric cancer has been progressed and popular in Japan, since it was first described in 1994. Several reconstruction methods can be adopted according to remnant stomach size, and balance of pros and cons. Roux-en-Y (R-Y) reconstruction is a one of standard options after LDG. Its complications include Petersen’s hernia and Roux stasis syndrome. Here we report our ingenious attempt, fixation of Roux limb and duodenal stump, for decreasing the development of Petersen’s hernia and Roux stasis syndrome.
To develop a method to decrease the development of Petersen’s hernia and Roux stasis syndrome.
We performed ante-colic R-Y reconstruction after LDG. After R-Y reconstruction, we fixed Roux limb onto the duodenal stump in a smooth radian. Via this small improvement in Roux limb, Roux limb was placed to the right of the ligament of Treitz. This not only changed the anatomy of the Petersen’s defect, but it also kept a fluent direction of gastrointestinal anastomosis and avoided a cross-angle after jejunojejunostomy. 31 patients with gastric cancer was performed this technique after R-Y reconstruction. Clinical parameters including clinicopathologic characteristics, perioperative outcomes, postoperative complication and follow-up data were evaluated.
The operative time was (308.0 ± 84.6 min). This improvement method took about 10 min. Two (6.5%) patients experienced pneumonia and pancreatitis, respectively. No patient required reoperation or readmission. All patients were followed up for at least 3 year, and none of the patients developed postoperative complications related to internal hernia or Roux stasis syndrome.
This 10 min technique is a very effective method to decrease the development of Petersen’s hernia and Roux stasis syndrome in patients who undergo LDG.
Core tip: We developed a method, fixation of Roux limb and duodenal stump. This not only changed the anatomy of the Petersen’s defect, but it also kept a fluent direction of gastrointestinal anastomosis and avoided a cross-angle after jejunojejunostomy. None of the patients had complications related to Petersen’s hernia and Roux stasis syndrome by at least three years of follow-up in this study. This technique is a simple and effective method to decrease the development of Petersen’s hernia and Roux stasis syndrome.
- Citation: Wu JZ, Orita H, Zhang S, Egawa H, Yube Y, Kaji S, Oka S, Fukunaga T. Easy fixation effects the prevention of Peterson’s hernia and Roux stasis syndrome. World J Gastrointest Surg 2020; 12(8): 346-354
- URL: https://www.wjgnet.com/1948-9366/full/v12/i8/346.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i8.346
Since the first laparoscopic distal gastrectomy (LDG) for gastric cancer was reported in Japan, it has been progressed and popular due to the benefits for patients[1]. According to survey from Nationwide Survey of Endoscopic Surgery in Japan, distal gastrectomy was accounted for the most proportion among all the laparoscopic gastrectomy[1,2].
Evidence-based oncological outcomes of LDG for gastric cancer were obtained from many random clinical trials[1,3,4]. After that, more and more attention was attracted to improve patients’ quality of life. Digestive tract reconstruction is a critical aspect of the procedure in addition to not only the oncologic goals of disease resection but also the quality of life for patients. Reconstruction methods by laparoscopy have been developed during more than 10 year. An optimal technique of digestive tract reconstruction after distal gastrectomy has not been reached definitive consensus. There are several reconstruction methods of digestive tract after laparoscopic distal gastrectomy including Billroth I, Billroth II, and Roux-en-Y anastomosis. Roux-en-Y gastrojejunostomy is now used worldwide for the prevention of alkaline reflux gastritis, esophagitis, dumping syndrome, and carcinogenesis of the gastric remnant.
A gastrojejunostomy in R-Y reconstruction can be performed through either the retrocolic or the antecolic route. The retrocolic reconstruction is conventionally and commonly performed by open surgery. The antecolic route for R-Y reconstruction is favored especially in the laparoscopic procedure with better exposure to the mesenteric defect and lesser mesenteric defects. However, some complications such as internal hernia are closely related with antecolic route for the reason that jejunojejunostomy and Petersen’s defect are created during reconstruction[5].
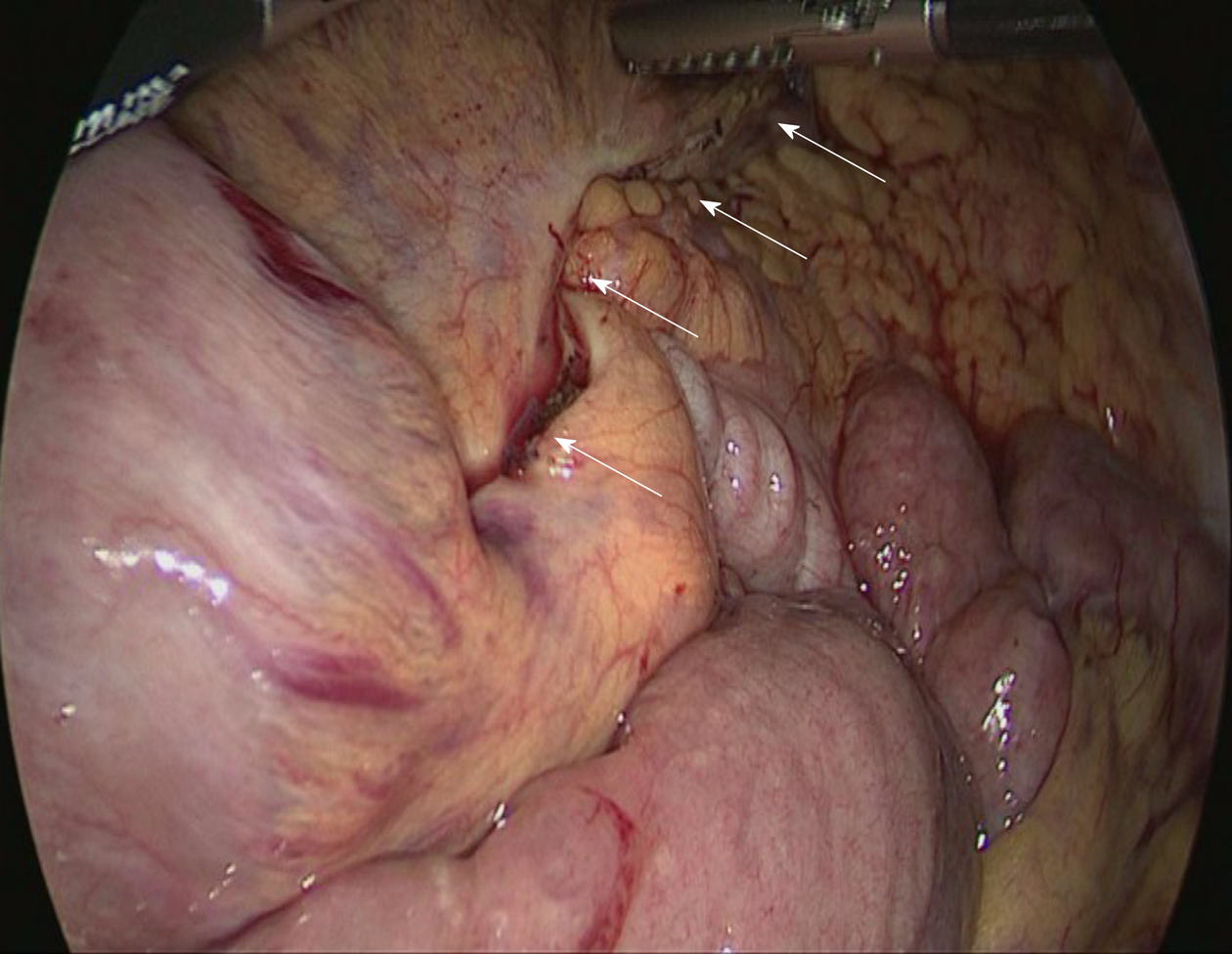
About 10% to 30% of the patients after R-Y reconstruction suffer from Roux stasis syndrome which consists of abdominal pain, vomiting and post-prandial nausea[6]. The pathogenic mechanisms of Roux stasis syndrome are not completely identified. It has been proposed that the occurrence of Roux stasis syndrome is related to functional obstruction of the Roux limb or interruption of electrical conduction caused by amputation of the jejunum[7]. Many improved anastomosis methods were invented, such as uncut R-Y reconstruction or β-shaped R-Y reconstruction[8,9]. However, some of them are technically complex elements and time-consuming. Given that surgical technical factors involving the Roux limb play an important role in the development of these two complications, we developed a method of fixation of Roux limb and duodenal stump to narrow the Petersen’s defect and decrease the development of Roux stasis syndrome (Figure 1).
In this retrospective study, we describe this simple method and report our experience with 31 successful modified laparoscopic Roux-en-Y gastrojejunostomy with fixation of Roux Limb and duodenal stump evaluate feasibility, safety, and short-term outcomes.
Between July 2015 and March 2017, 31 patients with gastric cancer underwent LDG with ante-colic R-Y reconstruction by the same surgeon at the Department of Gastroenterology and Minimally Invasive Surgery at Juntendo University School of Medicine. Clinical parameters included clinicopathologic characteristics, perioperative outcomes, postoperative complication and follow-up data.
Patient positioning and placement of the trocars: The patient was placed in the supine position and general anesthesia was induced. A 12 mm trocar was inserted through the umbilical region by the open method, and carbon dioxide pneumoperitoneum was established. The additional four trocars were placed, including two 12 mm trocars in the right and left lower abdomen and two 5mm trocars in the right and left upper abdomen.
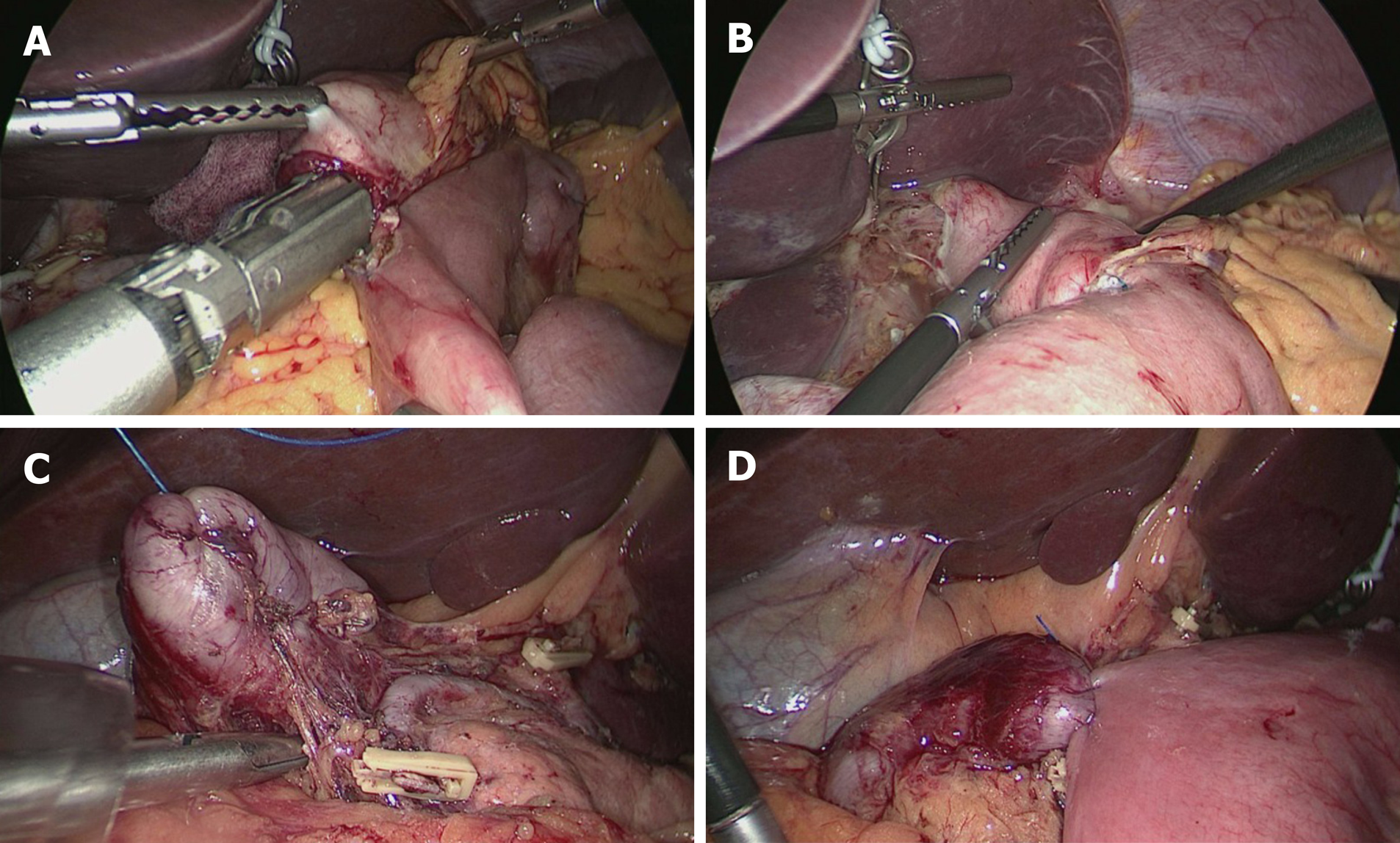
Laparoscopic intracorporeal Roux-en-Y gastrojejunostomy after distal gastrectomy: Laparoscopic mobilization of the stomach and lymph node dissection were performed in a conventional manner. The vagus nerve was not preserved. The duodenum was divided distal to the pylorus with an endoscopic linear stapler (Endo-GIA 60-3, Covidien), then the stomach was divided with two endoscopic linear staplers. Usually one-third or one-fifth of the stomach was preserved. The specimen was removed through an extended 4 cm incision in the umbilical port. The jejunum, 20 cm distal to the ligament of Treitz, was prepared for a Roux limb, and the mesentery of this jejunum was divided for a distance of 8 cm. The prepared jejunum then was divided with an endoscopic linear stapler to ensure a tension free-gastrojejunostomy. A side-side jejunojejunostomy was fashioned 30 cm distal to the planed gastrojejunostomy using endoscopic linear staplers under direct vision through the umbilical incision. The jejunojejunostomy defect was closed with nonabsorbable sutures in an intermittent fashion. Pneumoperitoneum was rebuilt and the jejunal limb was brought to the gastric remnant through an ante-colic route. A right-oriented Roux limb was created such that the cut end of the jejunal limb faced the greater curvature of the gastric remnant (Figure 2A). The jejunal limb was anastomosed to the greater curvature of the stomach side-to-side with an endoscopic stapler, then the site of entry for the linear stapler was closed using a running hand sewn suture (Figure 2B).
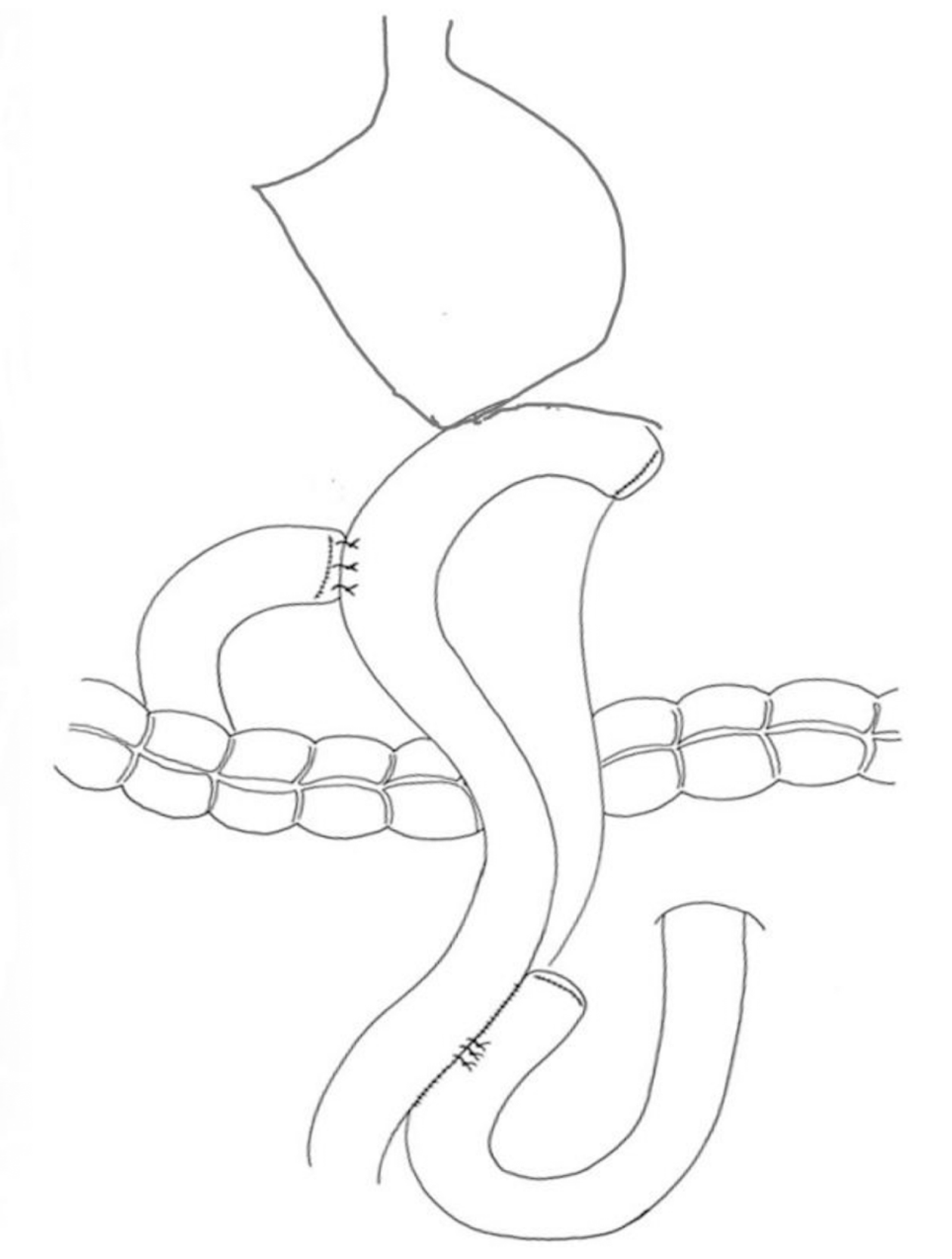
Surgical technique for fixation of Roux limb and duodenal stump: We summarized the surgical procedures as follows. All the procedures were performed laparoscopically. First, the duodenal stump was laparoscopically buried, with suturing performed by hand. The rows of staples on the duodenal stump may then be reinforced by a continuous absorbable seromuscular barbed suture (e.g., 3-0 V-loc, Covidien), which buries the suture line (Figure 2C). Second, the alimentary was then fixed to the duodenal stump at a location to prevent torsion of the Roux limb (Figure 2D). No intention was made to close the Petersen’s defect in any of the patients during the surgery. The final reconstruction is illustrated in Figure 3.
From July 2015 to March 2017, we performed this technique after R-Y reconstruction for gastric cancer in 31 consecutive patients (19 men and 12 women). The characteristics of the patients are shown in Table 1. The mean patient age was 66.2 ± 13.0 years (mean ± SD), and the mean BMI was 21.5 ± 2.7 kg/m2 (mean ± SD). 2 patients had a history of laparotomy. Most of the patients (48.4%) had stage IA gastric cancer according to the pathological staging of gastric cancer.
| Content | |
| Sex | |
| Male | 19 |
| Female | 12 |
| Age | 66.2 ± 13.0 |
| ASA score | |
| 1 | 29 |
| ≥ 2 | 2 |
| Body mass index (kg/m2) | 21.5 ± 2.7 |
| History of laparotomy | 2 |
| Pathological stage | |
| IA | 15 (48.4%) |
| IB | 1 (3.2%) |
| IIA | 2 (6.4%) |
| IIB | 6 (19.4%) |
| IIIA | 6 (19.4%) |
| IIIB | 1 (3.2%) |
The intraoperative data and postoperative outcomes are summarized in Table 2. The operative time was 308.0 ± 84.6 min (mean ± SD). The fixation time was 10 ± 1.6 min (mean ± SD). The blood loss volume was 70.1 ± 76.0 mL (mean ± SD). The number of lymph nodes harvested was 28.9 ± 4.1 (mean ± SD). After LDG, on average, the patients tolerated liquids on the first day and a soft diet on the second postoperative day. The postoperative hospital stay was 13.5 ± 2 d (mean ± SD).
| Content | |
| Operation time (min) | 308.0 ± 84.6 |
| Fixation time (min) | 10 ± 1.6 |
| Intraoperative blood loss (mL) | 70.1 ± 76.0 |
| Conversion to open surgery, n (%) | 0 (0) |
| Extent of lymph node dissection | |
| ≤ D1+ | 16 |
| D2 | 15 |
| Number of lymph nodes harvested | 28.9 ± 4.1 |
| Clear liquids initiated, median (d) | 1 |
| Soft diet initiated, median (d) | 2 |
| Postoperative hospital stay (d) | 13.5 ± 2 |
The postoperative complications are summarized in Table 3. There was no conversion to open surgery in any of the patients. Two patients experienced pneumonia and pancreatitis after surgery, respectively. All patients were discharged with satisfactory recovery and were evaluated postoperatively by routine abdominal computed tomography scan and endoscopy as part of follow-up. The median follow-up period was 44.5 mo (range 37-59 mo). None of the patients had complications related to internal hernia and Roux stasis syndrome during the follow-up period.
| Content | |
| Anastomotic leak or stenosis | 0 (0%) |
| Anastomotic bleeding | 0 (0%) |
| Roux stasis syndrome | 0 (0%) |
| Internal hernia | 0 (0%) |
| Pancreatitis | 1 (3.2%) |
| Pneumonia | 1 (3.2%) |
| Reoperation, n (%) | 0 (0%) |
| Readmission, n (%) | 0 (0%) |
Herein we report our method to reduce post-operative Peterson’s hernia and Roux stasis syndrome in patients undergoing LDG. There are reports that a laparoscopic approach, non-closure of mesenteric defects, and low BMI are independent risk factors for internal hernia by multivariate analysis[10-13]. One study reported a higher incidence of internal hernia after single-port surgery compared to multi-port surgery, resulting from the relatively difficult manipulation of laparoscopic instruments in single-port surgery[13].
The rate of Petersen’s hernia which is a type of internal hernia, with the laparoscopic ante-colic R-Y reconstruction approach without closure of Petersen’s defect, was reportedly 2.6% to 4.75% and generally was thought to be higher than with open approach[5,14,15]. One explanation is that laparoscopic surgery is less likely to form adhesions and promotes earlier intestinal peristalsis than laparotomy, which leads to a higher incidence of internal hernia[16]. Although all defects are closed at the time of the initial surgery, internal hernia still occurs in some cases[15,17]. Previous studies speculated that the large decrease in mesenteric fat after distal gastrectomy might lead to the reopening of the defect despite an initially complete suture[18-20]. An early diagnosis of internal hernia is a challenge for most surgeons because of atypical clinical symptoms and lack of sensitive imaging techniques[17]. Furthermore, the internal hernia may be delayed, so it is necessary to develop an effective technique to prevent an internal hernia during the surgery.
The boundaries of Petersen’s defect are defined as the transverse mesocolon, the mesentery of the Roux limb and the retroperitoneum[21]. Unlike with laparoscopic gastric bypass, subtotal resection of the stomach with lymph node dissection widens the space behind the Roux limb in the ante-colic Roux-Y reconstruction, which may often result in Petersen’s hernia. Closure of all the mesenteric defects with non-absorbable suture in a running fashion was considered the most effective method for preventing internal hernia[5,16,22], however, a tight closure of the Petersen’s defect from the root of the mesentery of the Roux limb and transverse mesocolon to the transverse colon is difficult with the laparoscopic view. As reported by Hirahara et al[16] one way to minimize the defect is to place the residual greater omentum in the defect between the Roux limb and the transverse mesocolon. Although this technique can prevent Petersen’s hernia, it may not be suitable for patients undergoing total resection of the omentum. In our approach to reducing the likelihood of Peterson’s hernia, we initially fix Roux limb onto the duodenal stump with a smooth radian and tension, then change the angle of the opening of Petersen’s defect and narrow the space behind the Roux limb. This procedure decreases the mobility of Roux limb and makes the mesentery of Roux limb and the transverse mesocolon stick tightly. Thus, this technique eliminates the narrowed Petersen’s defect through rapid formation of adhesions behind Roux limb. Compared with the many closure stitches needed to repair Petersen’s defect in a relatively poor exposure, our reported procedure does not require mesentery stitches, is time-saving and is simple and effective. Two large retrospective studies of internal hernia reported that the median interval time after gastrectomy for hernia formation was from 15 mo to 20.9 mo[11,13]. None of the patients developed internal hernias by at least three years of follow-up in this study. To some extent, the follow-up data supports our small change about Roux limb in surgical technique.
In addition, surgical technical factors with Roux limb have been taken into account for the cause of Roux stasis syndrome. Gowen[23] speculated that one of the causes for Roux stasis syndrome is partial obstruction near or at the gastrointestinal anastomosis, but without stomal stenosis. This author analyzed the types of partial obstruction and found that they were related to postoperative adhesions or a kinked loop around the gastrointestinal anastomosis as a result of non-standard surgical techniques. Masui et al[6] also suggested that the adhesion between Roux limb and the suture of the gastric remnant, which was produced a strong bend of Roux limb to the lesser curvature of gastric remnant, could be a cause of Roux stasis syndrome. To prevent this, we fix Roux limb onto the duodenal stump with appropriate tension, which ensures a fluent direction of the gastrointestinal anastomosis by avoiding the angle after the gastroenterostomy. Moreover, through this technique the alimentary limb lies to the right of the ligament of Treitz and does not cross the proximal jejunum (biliopancreatic limb), which allows digestive juices and food to pass smoothly into the distal small intestine.
In conclusion, here we report a case series of a simple and effective method for decreasing the development of Petersen’s hernia and Roux stasis syndrome following R-Y reconstruction. Although Petersen’s hernia is a rare complication of R-Y reconstruction, it is difficult to diagnose and may cause serious postoperative complications that require additional surgery and may even result in death[11,13]. Roux stasis syndrome is also widely reported and results in poor post-operative nutritional status[24-26]. Furthermore, with our described technique, no patients had complications related to internal hernia and Roux stasis syndrome. This technique is a simple and effective method to decrease the incidence of internal hernia and Roux stasis syndrome. There are some limitations in our study. Its retrospective nature may induce some bias. Because of the length of follow up, our study did not provide enough data to show conclusions about long-term outcomes.
Roux-en-Y reconstruction has been one of the standard options after laparoscopic distal gastrectomy. Its complications include Petersen’s hernia and Roux stasis syndrome. Although Petersen’s hernia is a rare complication, it is difficult to diagnose and cause serious postoperative complications. Meanwhile, Roux stasis syndrome is widely reported and reduces the post-operative nutritional status of patients.
Many improved methods were invented for decreasing the incidence of Petersen’s hernia and Roux stasis syndrome, however, some of them are technically complex elements and time-consuming. We developed an easy and effective method to narrow the Petersen’s defect and reduce the development of Roux stasis syndrome using surgical techniques.
The primary objective of the study was to develop an easy and effective method to decrease the development of Petersen’s hernia and Roux stasis syndrome.
We fixed Roux limb onto the duodenal stump in a smooth radian after Roux-en-Y reconstruction. Via this small improvement in Roux limb, Roux limb was placed to the right of the ligament of Treitz. This not only changed the anatomy of the Petersen’s defect, but it also kept a fluent direction of gastrointestinal retrospective analysis review of the data of 31 consecutive patients who was performed this technique between July 2015 and March 2017.
This improvement method took about 10 min. All patients were followed up for at least 3 year, and none of the patients developed postoperative complications related to internal hernia or Roux stasis syndrome.
This 10 min technique is a very effective method to decrease the development of Petersen’s hernia and Roux stasis syndrome in patients who undergo laparoscopic distal gastrectomy
In this study, we report a case series of a simple and effective method for decreasing the development of Petersen’s hernia and Roux stasis syndrome. Because of the length of follow up, our study did not provide enough data to show conclusions about long-term outcomes. We will continue to perform this technique and collect more data to prove the long-term effect of this technique.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhe MM S-Editor: Zhang L L-Editor: A P-Editor: Zhang YL
| 1. | Hirao M, Takiguchi S, Imamura H, Yamamoto K, Kurokawa Y, Fujita J, Kobayashi K, Kimura Y, Mori M, Doki Y; Osaka University Clinical Research Group for Gastroenterological Study. Comparison of Billroth I and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer: one-year postoperative effects assessed by a multi-institutional RCT. Ann Surg Oncol. 2013;20:1591-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Osugi H, Fukuhara K, Takada N, Takemura M, Kinoshita H. Reconstructive procedure after distal gastrectomy to prevent remnant gastritis. Hepatogastroenterology. 2004;51:1215-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Inokuchi M, Kojima K, Yamada H, Kato K, Hayashi M, Motoyama K, Sugihara K. Long-term outcomes of Roux-en-Y and Billroth-I reconstruction after laparoscopic distal gastrectomy. Gastric Cancer. 2013;16:67-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Kojima K, Yamada H, Inokuchi M, Kawano T, Sugihara K. A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg. 2008;247:962-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 132] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Kojima K, Inokuchi M, Kato K, Motoyama K, Sugihara K. Petersen's hernia after laparoscopic distal gastrectomy with Roux-en-Y reconstruction for gastric cancer. Gastric Cancer. 2014;17:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Masui T, Kubora T, Nakanishi Y, Aoki K, Sugimoto S, Takamura M, Takeda H, Hashimoto K, Tokuka A. The flow angle beneath the gastrojejunostomy predicts delayed gastric emptying in Roux-en-Y reconstruction after distal gastrectomy. Gastric Cancer. 2012;15:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Bar-Natan M, Larson GM, Stephens G, Massey T. Delayed gastric emptying after gastric surgery. Am J Surg. 1996;172:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Park JY, Kim YJ. Uncut Roux-en-Y Reconstruction after Laparoscopic Distal Gastrectomy Can Be a Favorable Method in Terms of Gastritis, Bile Reflux, and Gastric Residue. J Gastric Cancer. 2014;14:229-237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Motoyama K, Kojima K, Hayashi M, Kato K, Inokuchi M, Sugihara K. β-Shaped intracorporeal Roux-en-Y reconstruction after totally laparoscopic distal gastrectomy. Gastric Cancer. 2014;17:588-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Miyagaki H, Takiguchi S, Kurokawa Y, Hirao M, Tamura S, Nishida T, Kimura Y, Fujiwara Y, Mori M, Doki Y. Recent trend of internal hernia occurrence after gastrectomy for gastric cancer. World J Surg. 2012;36:851-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Han WH, Eom BW, Yoon HM, Kim YW, Ryu KW. Clinical characteristics and surgical outcomes of internal hernia after gastrectomy in gastric cancer patients: retrospective case control study. Surg Endosc. 2019;33:2873-2879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Kelly KJ, Allen PJ, Brennan MF, Gollub MJ, Coit DG, Strong VE. Internal hernia after gastrectomy for cancer with Roux-Y reconstruction. Surgery. 2013;154:305-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Kang KM, Cho YS, Min SH, Lee Y, Park KB, Park YS, Ahn SH, Park DJ, Kim HH. Internal hernia after gastrectomy for gastric cancer in minimally invasive surgery era. Gastric Cancer. 2019;22:1009-1015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Quebbemann BB, Dallal RM. The orientation of the antecolic Roux limb markedly affects the incidence of internal hernias after laparoscopic gastric bypass. Obes Surg. 2005;15:766-70; discussion 770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Kimura H, Ishikawa M, Nabae T, Matsunaga T, Murakami S, Kawamoto M, Kamimura T, Uchiyama A. Internal hernia after laparoscopic gastrectomy with Roux-en-Y reconstruction for gastric cancer. Asian J Surg. 2017;40:203-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Hirahara N, Matsubara T, Hayashi H, Takai K, Fujii Y, Tajima Y. Easy and secure closure of petersen's defect after laparoscopic distal gastrectomy with Roux-en-Y reconstruction. J Laparoendosc Adv Surg Tech A. 2015;25:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Steele KE, Prokopowicz GP, Magnuson T, Lidor A, Schweitzer M. Laparoscopic antecolic Roux-en-Y gastric bypass with closure of internal defects leads to fewer internal hernias than the retrocolic approach. Surg Endosc. 2008;22:2056-2061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Hope WW, Sing RF, Chen AY, Lincourt AE, Gersin KS, Kuwada TS, Heniford BT. Failure of mesenteric defect closure after Roux-en-Y gastric bypass. JSLS. 2010;14:213-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Miyato H, Kitayama J, Hidemura A, Ishigami H, Kaisaki S, Nagawa H. Vagus nerve preservation selectively restores visceral fat volume in patients with early gastric cancer who underwent gastrectomy. J Surg Res. 2012;173:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Papasavas PK, Caushaj PF, McCormick JT, Quinlin RF, Hayetian FD, Maurer J, Kelly JJ, Gagné DJ. Laparoscopic management of complications following laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2003;17:610-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 97] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Rogers AM, Ionescu AM, Pauli EM. When is a Petersen’s hernia not a Petersen’s hernia. J Am Coll Surg. 2008;207:121-124. [DOI] [Full Text] |
| 22. | Higa KD, Ho T, Boone KB. Internal hernias after laparoscopic Roux-en-Y gastric bypass: incidence, treatment and prevention. Obes Surg. 2003;13:350-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 311] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 23. | Gowen GF. Delayed gastric emptying after Roux-en-Y due to four types of partial obstruction. Ann Surg. 1992;215:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Mathias JR, Fernandez A, Sninsky CA, Clench MH, Davis RH. Nausea, vomiting, and abdominal pain after Roux-en-Y anastomosis: motility of the jejunal limb. Gastroenterology. 1985;88:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 207] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Miedema BW, Kelly KA, Camilleri M, Hanson RB, Zinsmeister AR, O'Connor MK, Brown ML. Human gastric and jejunal transit and motility after Roux gastrojejunostomy. Gastroenterology. 1992;103:1133-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Gustavsson S, Ilstrup DM, Morrison P, Kelly KA. Roux-Y stasis syndrome after gastrectomy. Am J Surg. 1988;155:490-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 141] [Article Influence: 3.8] [Reference Citation Analysis (0)] |