Published online May 27, 2020. doi: 10.4240/wjgs.v12.i5.236
Peer-review started: December 30, 2019
First decision: April 3, 2020
Revised: April 9, 2020
Accepted: May 5, 2020
Article in press: May 5, 2020
Published online: May 27, 2020
Processing time: 144 Days and 18.8 Hours
When gastroesophageal reflux contents reach above the upper esophageal sphincter, patients may, in addition to typical reflux symptoms, present with atypical, extraesophageal symptoms related to laryngopharyngeal reflux (LPR). Surgical treatment of LPR has shown to lead to 70% symptom improvement, however no gold standard for the diagnosis of LPR exists. In 2007, the Restech Dx-pH was released as a valid method to measure acid exposure above the upper esophageal sphincter. Recently, a new software update was introduced for analysis of measured pH data and calculation of composite scores. The effect of the changes applied to the new software version have not yet been analyzed.
To compare results generated by DataView 3 to the most recently released DataView 4.
All patients with gastroesophageal reflux disease symptoms were seen in a specialized surgical outpatient clinic for gastrointestinal function testing. Retrospective chart review was performed of all patients presenting with suspected gastroesophageal reflux disease and extraesophageal reflux symptoms, who underwent laryngopharyngeal pH monitoring using the Restech Dx-pH system (Respiratory Technology Corp., Houston, TX, United States) and simultaneous esophageal pH monitoring. DataView 3 and DataView 4 were used to evaluate Restech studies obtained. Diary entries such as mealtimes, supine and upright periods, and symptoms were entered manually to ensure accuracy and precise conversion of data between both software versions. Paired t test was performed for statistical analysis of results.
A total of 174 patients (63.8% female) met inclusion criteria, all suffering from extraesophageal reflux symptoms as well as typical gastroesophageal reflux disease symptoms. Mean RYAN score upright was 48.77 in DataView 3 compared to 22.17 in DataView 4, showing a significant difference (aP = 0.0001). Similar results were shown for supine period (mean RYAN Score DataView 3 5.29 vs 1.42 in DataView 4, cP = 0.0001). For upright periods 80 patients showed a decrease of value of the RYAN score with a mean of -58.9 (mean 51.1% decrease). For supine position 25 patients showed a decrease of value of the RYAN score with a mean of -15.13 [range (-153.44)–(-0.01)], which equals a mean decrease of value of 44.5%. Ten patients showed no oropharyngeal acid exposure in DataView 3, but mild/moderate (n = 7) or severe (n = 3) acid exposure in DataView 4. Correlation with positive esophageal pH measurement was improved in all 10 patients.
Results of both software versions cannot be compared to each other. However, our data suggests that DataView 4 may be an improvement of the Restech pH measurement in the evaluation of LPR.
Core tip: The Restech Dx-pH is a valid method to measure acid exposure above the upper esophageal sphincter. However, recently a new software update was introduced for calculation of composite scores. Patients with extraesophageal reflux symptoms, who underwent laryngopharyngeal pH monitoring using the Restech Dx-pH system and simultaneous esophageal pH monitoring were evaluated using DataView 3 and DataView 4. A total of 174 patients met inclusion criteria. Mean RYAN score upright and supine differed significantly between both software versions (a,cP = 0.0001) with composite scores mostly decreasing. Our data suggests that DataView 4 may be an improvement of the Restech pH measurement in the evaluation of laryngopharyngeal reflux.
- Citation: Müller DT, Schulte E, Babic B, Knepper L, Fuchs C, Schröder W, Bruns CJ, Leers JM, Fuchs HF. Software improvement for evaluation of laryngopharyngeal pH testing (Restech) – a comparison between DataView 3 and 4. World J Gastrointest Surg 2020; 12(5): 236-246
- URL: https://www.wjgnet.com/1948-9366/full/v12/i5/236.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i5.236
Given its prevalence of 10%-20%, gastroesophageal reflux disease (GERD) is considered one of the most clinically important benign disorders of the upper gastrointestinal tract[1]. The most frequent and typical symptoms of GERD include heartburn, regurgitation, and thoracic pain[2]. However, when gastroesophageal reflux contents reach above the upper esophageal sphincter, patients may also present with atypical, extraesophageal symptoms such as cough, hoarseness, globus, and shortness of breath related to laryngopharyngeal reflux (LPR)[3,4]. Surgical treatment of LPR has shown to lead to 70% of symptom improvement, making it an effective treatment option for selected patients[5]. Yet no gold standard for the diagnosis of LPR exists and due to their multifactorial origin, atypical symptoms can be a great diagnostic challenge, as GERD can be a suggested casualty or an aggravating cofactor[4,6]. In 2007, the Restech Dx-pH (Respiratory Technology Corp., Houston, TX, United States) was released as a valid method to measure acid exposure above the upper esophageal sphincter. The probe is placed slightly lateral to the uvula, and its antimony sensor detects both liquid and aerosolized acid. Because the sensor is able to resist drying out and does not require direct mucosal contact, the Restech pH probe may lead to more reliable results than previous diagnostic tests[7,8]. In addition, the literature has found the Restech Dx pH to have an 80% positive predictive value for a successful outcome of laparoscopic antireflux surgery in patients with primarily extraesophageal symptoms, making it an indispensable diagnostic tool in a preoperative setting[5]. However, previous studies validating the composite score for oropharyngeal pH testing (RYAN Score) and investigating correlation between clinical findings and oropharyngeal pH testing or correlation between esophageal and oropharyngeal pH testing utilized DataView software version 3[4,9,10]. In 2016, a new software update for the Restech Dx pH was released, DataView version 4, replacing DataView version 3 for analysis of measured pH data and calculation of composite scores. The effect of the changes applied to the new software version have not yet been analyzed.
The aim of this study was to compare results generated by DataView 3 to the most recently released DataView 4, and to validate the new software in a large patient cohort following a standardized protocol.
Our academic center is a certified center of excellence for surgery of the upper gastrointestinal tract. All patients with GERD symptoms were seen in a specialized surgical outpatient clinic for gastrointestinal function testing. Retrospective chart review was performed of all patients presenting with suspected gastroesophageal reflux disease and extraesophageal reflux symptoms, as previously defined, who underwent laryngopharyngeal pH monitoring using the Restech Dx-pH system (Respiratory Technology Corp., Houston, TX, United States) between December 2013 and October 2019. Approval of our institutional review board was obtained. Inclusion criteria were age over 18 years and complete gastrointestinal function testing, consisting of High-Resolution Manometry, upper-gastrointestinal endoscopy, contrast radiography, and simultaneous 24 h impedance-pH-monitoring and 24 h Restech pH-monitoring, performed according to the current European Association of Endoscopic Surgery recommendations for management of GERD[2]. All patients were evaluated using standardized symptom questionnaires about quality of life (GIQLI, HRQL) and the presence of symptoms such as heartburn, regurgitation, dysphagia, and extraesophageal symptoms as defined by others[11,12].
Patients underwent simultaneous esophageal and laryngopharyngeal pH-monitoring. Esophageal 24-h impedance pH monitoring was performed with a portable digital data recorder (Digitrapper Mark III, Promedia GmbH, Germany) connected to an antimony dual-sensor pH catheter according to previously described methodology[13]. Patients were instructed to remain in an upright position for the day, and recumbent phases of recording were only permitted at night. In addition, each subject’s diet was restricted to three meals per day and no liquids were allowed between meals. All patients were off PPIs for 7 d. Patients were asked to fill out a detailed diary including mealtimes, exact times of supine and upright periods, and symptoms experienced during the time of the study. Thresholds for distal esophageal pH-monitoring were obtained from Jamieson and coworkers[13]: Reflux episodes were defined as times when the esophageal pH dropped below 4 and evaluated separately for total, upright and supine phases. Test results were classified as abnormal if the percentage of time of esophageal exposure to pH < 4 exceeded 4.5%, 8.4%, and 3.5%, respectively. In addition, a composite score (DeMeester Score) > 14.72 was used define abnormal esophageal acid exposure[14].
Patients underwent simultaneous esophageal and laryngopharyngeal pH-monitoring. Laryngopharyngeal pH monitoring was performed according to a standardized protocol using the Restech pH Dx-pH device (Respiratory Technology Corp., Houston, TX, United States)[8]. Patients were off PPI for 7 d. Its proprietary teardrop-shaped pH sensor utilizes antimony technology, allowing it to measure pH in both liquid and aerosolized form in the oropharynx without the probe drying out. The pH probe is inserted transnasally until the tip of the probe, indicated by a flashing LED light, is seen lateral or slightly distal to the uvula. PH is then measured at a rate of 2 Hz and transmitted to a wireless data recorder. Refluxepisodes in the oropharynx are defined as times when the pH drops below 5.5 in upright and below 5 in supine position. Thresholds for laryngopharyngeal pH measurement were obtained from Ayazi et al[8]. The RYAN score, a composite score developed by Ayazi et al[8], is abnormal if > 9.41 in upright position and > 6.8 in supine position. In addition, the percentages of time of pH below thresholds for upright and supine position were recorded. Reflux episodes recorded during meal periods were excluded from the analysis. Patients abnormal RYAN score in either the upright or supine periods were considered to have a positive Restech study.
All patients underwent upper gastrointestinal endoscopy to identify complications associated with GERD (i.e., erythematous or erosive esophagitis or metaplastic changes). Gastroscopy was typically performed using an EVIS EXERA II GIF-H180 upper-GI-endoscope (Olympus Europa GmbH, Hamburg, Germany). The Los Angeles classification was used for grading of esophagitis if present. Biopsies were taken only if macroscopic lesions were present and analyzed by pathology. The diagnosis of Barrett’s Esophagus was confirmed if intestinal metaplasia was seen by pathology.
Contrast radiography was performed according to a standardized protocol in both upright and supine position and using Valsalva’s maneuver with either a water-soluble contrast medium (Gastrografin®, Bayer Schering Pharma AG, Germany) or barium suspension (Micropaque®, Guerbet GmbH, Sulzbach, Germany). A hiatal hernia was present if the gastroesophageal junction was located > 1 cm above the diaphragm in the supine position in upper G-I contrast radiography.
High Resolution Manometry (ManoScan 360; Sierra Scientific Instruments, Mountain View, CA, United States; Promedia GmbH, Germany) was performed on all patients as previously described[15]. A solid-state catheter with 36 circumferential pressure sensors spaced 1 cm apart along the catheter was passed transnasally until the upper esophageal sphincter and the lower esophageal sphincter/esophagogastric junction were visible. After a short adaptation period, baseline recording began to assess resting characteristics of the upper esophageal sphincter and lower esophageal sphincter according to a standardized protocol. This was followed by 10 swallows of 10 mL of water in a supine position spaced at 30 s intervals. MANOVIEW version 3.0 (Sierra Scientific Instruments, Mountain View, CA, United States; Promedia GmbH, Germany) was used for evaluation of test results. Proximal and distal esophageal margins of the esophagogastric junction were adjusted manually to ensure accuracy. Esophageal body motility was evaluated according to the criteria provided by Kahrilas et al[16]. Percentage of peristaltic contractions was noted with a distal contractile integral cutoff value of 100 mmHg/cm/s for failed peristalsis and 450 mmHg/cm/s for weak peristalsis. Normal esophageal motility was defined as at least 60% of swallows followed by peristaltic contractions, with a mean distal esophageal contraction amplitude greater than 40 mmHg.
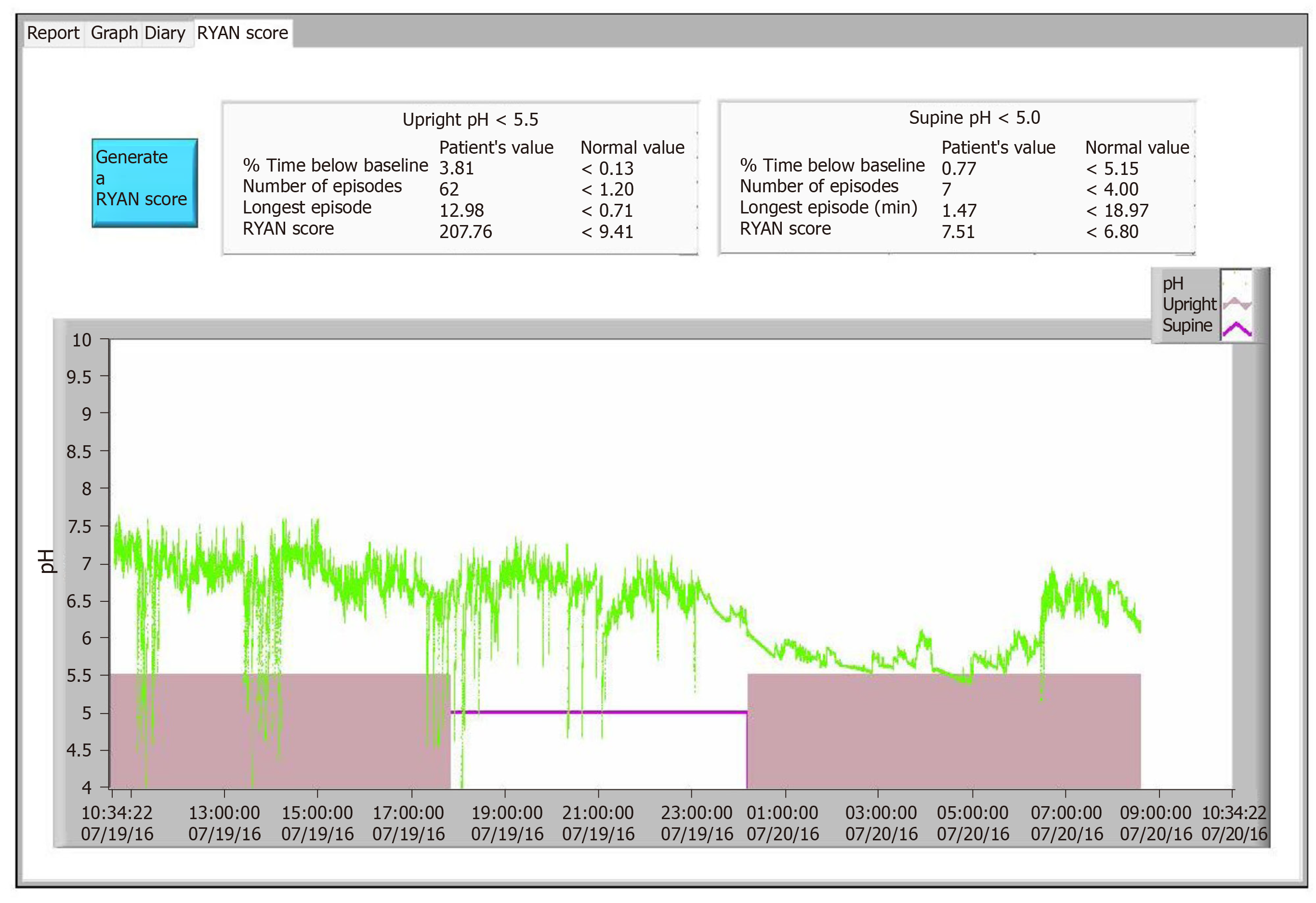
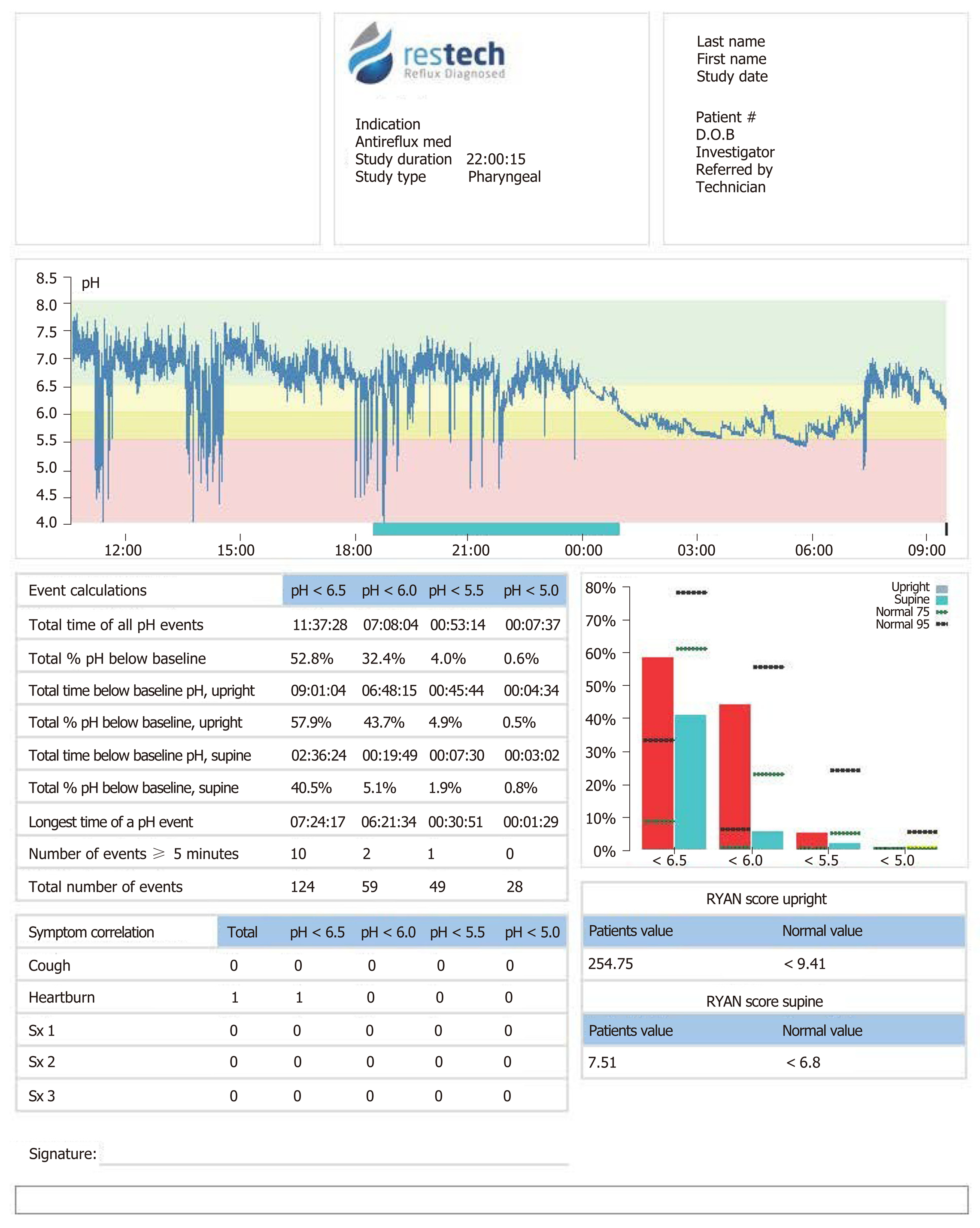
DataView Version 3 and DataView Version 4 were used to evaluate Restech studies obtained as described above. Changes made to DataView 4 included new criteria for when an event is no longer recorded as a single event, as the pH value must now recover 0.1 pH above the threshold, and not drop below that threshold again for 10 s. In practice, this means if the pH drops below the 5.5 threshold, and further decreases, the event is counted until the pH increases above the 5.6 mark and does not drop below the threshold again for 10 s. Furthermore, symptom button presses are not counted for 5 min after a button press of the same type. Correlation between a reflux event and a symptom is applied within +/- 5 min of the first button press. In addition, a cumulative correction factor is subtracted from each data point collected after 24 h to compensate for a pH drift beginning with 0.000002 pH and adding an additional 0.000002 per data point up to 0.34, as this is the total drift in pH over the second 24-h period. Diary entries such as mealtimes, supine and upright periods, and symptoms were entered manually to ensure accuracy and precise conversion of data between both software versions. Figure 1 shows a patient’s study evaluated using DataView 3. Figure 2 shows the same study evaluated using DataView 4.
Demographic data collection included age, gender, body mass index, results from gastrointestinal function testing (i.e., esophageal pH-metry results, Restech pH-metry results, High-Resolution Manometry results, endoscopic findings, contrast radiography), symptoms, and if patients underwent surgical intervention. Continuous variables are presented as means and range. Categorical data are presented as numbers and percentages. Paired Student t-test (for continuous variables) was used for all bivariate analyses. All tests were 2-sided, with statistical significance set at P ≤ 0.05. Data were analyzed by GraphPad (GraphPad Software, San Diego, CA, United States). Statistical review of the displayed data was performed.
A total of 174 patients (63.8% female) met inclusion criteria. All patients presented with extraesophageal reflux symptoms, including chronic cough, hoarseness, and/or sore throat as well as typical GERD symptoms such as regurgitation, dysphagia, and heartburn. Mean body mass index was 25.3 kg/m2, range 18.1–46.8, mean age was 51 years, range 22–85. A total of 44 patients had a history of laparoscopic antireflux surgery. In 16 patients, the Restech measurement was performed postoperatively, whereas 28 patients underwent oropharyngeal pH testing during their preoperative evaluation. For the purpose of software comparison, patients were not grouped according to surgical history.
Table 1 shows a comparison of values of the same pH measurement data analyzed using both software versions. The RYAN Scores upright and supine as well as the percent of time below threshold for upright and supine periods were the only parameters available for analysis in both software versions.
| DataView 3 | DataView 4 | ||||
| mean | Range | mean | Range | P value | |
| RYAN score upright | 48.77 | 2.12-630.6 | 22.17 | 0-287 | 0.0001 |
| % time below threshold upright (pH < 5.5) | 1.21 | 0-19.24 | 1.32 | 0-25.4 | 0.3301 |
| RYAN score supine | 5.29 | 2.17-175.64 | 1.42 | 0-28.86 | 0.0001 |
| % time below threshold supine (pH < 5) | 1.17 | 0-57.41 | 1.42 | 0-61.7 | 0.0069 |
The study next examined patients that initially had an abnormal Restech measurement in DataView 3 defined as a RYAN Score > 9.41 upright and/or > 6.8 supine. Table 2 shows how abnormal values changed while using the new software version DataView 4, evaluated separately for upright and supine periods.
| DataView 3 | Dataiew 4 | P value | |||
| mean | Range | mean | Range | ||
| RYAN score upright | 114.11 | 10.29-630.6 | 51.51 | 0-287 | 0.0001 |
| % time below threshold upright (pH < 5.5) | 2.92 | 0.11-19.24 | 2.94 | 0-2.54 | 0.9181 |
| RYAN score supine | 29.25 | 6.96-175.64 | 9.92 | 0-28.86 | 0.0304 |
| % time below threshold supine (pH < 5) | 10.03 | 0.1-57.41 | 12.16 | 0-61.7 | 0.0069 |
The value for a normal Restech pH measurement showing no abnormal acid exposure during the measurement dropped from 2.12 in upright position and 2.17 supine to 0 in DataView 4. Hence, mean changes between scores were only obtained for patients showing a RYAN score > 2.12 upright or > 2.17 supine. For the upright position, 80 patients showed a decrease of value of the RYAN score with a mean of -58.9 [range (-513.52)–(-0.18)], which equaled a mean decrease of 51.1%. Eighteen patients showed an increase of the RYAN score upright with a mean of 13.66 (range 0.02–175.45), which equaled a mean increase of 191.35%.
For supine position 25 patients showed a decrease of value of the RYAN score with a mean of -15.13 [range (-153.44)–(-0.01)], which equals a mean decrease of value of 44.5%. 4 Patients showed no change between both software versions and 5 patients showed an increase of the RYAN score in DataView 4 with a mean of 0.46 (range 0.01-0.77), which equaled a mean increase of 11.07%.
In 17 patients (9.77%), the RYAN Score upright and/or supine changed from showing abnormal oropharyngeal acid exposure to a normal test result or vice versa. Of those patients who went from an abnormal oropharyngeal acid exposure in DataView 3 to a normal RYAN score in DataView 4 (n = 15), 7 improved correlation with esophageal pH testing as they also showed a normal DeMeester score. One patient went from a normal result in DataView 3 to an abnormal result in DataView 4, improving correlation to an abnormal esophageal pH measurement.
Of the 10 patients that showed no oropharyngeal acid exposure in DataView 3, 7 changed to mild/medium acid exposure in DataView 4 and, 3 to severe acid exposure with a positive RYAN Score. Correlation with positive esophageal pH measurement was improved in all 10 patients. Two patients in this cohort underwent laparoscopic antireflux surgery, resulting in resolution of atypical symptoms. Three patients with a chief complaint of chronic cough showing no oropharyngeal acid exposure in DataView 3 appeared to have abnormal oropharyngeal acid exposure using DataView 4. For 2 of those patients, esophageal pH measurement was available, showing abnormal esophageal acid exposure and an improved correlation between both pH measurements. The third patient showed reflux esophagitis LA Grade A during endoscopy, indicating abnormal acid exposure as shown by an abnormal result of the Restech measurement.
Only 24-h pH measurements were available for analysis for this study. Thereby, the effect of the new correction factor for pH drift could not be examined.
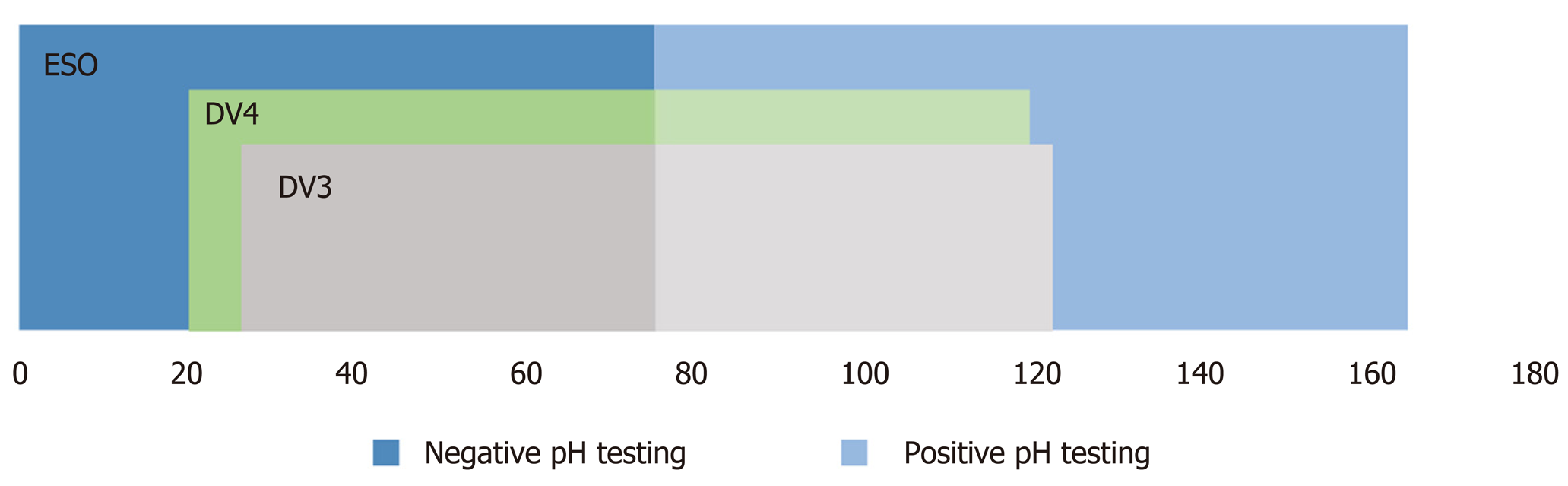
Correlation between esophageal and oropharyngeal pH metry was available for 164 patients. Forty-seven patients showed an abnormal esophageal acid exposure determined by a positive DeMeester Score and an abnormal oropharyngeal acid exposure in DataView 3 determined by a positive RYAN Score upright and/or supine. The same was true for 44 patients using the DataView 4 software. Normal test results for both pH measurements were shown in 49 patients using DataView 3 and 55 patients using DataView 4. Figure 3 shows correlating, and non-correlating test results obtained with both software versions. Overall 58.53% (n = 96) vs 60.37% (n = 99) showed correlation of esophageal and oropharyngeal pH measurement, resulting in no significant difference between both software versions.
The RYAN Score, a composite score calculated with a similar algorithm to the DeMeester Score used for esophageal pH measurement, was first introduced by Ayazi et al[8] in 2009. Normal thresholds and calculating algorithms were determined in 55 healthy subjects. A significant difference between upright and supine values was found, resulting in the development of two separate scores, RYAN Score upright and RYAN Score supine. Parameters used to calculate the RYAN score are percent of time below threshold (pH < 5.5 for upright and pH < 5 for supine), number of episodes and duration of longest episode for upright and supine respectively[8].
DataView 4 introduced changes to the originally validated algorithms of calculation, and the data presented here of a large cohort of patients with atypical symptoms showed a strong significant difference between composite scores calculated by both versions of the DataView software for calculating results of Restech studies. However, significant differences may be due to the fact that a normal oropharyngeal acid exposure was depicted with a RYAN Score of 2.12 upright and 2.17 supine in DataView 3, whereas this changed to a value of 0 in DataView 4. In order to exclude differences created by this change, this study analyzed positive RYAN Scores separately. A significant difference between composite scores of both software versions was again shown for the upright as well as the supine position. In 56.3 % of patients, the value of the RYAN score upright differed between both software versions, with 81.6% showing a score decrease from version 3 to 4 with an average decrease of 51.1%. Similar results were shown for supine position.
It is important to note that significant changes in the RYAN Score upright and supine are not reflected by changes in the percentage of pH below threshold, as no significant changes were shown for this parameter for the upright period. Hence, the change in calculation of the RYAN Score could be caused by a difference in number of episodes and/or the duration of the longest episode, values that are not available for comparison between both software versions as they are not shown separately on the report in DataView 4. A precise analysis of changes in the exact algorithm of calculation is therefore not available.
A previous paper from our group focused on the correlation of esophageal and laryngopharyngeal pH measurement using DataView version 3 and found that both measurements do not necessarily need to correspond[9]. Furthermore, we believe that different reflux scenarios exist, reflected by the four subgroups. One subgroup found 39% of patients had an abnormal esophageal pH metry but a normal Restech measurement (Group A). 23% of patients with a normal esophageal pH metry showed an abnormal Restech measurement (Group B). The other two groups (C and D) showed correlating results of positive-positive and negative-negative, respectively. Particularly in patients with a borderline abnormal esophageal pH measurement, the Restech measurement helped support the decision for or against laparoscopic antireflux surgery. Results from this study utilizing the same criteria used for the previous study showed that correlation to conventional pH metry did not change with the new software version. However, 10 patients with a previously normal measurement showed oropharyngeal acid exposure in DataView 4, and even though not all of them showed severe reflux with a positive RYAN score, correlation to an abnormal esophageal pH measurement was improved. This may suggest that studies evaluated in Data View 4 show an enhanced correlation to esophageal pH testing.
Another study focused on the correlation of clinical findings during laryngoscopy and results of oropharyngeal pH testing. No significant correlation was found, however only a small number of patients (n = 33) was included in the study and trends approaching statistical significance were noted[17]. A previous study has shown the Restech Dx-pH device to have a 69% sensitivity and 100% specificity for the responsiveness to medical therapy in patients with LPR, making it a valuable tool for patients that present with extraesophageal symptoms[18]. Changes made to the new software created the ability to divide abnormal oropharyngeal acid exposure into mild, moderate, or severe reflux. Only severe reflux is depicted in a positive RYAN Score. The effect of those changes and the new classification of reflux severity on the correlation of clinical findings or outcomes has not yet been evaluated.
As patients with primarily atypical symptoms depict a great diagnostic challenge, and due to the lack of specificity of previous diagnostic tests, many studies failed to identify which of these patients would benefit from a surgical intervention[19]. The Restech pH measurement has shown an 80% positive-predictive value for a successful outcome of laparoscopic antireflux surgery in patients with mainly extraesophageal symptoms[5]. A similar conclusion could be made from this research, as symptom improvement or resolution for atypical symptoms was shown for patients with an abnormal Restech test result. Further studies are needed to evaluate the impact of the new RYAN Score on the predictive value of the Restech Dx-pH, but in a preoperative setting, oropharyngeal pH measurement has become an indispensable diagnostic tool especially for those highly selective patients.
Furthermore, improvements made to the new Restech software address confounders that lay in the method of testing itself. Multiple button presses, either due to pressing the wrong button or having overlapping symptoms, previously led to confusion of symptom correlation. The fact that button presses are now only counted for a single symptom within a 5-min period in DataView 4 should result in more accurate symptom correlation. However, a scientific comparison between the old and the new software is not possible, as symptom correlation was not included in the evaluation report of DataView 3. Furthermore, we entered diary entries such as mealtimes, supine and upright periods, and symptoms manually. This ensured, that no wrong button presses were counted for symptom correlation, and that diary entries were accurately converted between both software versions and, importantly, between oropharyngeal and simultaneous esophageal pH measurement, ensuring a valid analysis of correlation between both measurements. However, manual data input relies on good patient compliance, as the patient has to maintain an accurate handwritten diary over the measurement period.
In addition, adding a timing threshold to the definition of an episode should improve specificity of the measurement especially in patients with multiple episodes within a short time period. However, further studies are needed to assess the specificity and sensitivity of the RYAN Score calculated by the new software version.
Limitations of our study include the lack of availability of all parameters affected by the changes applied to the new software version, as the final report created in DataView 3 does not show the same parameters than the report created in DataView 4 and vice versa. In addition, since only 24-h studies were available for analysis, a possible improvement of data by applying a new correction factor for pH drift after 24-h could not be examined. Also, for this study, results obtained from the Restech Dx pH were not evaluated separately depending on if the measurement was performed pre- or postoperatively, resulting in a greater heterogeneity of patient’s groups. Further multicentric studies are needed to evaluate the results of our study.
To our knowledge, this has been the first study analyzing the differences between both software versions using a large patient cohort and a standardized protocol.
In conclusion, this study shows that results of DataView 3 and 4 cannot be compared to each other. This may be especially important when comparing results of clinical research studies performed using DataView version 3. Further multicentric studies are needed to show the impact of the new software on results previously published on the Restech measurement. However, our data suggests that the new software version may be an improvement, dealing with confounders and improving the value of the Restech pH measurement in the evaluation of LPR.
When gastroesophageal reflux contents reach above the upper esophageal sphincter, patients may, in addition to typical reflux symptoms, present with atypical, extraesophageal symptoms related to laryngopharyngeal reflux (LPR). Surgical treatment of LPR has shown to lead to 70% symptom improvement, however no gold standard for the diagnosis of LPR exists. In 2007, the Restech Dx-pH was released as a valid method to measure acid exposure above the upper esophageal sphincter. Recently, a new software update was introduced for analysis of measured pH data and calculation of composite scores. The effect of the changes applied to the new software version have not yet been analyzed.
The aim of this study was to compare results generated by DataView 3 to the most recently released DataView 4, and to validate the new software in a large patient cohort following a standardized protocol. Our results may be especially important when comparing or reproducing results of clinical research studies previously performed using DataView version 3 with data obtained by the new software version 4.
The RYAN Score, the composite score calculated for oropharyngeal pH testing was first introduced in 2009. Normal thresholds and calculating algorithms were determined in 55 healthy subjects. A significant difference between upright and supine values was found, resulting in the development of two separate scores, RYAN Score upright and RYAN Score supine. Parameters used to calculate the RYAN score are percent of time below threshold (pH < 5.5 for upright and pH < 5 for supine), number of episodes and duration of longest episode for upright and supine respectively. DataView 4 introduced changes to the originally validated algorithms of calculation. Changes made included new criteria for when an event is no longer recorded as a single event, symptom button presses are not counted for 5 min after a button press of the same type and subtraction of a cumulative correction factor from each data point collected after 24 h to compensate for a pH drift. Our study compared the scores calculated by DataView 3 to those calculated by 4 as well as the percent of time below threshold for upright and supine periods.
All patients with gastroesophageal reflux disease symptoms were seen in a specialized surgical outpatient clinic for gastrointestinal function testing. Retrospective chart review was performed of all patients presenting with suspected gastroesophageal reflux disease and extraesophageal reflux symptoms, who underwent laryngopharyngeal pH monitoring using the Restech Dx-pH system (Respiratory Technology Corp., Houston, TX, United States) and simultaneous esophageal pH monitoring. DataView 3 and DataView 4 were used to evaluate Restech studies obtained. Diary entries such as mealtimes, supine and upright periods, and symptoms were entered manually to ensure accuracy and precise conversion of data between both software versions. Paired t test was performed for statistical analysis of results.
A total of 174 patients (63.8% female) met inclusion criteria, all suffering from extraesophageal reflux symptoms as well as typical gastroesophageal reflux disease symptoms. Mean RYAN score upright was 48.77 in DataView 3 compared to 22.17 in DataView 4, showing a significant difference (aP = 0.0001). Similar results were shown for supine period (mean RYAN Score DataView 3 5.29 vs 1.42 in DataView 4, cP = 0.0001). For upright periods 80 patients showed a decrease of value of the RYAN score with a mean of -58.9 (mean 51.1% decrease). For supine position 25 patients showed a decrease of value of the RYAN score with a mean of -15.13 [range (-153.44)–(-0.01)], which equals a mean decrease of value of 44.5%. Ten patients showed no oropharyngeal acid exposure in DataView 3, but mild/moderate (n = 7) or severe (n = 3) acid exposure in DataView 4. Correlation with positive esophageal pH measurement was improved in all 10 patients. Since only 24-h studies were available for analysis, a possible improvement of data by applying a new correction factor for pH drift after 24-h could not be examined. Also, for this study, results obtained from the Restech Dx pH were not evaluated separately depending on if the measurement was performed pre- or postoperatively, resulting in a greater heterogeneity of patient’s groups. Further multicentric studies are needed to evaluate the results of our study.
Overall, this study shows that results of DataView 3 and 4 cannot be compared to each other. This may be especially important when comparing results of clinical research studies performed using DataView version 3. However, our data suggests that the new software version may be an improvement, dealing with confounders and improving the value of the Restech pH measurement in the evaluation of LPR.
Further multicentric studies are needed to show the impact of the new software on results previously published on the Restech measurement. In addition, 48-h oropharyngeal pH studies are needed to analyze the impact of the new correction factor applied for pH drift on the measured data.
The authors wish to acknowledge Andrew Krauss for proofreading of the manuscript.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Inamori M, Tchilikidi KY S-Editor: Zhang L L-Editor: A E-Editor: Zhang YL
| 1. | Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1256] [Cited by in RCA: 1262] [Article Influence: 63.1] [Reference Citation Analysis (0)] |
| 2. | Fuchs KH, Babic B, Breithaupt W, Dallemagne B, Fingerhut A, Furnee E, Granderath F, Horvath P, Kardos P, Pointner R, Savarino E, Van Herwaarden-Lindeboom M, Zaninotto G; European Association of Endoscopic Surgery (EAES). EAES recommendations for the management of gastroesophageal reflux disease. Surg Endosc. 2014;28:1753-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 3. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-20; quiz 1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2368] [Cited by in RCA: 2454] [Article Influence: 129.2] [Reference Citation Analysis (2)] |
| 4. | Becker V, Drabner R, Graf S, Schlag C, Nennstiel S, Buchberger AM, Schmid RM, Saur D, Bajbouj M. New aspects in the pathomechanism and diagnosis of the laryngopharyngeal reflux-clinical impact of laryngeal proton pumps and pharyngeal pH metry in extraesophageal gastroesophageal reflux disease. World J Gastroenterol. 2015;21:982-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 5. | Worrell SG, DeMeester SR, Greene CL, Oh DS, Hagen JA. Pharyngeal pH monitoring better predicts a successful outcome for extraesophageal reflux symptoms after antireflux surgery. Surg Endosc. 2013;27:4113-4118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Koop H, Fuchs KH, Labenz J, Lynen Jansen P, Messmann H, Miehlke S, Schepp W, Wenzl TG; Mitarbeiter der Leitliniengruppe. [S2k guideline: gastroesophageal reflux disease guided by the German Society of Gastroenterology: AWMF register no. 021-013]. Z Gastroenterol. 2014;52:1299-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Issing WJ, Karkos PD, Perreas K, Folwaczny C, Reichel O. Dual-probe 24-hour ambulatory pH monitoring for diagnosis of laryngopharyngeal reflux. J Laryngol Otol. 2004;118:845-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Ayazi S, Lipham JC, Hagen JA, Tang AL, Zehetner J, Leers JM, Oezcelik A, Abate E, Banki F, DeMeester SR, DeMeester TR. A new technique for measurement of pharyngeal pH: normal values and discriminating pH threshold. J Gastrointest Surg. 2009;13:1422-1429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Fuchs HF, Müller DT, Berlth F, Maus MK, Fuchs C, Dübbers M, Schröder W, Bruns CJ, Leers JM. Simultaneous laryngopharyngeal pH monitoring (Restech) and conventional esophageal pH monitoring-correlation using a large patient cohort of more than 100 patients with suspected gastroesophageal reflux disease. Dis Esophagus. 2018;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Mazzoleni G, Vailati C, Lisma DG, Testoni PA, Passaretti S. Correlation between oropharyngeal pH-monitoring and esophageal pH-impedance monitoring in patients with suspected GERD-related extra-esophageal symptoms. Neurogastroenterol Motil. 2014;26:1557-1564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Velanovich V. Comparison of generic (SF-36) vs. disease-specific (GERD-HRQL) quality-of-life scales for gastroesophageal reflux disease. J Gastrointest Surg. 1998;2:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 158] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 12. | Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmülling C, Neugebauer E, Troidl H. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. Br J Surg. 1995;82:216-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 852] [Cited by in RCA: 885] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 13. | Jamieson JR, Stein HJ, DeMeester TR, Bonavina L, Schwizer W, Hinder RA, Albertucci M. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol. 1992;87:1102-1111. [PubMed] |
| 14. | Neto RML, Herbella FAM, Schlottmann F, Patti MG. Does DeMeester score still define GERD? Dis Esophagus. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 15. | Gyawali CP, Patel A. Esophageal motor function: technical aspects of manometry. Gastrointest Endosc Clin N Am. 2014;24:527-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 16. | Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE; International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1373] [Cited by in RCA: 1451] [Article Influence: 145.1] [Reference Citation Analysis (0)] |
| 17. | Agrawal N, Yadlapati R, Shabeeb N, Price CP, Lidder A, Shintani-Smith S, Bové M, Pandolfino J, Tan B. Relationship between extralaryngeal endoscopic findings, proton pump inhibitor (PPI) response, and pH measures in suspected laryngopharyngeal reflux. Dis Esophagus. 2019;32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Vailati C, Mazzoleni G, Bondi S, Bussi M, Testoni PA, Passaretti S. Oropharyngeal pH monitoring for laryngopharyngeal reflux: is it a reliable test before therapy? J Voice. 2013;27:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Swoger J, Ponsky J, Hicks DM, Richter JE, Abelson TI, Milstein C, Qadeer MA, Vaezi MF. Surgical fundoplication in laryngopharyngeal reflux unresponsive to aggressive acid suppression: a controlled study. Clin Gastroenterol Hepatol. 2006;4:433-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |