Published online Apr 27, 2020. doi: 10.4240/wjgs.v12.i4.129
Peer-review started: December 31, 2019
First decision: February 19, 2020
Revised: March 15, 2020
Accepted: March 28, 2020
Article in press: March 28, 2020
Published online: April 27, 2020
Processing time: 113 Days and 14.5 Hours
Complicated acute appendicitis (CAA) is a serious condition and carries significant morbidity in children. A strict diagnosis is challenging, as there are many lesions that mimic CAA. The management of CAA is still controversial. There are two options for treatment: Immediate operative management and non-operative management with antibiotics and/or drainage of any abscess or phlegmon. Each method of treatment has advantages and disadvantages. Operative management may be difficult due to the presence of inflamed tissues and may lead to detrimental events. In many cases, non-operative management with or without drainage and interval appendectomy is advised. The reasons for this approach include new medications and policies for the use of antibiotic therapy. Furthermore, advances in radiological interventions may overcome difficulties such as diagnosing and managing the complications of CAA without any surgeries. However, questions have been raised about the risk of recurrence, prolonged use of antibiotics, lengthened hospital stay and delay in returning to daily activities. Moreover, the need for interval appendectomy is currently under debate because of the low risk of recurrence. Due to the paucity of high-quality studies, more randomized controlled trials to determine the precise management strategy are needed. This review aims to study the current data on operative vs non-operative management for CAA in children and to extract any useful information from the literature.
Core tip: The management of paediatric patients with complicated acute appendicitis (CAA) is controversial. There are two options for treatment: non-operative management with antibiotics and/or drainage of any abscess or phlegmon and immediate operative management. Each method has advantages and disadvantages. However, operative management is suggested for CAA with perforation, while non-operative management is advised for CAA with abscess or phlegmon. There is a paucity of high-quality studies in the current literature. Further investigations with randomized control studies are warranted.
- Citation: Zavras N, Vaos G. Management of complicated acute appendicitis in children: Still an existing controversy. World J Gastrointest Surg 2020; 12(4): 129-137
- URL: https://www.wjgnet.com/1948-9366/full/v12/i4/129.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i4.129
Appendectomy for acute appendicitis (AA) in children persists as the most common abdominal surgery for paediatric surgeons[1]. It has been estimated that 70000 children are operated on for AA every year in the United States[2]. The lifetime risk of appendectomy is 23.1% for females and 12% for males[3], and the lifetime risk of developing AA is 6.7% for females and 8.6% for males[4]. Interestingly, the peak incidence of AA occurs from ages 10-14 years for males and 15-19 years for females[4].
The clinical history of AA can vary from mild symptoms (uncomplicated AA) to those with sepsis and bowel obstruction [complicated AA (CAA)] with perforation of the appendix and probably development of an intraperitoneal abscess[5]. Approximately 30%-74% of children present with CAA[6], with rates ranging between 69%-93% for children aged 2 to 5 years and up to 100% for 1-year-old children[7]. Although operative management has been considered for many years as the mainstay of treatment in children with AA[8], the presence of distorted anatomy due to inflamed tissues may lead to harmful events such as injury to the surrounding tissues and bowel wall, dissemination of the infection, blood loss, postoperative bowel obstruction, abscess or fistula formation, and postoperative wound complications[2,9,10].
The evidence that AA can be managed with non-operative management is not new. The first case of a spontaneous resolution of CAA was published in 1910[11]. In 1956 and in 1959, Coldrey[12] published a series of 137 patients with AA successfully treated with non-operative management. Almost two decades later, Janik et al[13] reported the successful management of 31/37 children with a palpable mass and no established peritonitis with the administration of fluids and close monitoring. In the mid-1990s, the interest in non-operative management in the adult population was renewed, and since then, a number of studies have investigated the efficiency and safety of non-operative management, first in uncomplicated AA and later in CAA[14,15]. Although the literature on paediatric patients is still limited, ongoing evidence indicates that non-operative management may be effective and safe for the management of uncomplicated AA[16,17].
Despite modern diagnostic adjuncts such as imaging techniques and improvements in anaesthetic and surgical care, controversies in the optimal management of CAA in the paediatric population still exist[18].
Taking into account recent improvements in the management of CAA, this review aims to provide an update on the existing controversies in operative management vs non-operative management for children with CAA.
A literature review was performed through PubMed and Google Scholar for original articles, reviews and meta-analyses from 1980 to December 2019 using the following Medical Subjects Headings (MeSH) terms: “appendicitis” [MeSH] and “complicated appendicitis” [MeSH] or “appendicular mass” [MeSH] or “abscess” [MeSH] or “phlegmon” [MeSH] or ‘’perforated” [MeSH] or “conservative treatment” [MeSH] or “operative treatment” [MeSH] or “interval appendectomy” [MeSH] and “children”. A secondary search of the most relevant articles was also conducted manually or through PubMed based on the related articles. All randomized controlled trials (RCTs), prospective and retrospective articles and systematic reviews were included. Articles including both adult and paediatric populations and papers based on case reports, case series, abstracts and letters were excluded. All articles were selected systematically for inclusion and critically evaluated.
CAA was defined as perforated appendicitis with or without the presence of an abscess or phlegmon[2] based on the surgeon’s findings during operation or the pathology report[19]. A phlegmon was defined as an inflammatory mass without an apparently defined abscess[19].
Operative management was defined as an early appendectomy performed either with laparotomy or laparoscopy within the first 24 h of hospitalization[20].
Non-operative management was defined as initial treatment with or without percutaneous abscess drainage for an abscess followed by interval appendectomy[21].
Treatment failure of non-operative management and percutaneous abscess drainage was defined as the need for an appendectomy operation during the same hospitalization period or within 7 d after discharge[22].
The complications included any surgical, medical or interventional adverse events (postoperative wound infection, small bowel obstruction, abscess or fistula formation) [2,9,10].
Hospital length of stay (LOS) for both operative management and non-operative management was defined as the total number of hospitalization days from admission to discharge and was calculated after reading the relevant articles in the literature.
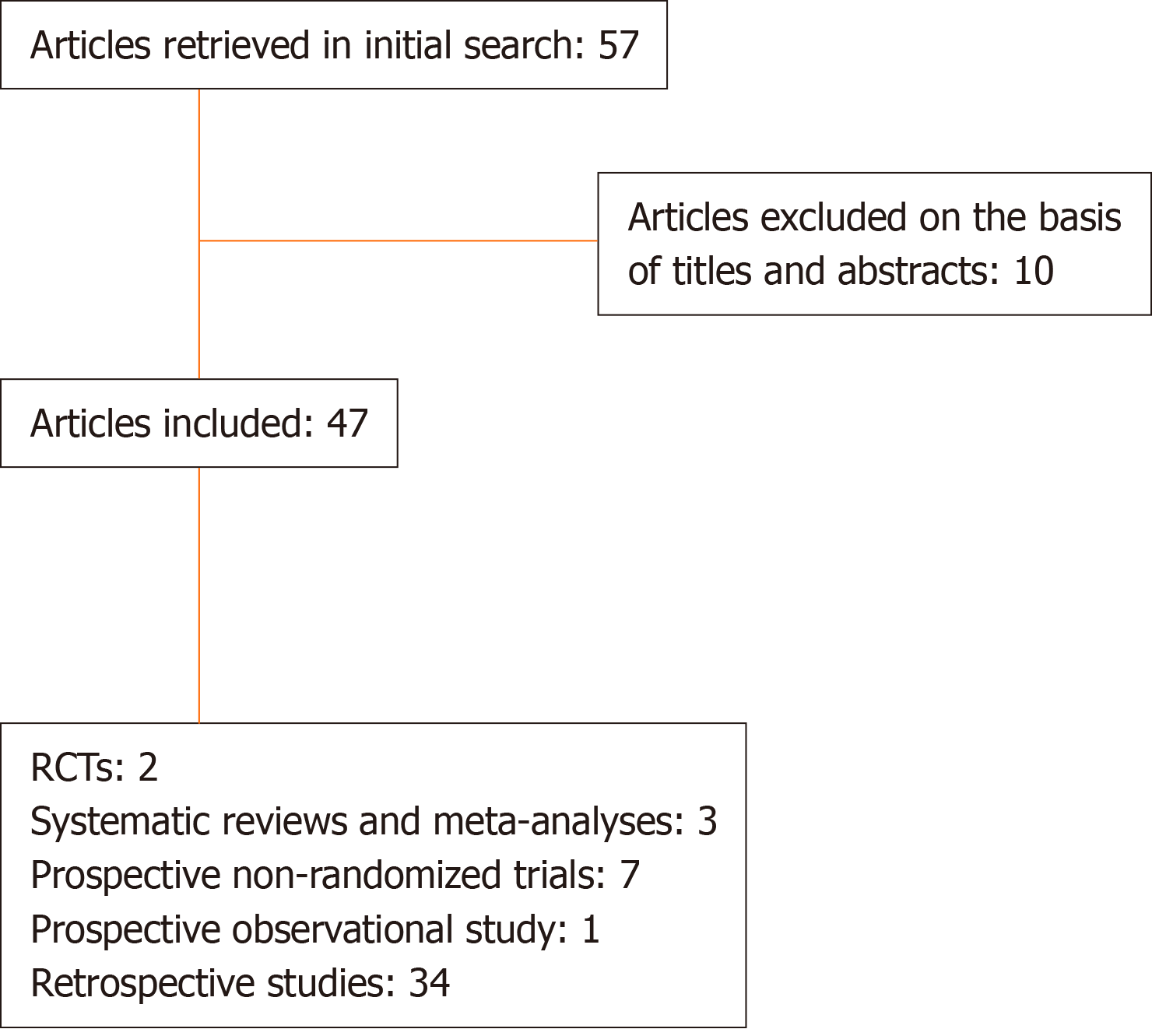
We included 47 articles published from August 1980 to December 2019 relevant to the management of CAA in children. Of them, three[23-25] were systematic reviews and meta-analyses, two[26,27] were prospective RCTs, seven were prospective non-randomized trials[28-34], one was a prospective observational study[35], and thirty-four[9,13,19-21,36-64] were retrospective studies (Figure 1). The therapeutic options regarding CAA are analysed in detail below.
Once a paediatric surgeon has to treat a patient with CAA, there are three strategies available for treatment: Antibiotics only, antibiotics followed by interval appendectomy, and appendectomy on admission (Table 1). We will separately discuss the three options with the pros and cons of each strategy.
| Non-operative management | Operative management |
| Antibiotic treatment | Immediate operative management |
| Percutaneous abscess drainage | Non-operative management followed by interval appendectomy |
Advances in antibiotic policy: Currently, the standard of care endorses the prompt administration of antibiotics in the management of CAA[65,66]. A survey of the European Pediatric Surgeons’ Association covering 42 countries (24 were from Europe) showed that 96% of surgeons start antibiotic therapy preoperatively in the case of CAA[66]. The same study showed that most surgeons choose a triple “standard therapy” comprising an aminoglycoside, a β-lactam and a regimen covering anaerobes. However, there is growing evidence that broad-spectrum single (piperacillin/tazobactam) or double-agent (ceftriaxone + metronidazole) therapy is equally effective and less expensive than triple-agent therapy and may lead to a shorter LOS[67-70]. This is in line with the recommendations of the American Pediatric Surgical Association (APSA) that state that broad-spectrum single or double-agent therapy is equally efficient and more cost-effective than three drugs[65]. It is noteworthy that a slight shift toward mono- or dual-agent therapy could be observed in the literature after the publication of the APSA recommendations[21,54].
A major issue arises from the use of broad-spectrum anti-Pseudomonas antibiotics such as piperacillin/tazobactam, imipenem or meropenem, vs narrow-spectrum antibiotics such as cefoxitin or cefazolin with metronidazole[70]. The clinical guidelines recommend the use of narrow-spectrum antibiotics in adults with complicated intra-abdominal infections and in most previously healthy children with uncomplicated AA who are not assumed to be susceptible to P. aeruginosa[71]. Kronman et al[71], in a large, retrospective cohort study of children suffering from either uncomplicated AA or CAA, showed that broad-spectrum antibiotics are not superior to narrow-spectrum antibiotics with respect to short-term postoperative complications, e.g., readmission rates, wound infections, bowel obstruction, and percutaneous drainage of abscesses, within 30 d of discharge. Researchers have shown that antibiotic agents with an expanded spectrum against P. aeruginosa and Enterococcus were efficient in 78% of patients who failed first-line antibiotics and helped them achieve successful non-operative management[72]. In such cases, second-line antibiotics are recommended before surgical intervention[71]. An important question concerns the duration of antibiotics use in children with CAA and non-operative management. The APSA recommendations suggest that the length of antimicrobial agent use should be based on clinical criteria such as pain, fever, bowel function and white blood cell count[43]. Usually, a 5-d policy for intravenous antibiotics followed by a 2-d regimen of oral antibiotics (total 7-d length of antibiotics use) is recommended[65]. This suggestion was supported further by a very late systematic review and meta-analysis that showed that the transition from intravenous to oral administration did not raise the risks for complications such as wound infection, postoperative abscess and re-admission[73].
Antibiotic treatment: The common indications that CAA demands urgent operative intervention has changed in the last decade. Several centres have reported the results of children with appendiceal abscesses or masses treated with antibiotics, both with or without drainage[29,32,35,36,40,43,50,54-56,58,59]. Most of these studies revealed a success rate between 60-100%. However, Svensson et al[74] questioned the results of some of these studies because the majority of them were retrospective and included meaningful selection bias. Furthermore, without an operation, it is difficult to declare that all patients had definite CAA despite appropriate blood tests and radiological imaging. Although the presence of an appendicolith is thought to be a predictor of non-operative management failure[50,54] and recurrence, other researchers found no correlation between this factor and the outcomes[75].
We conclude that the optimal antimicrobial therapy and duration of antibiotics use in children with CAA need further investigation with RCTs.
Percutaneous abscess drainage: During the 1980s, a period of growth and acceptance of radiological interventional techniques in children started[76]. Percutaneous abscess drainage is a well-established procedure of choice for treating intra-abdominal abscesses of various aetiologies[77]. In the case of CAA, an intra-abdominal abscess may occur either before or after appendectomy and may be found anywhere in the abdominal cavity and/or pelvis[64]. Drainage is usually performed with the Seldinger technique under ultrasound or computed tomography (CT) guidance or a combination of both imaging modalities[64]. In the case of peri-appendicular abscesses, the anterior abdominal transperitoneal approach is usually performed[78,79], while for abscesses located anterior to the rectum, the transrectal or transgluteal approach may be used[79].
The incidence of intra-abdominal or pelvis abscesses is estimated to be approximately 3.8% in patients with CAA[80]. A delay in the diagnosis of AA is a possible risk factor, although there is evidence that some patients might be prone to abscess formation despite prompt management[81]. Several authors[26,53,54,57,61,62] have documented beneficial results with percutaneous abscess drainage in terms of reduced complication rates, acceptable LOS, and rapid recovery to oral feeding and return to normal activities. In a European Pediatric Surgeons’ Association survey, 59% of paediatric surgeons suggested a combination of antibiotics and percutaneous abscess drainage[66]. Luo et al[57], in a large series of children with appendiceal abscesses, found that patients treated with non-operative management and percutaneous abscess drainage had a significantly lower percentage of recurrent appendicitis, a lower possibility of requiring an interval appendectomy, and fewer postoperative complications after interval appendectomy than those without percutaneous abscess drainage. In contrast, Bonadio et al[58] reported a greater LOS, longer mean duration of fever, longer period of antibiotics use, more radiological procedures, higher complication rates and more unscheduled hospitalizations after discharge for patients who received percutaneous abscess drainage. Keckler et al[52] mentioned that multiple CT scans and major complications may follow percutaneous abscess drainage, such as ileal, colonic and bladder perforation and buttock/thigh abscesses, while in the interval appendectomy group, only one patient developed a pelvic phlegmon that responded to intravenous antibiotics. Gasior et al[64] suggested that only abscesses greater than 20 cm2 should be drained. Some authors advocate for the installation of a tissue plasminogen activator into the abdominal cavity[82] to facilitate drainage of thick and septated abscesses. In a recent RCT, St Peter et al[83] found that compared to the control group. patients who underwent tissue plasminogen activator installation had a longer duration of hospitalization, while no differences concerning the use of antibiotics, drainage duration or total hospitalization were found.
We could conclude that although arguments may be raised for percutaneous abscess drainage, there is evidence that drainage of the abdominal cavity may have favourable results in selected patients.
Immediate operative management vs non-operative management with delayed appendectomy: Although many studies[23,26,27,55] propose early operative management for children with CAA, there are only two RCTs supporting this option for treatment. In the first study[26], 40 patients with similar characteristics on admission and a diagnosis of CAA were randomized to immediate operative management and non-operative management group, with the latter undergoing delayed appendectomy. Patients operated on early had fewer health care visits and CT scans than those with delayed surgery. No better outcomes were found in the non-operative management group than in the operative management group. Blakely et al[27] studied a cohort of 131 patients who were diagnosed with perforated appendicitis without abscess on admission, and they were randomized in a non-blinded manner for early operative management or non-operative management followed by interval appendectomy. The authors found that patients in the non-operative management group had higher complication rates and higher hospital charges than those in the operative management group. On the other hand, a meta-analysis by Duggan et al[23] showed that early appendectomy for patients with perforated appendicitis without abscess significantly reduced unplanned readmissions [Odds ratio (OR) = 0.08, 95% confidence interval (CI): 0.01-0.67], adverse events (OR = 0.28, 95%CI: 0.1-0.77) and total charges. A recent meta-analysis by Vaos et al[24] reported that operative management was associated with shorter LOS (SD = 0.25, 95%CI: 0.07-0.43, P = 0.007), but the overall complication rates (OR = 0.22, 95%CI: 0.14-0.38, P = 0.001) and incidence of wound infection(OR = 0.40, 95%CI: 0.17-0.96, P = 0.041) were significantly lower with non-operative management. The presence of intra-abdominal abscess and postoperative ileus was not affected by the treatment option. In a recent meta-analysis, Fugazzola et al[25] separately studied patients with free perforated appendicitis and those with abscess or phlegmon. The researchers reported better outcomes regarding complication rates and readmissions in patients with appendicular abscess or phlegmon treated with non-operative management. In contrast, the authors found a lower complication rate and fewer re-admissions for the group of patients with free perforated appendicitis treated with operative management.
Summarizing the results of the abovementioned studies, it seems that there are two main types of CAA: CAA with perforation without abscess and CAA with abscess or phlegmon. The main conclusion is that operative management is the preferred treatment option for patients with perforated appendicitis without abscess, while non-operative management is advised in cases of perforated appendicitis with abscess or phlegmon.
Although AA is a common surgical disease, it may be expressed with a wide range of severity, ranging from simple to severe. In the case of CAA, operative management seems to be the preferable choice of treatment, while non-operative management is recommended for CAA with abscess or phlegmon. However, because of the paucity of high-quality studies, there is a need for more RCTs to determine the precise management strategy.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ho CM, Aydin M S-Editor: Wang YQ L-Editor: A E-Editor: Xing YX
| 1. | Omling E, Salö M, Saluja S, Bergbrant S, Olsson L, Persson A, Björk J, Hagander L. Nationwide study of appendicitis in children. Br J Surg. 2019;106:1623-1631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | López JJ, Deans KJ, Minneci PC. Nonoperative management of appendicitis in children. Curr Opin Pediatr. 2017;29:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | Howell EC, Dubina ED, Lee SL. Perforation risk in pediatric appendicitis: assessment and management. Pediatric Health Med Ther. 2018;9:135-145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1307] [Cited by in RCA: 1301] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 5. | Richardsen I, Schöb DS, Ulmer TF, Steinau G, Neumann UP, Klink CD, Lambertz A. Etiology of Appendicitis in Children: The Role of Bacterial and Viral Pathogens. J Invest Surg. 2016;29:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Ponsky TA, Huang ZJ, Kittle K, Eichelberger MR, Gilbert JC, Brody F, Newman KD. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292:1977-1982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 209] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 7. | Nance ML, Adamson WT, Hedrick HL. Appendicitis in the young child: a continuing diagnostic challenge. Pediatr Emerg Care. 2000;16:160-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 126] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Hall NJ, Eaton S. Non-operative management of appendicitis in children. Arch Dis Child. 2018;103:498-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Gillick J, Velayudham M, Puri P. Conservative management of appendix mass in children. Br J Surg. 2001;88:1539-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Lasson A, Lundagårds J, Lorén I, Nilsson PE. Appendiceal abscesses: primary percutaneous drainage and selective interval appendicectomy. Eur J Surg. 2002;168:264-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Coccolini F, Fugazzola P, Sartelli M, Cicuttin E, Sibilla MG, Leandro G, De' Angelis GL, Gaiani F, Di Mario F, Tomasoni M, Catena F, Ansaloni L. Conservative treatment of acute appendicitis. Acta Biomed. 2018;89:119-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 12. | Coldrey E. Treatment of Acute Appendicitis. Br Med J. 1956;2:1458-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Janik JS, Ein SH, Shandling B, Simpson JS, Stephens CA. Nonsurgical management of appendiceal mass in late presenting children. J Pediatr Surg. 1980;15:574-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 284] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 15. | Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010;147:818-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 223] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Xu J, Liu YC, Adams S, Karpelowsky J. Acute uncomplicated appendicitis study: rationale and protocol for a multicentre, prospective randomised controlled non-inferiority study to evaluate the safety and effectiveness of non-operative management in children with acute uncomplicated appendicitis. BMJ Open. 2016;6:e013299. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Hall NJ, Eaton S, Abbo O, Arnaud AP, Beaudin M, Brindle M, Bütter A, Davies D, Jancelewicz T, Johnson K, Keijzer R, Lapidus-Krol E, Offringa M, Piché N, Rintala R, Skarsgard E, Svensson JF, Ungar WJ, Wester T, Willan AR, Zani A, St Peter SD, Pierro A. Appendectomy versus non-operative treatment for acute uncomplicated appendicitis in children: study protocol for a multicentre, open-label, non-inferiority, randomised controlled trial. BMJ Paediatr Open. 2017;1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 684] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 19. | Roach JP, Partrick DA, Bruny JL, Allshouse MJ, Karrer FM, Ziegler MM. Complicated appendicitis in children: a clear role for drainage and delayed appendectomy. Am J Surg. 2007;194:769-72; discussion 772-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Tsai HY, Chao HC, Yu WJ. Early appendectomy shortens antibiotic course and hospital stay in children with early perforated appendicitis. Pediatr Neonatol. 2017;58:406-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Badru F, Piening N, Munoz Abraham AS, Osei H, Greenspon J, Chatoorgoon K, Fitzpatrick C, Villalona GA. Abscess and symptoms duration upon presentation should guide decision algorithms for early versus interval appendectomy in children. Pediatr Neonatol. 2019;60:530-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Olsen J, Skovdal J, Qvist N, Bisgaard T. Treatment of appendiceal mass--a qualitative systematic review. Dan Med J. 2014;61:A4881. [PubMed] |
| 23. | Duggan EM, Marshall AP, Weaver KL, St Peter SD, Tice J, Wang L, Choi L, Blakely ML. A systematic review and individual patient data meta-analysis of published randomized clinical trials comparing early versus interval appendectomy for children with perforated appendicitis. Pediatr Surg Int. 2016;32:649-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Vaos G, Dimopoulou A, Gkioka E, Zavras N. Immediate surgery or conservative treatment for complicated acute appendicitis in children? A meta-analysis. J Pediatr Surg. 2019;54:1365-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Fugazzola P, Coccolini F, Tomasoni M, Stella M, Ansaloni L. Early appendectomy vs. conservative management in complicated acute appendicitis in children: A meta-analysis. J Pediatr Surg. 2019;54:2234-2241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 26. | St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM, Murphy JP, Snyder CL, Sharp RJ, Andrews WS, Holcomb GW, Ostlie DJ. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010;45:236-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 27. | Blakely ML, Williams R, Dassinger MS, Eubanks JW, Fischer P, Huang EY, Paton E, Culbreath B, Hester A, Streck C, Hixson SD, Langham MR. Early vs interval appendectomy for children with perforated appendicitis. Arch Surg. 2011;146:660-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 28. | Karp MP, Caldarola VA, Cooney DR, Allen JE, Jewett TC. The avoidable excesses in the management of perforated appendicitis in children. J Pediatr Surg. 1986;21:506-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Kogut KA, Blakely ML, Schropp KP, Deselle W, Hixson SD, Davidoff AM, Lobe TE. The association of elevated percent bands on admission with failure and complications of interval appendectomy. J Pediatr Surg. 2001;36:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Samuel M, Hosie G, Holmes K. Prospective evaluation of nonsurgical versus surgical management of appendiceal mass. J Pediatr Surg. 2002;37:882-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Weber TR, Keller MA, Bower RJ, Spinner G, Vierling K. Is delayed operative treatment worth the trouble with perforated appendicitis is children? Am J Surg. 2003;186:685-688; discussion 688-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Henry MC, Gollin G, Islam S, Sylvester K, Walker A, Silverman BL, Moss RL. Matched analysis of nonoperative management vs immediate appendectomy for perforated appendicitis. J Pediatr Surg. 2007;42:19-23; discussion 23-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Whyte C, Levin T, Harris BH. Early decisions in perforated appendicitis in children: lessons from a study of nonoperative management. J Pediatr Surg. 2008;43:1459-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Tanaka Y, Uchida H, Kawashima H, Fujiogi M, Suzuki K, Takazawa S, Deie K, Amano H, Iwanaka T. More than one-third of successfully nonoperatively treated patients with complicated appendicitis experienced recurrent appendicitis: Is interval appendectomy necessary? J Pediatr Surg. 2016;51:1957-1961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Nazarey PP, Stylianos S, Velis E, Triana J, Diana-Zerpa J, Pasaron R, Stylianos V, Malvezzi L, Knight C, Burnweit C. Treatment of suspected acute perforated appendicitis with antibiotics and interval appendectomy. J Pediatr Surg. 2014;49:447-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Puri P, Boyd E, Guiney EJ, O'Donnell B. Appendix mass in the very young child. J Pediatr Surg. 1981;16:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Shipsey MR, O'Donnell B. Conservative management of appendix mass in children. Ann R Coll Surg Engl. 1985;67:23-24. [PubMed] |
| 38. | Wilson-Storey D, Scobie WG. Appendix masses. Pediatr Surg Int. 1989;4:168-170. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Gahukamble DB, Khamage AS, Gahukamble LD. Management of appendicular mass in children. Ann Trop Paediatr. 1993;13:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Weiner DJ, Katz A, Hirschi RB, Drongowski R, Coran AG. Interval appendectomy in perforated appendicitis. Pediatr Surg Int. 1995;10:82-85. [DOI] [Full Text] |
| 41. | Surana R, Puri P. Appendiceal mass in children. Pediatr Surg Int. 1995;10:79-81. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Ein SH, Shandling B. Is interval appendectomy necessary after rupture of an appendiceal mass? J Pediatr Surg. 1996;31:849-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 52] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Bufo AJ, Shah RS, Li MH, Cyr NA, Hollabaugh RS, Hixson SD, Schropp KP, Lasater OE, Joyner RE, Lobe TE. Interval appendectomy for perforated appendicitis in children. J Laparoendosc Adv Surg Tech A. 1998;8:209-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 44. | Karaca I, Altintoprak Z, Karkiner A, Temir G, Mir E. The management of appendiceal mass in children: is interval appendectomy necessary? Surg Today. 2001;31:675-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 45. | Ho CM, Chen Y, Lai HS, Lin WH, Hsu WM, Chen WJ. Comparison of critical conservative treatment versus emergency operation in children with ruptured appendicitis with tumor formation. J Formos Med Assoc. 2004;103:359-363. [PubMed] |
| 46. | Erdoğan D, Karaman I, Narci A, Karaman A, Cavuşoğlu YH, Aslan MK, Cakmak O. Comparison of two methods for the management of appendicular mass in children. Pediatr Surg Int. 2005;21:81-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | Vane DW, Fernandez N. Role of interval appendectomy in the management of complicated appendicitis in children. World J Surg. 2006;30:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Owen A, Moore O, Marven S, Roberts J. Interval laparoscopic appendectomy in children. J Laparoendosc Adv Surg Tech A. 2006;16:308-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 49. | Emil S, Duong S. Antibiotic therapy and interval appendectomy for perforated appendicitis in children: a selective approach. Am Surg. 2007;73:917-922. [PubMed] |
| 50. | Aprahamian CJ, Barnhart DC, Bledsoe SE, Vaid Y, Harmon CM. Failure in the nonoperative management of pediatric ruptured appendicitis: predictors and consequences. J Pediatr Surg. 2007;42:934-938; discussion 938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 69] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 51. | Puapong D, Lee SL, Haigh PI, Kaminski A, Liu IL, Applebaum H. Routine interval appendectomy in children is not indicated. J Pediatr Surg. 2007;42:1500-1503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 52. | Keckler SJ, Tsao K, Sharp SW, Ostlie DJ, Holcomb GW, St Peter SD. Resource utilization and outcomes from percutaneous drainage and interval appendectomy for perforated appendicitis with abscess. J Pediatr Surg. 2008;43:977-980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 53. | Fawley J, Gollin G. Expanded utilization of nonoperative management for complicated appendicitis in children. Langenbecks Arch Surg. 2013;398:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Zhang HL, Bai YZ, Zhou X, Wang WL. Nonoperative management of appendiceal phlegmon or abscess with an appendicolith in children. J Gastrointest Surg. 2013;17:766-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 55. | Calvert CE, Tracy S, Zhou J, Graham D, Lebowitz M, Dennett KV, Chen C. Treatment of perforated appendicitis in children: focus on phlegmon. Am Surg. 2014;80:314-316. [PubMed] |
| 56. | Furuya T, Inoue M, Sugito K, Goto S, Kawashima H, Kaneda H, Masuko T, Ohashi K, Ikeda T, Koshinaga T. Effectiveness of Interval Appendectomy After Conservative Treatment of Pediatric Ruptured Appendicitis with Abscess. Indian J Surg. 2015;77:1041-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Luo CC, Cheng KF, Huang CS, Lo HC, Wu SM, Huang HC, Chien WK, Chen RJ. Therapeutic effectiveness of percutaneous drainage and factors for performing an interval appendectomy in pediatric appendiceal abscess. BMC Surg. 2016;16:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 58. | Bonadio W, Rebillot K, Ukwuoma O, Saracino C, Iskhakov A. Management of Pediatric Perforated Appendicitis: Comparing Outcomes Using Early Appendectomy Versus Solely Medical Management. Pediatr Infect Dis J. 2017;36:937-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 59. | Bonadio W, Langer M, Cueva J, Haaland A. Impact of Percutaneous Drainage on Outcome of Intra-abdominal Infection Associated With Pediatric Perforated Appendicitis. Pediatr Infect Dis J. 2017;36:952-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 60. | Zhang H, Bai Y, Wang W. Nonoperative management of appendiceal phlegmon or abscess in children less than 3 years of age. World J Emerg Surg. 2018;13:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 61. | Saluja S, Sun T, Mao J, Steigman SA, Oh PS, Yeo HL, Sedrakyan A, Merianos DJ. Early versus late surgical management of complicated appendicitis in children: A statewide database analysis with one-year follow-up. J Pediatr Surg. 2018;53:1339-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 62. | Zhang Y, Stringel G, Bezahler I, Maddineni S. Nonoperative Management of Periappendiceal Abscess in Children: A Comparison of Antibiotics Alone Versus Antibiotics Plus Percutaneous Drainage. J Pediatr Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 63. | Zhang Y, Deng Q, Zhu H, Chen B, Qiu L, Guo C. Intermediate-term evaluation of interval appendectomy in the pediatric population. Eur J Trauma Emerg Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 64. | Gasior AC, Marty Knott E, Ostlie DJ, St Peter SD. To drain or not to drain: an analysis of abscess drains in the treatment of appendicitis with abscess. Pediatr Surg Int. 2013;29:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 65. | Lee SL, Islam S, Cassidy LD, Abdullah F, Arca MJ; 2010 American Pediatric Surgical Association Outcomes and Clinical Trials Committee. Antibiotics and appendicitis in the pediatric population: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J Pediatr Surg. 2010;45:2181-2185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 66. | Zani A, Hall NJ, Rahman A, Morini F, Pini Prato A, Friedmacher F, Koivusalo A, van Heurn E, Pierro A. European Paediatric Surgeons' Association Survey on the Management of Pediatric Appendicitis. Eur J Pediatr Surg. 2019;29:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 67. | Goldin AB, Sawin RS, Garrison MM, Zerr DM, Christakis DA. Aminoglycoside-based triple-antibiotic therapy versus monotherapy for children with ruptured appendicitis. Pediatrics. 2007;119:905-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 68. | Nadler EP, Reblock KK, Ford HR, Gaines BA. Monotherapy versus multi-drug therapy for the treatment of perforated appendicitis in children. Surg Infect (Larchmt). 2003;4:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 69. | St Peter SD, Tsao K, Spilde TL, Holcomb GW, Sharp SW, Murphy JP, Snyder CL, Sharp RJ, Andrews WS, Ostlie DJ. Single daily dosing ceftriaxone and metronidazole vs standard triple antibiotic regimen for perforated appendicitis in children: a prospective randomized trial. J Pediatr Surg. 2008;43:981-985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 70. | Fishman SJ, Pelosi L, Klavon SL, O'Rourke EJ. Perforated appendicitis: prospective outcome analysis for 150 children. J Pediatr Surg. 2000;35:923-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 71. | Kronman MP, Oron AP, Ross RK, Hersh AL, Newland JG, Goldin A, Rangel SJ, Weissman SJ, Zerr DM, Gerber JS. Extended- Versus Narrower-Spectrum Antibiotics for Appendicitis. Pediatrics. 2016;138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 72. | Parmentier B, Berrebi D, Peycelon M, Doit C, Ghoneimi AE, Bonnard A. Failure of First-Line Antibiotics in Nonoperative Management of Appendiceal Mass, toward a Second-Line Instead of Surgery? Eur J Pediatr Surg. 2016;26:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 73. | Wang C, Li Y, Ji Y. Intravenous versus intravenous/oral antibiotics for perforated appendicitis in pediatric patients: a systematic review and meta-analysis. BMC Pediatr. 2019;19:407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 74. | Svensson JF, Hall NJ, Eaton S, Pierro A, Wester T. A review of conservative treatment of acute appendicitis. Eur J Pediatr Surg. 2012;22:185-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 75. | Levin T, Whyte C, Borzykowski R, Han B, Blitman N, Harris B. Nonoperative management of perforated appendicitis in children: can CT predict outcome? Pediatr Radiol. 2007;37:251-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 76. | Towbin RB. Pediatric interventional procedures in the 1980s: A period of development, growth, and acceptance. Radiology. 1989;170:1081-1090. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 77. | McCann JW, Maroo S, Wales P, Amaral JG, Krishnamurthy G, Parra D, Temple M, John P, Connolly BL. Image-guided drainage of multiple intraabdominal abscesses in children with perforated appendicitis: an alternative to laparotomy. Pediatr Radiol. 2008;38:661-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 78. | Gervais DA, Brown SD, Connolly SA, Brec SL, Harisinghani MG, Mueller PR. Percutaneous imaging-guided abdominal and pelvic abscess drainage in children. Radiographics. 2004;24:737-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 63] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 79. | Hogan MJ. Appendiceal abscess drainage. Tech Vasc Interv Radiol. 2003;6:205-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 80. | Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 267] [Article Influence: 14.8] [Reference Citation Analysis (1)] |
| 81. | Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245:886-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 307] [Article Influence: 17.1] [Reference Citation Analysis (1)] |
| 82. | Shawyer AC, Amaral JG, Langer JC. The role of tissue plasminogen activator in the management of complex intra-abdominal abscesses in children. J Pediatr Surg. 2012;47:1380-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 83. | St Peter SD, Shah SR, Adibe OO, Sharp SW, Reading B, Cully B, Holcomb GW, Rivard DC. Saline vs Tissue Plasminogen Activator Irrigations after Drain Placement for Appendicitis-Associated Abscess: A Prospective Randomized Trial. J Am Coll Surg. 2015;221:390-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |