Published online Mar 27, 2020. doi: 10.4240/wjgs.v12.i3.104
Peer-review started: October 19, 2019
First decision: November 19, 2019
Revised: December 2, 2019
Accepted: December 23, 2019
Article in press: December 23, 2019
Published online: March 27, 2020
Processing time: 131 Days and 19.9 Hours
Acute esophageal necrosis (AEN) is a rare entity with multifactorial etiology, usually presenting with signs of upper gastrointestinal bleeding.
To systematically review all available data on demographics, clinical features, outcomes and management of this medical condition.
A systematic literature search was performed with respect to the PRISMA statement (end-of-search date: October 24, 2018). Data on the study design, interventions, participants and outcomes were extracted by two independent reviewers.
Seventy-nine studies were included in this review. Overall, 114 patients with AEN were identified, of whom 83 were males and 31 females. Mean patient age was 62.1 ± 16.1. The most common presenting symptoms were melena, hematemesis or other manifestations of gastric bleeding (85%). The lower esophagus was most commonly involved (92.9%). The most widely implemented treatment modality was conservative treatment (75.4%), while surgical or endoscopic intervention was required in 24.6% of the cases. Mean overall follow-up was 66.2 ± 101.8 d. Overall 29.9% of patients died either during the initial hospital stay or during the follow-up period. Gastrointestinal symptoms on presentation [Odds ratio 3.50 (1.09-11.30), P = 0.03] and need for surgical or endoscopic treatment [surgical: Odds ratio 1.25 (1.03-1.51), P = 0.02; endoscopic: Odds ratio 1.4 (1.17-1.66), P < 0.01] were associated with increased odds of complications. A sub-analysis separating early versus late cases (after 2006) revealed a significantly increased frequency of surgical or endoscopic intervention (9.7 % vs 30.1% respectively, P = 0.04)
AEN is a rare condition with controversial pathogenesis and unclear optimal management. Although the frequency of surgical and endoscopic intervention has increased in recent years, outcomes have remained the same. Therefore, further research work is needed to better understand how to best treat this potentially lethal disease.
Core tip: This manuscript’s aim was to systematically review and synthesize all available data on demographics, clinical features, outcomes and the management of acute esophageal necrosis. According to our results, acute esophageal necrosis is a rare condition with controversial pathogenesis and unclear optimal management. Although the frequency of surgical and endoscopic intervention has increased in recent years, outcomes have remained the same. Therefore, further investigations are needed to better understand how to best treat this potentially lethal disease.
- Citation: Schizas D, Theochari NA, Mylonas KS, Kanavidis P, Spartalis E, Triantafyllou S, Economopoulos KP, Theodorou D, Liakakos T. Acute esophageal necrosis: A systematic review and pooled analysis. World J Gastrointest Surg 2020; 12(3): 104-115
- URL: https://www.wjgnet.com/1948-9366/full/v12/i3/104.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i3.104
Acute esophageal necrosis (AEN), also known as acute necrotizing esophagitis (ANE) or black esophagus is a rare and potentially devastating medical condition. Diagnosis is typically made with upper endoscopy. The most common endoscopic finding is a striking diffuse circumferential black discoloration of the esophageal mucosa which is associated with histologic evidence of extensive mucosal necrosis. The pathogenesis of AEN appears to be multifactorial. That said, ischemia has been reported as the most common etiology[1,2]. Gastric outlet obstruction with massive reflux of gastric secretions, viral infection, hypersensitivity to antibiotics, hypothermia, and corrosive trauma can also lead to AEN[1,3]. Typically, patients present at the emergency room with signs of upper gastrointestinal (GI) hemorrhage such as coffee-ground emesis, melena or hematemesis[4]. Conservative management with adequate hydration, proton pump inhibitors, antibiotics, acid suppression or sucralfate suspension administration is employed either as definitive or first-line treatment depending on disease severity[4]. Emergency surgical intervention followed by patient support until clinical stabilization can also be considered in case of necrosis and perforation[5].
Given the rarity of AEN, our experience with this condition is primarily based on case reports and small case series. To better understand the demographics, clinical features, and outcomes of this uncommon esophageal disease, we performed a systematic review of literature published within the period 1990 to 2018. Our study includes 160 cases of AEN and constitutes the largest to date review of “black esophagus”[6]. Overall, the present work may serve as a useful guide to clinicians contemplating how to best treat this rare condition.
We performed a PubMed/Medline search for English-language case reports and case series, using the keywords "acute esophageal necrosis" OR "black esophagus" OR "acute necrotizing esophagitis". Articles were screened by 2 independent reviewers (Theochari NA, Schizas D) and conflicts were resolved by a third reviewer (Kanavidis P). The reference lists of systematically reviewed articles were hand-searched for potentially eligible, missed studies. Data extraction of the articles included in our review was performed by Theochari NA and Schizas D.
Eligible articles were identified on the basis of the following inclusion criteria: (1) Papers published in English; (2) Primary research papers; (3) Papers that included patients older than 18 years old; and (4) Papers that included patients who were treated for AEN. Exclusion criteria were the following: (1) Papers that are not published in English; (2) Reviews, letters to the editor; and (3) Papers with inadequate data.
Variables were summarized as mean and standard deviation when continuous, or frequencies and percentages when categorical. Continuous variables were analyzed with independent samples student’s t-test, for normally distributed variables, or Mann-Whitney U-test otherwise (Kolmogorov-Smirnov test of normality was used). For categorical variables Pearson’s Chi-Square test was used, with Yates’ continuity correction when appropriate, whereas for ordinal variables we used Wilcoxon rank sum test. Univariate logistic regression was performed with logit transformation of data. Exploratorily, the outcome “death” was dichotomized and logistic regression was utilized since performing valid time-to-event analyses was not deemed feasible due to missing data and inadequate follow-up data. The level of statistical significance was set at 5%. Statistical analysis was performed with R-project environment for statistical computing (https://www.r-project.org/).
This study is registered with the PROSPERO registry and its unique identifying number is: CRD42018112571.
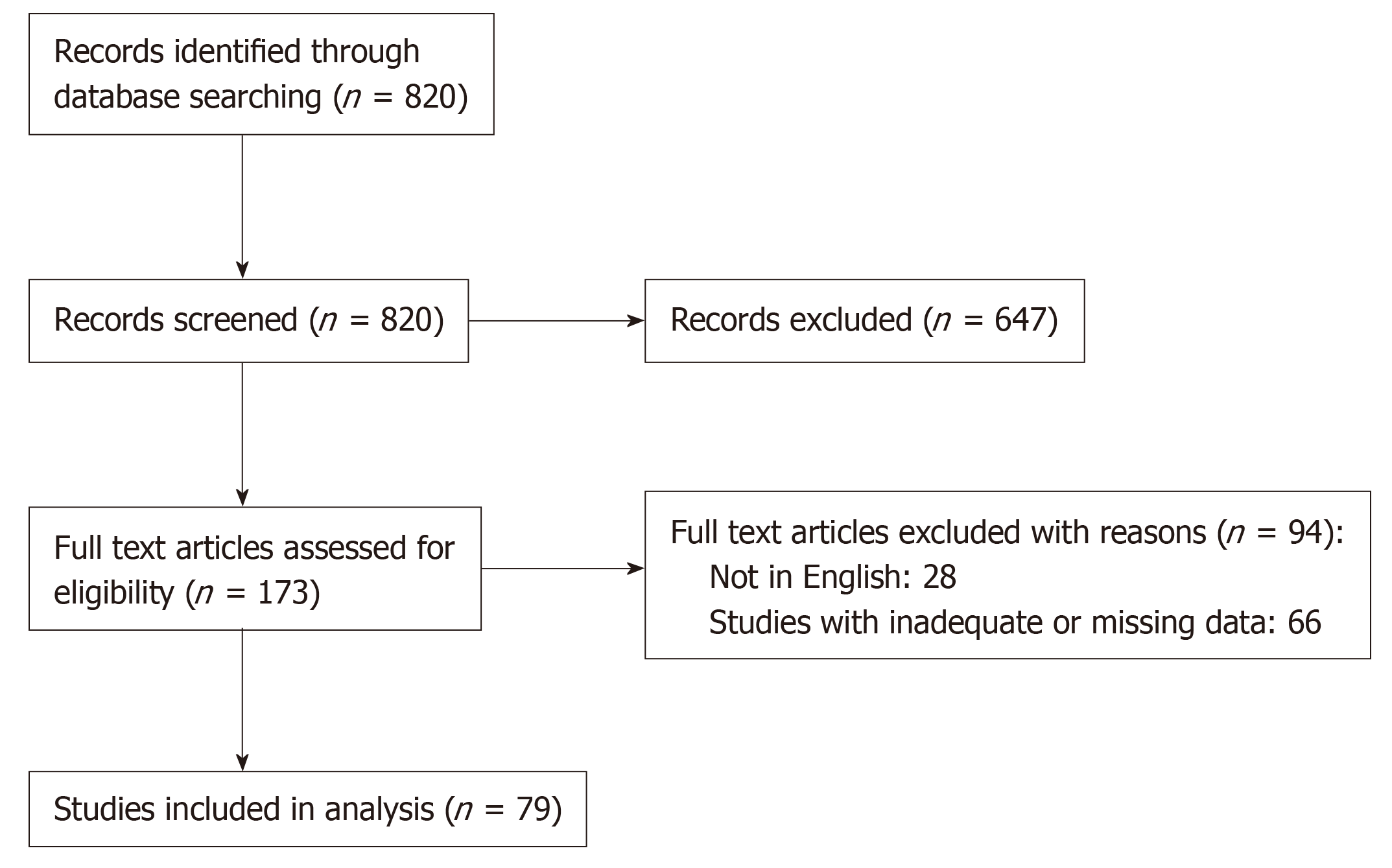
The search produced 820 PubMed results (October 24, 2018). The publications matching our selection criteria were 81. Ultimately, 79 studies satisfied our inclusion criteria and were selected for data collection (Figure 1). Of those, 69 were case reports[3,5,7-64] and 10 were cases series[2,65-73] including 69 and 45 patients respectively. A total of 114 of 160 patients were selected for the pooled analysis, as some case series did not publish individual patient data.
There were 114 patients who were diagnosed with AEN included in our study, of which 83 male and 31 female (M:F ratio of 2.7:1). Mean age was 62.1 ± 16.1. The most common presenting symptom was melena, hematemesis or other manifestation of gastric bleeding (85%), followed by epigastric or chest pain (29.2%) and other peptic symptoms (25.7%), including nausea, vomiting and dysphagia. Other symptoms such as fever, weakness, dyspnea, hypotension were less common (23.9%).
Patients had a diverse medical history, including diabetes mellitus or diabetic ketoacidosis, cardiopulmonary disease (chronic obstructive pulmonary disease, hypertension, heart failure, atrial fibrillation, myocardial infarct, angina), alcohol abuse, chronic kidney disease or other kidney-related disease (i.e., nephrectomy), liver-related disease (cirrhosis, liver transplantation) and others (stroke, gastroesophageal reflux disease, GI ulcers, chronic pancreatitis, prostate hypertrophy). Relative frequencies are displayed in Table 1, grouped by affected system.
| Clinicopathological features | |||
| Gender | Σ = 114 | ||
| Male | 83 | 72.8% | |
| Female | 31 | 27.2% | |
| Age (yr) | 62.1 ± 16.1 | 114 | |
| Admission symptoms | Σ = 113 | ||
| Bleeding | 96 | 85.0% | |
| Peptic | 29 | 25.7% | |
| Pain | 33 | 29.2% | |
| Other symptom | 27 | 23.9% | |
| Medical history | Σ = 110 | ||
| Cardiopulmonary | 52 | 47.3% | |
| Diabetes | 40 | 36.4% | |
| Alcohol | 31 | 28.2% | |
| Kidney | 17 | 15.5% | |
| Liver | 19 | 17.3% | |
| Other | 61 | 55.5% | |
| Clinical findings | Σ = 38 | ||
| Shock | 11 | 28,9% | |
| Malnutrition | 1 | 2.6% | |
| AKI | 3 | 7.9% | |
| Other | 24 | 63.2% | |
| Involvement of esophagus (relative to GEJ) | Σ = 98 | ||
| Upper | 33 | 33.7% | |
| Middle | 63 | 64.3% | |
| Lower | 91 | 92.9% | |
Clinical findings on admission were not always reported, but the most severe among them were signs of hypovolemic or septic shock/multiple organ dysfunction/sepsis (73%), acute kidney injury (20%) and malnutrition (7%). Lower esophageal involvement was almost always present (92.9%), with extension to the middle esophagus in many cases (64.3%). Upper esophagus was involved in only 33.7% of the cases.
Surgical or endoscopic intervention was required in 24.6% of the cases, whereas 75.4% were treated conservatively. Data available for the cases where intervention was required reveals that endoscopic treatment was preferred in 15 cases (14%), 2 of which later required surgical re-intervention, while surgical-first approach was used in 11 cases (10%). Most survivors received a follow-up endoscopy (89%), with a complication rate of 18.7%. A total of 32 patients died (29.9%), either during the initial hospital stay or during the follow-up period. Follow-up data was available for 78.9% of the patients. Mean overall follow-up was 66.2 ± 101.8 d, (or 82.9 ± 113.2 d among survivors) (Tables 2 and 3).
| Treatment modalities | |||
| Intervention | Σ = 114 | ||
| Yes | 28 | 24.6% | |
| No | 86 | 75.4% | |
| Management | Σ = 105 | ||
| Conservative | 79 | 75.2% | |
| Surgical | 11 | 10.5% | |
| Endoscopic | 13 | 12.4% | |
| Endoscopic + surgical | 2 | 1.9% | |
| Follow-up endoscopy | Yes | 67 | 58.8% |
| Complications | Yes | 14 | 12.3% |
| Death | Yes | 32 | 29.9% |
| FUP (overall; mean; SD) | 66.2 ± 101.8 | 90 | 90/114 |
| FUP (dead; mean; SD) | 16.6 ± 21.8 | 23 | 23/32 |
| FUP (alive; mean; SD) | 82.9 ± 113.2 | 65 | 65/75 |
| Endoscopic intervention | |
| Modalities | n (%) |
| Stenting | 1 (7.5) |
| Savary dilatations | 1 (7.5) |
| Balloοn dilatations | 11 (85) |
| Total | 13 |
On univariate logistic regression, GI symptoms on presentation [Odds ratio (OR) 3.50 (1.09-11.30), P = 0.03] and need for surgical or endoscopic treatment [surgical: OR 1.25 (1.03-1.51), P = 0.02; endoscopic: OR 1.4 (1.17-1.66), P < 0.01] were associated with increased odds of complications (Table 4). Patients that underwent both endoscopic and surgical intervention had even higher complication rate; OR 2.58 (1.7-3.93), P < 0.01. Exploratory logistic regression for the dichotomized “death” endpoint (Table 5) did not reveal any statistically significant prognostic factors.
| OR | LCI | HCI | P value | ||
| Gender | Male | 0.95 | 0.83 | 1.09 | 0.45 |
| Female | (ref) | ||||
| Age | +1 yr | 0.990 | 0.957 | 1.025 | 0.553 |
| Admission symptoms | Bleeding | 0.60 | 0.16 | 2.91 | 0.48 |
| Peptic | 3.50 | 1.09 | 11.30 | 0.03 | |
| Pain | 2.00 | 0.61 | 6.29 | 0.24 | |
| Other symptom | 0.86 | 0.18 | 3.04 | 0.83 | |
| None | (ref) | ||||
| Medical history | Cardiac | 0.63 | 0.18 | 1.95 | 0.43 |
| Diabetes mellitus | 1.46 | 0.45 | 4.53 | 0.52 | |
| Alcohol abuse | 1.08 | 0.28 | 3.54 | 0.90 | |
| Kidney diseases | 0.94 | 0.14 | 3.94 | 0.94 | |
| Liver diseases | 3.41 | 0.94 | 11.49 | 0.05 | |
| Other | 0.85 | 0.27 | 2.66 | 0.78 | |
| Clinical findings | Malnutrition | 0.87 | 0.44 | 1.74 | 0.70 |
| AKI | 0.87 | 0.58 | 1.30 | 0.50 | |
| Other | 1.15 | 0.77 | 1.73 | 0.50 | |
| Involvement of esophagus (to GEJ) | Upper | 2.67 | 0.74 | 9.99 | 0.13 |
| Middle | 0.97 | 0.27 | 3.94 | 0.96 | |
| Lower | 1.13 | 0.88 | 1.44 | 0.33 | |
| Intervention | Yes | 11.39 | 3.41 | 45.44 | < 0.01 |
| No | (ref) | ||||
| Management | Conservative | (ref) | |||
| Surgical | 1.25 | 1.03 | 1.51 | 0.02 | |
| Endoscopic | 1.4 | 1.17 | 1.66 | < 0.01 | |
| Endoscopic + surgical | 2.58 | 1.7 | 3.93 | < 0.01 | |
| OR | LCI | HCI | P value | ||
| Gender | Male | 0.99 | 0.40 | 2.58 | 0.99 |
| Female | (ref) | ||||
| Age | +1 yr | 1.02 | 0.99 | 1.05 | 0.30 |
| Admission symptoms | Bleeding | 1.33 | 0.42 | 5.09 | 0.64 |
| Peptic | 0.72 | 0.26 | 1.85 | 0.51 | |
| Pain | 0.31 | 0.10 | 0.84 | 0.03 | |
| Other symptom | 0.83 | 0.29 | 2.15 | 0.70 | |
| None | (ref) | ||||
| Medical history | Cardiac | 1.06 | 0.46 | 2.44 | 0.88 |
| Diabetes mellitus | 0.81 | 0.32 | 1.92 | 0.64 | |
| Alcohol abuse | 0.80 | 0.30 | 2.01 | 0.65 | |
| Kidney diseases | 2.34 | 0.75 | 7.21 | 0.13 | |
| Liver diseases | 1.47 | 0.50 | 4.10 | 0.47 | |
| Other | 0.55 | 0.23 | 1.26 | 0.16 | |
| Clinical findings | malnutrition | 0.75 | 0.30 | 1.87 | 0.54 |
| AKI | 1.05 | 0.61 | 1.83 | 0.85 | |
| Other | 0.95 | 0.55 | 1.65 | 0.85 | |
| Involvement of esophagus (to GEJ) | Upper | 0.57 | 0.20 | 1.49 | 0.27 |
| Middle | 0.59 | 0.24 | 1.49 | 0.26 | |
| Lower | 1.37 | 0.91 | 2.08 | 0.13 | |
| Intervention | Yes | 0.63 | 0.21 | 1.69 | 0.38 |
| No | (ref) | ||||
| Management | Conservative | (ref) | |||
| Surgical | 0.96 | 0.71 | 1.30 | 0.79 | |
| Endoscopic | 0.77 | 0.59 | 1.00 | 0.06 | |
| Endoscopic + surgical | 0.71 | 0.29 | 1.75 | 0.46 | |
A sub-analysis separating early versus late cases (after 2006) revealed a significantly increased frequency of surgical or endoscopic intervention of 30.1% for the late cases, compared to 9.7% for the early cases (P = 0.04). Mortality rate, however, was similar, for the late (30.3%) and the early cases (29%) (P = 1.00).
ANE was first described by Goldenberg et al[1] in 1990 . The largest case series of AEN published to date included 29 and 16 cases respectively[74,75]. In 2007, Gurvits et al[6] attempted for the first time to present a review of the literature and described 88 patients with black esophagus. Since then, no systematic or broad review of the published literature has been performed. To guide clinicians treating patients with AEN using up-to-date information we systematically reviewed relevant literature from 1990 until 2018. Our analysis includes 114 patients and provides a comprehensive overview of the demographics, clinical features, treatment options, and outcomes of patients with AEN.
Several theories have been proposed to explain the pathogenesis of AEN. The most popular is ischemia due to low flow rates or shock. Reichart et al[3] reported that ischemic AEN is typically secondary to cardiac dysfunction, prolonged hypotension or sepsis. Our findings support this statement with 47.3% of the patients described in this review having a cardiopulmonary medical history. Another factor that argues in favor of an ischemic etiology in the present study is the predominance of esophageal necrosis in the middle and lower thirds of esophagus (64.3% and 92.9% respectively) which are usually less vascularized and thus more prone to ischemic injury. Other causes of AEN include gastric outlet obstruction with massive reflux of gastric secretions, viral infection, hypersensitivity to antibiotics, hypothermia and corrosive trauma[3].
According to our analysis, AEN affects predominately men (72%) at a mean age of 62 years. Nevertheless, AEN can develop at virtually any age. In our review AEN, was seen in 6 patients in the third decade of life and in male patient at the age of 10 year[17]. The majority (85%) of patients presented at the ER with symptoms of upper GI bleeding i.e., melena, hematemesis or other manifestations of gastric bleeding. Associated clinical findings were not always reported, but the most commonly reported ones were hypovolemic or septic shock[74]. Patients’ medical history may also be a serious risk factor for ANE[76]. Most patients included in this systematic review had history of a significant cardiopulmonary disease (47.3%) while others suffered from diabetes mellitus (36.4%), alcohol abuse (28.2%), as well as liver (17.3%) and kidney related disease (15.5%).
The diagnosis of AEN is made endoscopically by identifying diffuse circumferential progressive black discoloration of the esophagus with abrupt demarcation at the Z-line. In six cases reported in this review, the mucosa of the esophagus was also covered by yellow or white exudates at the time of initial scoping[8,73]. Histologically, AEN specimens shows necrotic debris, mucosal and submucosal necrosis with a local inflammatory response[8,73].
Given the rarity of the condition, there are no clear guidelines regarding how to best manage patients with AEN. Most authors recommend a conservative treatment approach which includes correction of underlying disorders, total parenteral nutrition, adequate intravenous hydration, broad spectrum antibiotics, proton pump inhibitors and sucralfate suspension[4]. Blood cell transfusion is also recommended when necessary. In case of necrosis or perforation, early surgical or endoscopic intervention is required[5]. In this systematic review, surgery was performed as first line treatment in 11 cases whereas endoscopic treatment was used in 15 patients, 2 of which later required surgical re -intervention. Surprisingly, a sub- analysis that we conducted, separating cases before and after 2006 (i.e., when the last systematic review was published) showed that the frequency of surgical or endoscopic intervention was significantly increased from 9.7% (before 2006) to 30.1% (after 2006) (P = 0.04). That said, the increased rate of operative intervention did not seem to affect overall patient outcomes.
The most commonly reported complication is stricture while others can be stenosis, abscesses, tracheoesophageal fistula and perforation of the esophagus[1]. In this systematic review only 14 (12.3% of the patients) developed complications. Of them, 10 (70%) developed an esophageal stricture and four (30%) a tracheoesophageal fistula. Interestingly, univariate logistic regression revealed an association between the presence of GI symptoms on admission [OR 3.50 (1.09-11.30), P = 0.03] with increased odds of post-AEN complications. Patients that required surgical or endoscopic treatment [surgical: OR 1.25 (1.03-1.51), P = 0.02; endoscopic: OR 1.4 (1.17-1.66), P < 0.01] were also more likely to develop complications. This is not surprising since patients with more severe disease at presentation are more likely to receive surgical intervention. Moreover, patients that underwent both endoscopic and surgical intervention had an even higher complication rate [OR 2.58 (1.7-3.93), P < 0.01].
A total of 32 patients included in our study died (29.9%), either during the initial hospital stay or subsequently at follow-up. The high mortality rate that is seen in AEN may be potentially related to patient characteristics such as serious medical history, older age and higher incidence of malignancy[1].
Methodological strengths of the present paper include: (1) Comprehensive literature search using rigorous and systematic methodology; and (2) Detailed data extraction. We also performed a sub-analysis separating early versus late cases[6] (after 2006 when the last systematic review was published) which showed that the implementation of surgical/endoscopic interventions have increased threefold.
This analysis has certain limitations. As with any systematic review, certain studies did not report on all outcomes of interest and therefore all cumulative results were estimated based on available data. Only papers published in English were eligible and all included studies were retrospective case reports or small case series. Lastly, due to missing data, performing strong survival modeling was not possible and therefore we treated “death” as a binary outcome and performed logistic regression to provide an approximation of mortality predictors.
In conclusions, AEN is a rare condition with high mortality. Although, the etiology of this disease is likely multi-factorial, ischemia seems to play a pivotal role in pathogenesis. The diagnosis of AEN is mainly based on upper GI endoscopy revealing a black-appearing esophageal mucosa circumferentially. Although the rate of operative interventions has increased in recent years, conservative treatment still seems to be the most commonly used treatment approach. Black esophagus is anticipated to become a more commonly recognized and described entity. To that end, a staging system that classifies the patients with AEN according to their symptoms on admission, their medical history and the endoscopic findings would be meaningful. Overall, further investigations are needed to better understand the risk factors, pathogenesis, diagnostic challenges and optimum treatment approach for this rare but potentially lethal condition.
Acute esophageal necrosis (AEN) is a severe medical condition with multifactorial etiology. Our experience is mainly based on case reports and small case series.
Given the rarity of this entity, further investigations are needed to better understand the risk factors, pathogenesis, diagnostic challenges and how to best treat this potentially lethal disease.
Our objective was to investigate all available data on demographics, clinical features, outcomes of this condition and to suggest the best management.
We performed a systematic literature search with respect to the PRISMA statement. Univariate logistic regression was performed with logit transformation of data.
Overall, 114 patients with AEN were included in this study. The most common symptoms on admission were melena, hematemesis or other manifestations of gastric bleeding. With regards to treatment modalities, conservative treatment was the most widely implemented choice followed by surgical or/and endoscopic intervention. A sub-analysis separating early versus late cases (after 2006) revealed a significantly increased frequency of surgical or endoscopic intervention. Nevertheless, further research work is needed to better understand how to best treat this potentially deadly disease.
To the best of our knowledge, this is the most up to date and comprehensive systematic review regarding AEN. This rare entity seems to have multi-factorial etiology, but ischemia seems to play the most significant role in pathogenesis. Diagnosis is made by upper gastrointestinal endoscopy, while conservative treatment seems to be still the most popular modality. Nevertheless, our study revealed that operative interventions have increased the last years. Black esophagus is a medical condition that is still difficult recognized. To that end, a staging system that classifies the patients with AEN according to their symptoms on admission, their medical history and the endoscopic findings would be meaningful.
Further investigations are needed to better understand the risk factors, pathogenesis, diagnostic challenges and optimum treatment approach for this rare but potentially lethal condition.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C, C, C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aktekin A, Cremers I, Dogan U, Isik A, Mercado MA, Okamoto H, Yeh HZ S-Editor: Yan JP L-Editor: A E-Editor: Ma YJ
| 1. | Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology. 1990;98:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 134] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Gurvits GE, Cherian K, Shami MN, Korabathina R, El-Nader EM, Rayapudi K, Gandolfo FJ, Alshumrany M, Patel H, Chowdhury DN, Tsiakos A. Black esophagus: new insights and multicenter international experience in 2014. Dig Dis Sci. 2015;60:444-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 99] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 3. | Reichart M, Busch OR, Bruno MJ, Van Lanschot JJ. Black esophagus: a view in the dark. Dis Esophagus. 2000;13:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol. 2010;16:3219-3225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 160] [Cited by in RCA: 199] [Article Influence: 13.3] [Reference Citation Analysis (2)] |
| 5. | Hwang J, Weigel TL. Acute esophageal necrosis: "black esophagus". JSLS. 2007;11:165-167. [PubMed] |
| 6. | Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 162] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Trappe R, Pohl H, Forberger A, Schindler R, Reinke P. Acute esophageal necrosis (black esophagus) in the renal transplant recipient: manifestation of primary cytomegalovirus infection. Transpl Infect Dis. 2007;9:42-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Nagri S, Hwang R, Anand S, Kurz J. Herpes simplex esophagitis presenting as acute necrotizing esophagitis ("black esophagus") in an immunocompetent patient. Endoscopy. 2007;39 Suppl 1:E169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Kim YH, Choi SY. Black esophagus with concomitant candidiasis developed after diabetic ketoacidosis. World J Gastroenterol. 2007;13:5662-5663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Tanaka K, Toyoda H, Hamada Y, Aoki M, Kosaka R, Noda T, Katsurahara M, Nakamura M, Ninomiya K, Inoue H, Imoto I, Takei Y. A relapse case of acute necrotizing esophagitis. Endoscopy. 2007;39 Suppl 1:E305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Hong JW, Kim SU, Park HN, Seo JH, Lee YC, Kim H. Black esophagus associated with alcohol abuse. Gut Liver. 2008;2:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Maher MM, Nassar MI. Black esophagus: a case report. Cases J. 2008;1:367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Neumann DA 2nd, Francis DL, Baron TH. Proximal black esophagus: a case report and review of the literature. Gastrointest Endosc. 2009;70:180-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Katsuhara K, Takano S, Yamamoto Y, Ueda S, Nobuhara K, Kiyasu Y. Acute esophageal necrosis after lung cancer surgery. Gen Thorac Cardiovasc Surg. 2009;57:437-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Lee JK, Bhargava V, Mittal RK, Ghosh P. Achalasia, alcohol-stasis, and acute necrotizing esophagitis: connecting the dots. Dig Dis Sci. 2011;56:612-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Garas G, Wou C, Sawyer J, Amygdalos I, Gould S. Acute oesophageal necrosis syndrome. BMJ Case Rep. 2011;2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Gaissert HA, Breuer CK, Weissburg A, Mermel L. Surgical management of necrotizing Candida esophagitis. Ann Thorac Surg. 1999;67:231-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Calabrese C, Liguori G. Acute esophageal necrosis. Clin Gastroenterol Hepatol. 2011;9:A30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | van de Wal-Visscher E, Nieuwenhuijzen GA, van Sambeek MR, Haanschoten M, Botman KJ, de Hingh IH. Type B aortic dissection resulting in acute esophageal necrosis. Ann Vasc Surg. 2011;25:837.e1-837.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Albuquerque A, Ramalho R, Rios E, Lopes JM, Macedo G. Black esophagus. Dis Esophagus. 2013;26:333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Carrera VG, Rodriguez SV, Gonzalez de la Ballina Gonzalez E, Luis Ulla Rocha J. Acute esophageal necrosis in a patient with multiple comorbidity. Ann Gastroenterol. 2012;25:162. [PubMed] |
| 22. | Kabaçam G, Yakut M, Soykan I. Acute esophageal necrosis: a rare cause of gastrointestinal bleeding. Dig Endosc. 2012;24:283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Pereira O, Figueira-Coelho J, Picado B, Costa JN. Black oesophagus. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Maroy B. Black esophagus complicating variceal bleeding. Endoscopy. 2013;45 Suppl 2 UCTN:E237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Román Fernández A, López Álvarez A, Fossati Puertas S, Areán González I, Varela García O, Viaño López PM. Black esophagus (acute esophageal necrosis) after spinal anesthesia. Rev Esp Anestesiol Reanim. 2014;61:401-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Abed J, Mankal P, Judeh H, Kim S. Acute Esophageal Necrosis: A Case of Black Esophagus Associated with Bismuth Subsalicylate Ingestion. ACG Case Rep J. 2014;1:131-133. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Tse A, Basu S, Ali H, Hamouda A. Black necrotic oesophagus following the use of biodegradable stent for benign oesophageal stricture. J Surg Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Barjas E, Pires S, Lopes J, Valente A, Oliveira E, Palma R, Raimundo M, Alexandrino P, Moura MC. Cytomegalovirus acute necrotizing esophagitis. Endoscopy. 2001;33:735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Gómez V, Propst JA, Francis DL, Canabal JM, Franco PM. Black esophagus: an unexpected complication in an orthotopic liver transplant patient with hemorrhagic shock. Dig Dis Sci. 2014;59:2597-2599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Kimura Y, Seno H, Yamashita Y. A case of acute necrotizing esophagitis. Gastrointest Endosc. 2014;80:525-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Barnes T, Yan S, Kaakeh Y. Necrotizing Esophagitis and Bleeding Associated With Cefazolin. Ann Pharmacother. 2014;48:1214-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 32. | Zacharia GS, Sandesh K, Ramachandran T. Acute esophageal necrosis: an uncommon cause of hematemesis. Oman Med J. 2014;29:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Shimamura Y, Nakamura K, Ego M, Omata F. Advanced endoscopic imaging in black esophagus. Can J Gastroenterol Hepatol. 2014;28:471-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Caravaca-Fontán F, Jimenez S, Fernández-Rodríguez A, Marcén R, Quereda C. Black esophagus in the early kidney post-transplant period. Clin Kidney J. 2014;7:613-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | Talebi-Bakhshayesh M, Samiee-Rad F, Zohrenia H, Zargar A. Acute Esophageal Necrosis: A Case of Black Esophagus with DKA. Arch Iran Med. 2015;18:384-385. [PubMed] |
| 36. | Abu-Zaid A, Solimanie S, Abudan Z, Al-Hussaini H, Azzam A, Amin T. Acute esophageal necrosis (black esophagus) in a 40-year-old man. Ann Saudi Med. 2015;35:80-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Salem GA, Ahluwalia S, Guild RT. A case of acute oesophageal necrosis (AEN) in a hypothermic patient. The grave prognosis of the black oesophagus. Arab J Gastroenterol. 2015;16:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Iorio N, Bernstein GR, Malik Z, Schey R. Acute Esophageal Necrosis Presenting With Henoch-Schönlein Purpura. ACG Case Rep J. 2015;3:17-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Katsinelos P, Christodoulou K, Pilpilidis I, Papagiannis A, Xiarchos P, Tsolkas P, Vasiliadis I, Eugenidis N. Black esophagus: an unusual finding during routine endoscopy. Endoscopy. 2001;33:904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Galanopoulos M, Anastasiadis S, Archavlis E, Mantzaris GJ. Black esophagus: an uncommon cause of upper gastrointestinal bleeding. Intern Emerg Med. 2016;11:1019-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 41. | Rigolon R, Fossà I, Rodella L, Targher G. Black esophagus syndrome associated with diabetic ketoacidosis. World J Clin Cases. 2016;4:56-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 42. | Galtés I, Gallego MÁ, Esgueva R, Martin-Fumadó C. Acute oesophageal necrosis (black oesophagus). Rev Esp Enferm Dig. 2016;108:154-155. [PubMed] |
| 43. | Sharma V, De A, Ahuja A, Lamoria S, Lamba BM. Acute Esophageal Necrosis Caused by Candidiasis in a Patient with Systemic Lupus Erythematosus. J Emerg Med. 2016;51:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 44. | Pautola L, Hakala T. Medication-induced acute esophageal necrosis: a case report. J Med Case Rep. 2016;10:267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 45. | Rodrigues BD, Dos Santos R, da Luz MM, Chaves E Silva F, Reis IG. Acute esophageal necrosis. Clin J Gastroenterol. 2016;9:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Joubert KD, Betzold RD, Steliga MA. Successful Treatment of Esophageal Necrosis Secondary to Acute Type B Aortic Dissection. Ann Thorac Surg. 2016;102:e547-e549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 47. | Sakatoku Y, Fukaya M, Miyata K, Nagino M. Successful bypass operation for esophageal obstruction after acute esophageal necrosis: a case report. Surg Case Rep. 2017;3:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 48. | Alcaide N, Fernández Salazar L, Ruiz Rebollo L, González Obeso E. Acute esophageal necrosis resolved in 72 hours. Rev Esp Enferm Dig. 2017;109:217. [PubMed] |
| 49. | Bonaldi M, Sala C, Mariani P, Fratus G, Novellino L. Black esophagus: acute esophageal necrosis, clinical case and review of literature. J Surg Case Rep. 2017;2017:rjx037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 50. | Odelowo OO, Hassan M, Nidiry JJ, Marshalleck JJ. Acute necrotizing esophagitis: a case report. J Natl Med Assoc. 2002;94:735-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Manno V, Lentini N, Chirico A, Perticone M, Anastasio L. Acute esophageal necrosis (black esophagus): a case report and literature review. Acta Diabetol. 2017;54:1061-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 52. | Kim DB, Bowers S, Thomas M. Black and White Esophagus: Rare Presentations of Severe Esophageal Ischemia. Semin Thorac Cardiovasc Surg. 2017;29:256-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Matsuo T, Ishii N. Acute Esophageal Necrosis. N Engl J Med. 2017;377:1378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 54. | Khan AM, Hundal R, Ramaswamy V, Korsten M, Dhuper S. Acute esophageal necrosis and liver pathology, a rare combination. World J Gastroenterol. 2004;10:2457-2458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 55. | Rejchrt S, Douda T, Kopácová M, Siroký M, Repák R, Nozicka J, Spacek J, Bures J. Acute esophageal necrosis (black esophagus): endoscopic and histopathologic appearance. Endoscopy. 2004;36:1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 56. | Yamauchi J, Mitsufuji S, Taniguchi J, Sakai M, Tatsumi N, Yasuda Y, Konishi H, Wakabayashi N, Kataoka K, Okanoue T. Acute esophageal necrosis followed by upper endoscopy and esophageal manometry/pH test. Dig Dis Sci. 2005;50:1718-1721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 57. | Endo T, Sakamoto J, Sato K, Takimoto M, Shimaya K, Mikami T, Munakata A, Shimoyama T, Fukuda S. Acute esophageal necrosis caused by alcohol abuse. World J Gastroenterol. 2005;11:5568-5570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 58. | Del Hierro PM. Acute Necrotizing Esophagitis Followed by Duodenal Necrosis. Gastroenterology Res. 2011;4:286-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 59. | Geller A, Aguilar H, Burgart L, Gostout CJ. The black esophagus. Am J Gastroenterol. 1995;90:2210-2212. [PubMed] |
| 60. | Obermeyer R, Kasirajan K, Erzurum V, Chung D. Necrotizing esophagitis presenting as a black esophagus. Surg Endosc. 1998;12:1430-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 61. | Katsinelos P, Pilpilidis I, Dimiropoulos S, Paroutoglou G, Kamperis E, Tsolkas P, Kapelidis P, Limenopoulos B, Papagiannis A, Pitarokilis M, Trakateli C. Black esophagus induced by severe vomiting in a healthy young man. Surg Endosc. 2003;17:521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 62. | Carter RR, Coughenour JP, Van Way CW, Goldstrich J. Acute esophageal necrosis with pneumomediastinum: a case report. Mo Med. 2007;104:276-278. [PubMed] |
| 63. | Le K, Ahmed A. Acute necrotizing esophagitis: case report and review of the literature. J La State Med Soc. 2007;159:330, 333-338. [PubMed] |
| 64. | Usmani A, Samarany S, Nardino R, Shaib W. Black esophagus in a patient with diabetic ketoacidosis. Conn Med. 2011;75:467-468. [PubMed] |
| 65. | Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963-2003. Dis Esophagus. 2006;19:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 66. | Singh D, Singh R, Laya AS. Acute esophageal necrosis: a case series of five patients presenting with "Black esophagus". Indian J Gastroenterol. 2011;30:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 67. | Wu MH, Wu HY. Incremental change in acute esophageal necrosis: report of two cases. Surg Today. 2014;44:363-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 68. | Worrell SG, Oh DS, Greene CL, DeMeester SR, Hagen JA. Acute esophageal necrosis: a case series and long-term follow-up. Ann Thorac Surg. 2014;98:341-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 69. | Shafa S, Sharma N, Keshishian J, Dellon ES. The Black Esophagus: A Rare But Deadly Disease. ACG Case Rep J. 2016;3:88-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 70. | Koop A, Bartel MJ, Francis D. A Case of Acute Esophageal Necrosis and Duodenal Disease in a Patient With Adrenal Insufficiency. Clin Gastroenterol Hepatol. 2016;14:A17-A18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 71. | Kalva NR, Tokala MR, Dhillon S, Pisoh WN, Walayat S, Vanar V, Puli SR. An Unusual Cause of Acute Upper Gastrointestinal Bleeding: Acute Esophageal Necrosis. Case Rep Gastrointest Med. 2016;2016:6584363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 72. | Averbukh LD, Mavilia MG, Gurvits GE. Acute Esophageal Necrosis: A Case Series. Cureus. 2018;10:e2391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 73. | Ben Soussan E, Savoye G, Hochain P, Hervé S, Antonietti M, Lemoine F, Ducrotté P. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc. 2002;56:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 93] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 74. | Augusto F, Fernandes V, Cremers MI, Oliveira AP, Lobato C, Alves AL, Pinho C, de Freitas J. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy. 2004;36:411-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 75. | Yasuda H, Yamada M, Endo Y, Inoue K, Yoshiba M. Acute necrotizing esophagitis: role of nonsteroidal anti-inflammatory drugs. J Gastroenterol. 2006;41:193-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 76. | Moretó M, Ojembarrena E, Zaballa M, Tánago JG, Ibánez S. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy. 1993;25:534-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 2.2] [Reference Citation Analysis (0)] |