Published online Sep 27, 2019. doi: 10.4240/wjgs.v11.i9.373
Peer-review started: May 20, 2019
First decision: August 2, 2019
Revised: August 24, 2019
Accepted: September 10, 2019
Article in press: September 10, 2019
Published online: September 27, 2019
Processing time: 131 Days and 20.1 Hours
Tuberculosis (TB) has a rare extrapulmonary manifestation known as esophageal tuberculosis, accounting for 0.2% of total TB patients. Esophageal TB typically presents with dysphagia, with retrosternal pain or odynophagia, but generalized symptoms such as low-grade fever, decreased appetite, and weight loss are also observed. Esophageal carcinoma and Crohn’s disease of the esophagus are important differential diagnoses with similar presentation.
We present a case of a 25-year-old male, who presented with esophageal TB mimicking an esophageal carcinoma. Lab work-up, Mantoux test, and chest X-ray were normal. Barium-swallow examination showed moderate dilatation of distal esophagus with a nodular and irregular mucosa. Computed tomography showed significant thickening of thoracic and distal esophagus with infiltration into the lesser omentum and large, centrally necrotic lymph nodes on gastro-hepatic ligament suggestive of a possible malignancy. Esophagoscopy was performed and a biopsy of mural thickening was performed and sent for histopathological examination. The histopathology report and TB-polymerase chain reaction confirmed the diagnosis of esophageal TB. The patient was started on anti-tuberculous therapy (ATT), and complete resolution of symptoms and disease was achieved in 6 mo.
Esophageal TB is an extremely rare, yet important differential diagnosis in a patient presenting with dysphagia. Esophageal TB can mimic esophageal carcinoma on computed tomography scan. The patient responded well to a complete course of ATT.
Core tip: Tuberculosis (TB) has a rare extrapulmonary manifestation known as esophageal tuberculosis, which accounts for 0.2% of total TB patients. Esophageal TB typically presents with dysphagia and retrosternal pain. We present a case of a 25-year-old male, who presented with esophageal TB mimicking an esophageal carcinoma. The lab work-up and chest X-ray were unremarkable. Esophagoscopy was performed and a biopsy of mural thickening was taken. The histopathology report and TB-polymerase chain reaction test confirmed the diagnosis of esophageal TB. The patient was started on anti-tuberculous therapy, and complete resolution of symptoms and disease was achieved in 6 mo.
- Citation: Khan MS, Maan MHA, Sohail AH, Memon WA. Primary esophageal tuberculosis mimicking esophageal carcinoma on computed tomography: A case report. World J Gastrointest Surg 2019; 11(9): 373-380
- URL: https://www.wjgnet.com/1948-9366/full/v11/i9/373.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i9.373
Tuberculosis (TB) is an infectious disease with various presentations, including a rare extrapulmonary manifestation known as esophageal TB, which accounts for less than 0.2% of all TB patients[1]. Primary esophageal TB is extremely rare with only a few cases reported in literature. Dysphagia or retrosternal pain is one of the most common symptoms reported for esophageal TB, but abdominal discomfort, odynophagia, hematemesis and weight loss can also be present[2]. The main differential diagnoses are esophageal cancer and Crohn’s disease of the esophagus, both having completely different management options than esophageal TB[3]. Thus, it is imperative to keep esophageal TB as an important differential diagnosis, particularly in cases of dysphagia[4]. We present a case of a 25-year-old male with esophageal TB mimicking esophageal carcinoma.
A 25-year-old male presented with complaints of progressive dysphagia for both liquids and solids for 1 mo associated with epigastric pain.
The patient described the pain as intermittent, dull, non-radiating, and a 5 in severity on a scale of 1-10, with no exacerbating or relieving factors. The patient reported 10 kg weight loss in the last 8 mo. On review of systems, the patient denied chest pain, dyspnea, productive cough, nausea, vomiting, hematemesis, melena, hematochezia, altered bowel habits, fever, night sweats or anorexia.
The patient’s past medical and surgical history was unremarkable, with no prior hospital admissions. He had no known co-morbid conditions.
The patient’s personal history was unremarkable with no addictions reported. There was no history of long-standing diseases including cancer in his family.
The patient’s physical examination including vital signs was within normal limits.
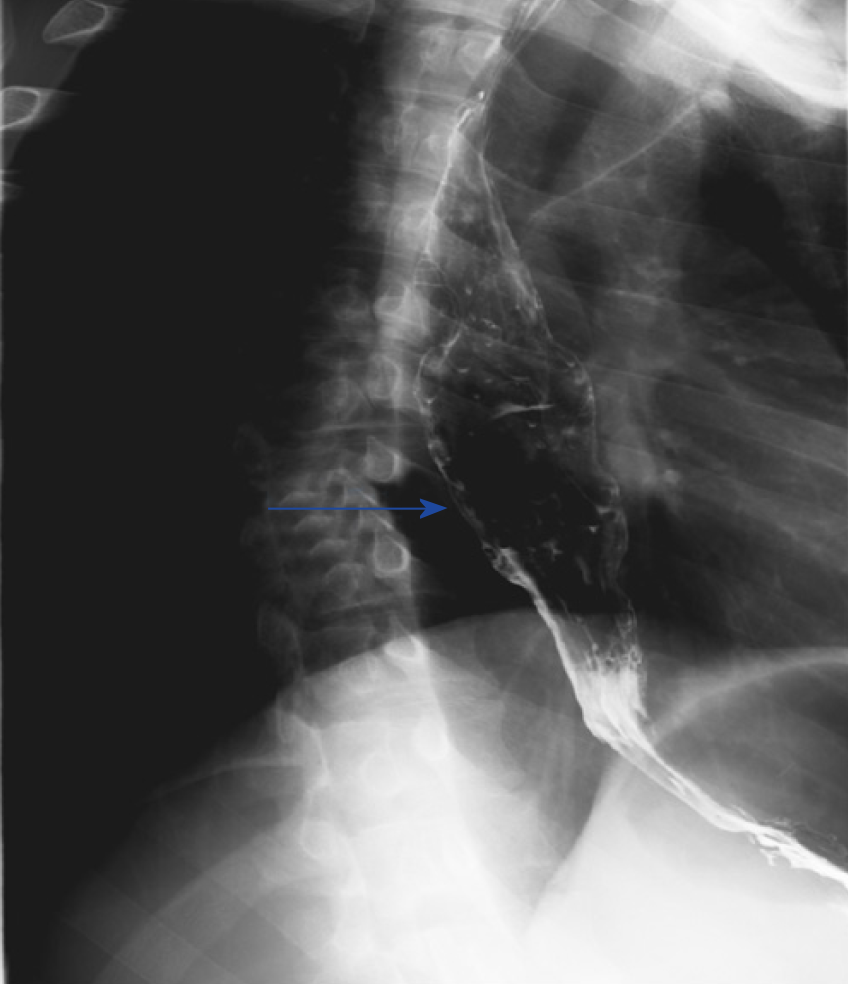
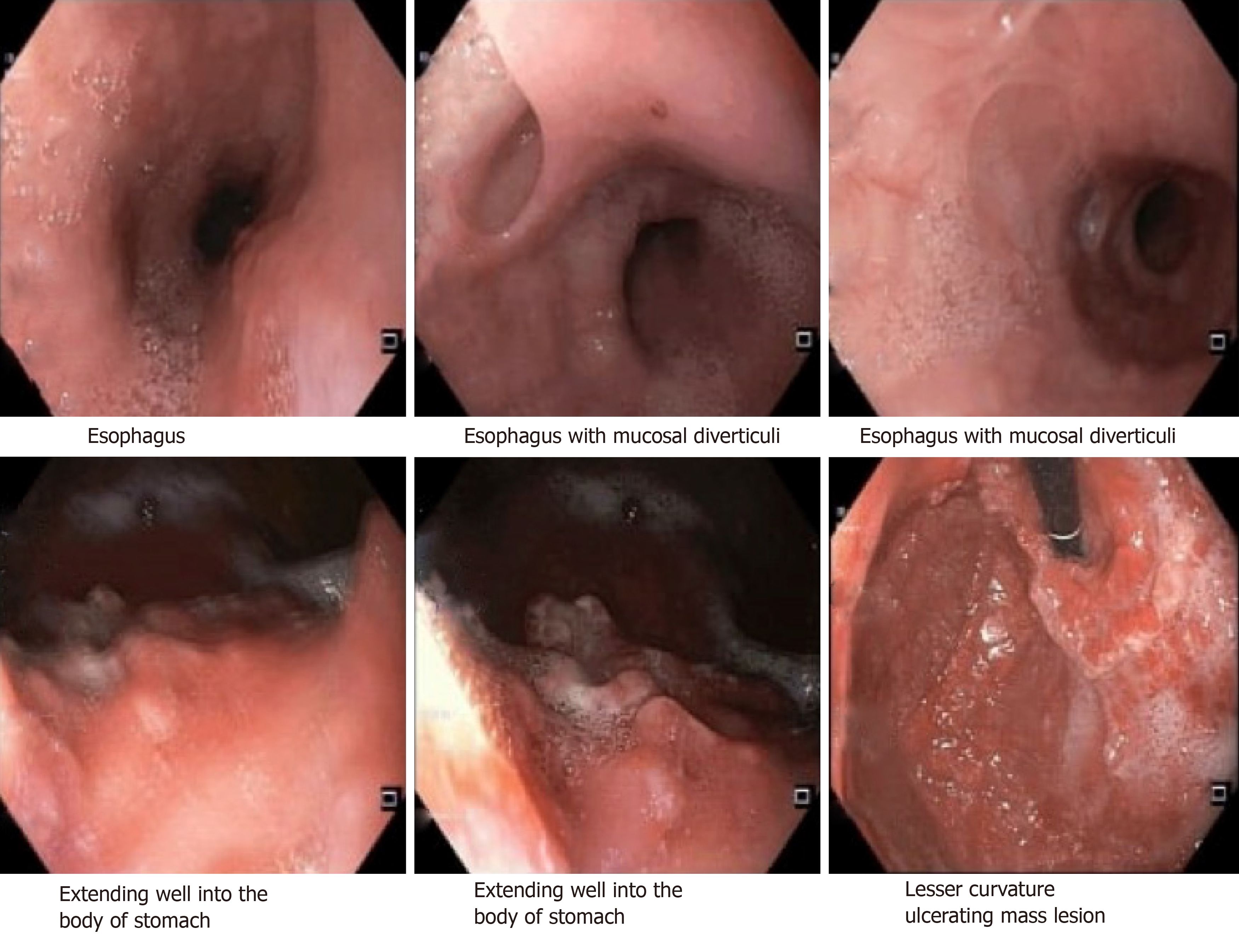
Routine laboratory work-up was done which turned out to be normal. Mantoux test was performed which was negative, and the chest X-ray was unremarkable. A barium-swallow examination was performed which showed moderate dilatation of the distal portion of esophagus with mucosal irregularity and nodularity (Figure 1). Thickening and narrowing of the gastro-esophageal junction was present but there was no evidence of a tight stricture (Figure 2). These findings were suggestive of inflammatory etiology.
Barium swallow examination shows slight thickening and narrowing of the gastro-esophageal junction with mucosal irregularity, no Figure 3 Computed tomography sagittal section shows dilated and fluid-filled distal esophagus with significant mural thickening of the distal esophagus.
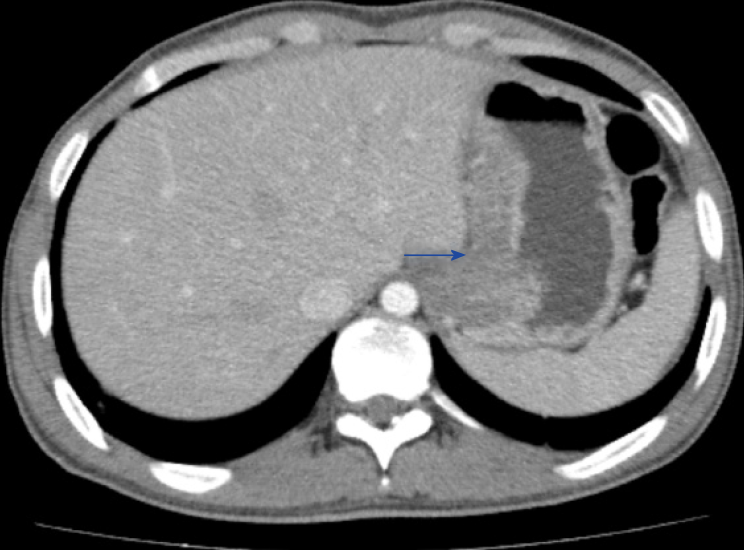
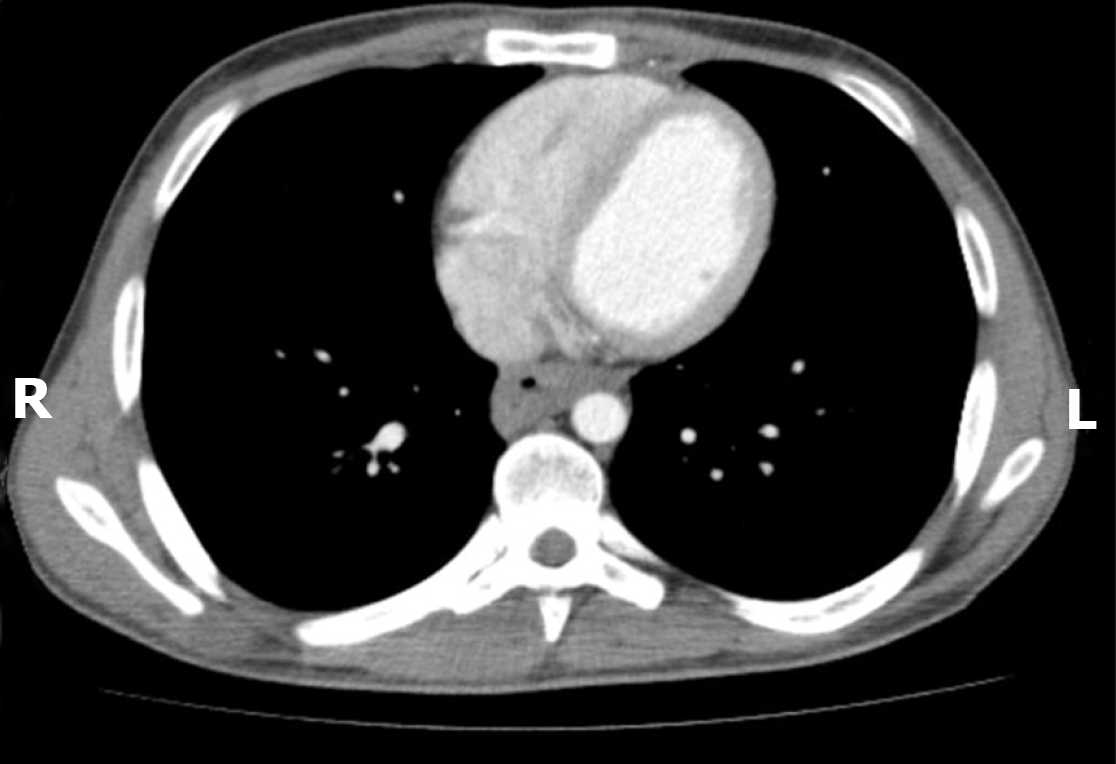
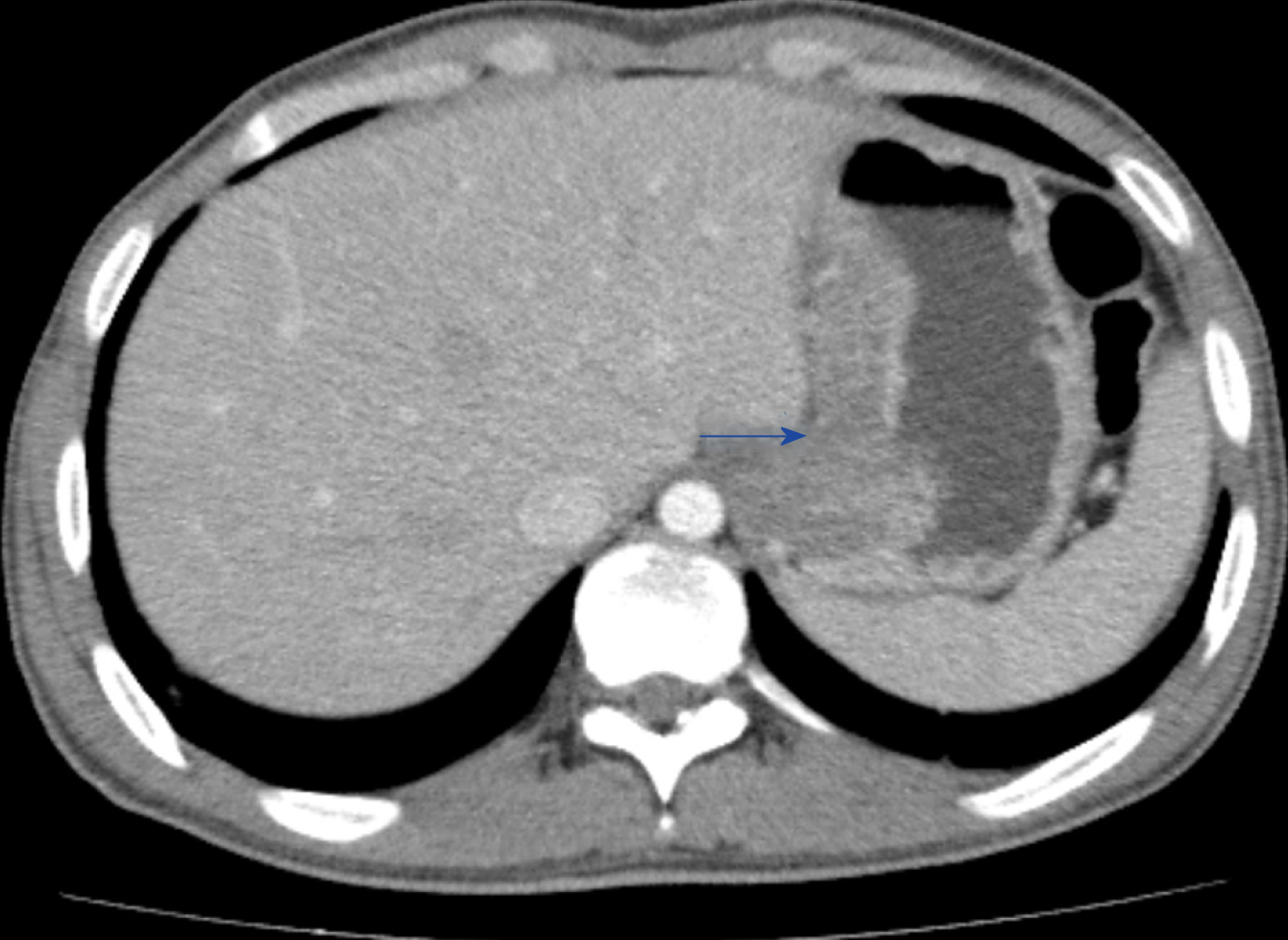
Computed tomography (CT) scan of the chest, abdomen and pelvis with contrast showed significant circumferential thickening of thoracic esophagus. The distal esophagus was dilated and fluid-filled with significant mural thickening near the gastro-esophageal junction (Figures 3-5). There was significant infiltration in the lesser omentum and enlarged, centrally necrotic lymph nodes were seen in the gastro-hepatic ligament, which pointed towards the possibility of malignancy (Figure 6).
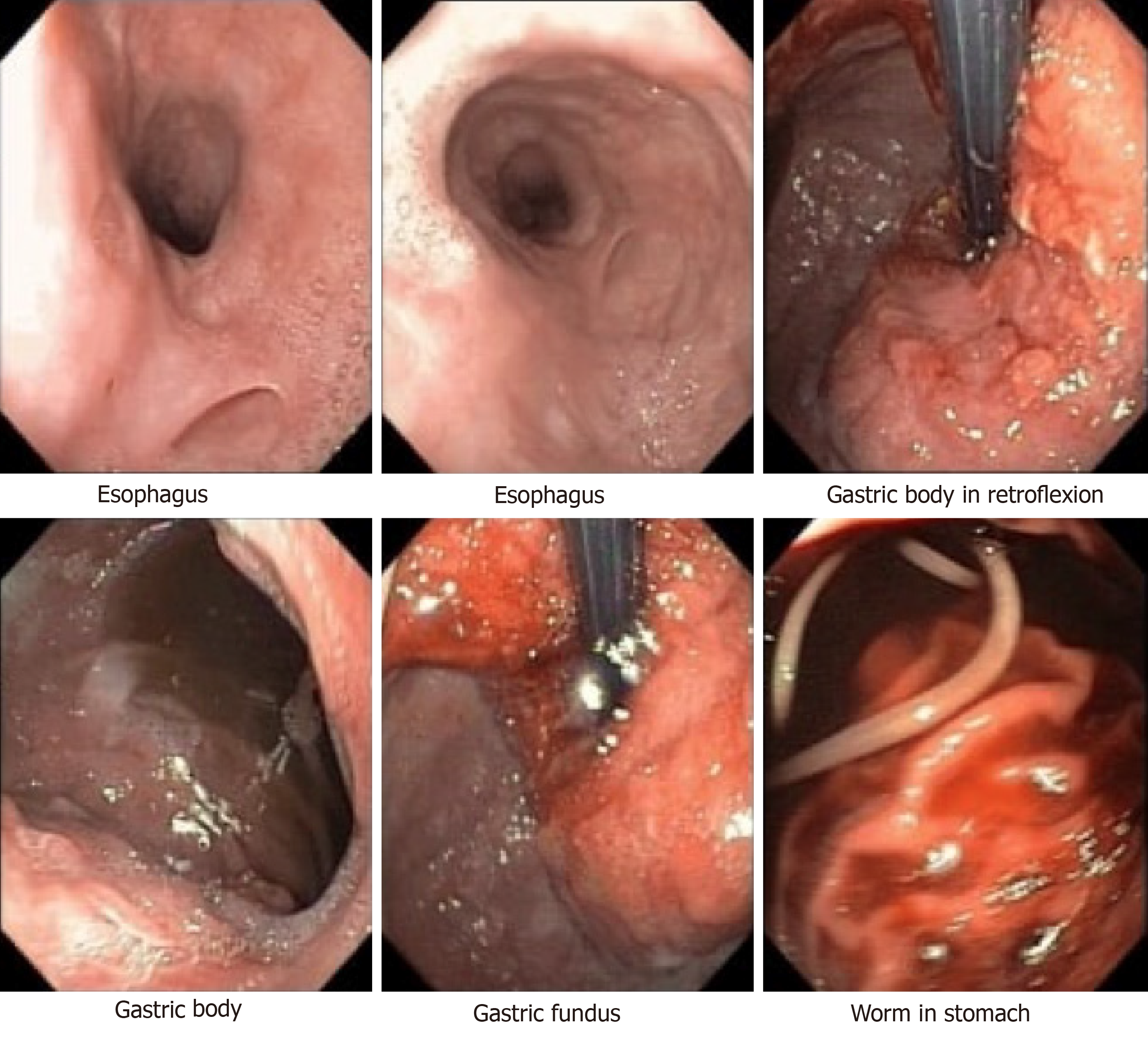
During esophagoscopy, a large circumferential growth was visualized starting from the middle and distal part of esophagus, involving the gastro-esophageal junction and extending up to 5 cm into the cardia of the stomach (Figures 7 and 8). The growth appeared glandular with thickened folds suggesting adenocarcinoma, neuroendo-crine tumor, or lymphoma.
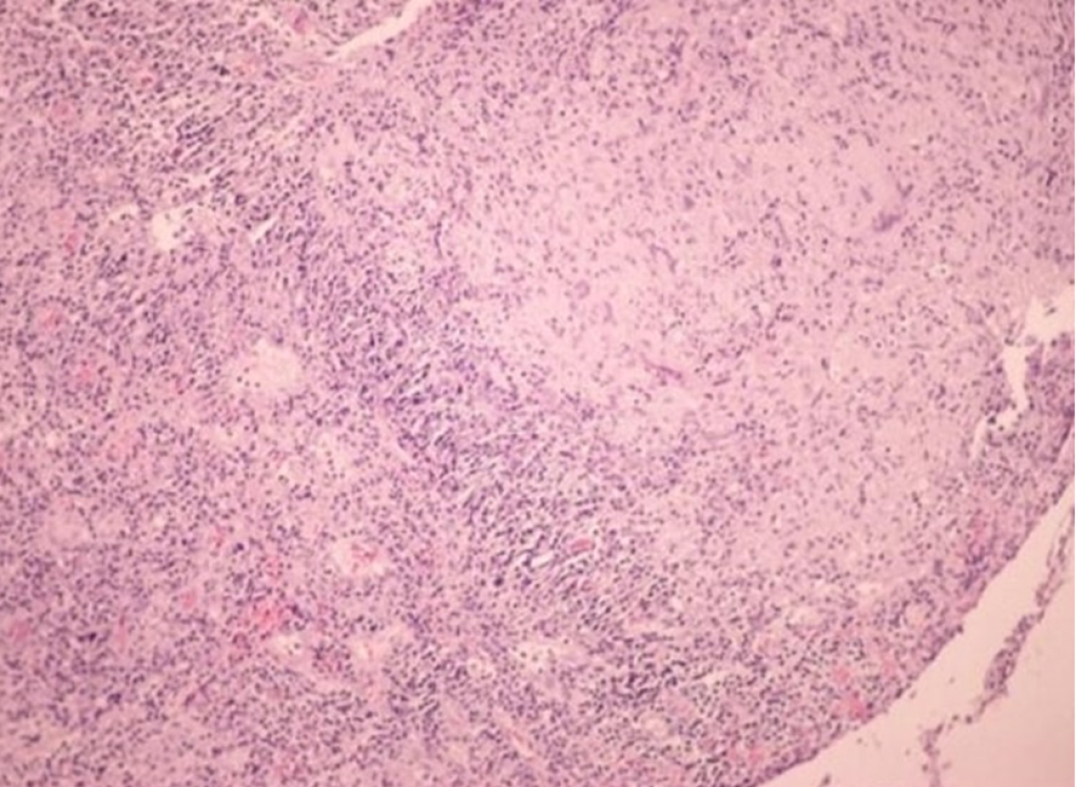
Biopsy of the mural thickening was performed. Histopathological examination showed hyperplastic changes in the mucosa and reactive atypia of the lining epithelium (Figure 9). Severe acute and chronic inflammation was present and occasional dilated glands were seen along with polypoid and pseudo-polypoid formation consisting of ulcer, slough, and granulation tissue. There was no evidence of a neoplastic lesion. PCR was positive for Mycobacterium tuberculosis in the esophageal biopsy. Subsequent cultures also showed M. tuberculosis growth.
Following the CT scan report, we strongly suspected a possible malignancy, which made esophage-al carcinoma and lymphoma our top differential diagnoses. Due to its high incidence in Pakistan, we also included TB in our list of differential diagnoses. However, the lack of supporting history, unremarkable laboratory work-up, negative Mantoux test, normal chest X-ray, and most importantly, absence of signs of active or past pulmonary TB on CT scan made the diagnosis a challenge. In the end, the histopathology report helped in ruling out a possible malignancy, and combined with a positive TB-PCR result, we made the final diagnosis of esophageal TB.
The patient was started on a 6-mo course with anti-tuberculous therapy (ATT) comprised of rifampicin, isoniazid, ethambutol, and pyrazinamide.
A significant response to ATT was noted, as the CT scan done at 1-mo follow-up showed significant interval reduction in esophageal mural thickening as well as size of the soft tissue infiltrating the lesser omentum. Dysphagia resolved within the first 2 mo. Following 6 mo of treatment, the patient had gained 8 kg in weight and reported the complete resolution of symptoms.
Esophageal TB is an extremely rare extrapulmonary manifestation of TB, constituting only 2.8% of total gastrointestinal TB cases[5]. In most cases, esophageal TB occurs secondary to direct extension from surrounding structures, such as infected mediastinal lymph nodes or a pulmonary focus. Primary esophageal TB cases have rarely been reported. In our patient, there was no previous history of TB along with absence of any signs of active or past pulmonary TB on imaging, suggesting primary esophageal TB. Moreover, the middle-third of esophagus is usually involved in secondary esophageal TB cases, with involvement of mediastinal or hilar lymph nodes[1]. In contrast, the distal esophagus was involved in this patient and there was no mediastinal or hilar lymphadenopathy, and lymph nodes in the gastro-hepatic ligament were involved instead.
Dysphagia is the most common presenting symptom, but odynophagia and retrosternal pain have also been reported[1,5]. Other symptoms including low-grade fever, malaise, decrease in appetite, and weight loss[4-6]. In severe cases where a trachea-esophageal fistula has formed, complaints of choking on swallowing and aspiration pneumonia can be found[7]. Thus, the non-specific presentation, combined with the rarity of the disease and limited evidence in the existing literature means that esophageal TB can be misdiagnosed (e.g., as esophageal cancer) and may lead to unnecessary interventions[6].
However, the unique aspect of this case was how the lesion mimicked an esophageal carcinoma on imaging which posed a diagnostic predicament. Only a handful of cases of esophageal TB mimicking esophageal carcinoma have been reported[7-11]. Interestingly, the natural course of esophageal TB leads to varying endoscopic and biopsy features. Most of the reported cases had one of the two types of lesions; either ulcers or an extrinsic bulge into the lumen. The presence of a hyperplastic lesion on histopathology, as seen in this patient, is also less commonly reported. Whereas the cases presenting with extrinsic bulge can be mistaken for sub-mucosal tumor; an ulcer or a hyperplastic lesion can be misdiagnosed as a carcinoma or lymphoma, which was also part of our differential diagnoses at one point. Other differentials include Crohn’s and Behcet’s disease.
Endoscopic ultrasound (EUS) is an important modality for diagnosis, which is especially useful in cases of extrinsic bulge lesions, as it helps identify the exact layer of the esophageal wall the lesion is located in. Similarly, in cases with submucosal bulge, EUS-guided fine needle aspiration is preferred over normal endoscopic biopsy as it has a higher sensitivity because the biopsy of the lesion can be collected along with the adjacent lymph nodes as well[7]. Histopathology report and TB-PCR remain investigations of choice in reaching the diagnosis of esophageal TB[12]. However, the sensitivity of identifying typical caseating granulomas on histopathology of endoscopy samples is low, ranging from 25.0% to 60.8%. This is because of either low density of tuberculous granulomas in affected tissue or insufficient representation of the submucosal layer, main site of tuberculous granulomas, on endoscopic biopsies[13]. Acid-fast bacillus staining of the biopsy sample is another option, but it has lower sensitivity[7]. CT scan with contrast is also a useful tool, and particularly helps delineate lymph node involvement.
Esophageal TB is primarily managed conservatively with a 6 mo course of ATT in immunocompetent patients. In this regimen, rifampicin, isoniazid, ethambutol, and pyrazinamide are given for the first 2 mo, followed by rifampicin and isoniazid for another 4 mo[2]. Surgery is considered as an option in cases of complications, such as a bleeding aorto-esophageal fistula, stricture or trachea-esophageal fistula[1]. These complications are very rare and can be effectively avoided with a complete course of ATT as in this patient.
In conclusion, esophageal TB is a rare disease that may mimic esophageal carcinoma on CT scan. Contrast enhanced CT scan, endoscopy followed by biopsy for histopathology, and TB-PCR are important tools for identifying the disease process. A complete course of ATT is the treatment of choice and usually prevents any further complications, and thus, the need for surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Pakistan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bandyopadhyay SK S-Editor: Ma RY L-Editor: Filipodia E-Editor: Zhou BX
| 1. | Anees A, Singh KD, Khan MA, Khan S. Tubercular esophagocutaneous fistula: A rare case. International Journal of Health & Allied Sciences. 2017;6:53. [DOI] [Full Text] |
| 2. | Gomes J, Antunes A, Carvalho A, Duarte R. Dysphagia as a manifestation of esophageal tuberculosis: a report of two cases. J Med Case Rep. 2011;5:447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Griga T, Duchna HW, Orth M, Nicolas V, Müller KM, Schultze-Werninghaus G, May B. Tuberculous involvement of the esophagus with oesophagobroncheal fistula. Digest Liver Dis. 2002;34:528-531. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Mou Y, Zeng H, Wang QM, Yi H, Liu W, Wen D, Hu B. Esophageal tuberculosis initially misdiagnosed by endoscopy as a submucosal tumor. Endoscopy. 2015;47 Suppl 1 UCTN:E30-E31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Patel N, Amarapurkar D, Agal S, Baijal R, Kulshrestha P, Pramanik S, Gupte P. Gastrointestinal luminal tuberculosis: establishing the diagnosis. J Gastroenterol Hepatol. 2004;19:1240-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Tang Y, Shi W, Sun X, Xi W. Endoscopic ultrasound in diagnosis of esophageal tuberculosis: 10-year experience at a tertiary care center. Dis Esophagus. 2017;30:1-6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Hu Z, Wang X, Gong L, Zhou Y, Meng M, Feng H, Tang S, Zhou Z. Case Report Esophageal tuberculosis presenting as a submucosal tumor. Int J Clin Exp Med. 2018;11:1226-1232. |
| 8. | Sharma V, Rana SS, Chhabra P, Sharma R, Gupta N, Bhasin DK. Primary esophageal tuberculosis mimicking esophageal cancer with vascular involvement. Endosc Ultrasound. 2016;5:61-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Leung VK, Chan WH, Chow TL, Luk IS, Chau TN, Loke TK. Oesophageal tuberculosis mimicking esophageal carcinoma. Hong Kong Med J. 2006;12:473. |
| 10. | Huang YK, Wu YC, Liu YH, Liu HP. Esophageal tuberculosis mimicking submucosal tumor. Interact Cardiovasc Thorac Surg. 2004;3:274-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Li Q, Ou Y, Liu T, Leng A. A Case Report of Mimicking Sub mucosal Tumor on Esophageal Tuberculosis. J Vasc Med Surg. 2016;4:2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Khanna V, Kumar A, Alexander N, Surendran P. A case report on esophageal tuberculosis - A rare entity. Int J Surg Case Rep. 2017;35:41-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Welzel TM, Kawan T, Bohle W, Richter GM, Bosse A, Zoller WG. An unusual cause of dysphagia: esophageal tuberculosis. J Gastrointestin Liver Dis. 2010;19:321-324. |