Published online Jun 27, 2019. doi: 10.4240/wjgs.v11.i6.296
Peer-review started: April 18, 2019
First decision: May 31, 2019
Revised: June 6, 2019
Accepted: June 21, 2019
Article in press: June 21, 2019
Published online: June 27, 2019
Processing time: 71 Days and 9.6 Hours
Paraduodenal pancreatitis (PP) is a rare form of chronic pancreatitis presenting with symptoms of duodenal obstruction. Conservative treatment is often unsuccessful and pancreaticoduodenectomy is the preferred surgical approach. A mini review of the outcomes of surgical therapy for PP shows that the results of pancreaticoduodenectomy are predominantly favorable.
In our case report of PP, we describe an unusual course first presenting with the symptoms of chronic pancreatitis and a pseudocyst of the pancreatic tail. A pseudocystojejunostomy was performed and the late postoperative course was complicated with the symptoms of duodenal obstruction. At laparotomy, PP was found and the patient was treated with a total pancreatectomy. The postoperative course was uneventful and good weight gain with resolution of pain was demonstrated at follow up visits.
Surgery is currently the optimal treatment option for PP. It is also the best diagnostic tool in distinguishing between pancreatitis and pancreatic adenocarcinoma.
Core tip: Paraduodenal pancreatitis (PP) is a rare form of chronic pancreatitis presenting with symptoms of duodenal obstruction. Conservative treatment is often unsuccessful and pancreaticoduodenectomy is the preferred surgical approach. Differential diagnosis from carcinoma of the pancreatic head can be quite difficult and it is often only postoperative pathology that provides the definitive diagnosis. In this case report we present an uncommon case where PP was associated with a necrotic pseudocyst of the tail of the pancreas and the patient was treated with total pancreatectomy.
- Citation: Mikulić D, Bubalo T, Mrzljak A, Škrtić A, Jadrijević S, Kanižaj TF, Kocman B. Role of total pancreatectomy in the treatment of paraduodenal pancreatitis: A case report. World J Gastrointest Surg 2019; 11(6): 296-302
- URL: https://www.wjgnet.com/1948-9366/full/v11/i6/296.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i6.296
Paraduodenal pancreatitis (PP) is an often unrecognized form of chronic pancreatitis that can present with diagnostic and therapeutic dilemmas. It is a rare form of focal pancreatitis involving the area of the paraduodenal groove, that is, the area between the dorso-cranial portion of the pancreatic head, duodenum and the common bile duct. It was first described in 1970 and the authors proposed the term ’’duodenal dystrophy’’[1]. Several other synonyms for PP have appeared based on different pathologic and imaging characteristics of this uncommon disease, including: Groove pancreatitis, paraduodenal wall cysts, cystic pancreatic heterotopic dystrophy, myoadenomatosis of the duodenum and pancreatic hamartoma of the duodenum[2]. The exact incidence of PP is difficult to establish as it is often unrecognized, but is reported to be found in 12.8%-19.5% of surgical specimens after pancreaticoduo-denectomy for chronic pancreatitis[2,3]. PP is frequently associated with the presence of heterotopic pancreatic tissue in the duodenal wall, therefore, the pathogenesis of PP is believed to be related to chronic inflammation of this tissue. Alcohol consumption is found to be the culprit in most patients. In 15 retrospective reports, 79.68% patients (251 out of 305) with PP were alcohol abusers[4].
PP is clinically manifested by recurrent episodes of pancreatitis, chronic abdominal pain located mostly in the epigastrium, obstructive jaundice, weight loss, nausea and vomiting caused by duodenal stenosis[2,5]. Diagnosis is based on computer tomography (CT) and magnetic resonance (MR) imaging and endoscopic ultrasound. Differential diagnosis from carcinoma of the pancreatic head can be quite difficult and it is often only postoperative pathology that provides the definitive diagnosis.
Different treatment modalities have been proposed for PP, ranging from medical management to endoscopic treatment to surgical resection. However, it seems that surgical therapy, namely pancreaticoduodenectomy (PD) offers the best long-term results in patients with PP[6,7]. Apart from symptom resolution, it also provides for definitive pathologic diagnosis and prevents recurrence[8-10].
The purpose of this review is to summarize the cases of PP treated with PD that have been published to date, to evaluate the results and analyze the role of surgical therapy. Also, we present an uncommon case where PP was associated with a necrotic pseudocyst of the tail of the pancreas and the patient was treated by total pancreatectomy (TP).
A PubMed literature search was performed for studies dealing with surgical treatment for PP published between 2000 and 2018. Key words used were groove pancreatitis, PP, duodenal wall cyst, cystic pancreatic heterotopic dystrophy, myoadenomatosis of the duodenum, pancreatic hamartoma of the duodenum and synonyms, surgical treatment, surgery and pancreaticoduodenectomy. Only studies published in English were analyzed (Table 1).
| Ref. | Study design | Period | No. of patients | No. of operated patients |
| Rahman et al[9] | Prospective | 2000-2005 | 11 | 11 |
| Egorov et al[6] | Prospective | 2004-2013 | 62 | 52 |
| Casetti et al[10] | Prospective | 1990-2006 | 58 | 58 |
| Oza et al[15] | Case control | 2000-2013 | 13 | 9 |
| Jounnaud et al[16] | Retrospective | 1990-2004 | 23 | 14 |
| Rebours et al[17] | Retrospective | 1995-2004 | 105 | 29 |
A 69-year old man presented with a history of chronic alcoholic pancreatitis and an 8 cm x 6 cm pseudocyst of the pancreatic tail. He complained of long lasting symptoms including chronic abdominal pain, nausea and early satiety.
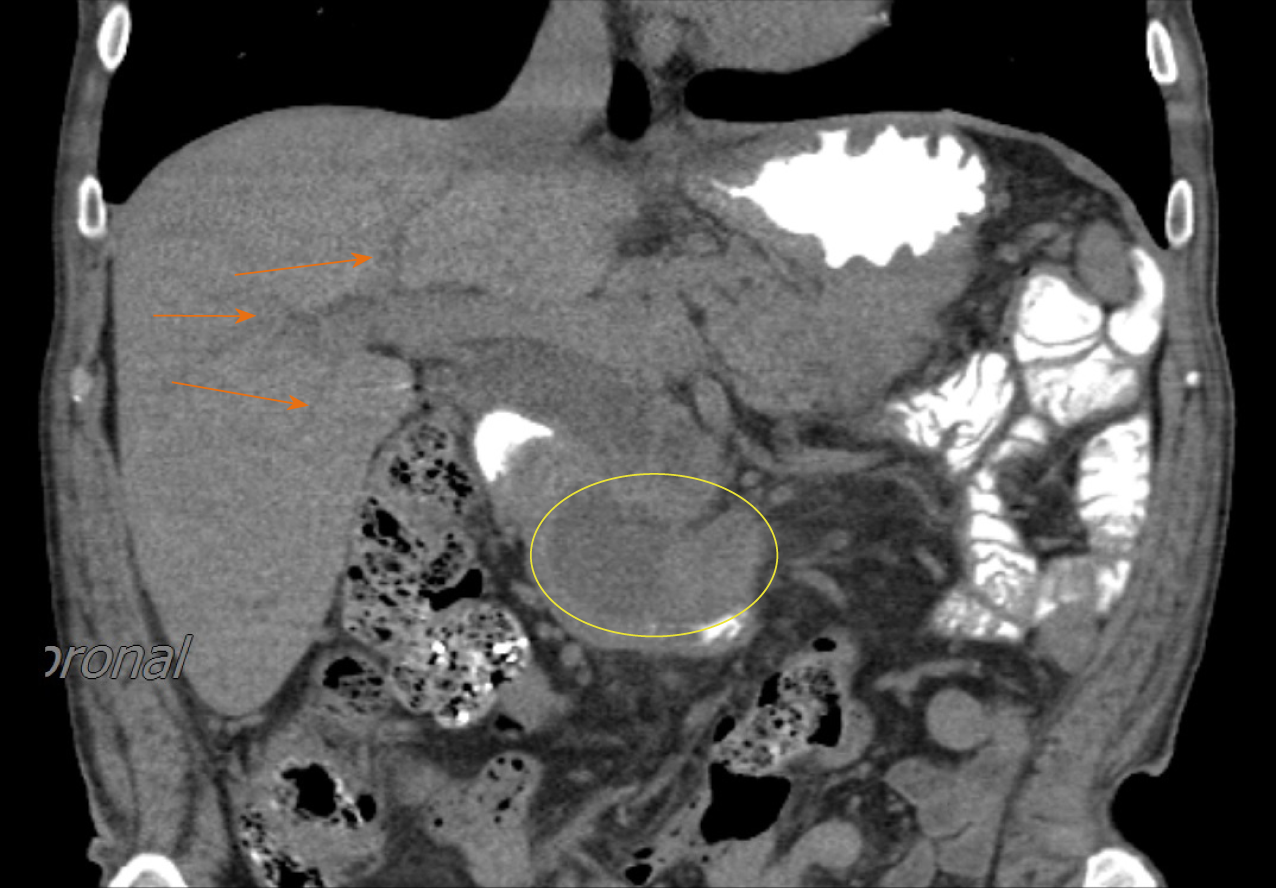
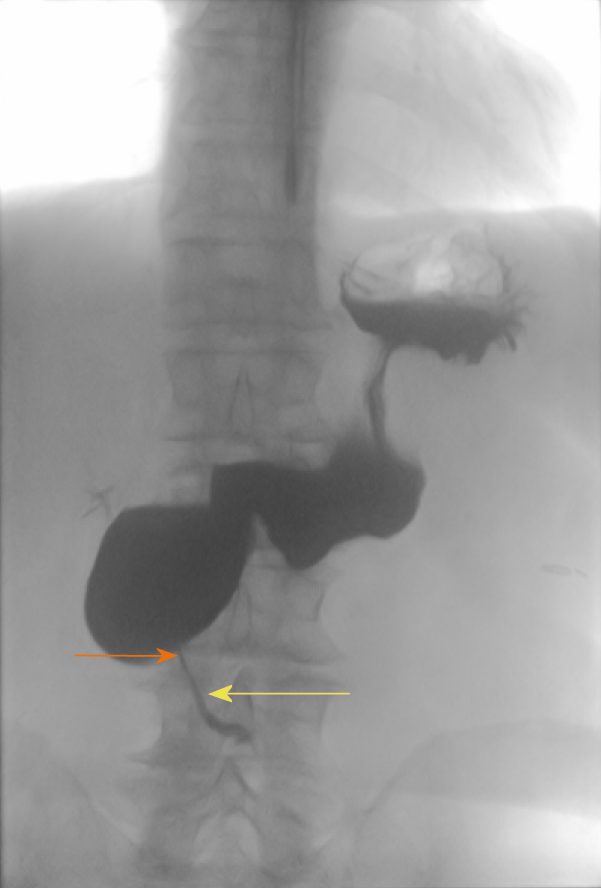
Preoperative upper endoscopy and multi-slice computer tomography (MSCT) showed no other pathological findings, with normal appearance of the duodenum and the pancreatic head. He underwent an uneventful surgical pseudocystojejunostomy with a normal operative and early postoperative course. Three months postoperatively he presented to the emergency department with epigastric pain, intense nausea, vomiting, intolerance of solid food and profound weight loss. An urgent MSCT showed a markedly enlarged pancreatic head with suspected tumor involvement of the pancreatico-duodenal complex and dilation of the intrahepatic and extrahepatic bile ducts (Figure 1). On upper endoscopy, obstruction of the duodenum was apparent with duodenal biopsy showing nonspecific mucosal changes consistent with chronic inflammation. Upper gastrointestinal series also showed obstruction of the duodenum (Figure 2). A decision was made to perform a PD. At laparotomy, the operation was extended into a TP since the pancreatic tail showed marked atrophy with necrotic debris filling the residual psudocyst. Both operative and postoperative courses were uneventful. The patient was released on the 10th postoperative day and after 6 months of follow-up, the patient was unremarkable, with no pain and a weight gain of 7 kg. The control of his diabetes is satisfactory with HbA1c value of 7%.
Apart from chronic pancreatitis the patient had no significant past medical history.
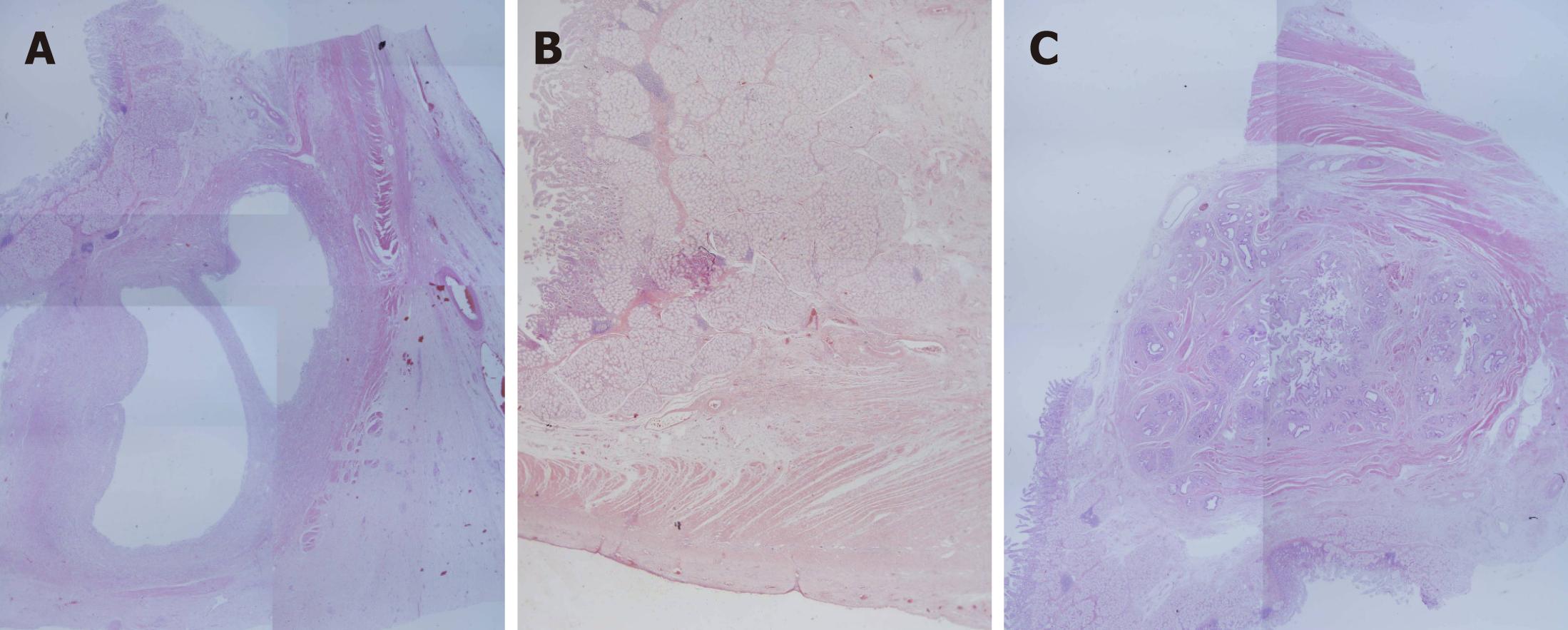
Pathology report showed a thickened duodenal mucosa with cysts ranging in dia-meter up to 0.9 cm containing clear fluid, permeating at the interface between the duodenum and the pancreas. Hyperplasia of Brunner's glands and smooth muscle cells was visible with proliferation of connective tissue in lamina propria, submucosal and subserosal tissues. Pancreatic tissue in the paraduodenal area showed a reduction of the lobular arhitecture that was replaced with connective tissue. Epithelial changes in the pancreatic periferal small ducts were consistent with pancreatic intraepithelial neoplasia (PanIN) 2 and 3 in unaffected pancreatic tissue. Serial sectioning of the specimen revealed the minor papilla proximal to the major papilla. Papilla was affected with the disease (Figure 3).
PP is described as an inflammatory process between the C-loop of the duodenum and the head of the pancreas. It is mainly associated with male gender, smoking and alcohol consumption[3]. Duodenal stenosis and cystic lesions in the duodenum are common findings. It is clearly a distinct entity from chronic pancreatitis of the pancreas proper and from pancreatic pseudocysts. Cystic lesions of PP are lined with epithelium and they are located inside the duodenal wall with no connection to the pancreas proper[5]. On the other hand, in a number of patients, PP is associated with more extensive chronic pancreatitis and pancreatic pseudocysts.
Two theories exist regarding the pathophysiology of the disease. First, PP may be the consequence of obstruction of small ducts of heterotopic pancreatic tissue in the duodenum leading to acute and chronic inflammation[11]. Second mechanism associates the toxic effects of alcohol in heterotopic pancreas leading to chronic inflammation. The mechanisms of obstruction and alcohol toxicity in pancreatitis of the pancreaticoduodenal groove may even be synergistic[5].
In most series, patients with PP are first offered medical management. Conservative treatment relies on analgetics, alcohol abstinence, octreotide and endoscopic fenestra-tion of the cysts. However, when conservative treatment fails, surgery is performed with pancreaticoduodenectomy playing a central role in the surgical armamentarium.
In this mini-review, we have analyzed several reports focusing on surgical tre-atment of PP. Results of surgical treatment are overall good with 80% of patients reporting complete relief of symptoms after surgery. The majority of patients in the analyzed studies have been treated with pancreaticoduodenectomy. The procedures that are performed less often include bypass procedures, pancreas preserving duodenal resections and duodenum preserving pancreatic head resections (Table 2). Bypass procedures may relieve the symptoms but they can not prevent recurrents bouts of pancreatitis. The efficiency of duodenum and pancreas preserving resections is limited by incomplete resection of the groove area[6]. On the other hand, pancrea-ticoduodenectomy is usually effective since all of the diseased tissue is removed. Literature analyzed in this mini-review provides evidence that suggests good outcomes after pancreaticoduodenectomy for PP. Most of the patients experience pain relief and weight gain. Even though it is a major procedure with significant morbidity and mortality, PD is still the best option both for diagnostic and for therapeutic mana-gement of PP.
| Characteristics of operated patients | 173 (100) |
| PD | 134 (77.5) |
| Pancreas preserving duodenal resection | 10 (5.8) |
| Duodenum preserving pancreatic head resection | 5 (2.9) |
| Bypass | 16 (9.2) |
| Pseudocyst drainage | 8 (4.6) |
| Outcome | |
| Success | 136 (78.6) |
| Partial success | 35 (20.2) |
| Failure | 2 (1.2) |
In the literature, we have not found any reports of TP for PP. Our patient had an atypical course first presenting with a symptomatic pseudocyst of the pancreatic tail and chronic pancreatitis of the pancreas proper. At the time, he had no signs of duodenal obstruction or other symptoms of PP. Only several months after pseudocy-stojejunostomy, there was an exacerbation of PP with complete duodenal obstruction that prompted surgery. Due to necrosis and atrophy of the remaining body and tail of the pancreas, the decision was made to perform a TP. Despite being a more extensive operation than PD, TP today has similar postoperative outcomes without the risk of a pancreatic fistula[12]. In the past, metabolic problems such as brittle insulin-dependent diabetes mellitus and malabsorption due to loss of pancreatic exocrine secretion were difficult to control. Weight loss, diarrhea and malabsorption often contributed to cachexia-like syndrome and to considerable loss of quality of life in patients after TP. Due to these reasons, TP was largely abandoned for a long time[13].
Significant improvements in the control of diabetes together with the pancreatic enzyme treatments for exocrine pancreatic insufficiency provide good options for overcoming postoperative consequences of TP[14]. Therefore, chronic pancreatitis with involvement of both the head and the body of pancreas can be one of the emerging indications for this operation.
This report highlights good outcomes of surgical treatment for PP. Apart from symptom relief, it is frequently also the best diagnostic tool since differential diagnosis between PP and pancreatic head adenocarcinoma can often be quite difficult. PD is the usual surgical approach, however, TP can also be a good choice if the body and tail of the pancreas are consumed with pseudocysts or chronic pancrea-titis.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Croatia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fan Y, Jin C, Lieto E S-Editor: Ma YJ L-Editor: A E-Editor: Wang J
| 1. | Potet F, Duclert N. [Cystic dystrophy on aberrant pancreas of the duodenal wall]. Arch Fr Mal App Dig. 1970;59:223-238. [PubMed] |
| 2. | Adsay NV, Zamboni G. Paraduodenal pancreatitis: a clinico-pathologically distinct entity unifying "cystic dystrophy of heterotopic pancreas", "para-duodenal wall cyst", and "groove pancreatitis". Semin Diagn Pathol. 2004;21:247-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 137] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 3. | Becker V, Mischke U. Groove pancreatitis. Int J Pancreatol. 1991;10:173-182. [PubMed] |
| 4. | Pezzilli R, Santini D, Calculli L, Casadei R, Morselli-Labate AM, Imbrogno A, Fabbri D, Taffurelli G, Ricci C, Corinaldesi R. Cystic dystrophy of the duodenal wall is not always associated with chronic pancreatitis. World J Gastroenterol. 2011;17:4349-4364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Fléjou JF, Potet F, Molas G, Bernades P, Amouyal P, Fékété F. Cystic dystrophy of the gastric and duodenal wall developing in heterotopic pancreas: an unrecognised entity. Gut. 1993;34:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Egorov VI, Vankovich AN, Petrov RV, Starostina NS, Butkevich ATs, Sazhin AV, Stepanova EA. Pancreas-preserving approach to "paraduodenal pancreatitis" treatment: why, when, and how? Experience of treatment of 62 patients with duodenal dystrophy. Biomed Res Int. 2014;2014:185265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Galloro G, Napolitano V, Magno L, Diamantis G, Nardone G, Bruno M, Mollica C, Persico G. Diagnosis and therapeutic management of cystic dystrophy of the duodenal wall in heterotopic pancreas. A case report and revision of the literature. JOP. 2008;9:725-732. [PubMed] |
| 8. | Pessaux P, Lada P, Etienne S, Tuech JJ, Lermite E, Brehant O, Triau S, Arnaud JP. Duodenopancreatectomy for cystic dystrophy in heterotopic pancreas of the duodenal wall. Gastroenterol Clin Biol. 2006;30:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Rahman SH, Verbeke CS, Gomez D, McMahon MJ, Menon KV. Pancreatico-duodenectomy for complicated groove pancreatitis. HPB (Oxford). 2007;9:229-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Casetti L, Bassi C, Salvia R, Butturini G, Graziani R, Falconi M, Frulloni L, Crippa S, Zamboni G, Pederzoli P. "Paraduodenal" pancreatitis: results of surgery on 58 consecutives patients from a single institution. World J Surg. 2009;33:2664-2669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Leger L, Lemaigre G, Lenriot JP. [Cysts on heterotopic pancreas of the duodenal wall]. Nouv Presse Med. 1974;3:2309-2314. [PubMed] |
| 12. | Casadei R, Monari F, Buscemi S, Laterza M, Ricci C, Rega D, D'Ambra M, Pezzilli R, Calculli L, Santini D, Minni F. Total pancreatectomy: indications, operative technique, and results: a single centre experience and review of literature. Updates Surg. 2010;62:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 13. | Barbier L, Jamal W, Dokmak S, Aussilhou B, Corcos O, Ruszniewski P, Belghiti J, Sauvanet A. Impact of total pancreatectomy: short- and long-term assessment. HPB (Oxford). 2013;15:882-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 14. | Epelboym I, Winner M, DiNorcia J, Lee MK, Lee JA, Schrope B, Chabot JA, Allendorf JD. Quality of life in patients after total pancreatectomy is comparable with quality of life in patients who undergo a partial pancreatic resection. J Surg Res. 2014;187:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Oza VM, Skeans JM, Muscarella P, Walker JP, Sklaw BC, Cronley KM, El-Dika S, Swanson B, Hinton A, Conwell DL, Krishna SG. Groove Pancreatitis, a Masquerading Yet Distinct Clinicopathological Entity: Analysis of Risk Factors and Differentiation. Pancreas. 2015;44:901-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Jouannaud V, Coutarel P, Tossou H, Butel J, Vitte RL, Skinazi F, Blazquez M, Hagège H, Bories C, Rocher P, Belloula D, Latrive JP, Meurisse JJ, Eugène C, Dellion MP, Cadranel JF, Pariente A; Association Nationale des Hépato-Gastroentérologues des Hôpitaux généraux. Cystic dystrophy of the duodenal wall associated with chronic alcoholic pancreatitis. Clinical features, diagnostic procedures and therapeutic management in a retrospective multicenter series of 23 patients. Gastroenterol Clin Biol. 2006;30:580-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Rebours V, Lévy P, Vullierme MP, Couvelard A, O'Toole D, Aubert A, Palazzo L, Sauvanet A, Hammel P, Maire F, Ponsot P, Ruszniewski P. Clinical and morphological features of duodenal cystic dystrophy in heterotopic pancreas. Am J Gastroenterol. 2007;102:871-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |