Published online Mar 27, 2019. doi: 10.4240/wjgs.v11.i3.169
Peer-review started: February 20, 2019
First decision: February 26, 2019
Revised: March 2, 2019
Accepted: March 20, 2019
Article in press: March 20, 2019
Published online: March 27, 2019
Processing time: 35 Days and 15.7 Hours
Enhanced recovery after surgery (ERAS) reduces hospitalization and complication following colorectal surgery. Whether the experience of multidisciplinary ERAS team affects patients’ outcomes is unknown.
To evaluate and establish a learning curve of ERAS program for open colorectal surgery.
This was a review of prospectively collected database of 380 “unselected” patients undergoing elective “open” colectomy and/or proctectomy under ERAS protocol from 2011 (commencing ERAS application) to 2017 in a university hospital. Patients were divided into 5 chronological groups (76 cases per quintile). Surgical outcomes and ERAS compliance among quintiles were compared. Learning curves were calculated based on criteria of optimal recovery: defined as absence of major postoperative complications, discharge by postoperative day 5, and no 30-d readmission.
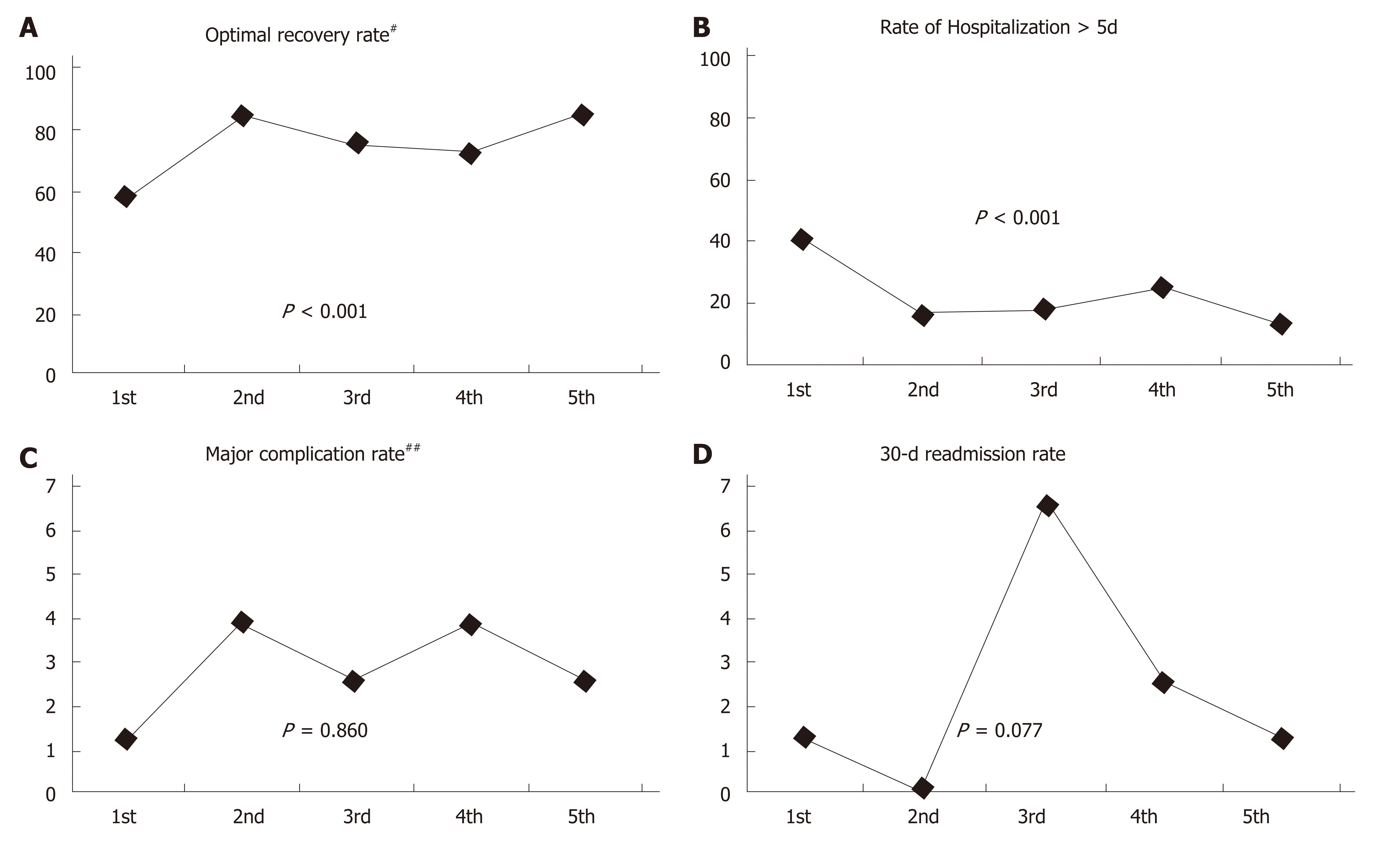
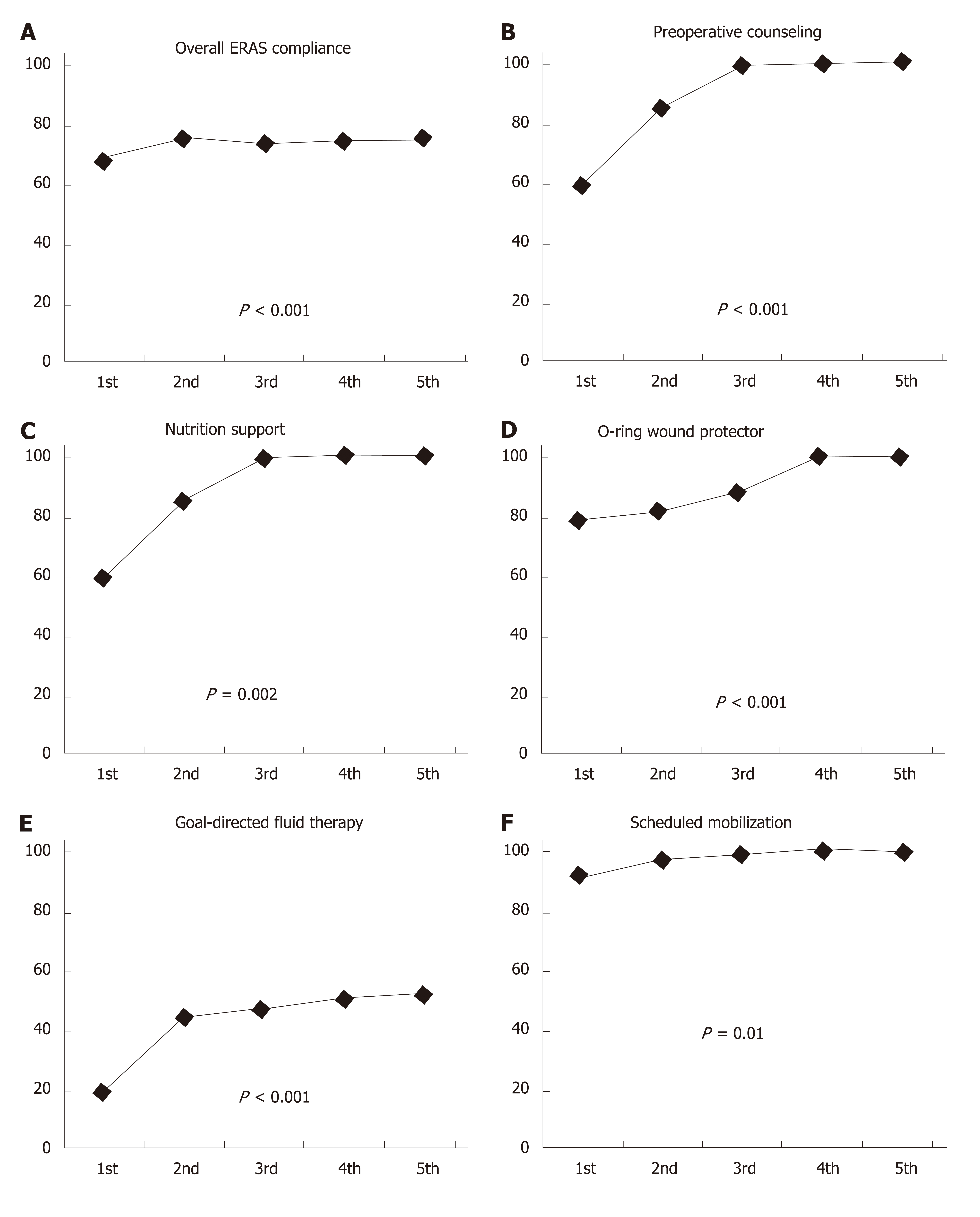
Hospitalization more than 5 d occurred in 22.6% (n = 86), major complication was present in 2.9% (n = 11) and 30-d readmission rate was 2.4% (n = 9) accounting for unsuccessful recovery of 25% (n = 95). Conversely, the overall rate of optimal recovery was 75%. The optimal recovery significantly increased from 57.9% in 1st quintile to 72.4%-85.5% in the following quintiles (P < 0.001). Average compliance with ERAS protocol gradually increased over the time - from 68.6% in 1st quintile to 75.5% in 5th quintile (P < 0.001). The application of preoperative counseling, nutrition support, goal-directed fluid therapy, O-ring wound protector and scheduled mobilization significantly increased over the study period.
A number of 76 colorectal operations are required for a multidisciplinary team to achieve a significantly higher rate of optimal recovery and high compliance with ERAS program for open colorectal surgery.
Core tip: Whether the learning curve of surgeon and multidisciplinary team affects enhanced recovery after surgery (ERAS) outcomes is unknown. This study showed that a number of 76 cases are required for an ERAS team to achieve a high compliance (> 70%) with ERAS program and a significantly higher rate of optimal recovery following open colorectal surgery. The application of preoperative counseling, nutrition support, goal-directed fluid therapy, O-ring wound protector and scheduled mobilization significantly increased over the study period.
- Citation: Lohsiriwat V. Learning curve of enhanced recovery after surgery program in open colorectal surgery. World J Gastrointest Surg 2019; 11(3): 169-178
- URL: https://www.wjgnet.com/1948-9366/full/v11/i3/169.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i3.169
Enhanced recovery after surgery (ERAS) has been shown to reduce morbidities and length of hospital stay following elective and emergency colorectal surgery[1,2]. This multimodal program introduces a number of preoperative, intraoperative and postoperative measures aiming to minimize surgical stress responses and facilitate patient’s recovery[3]. There have been several reports showing that improved adherence to the ERAS program is significantly associated with improved clinical outcomes after colorectal operations[4,5]. However, the effective implementation of ERAS requires close collaboration of multidisciplinary ERAS team comprising surgeons, anesthesiologists, nurses, nutritionists and physiotherapists. The initial stage of ERAS application into surgical practice could be a crucial phase of this patient-centered perioperative pathway because the workflow of heath care personals needs to be adopted and the guideline has to assimilate into a daily practice. A prospective study of early implementation of ERAS program in laparoscopic colorectal surgery has demonstrated that at least 30 patients and a period of 6 mo are required to achieve an ERAS compliance of 80% or more[6].
Despite increasing uptake of laparoscopic colorectal surgery worldwide, open surgery still remained the most common approach for colorectal resections[7,8]. When comparing laparoscopy and open surgery within an ERAS program for colorectal surgery, the latter had a higher rate of complication and was more difficulty to implement an ERAS program[9]. There are several studies on the impact of ERAS compliance on surgical outcomes[4,5,10,11], but little attention is drawn to the analysis of the early stage of ERAS implementation into colorectal operation especially in an open surgery - as a learning curve of a multidisciplinary ERAS team.
The primary objective of the study was to evaluate and establish the learning curve for the implementation of an ERAS program in “open” colorectal operations using defined criteria of optimal recovery (no major postoperative complication, i.e., Clavien-Dindo grade ≥ III, discharge by postoperative day 5, and no 30-d readmission)[12].
A prospectively collected database has been maintained since the beginning of ERAS program in 2011 for elective colorectal surgery in our Colorectal Unit (Faculty of Medicine Siriraj Hospital, Mahidol University - the largest tertiary referral hospital in Thailand). All unselected patients undergoing open colectomy and/or proctectomy with this ERAS program from January 2011 to October 2017 were reviewed. Patients undergoing laparoscopic colorectal surgery were excluded because this study focused on the analysis of learning curve for ERAS program - not the that for laparoscopic surgery which may be influenced by surgeon’s experience and operative complexity. Moreover, laparoscopy might be a key factor offering independent advantages beyond an ERAS program[9,10]. Patients undergoing non-resection surgery (e.g., loop colostomy and colonic bypass procedures) and those with clinical peritonitis or acute colonic obstruction were also excluded. The study was approved by the institutional ethics committee (Si 498/2017) and written informed consent was obtained from each patient.
The application of ERAS strategies into elective colorectal surgery in our unit was initiated by a board-certified colorectal surgeon (the author) who learnt the concept of this perioperative care pathway while studying a PhD degree in Gastrointestinal Surgery in the United Kingdom. In late 2010, a multidisciplinary ERAS team was formed by a colorectal surgeon, two anesthesiologists, a nutritionist, ostomy nurses, nursing staffs and surgical residents. At that time, our ERAS protocol for open colorectal operations had 17 core elements (Table 1) which were adopted from the consensus review of ERAS society for elective colorectal surgery[13]. In early 2011, the protocol was routinely applied into a daily surgical practice with a regular audition. We set a targeted discharge by postoperative day 5 because in the literature review an ERAS protocol reduced the length of hospital stay by 2-3 d[1] and hospital stay after open colorectal operations under a conventional pathway in our unit was about 7-8 d[14,15]. Patients would be discharged from the hospital if they met all criteria: no fever, satisfactory gastrointestinal recovery, adequate pain control with oral analgesics, and a good level of ambulation. All of the patients were scheduled for follow-up at 7-10 d and 30 d after an operation. Notably, all of the studied patients were operated on and treated by single surgeon (the author) and his multidisciplinary team. Since an ERAS program is a dynamic multimodal care pathway, some elements were added into the program later. These interventions were the administration of synthetic albumin in patients with persistent oliguria after the adequate infusion of crystalloid solution (from June 2015) and the routine postoperative administration of prokinetic agent (from April 2016).
| Preadmission |
| 1 Cessation of smoking and intake of alcohol; 2 Nutrition assessment and nutrition support as needed; 3 Medical optimization of chronic disease |
| Preoperative |
| 4 Structured preoperative counseling to patients and their relatives; 5 No mechanical bowel preparation; 6 Administration of appropriate prophylactic antibiotics; 7 Prophylaxis of postoperative nausea and vomiting |
| Intraoperative |
| 8 Use of epidural anesthesia; 9 Use of atraumatic O-ring wound retractor/protector; 10 Avoid hypothermia; 11 Maintaining fluid balance and vasopressors to support blood pressure control; 12 No intraabdominal or pelvic drain |
| Postoperative |
| 13 Early intake of oral fluids and semi-solid foods (day of surgery); 14 Early ambulation (postoperative day 1); 15 Multimodal approach to opioid-sparing pain control; 16 Removal of urinary catheter by postoperative day 3; 17 Discontinuous intravenous fluid infusion by postoperative day 3 |
Data including patient characteristics, operative details, and postoperative outcomes were prospectively collected. Patient characteristics included age, gender, body mass index, American Society of Anesthesiologists (ASA) classification, and ColoRectal Physiological and Operative Severity Score for the enUmeration of Mortality and Morbidity (CR-POSSUM) score[16]. Operative details included type of operation, operative time, and estimated blood loss. Postoperative outcomes included postoperative complications (graded I-V according to the Clavien-Dindo classification system)[17], time to tolerate solid food, time to first bowel movement, length of postoperative stay, death and readmission within 30 d after the operation. Overall compliance with ERAS protocol of each patient was determined based on our initial ERAS protocol (17 core elements).
Patients were divided into 5 chronological groups (1st–5th quintile). Surgical outcomes and compliance with ERAS protocol between groups were compared. Learning curves were calculated based on the criteria of optimal recovery (defined as no major postoperative complication, i.e., Clavien-Dindo grade ≥ III, discharge by postoperative day 5, and no 30-d readmission)[12].
All statistical analyzes were performed using the PASW Statistics software (SPSS version 18.0 for Windows, Illinois, United States). Continuous variables were expressed as mean ± SD or median (interquartile range; IQR) and were compared among groups using one-way analysis of variance (ANOVA) or the Kruskal-Wallis test. Categorical data were expressed as number (percentage) and were compared using the Pearson Chi-square test or Fisher exact probability test. A P-value of <0.05 was considered statistically significant.
During the study period of 82 mo, 489 colorectal resections were performed by the author and his multidisciplinary team under an ERAS protocol. Of these, 57 operations were for acute colonic obstruction or peritonitis, and 52 operations were laparoscopic surgery. Therefore, there were 380 patients undergoing elective “open” colectomy and/or proctectomy. These patients were divided into 5 chronological groups (76 cases per quintile). Of 380 cases, 75 patients (20%) had ASA classification ≥ 3 and a median CR-POSSUM predicting mortality of 1.8 (IQR 1.00-2.58). Colorectal cancer was the most indication for surgery (n = 347, 91%). Some 165 patients (43%) underwent proctectomy and 82 patients (22%) had temporary or permanent stoma formation. Patients’ characteristic and operative details were comparable among quintiles (Table 2).
| Overall | 1st quintile | 2nd quintile | 3rd quintile | 4th quintile | 5th quintile | P value | |
| (n = 380) | (n = 76) | (n = 76) | (n = 76) | (n = 76) | (n = 76) | ||
| Age (yr) | 62.8 ± 12.7 | 60.9 ± 14.8 | 65.2 ± 11.2 | 63.7 ± 12.4 | 61.6 ± 12.9 | 62.4 ± 11.5 | 0.227 |
| Male | 206 (54) | 43 (57) | 40 (53) | 41 (54) | 44 (51) | 38 (50) | 0.877 |
| BMI (kg/m2) | 23.0 ± 4.1 | 23.7 ± 4.5 | 23.0 ± 3.8 | 23.2 ± 3.8 | 22.3 ± 4.2 | 23.1 ± 3.9 | 0.371 |
| ASA classification ≥ 3 | 75 (20) | 9 (12) | 19 (25) | 20 (26) | 13 (17) | 14 (18) | 0.146 |
| CR-POSSUM | 1.80 | 1.77 | 1.88 | 1.75 | 1.80 | 1.90 | 0.675 |
| Predicting mortality | (1.00-2.58) | (0.96-2.58) | (0.98-3.18) | (0.95-2.58) | (1.30-3.28) | (1.30-2.50) | |
| Hematocrit (%) | 36.8 ± 5.4 | 36.6 ± 5.5 | 36.1 ± 5.1 | 37.3 ± 5.5 | 37.4 ± 5.6 | 36.5 ± 5.3 | 0.548 |
| Cancer surgery | 347 (91) | 70 (92) | 68 (90) | 69 (91) | 71 (93) | 69 (91) | 0.930 |
| Rectal surgery | 165 (43) | 34 (45) | 30 (40) | 39 (38) | 40 (53) | 32 (42) | 0.397 |
| Stoma formation | 82 (22) | 19 (25) | 20 (26) | 13 (17) | 20 (26) | 10 (13) | 0.157 |
| Multi-organ Resection1 | 36 (10) | 9 (12) | 10 (13) | 5 (7) | 9 (12) | 3 (4) | 0.227 |
| Blood loss (mL) | 150 (73-300) | 200 (100-425) | 200 (100-400) | 150 (90-300) | 150 (55-385) | 140 (55-200) | 0.067 |
Prolonged hospitalization > 5 d occurred in 22.6% (n = 86), major postoperative complication was present in 2.9% (n = 11) and the rate of 30-d readmission was 2.4% (n = 9) - accounting for unsuccessful recovery of 25% (n = 95). Accordingly, the overall rate of optimal recovery in this ERAS program was 75%. The rate of optimal recovery significantly increased from 57.9% in 1st quintile to 72.4%-85.5% in the following quintiles (P < 0.001) (Figure 1). The average compliance with ERAS protocol gradually increased over the time - from 68.6% in the first quintile to 75.5% in the last quintile (P < 0.001) (Table 3). Regarding each individual element of our ERAS protocol, the compliance of 5 out of 17 ERAS elements have increased over the study period. These elements were preoperative detailed counseling, perioperative nutrition support, intraoperative goal-directed fluid therapy, intraoperative use of atraumatic O-ring wound protector and postoperative scheduled mobilization (Figure 2).
| Overall | 1st quintile | 2nd quintile | 3rd quintile | 4th quintile | 5th quintile | P value | |
| (n = 380) | (n = 76) | (n = 76) | (n = 76) | (n = 76) | (n = 76) | ||
| Time to resume normal diet (d) | 2 (1-3) | 2 (1-3) | 1 (0-2)a | 2 (0-2.8) | 2 (1-3) | 2 (1-2) | < 0.001a |
| Time to first bowel movement (d) | 3 (2-3) | 3 (2-3) | 3 (2-3) | 3 (2-3) | 2 (2-4) | 3 (2-3) | 0.848 |
| Overall complication | 83 (21.8) | 18 (23.7) | 20 (26.3) | 16 (21.1) | 18 (23.7) | 11 (14.5) | 0.457 |
| Major complication1 | 11 (2.9) | 1 (1.3) | 3 (3.9) | 2 (2.6) | 3 (3.9) | 2 (2.6) | 0.860 |
| Hospital stay (d) | 4 (4-5) | 5 (4-7)b | 4 (4-5) | 4 (4-5) | 5 (4-5.8) | 4 (3-5) | 0.015a |
| Hospital stay >5 d | 86 (22.6) | 31 (40.8)c | 12 (15.8) | 15 (18.4) | 19 (25.0) | 10 (13.2) | < 0.001a |
| 30-d readmission | 9 (2.4) | 1 (1.3) | 0 | 5 (6.6) | 2 (2.6) | 1 (1.3) | 0.077 |
| 30-d mortality | 1 (0.3) | 0 | 1 (1.3) | 0 | 0 | 0 | 0.405 |
| ERAS compliance % | 73.5 ± 11.8 | 68.6 ± 16d | 75.4 ± 11.1 | 73.7 ± 9.9 | 74.3 ± 10.2 | 75.5 ± 9.5 | < 0.001 a |
| Optimal recovery2 | 288 (75.0) | 44 (57.9)e | 64 (84.2) | 57 (75.0) | 55 (72.4) | 65 (85.5) | < 0.001 a |
An ERAS program is an integrated, evidence-based approach that fundamentally changes in perioperative care and surgical practice, and can therefore take time to achieve favorable outcomes. The introduction of ERAS in daily practice could be a learning-by-doing process relying on experiencing as a way for a multidisciplinary ERAS team to acquire skill and familiarize each ERAS element in order to get better surgical outcomes. The learning curve of ERAS implementation is somewhat different from that of a surgical intervention because an ERAS implementation requires both technical maneuvers and non-technical skills such as communication, collaboration and commitment from both patients and all members of multidisciplinary ERAS team.
The first step in determining the learning curve of ERAS program in colorectal surgery is the selection of an appropriate outcome measure. In this regard, we use a composite endpoint of three relevant clinical outcomes (no major postoperative complication, discharge by postoperative day 5, and no 30-d readmission) to determine an optimal recovery. These surgical outcomes have commonly been used as a proxy in the measurement of successful ERAS implementation in the literature[6,11,12]. Based on our prospectively collected database of colorectal surgery in a university hospital, this study demonstrated that a number of 76 colorectal operations are required for a multidisciplinary team to achieve a high rate of ERAS compliance and a high rate of optimal recovery following an open colorectal resection. It is worth noting that the 3rd quintile had the highest rate of 30-d readmission although it did not reach a statistical significance. There are several possible explanations on these findings such as the 3rd quintile had the highest percentage of patients with ASA classification ≥ 3. High ASA classification has been shown to be an independent predictor of readmission after major traumatic injury and general surgery[18,19].
It would appear that the implementation of ERAS program in open colorectal surgery may have a longer learning curve (i.e., more patients and a longer period of time) to achieve an optimal recovery than that in laparoscopic surgery. Pedziwiatr et al[6] showed that at least 30 patients over a period of 6 mo were required before their multidisciplinary team can effectively integrate an ERAS protocol into laparoscopic colorectal surgery. In this European study, there was a significant increase in some ERAS elements implemented over the study period such as no drains, use of epidural analgesia, early feeding and early ambulation. In the Alberta Heath Services Canada, Gramlich et al[20] reported that the active phase of ERAS implementation took 9-12 mo and recommended to use data on a baseline cohort of 50 patients in pre- and post-implementation period to define compliance with ERAS program. A possible explanation for a longer learning curve of successful ERAS implementation in open colorectal surgery is the fact that open surgery is associated with a higher systemic stress response and more surgical trauma than laparoscopic surgery[21,22]. Therefore, patients undergoing open surgery could have a higher rate of postoperative complication and are more difficulty to follow an ERAS protocol[9,23], especially for postoperative compliance with an ERAS protocol[12]. Although it may take more times to achieve a successful ERAS program in open colorectal surgery, a recent report from 15 academic hospitals in Canada has suggested that ERAS has more positive effect in patients undergoing open surgery than those with laparoscopic approach[12].
The introduction of the ERAS program required a closed collaboration and communication among surgical team members and other health care professionals as well as the continuous monitoring of its outcomes. Since not all elements could be introduced immediately, the ERAS compliance was lower than 70% in the early period of ERAS implementation in our institute. However, the rate of ERAS compliance significantly increased after our multidisciplinary ERAS team experienced the application of this program in 76 patients. A high ERAS compliance was then maintained thereafter at approximately 75%. Increasing ERAS compliance has been shown to be associated with a successful improved outcome including fewer complications, shorter hospital stay[4,5] and better oncological outcomes[24]. Two large European studies have suggested a cut-off point at 70% compliance with ERAS protocol to be correlated with a significant improvement in short-term and long-term outcomes following colorectal surgery[24,25]. It is arguable that full implementation of ERAS program may be not required to achieve better clinical outcomes.
Some components of our ERAS protocol encountered difficulties in their initial implementation, partly, due to the habit of conventional care and the lack of knowledge or instruments. Thanks to the cooperation of our multidisciplinary ERAS team and the support of hospital authorities, many components of our ERAS protocol increasingly implemented over the study period including preoperative detailed counseling, perioperative nutrition support, intraoperative goal-directed fluid therapy, intraoperative use of atraumatic O-ring wound protector and postoperative scheduled mobilization. A recent multi-center observational study in Ontario suggested that postoperative ERAS interventions had the greatest impact on optimal recovery after colorectal surgery[12].
This study has three major strengths. First, the data was extracted from a prospectively collected database of unselected patients undergoing open colectomy and/or proctectomy with an ERAS protocol. All patients were operated on and taken care of by the same surgeon and his multidisciplinary team thus resulting in minimizing bias. Second, to determine an optimal recovery, this study used a composite endpoint of three clinical outcomes (no major postoperative complication, discharge by postoperative day 5, and no 30-d readmission) which have commonly been used as a proxy in the measurement of successful ERAS implementation[6,11,12]. Third, this study provided detailed data on compliance with ERAS protocol and its individual elements.
The limitations of this study include the fact that it included only open colorectal operation. Whether the learning curve in this study is applicable to laparoscopic colorectal surgery or other intra-abdominal operations needs to be determined. Second, this study used only common clinical outcomes (i.e., major complication, hospital stay and readmission) as representatives for optimal recovery[6,11,12]. It did not assess any patient-reported outcomes such as time to return to normal activities and quality of life – which could be other important outcome measures for optimal recovery in the future study. Last, we acknowledged that there are several methods to quantify learning curve such as a simple linear regression and various curve fitting methods, a cumulative sum analysis and a chronological division of consecutive cases (data splitting method)[26] – each has its pros and cons. We used the latter design because it was evident that data splitting method can be used to identify a change over time even in case of case-mix complexity[27]. As a result, it was the most common method used to measure the learning curve effect in health technology[27]. However, the cut-off point of consecutive cases is arbitrary and information derived from the underlying learning curve may be limited.
This study showed that a number of 76 colorectal operations are required for a multidisciplinary team to achieve a significantly higher rate of optimal recovery and compliance with an ERAS protocol for open colorectal operation. These findings could call surgical communities to find the best ways to shorten the learning curve of ERAS program – especially in open laparotomy. It may include a structured program of education, training, cooperation and experience sharing between surgeons and non-surgical health care personals as an integrated ERAS team, or between a well-established ERAS center and a newly-implied ERAS hospital. The regular audition of relevant outcomes and closed collaboration between many different stakeholders, including patients and their family, are also required to achieve the best care and optimal recovery of surgical patients.
Enhanced recovery after surgery (ERAS) reduces hospitalization and complication following colorectal surgery. Whether the experience of multidisciplinary ERAS team affects patients’ outcomes is unknown especially for open colorectal surgery – which is known to be associated with higher rates of complication and more difficulty to implement an ERAS program than laparoscopic surgery.
The initial stage of ERAS application into surgical practice, i.e., learning curve, could be a crucial phase of this patient-centered perioperative pathway because the workflow of heath care personals needs to be adopted and the guideline has to assimilate into a daily practice.
This study aimed to evaluate and establish a learning curve of ERAS program for open colorectal surgery.
This was a review of prospectively collected database of 380 “unselected” patients undergoing elective “open” colectomy and/or proctectomy under ERAS protocol from 2011 (commencing ERAS application) to 2017 in a university hospital. Patients were divided into 5 chronological groups (76 cases per quintile). Surgical outcomes and ERAS compliance among quintiles were compared. Learning curves were calculated based on criteria of optimal recovery: defined as absence of major postoperative complications, discharge by postoperative day 5, and no 30-d readmission.
Hospitalization more than 5 d occurred in 22.6% (n = 86), major complication was present in 2.9% (n = 11) and 30-d readmission rate was 2.4% (n = 9) accounting for unsuccessful recovery of 25% (n = 95). Conversely, the overall rate of optimal recovery was 75%. The optimal recovery significantly increased from 57.9% in 1st quintile to 72.4%-85.5% in the following quintiles (P < 0.001). Average compliance with ERAS protocol gradually increased over the time - from 68.6% in 1st quintile to 75.5% in 5th quintile (P < 0.001). The application of preoperative counseling, nutrition support, goal-directed fluid therapy, O-ring wound protector and scheduled mobilization significantly increased over the study period.
A number of 76 colorectal operations are required for a multidisciplinary team to achieve a significantly higher rate of optimal recovery and high compliance with ERAS program for open colorectal surgery.
These findings could call surgical communities to find the best ways to shorten the learning curve of ERAS program – especially in open laparotomy. The barriers to the conduct, application and maintenance of ERAS program for colorectal surgery should be identified and solved systematically in order to achieve the best care and optimal recovery of surgical patients.
The author would like to thank Mr. Suthipol Udompunthurak from Clinical Epidemiology Unit, the Office for Research and Development, Faculty of Medicine Siriraj Hospital, for his kind assistance with statistical analysis.
Specialty type: Gastroenterology and hepatology
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Manuscript source: Invited manuscript
P-Reviewer: Kopljar M, Isik ARDA S-Editor: Ji FF L-Editor: A E-Editor: Zhang YL
| 1. | Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56:667-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 339] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 2. | Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol. 2014;20:13950-13955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 105] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Ljungqvist O, Scott M, Fearon KC. Enhanced Recovery After Surgery: A Review. JAMA Surg. 2017;152:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1487] [Cited by in RCA: 2183] [Article Influence: 272.9] [Reference Citation Analysis (0)] |
| 4. | Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J; Enhanced Recovery After Surgery Study Group. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146:571-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 570] [Cited by in RCA: 618] [Article Influence: 44.1] [Reference Citation Analysis (0)] |
| 5. | ERAS Compliance Group. The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg. 2015;261:1153-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 470] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 6. | Pędziwiatr M, Kisialeuski M, Wierdak M, Stanek M, Natkaniec M, Matłok M, Major P, Małczak P, Budzyński A. Early implementation of Enhanced Recovery After Surgery (ERAS®) protocol - Compliance improves outcomes: A prospective cohort study. Int J Surg. 2015;21:75-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 124] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 7. | Dobbins TA, Young JM, Solomon MJ. Uptake and outcomes of laparoscopically assisted resection for colon and rectal cancer in Australia: a population-based study. Dis Colon Rectum. 2014;57:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Lee MG, Chiu CC, Wang CC, Chang CN, Lee SH, Lee M, Hsu TC, Lee CC. Trends and Outcomes of Surgical Treatment for Colorectal Cancer between 2004 and 2012- an Analysis using National Inpatient Database. Sci Rep. 2017;7:2006. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015;29:3443-3453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 10. | Braga M, Borghi F, Scatizzi M, Missana G, Guicciardi MA, Bona S, Ficari F, Maspero M, Pecorelli N; PeriOperative Italian Society. Impact of laparoscopy on adherence to an enhanced recovery pathway and readiness for discharge in elective colorectal surgery: Results from the PeriOperative Italian Society registry. Surg Endosc. 2017;31:4393-4399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Pecorelli N, Hershorn O, Baldini G, Fiore JF, Stein BL, Liberman AS, Charlebois P, Carli F, Feldman LS. Impact of adherence to care pathway interventions on recovery following bowel resection within an established enhanced recovery program. Surg Endosc. 2017;31:1760-1771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 12. | Aarts MA, Rotstein OD, Pearsall EA, Victor JC, Okrainec A, McKenzie M, McCluskey SA, Conn LG, McLeod RS; iERAS group. Postoperative ERAS Interventions Have the Greatest Impact on Optimal Recovery: Experience With Implementation of ERAS Across Multiple Hospitals. Ann Surg. 2018;267:992-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 126] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 13. | Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1001] [Cited by in RCA: 1011] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 14. | Lohsiriwat V, Lohsiriwat D, Chinswangwatanakul V, Akaraviputh T, Lert-Akyamanee N. Comparison of short-term outcomes between laparoscopically-assisted vs. transverse-incision open right hemicolectomy for right-sided colon cancer: a retrospective study. World J Surg Oncol. 2007;5:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Lohsiriwat V, Lohsiriwat D, Boonnuch W, Chinswangwatanakul V, Akaraviputh T, Riansuwan W, Lert-akyamanee N. Outcomes of sphincter-saving operation for rectal cancer without protective stoma and pelvic drain, and risk factors for anastomotic leakage. Dig Surg. 2008;25:191-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, Windsor AC. Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg. 2004;91:1174-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 246] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 17. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24515] [Article Influence: 1167.4] [Reference Citation Analysis (0)] |
| 18. | Tran A, Mai T, El-Haddad J, Lampron J, Yelle JD, Pagliarello G, Matar M. Preinjury ASA score as an independent predictor of readmission after major traumatic injury. Trauma Surg Acute Care Open. 2017;2:e000128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Tevis SE, Weber SM, Kent KC, Kennedy GD. Nomogram to Predict Postoperative Readmission in Patients Who Undergo General Surgery. JAMA Surg. 2015;150:505-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Gramlich LM, Sheppard CE, Wasylak T, Gilmour LE, Ljungqvist O, Basualdo-Hammond C, Nelson G. Implementation of Enhanced Recovery After Surgery: a strategy to transform surgical care across a health system. Implement Sci. 2017;12:67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 104] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 21. | Delgado S, Lacy AM, Filella X, Castells A, García-Valdecasas JC, Pique JM, Momblán D, Visa J. Acute phase response in laparoscopic and open colectomy in colon cancer: randomized study. Dis Colon Rectum. 2001;44:638-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 131] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Veenhof AA, Vlug MS, van der Pas MH, Sietses C, van der Peet DL, de Lange-de Klerk ES, Bonjer HJ, Bemelman WA, Cuesta MA. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care: a randomized trial. Ann Surg. 2012;255:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 246] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 23. | Zhuang CL, Huang DD, Chen FF, Zhou CJ, Zheng BS, Chen BC, Shen X, Yu Z. Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2015;29:2091-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Gustafsson UO, Oppelstrup H, Thorell A, Nygren J, Ljungqvist O. Adherence to the ERAS protocol is Associated with 5-Year Survival After Colorectal Cancer Surgery: A Retrospective Cohort Study. World J Surg. 2016;40:1741-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 255] [Article Influence: 31.9] [Reference Citation Analysis (0)] |
| 25. | Pisarska M, Pędziwiatr M, Małczak P, Major P, Ochenduszko S, Zub-Pokrowiecka A, Kulawik J, Budzyński A. Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. Int J Surg. 2016;36:377-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 26. | Khan N, Abboudi H, Khan MS, Dasgupta P, Ahmed K. Measuring the surgical 'learning curve': methods, variables and competency. BJU Int. 2014;113:504-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 27. | Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT. Statistical assessment of the learning curves of health technologies. Health Technol Assess. 2001;5:1-79. [PubMed] |