Published online Feb 27, 2019. doi: 10.4240/wjgs.v11.i2.93
Peer-review started: February 11, 2019
First decision: February 19, 2019
Revised: February 23, 2019
Accepted: February 24, 2019
Article in press: February 25, 2019
Published online: February 27, 2019
Processing time: 17 Days and 21 Hours
Single loop reconstruction (SLR) was routine in our institution for patients undergoing pancreatico-duodenectomy (PD). Roux-en Y reconstruction with an isolated gastric limb (RIGL) recently became the reconstruction of choice.
To evaluate the impact of RIGL on incidence and severity of delayed gastric emptying (DGE).
This is a single institution, retrospective analysis of patients undergoing PD. All patients undergoing PD from July 2010 through December 2016 were included in the study. Outcome of RIGL were compared to SLR. Primary measure of outcome included incidence and severity of DGE. Secondary measures of outcome were overall complications and postoperative mortality.
One hundred and seventy-nine patients were included in the study. Fifty-two had RIGL, 127 had SLR. Overall complication rate was 40.2%, patients in the RIGL group experienced lower rates of DGE (15.4% vs 59.1%, P = 0.001). Other patient related outcomes were also significantly reduced: day of nasogastric tube removal (3 vs 5, P < 0.001), regain of normal diet (8 vs 9, P < 0.001). On multivariate analysis RIGL was associated independently with reduced rates of DGE (P < 0.001, OR 0.14)
The current study shows that RIGL reduces the rate of DGE after PD. Further prospective randomized controlled trials are required to affirm the current data.
Core tip: This single institution retrospective analysis showed that patients undergoing pancreatico-duodenectomy with reconstruction in a roux en Y with isolated gastric limb fashion have significantly reduced rates of delayed gastric emptying with no change in operative postoperative and oncological outcome. This type of reconstruction may improve patient’s quality of life and reduces patient's related costs.
- Citation: Ben-Ishay O, Zhaya RA, Kluger Y. Dual loop (Roux en Y) reconstruction with isolated gastric limb reduces delayed gastric emptying after pancreatico-duodenectomy. World J Gastrointest Surg 2019; 11(2): 93-100
- URL: https://www.wjgnet.com/1948-9366/full/v11/i2/93.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i2.93
Pancreatico-duodenectomy (PD) is a procedure used for various peri-ampullary pathologies. Although practiced for many years, the procedure is still fraught with significant morbidity and mortality. Mortality was significantly reduced over the years where’s morbidity still peaks at 40%-50%[1-3]. Complications specifically related to the procedure include postoperative pancreatic fistula (POPF), hemorrhage, abscess, biliary and intestinal leaks. Delayed gastric emptying (DGE) is common amongst patients undergoing PD. The presumed etiology for this complication is neurological[4,5] or hormonal in origin[6-8]. Definite explanation for the high rates of DGE though in this cohort of patients is still lacking and appears to be multifactorial. DGE prolongs the hospital stay, increases the associated morbidity, compromise patient’s quality of life and increase patient’s related costs.
The impact of the type of intestinal reconstruction and its association with DGE in PD was previously studied. Studies demonstrated that ante colic reconstruction is preferred over a retro colic in single loop reconstruction (SLR) leading to reduced rates of DGE[9]. Isolated pancreatic limb was also studied with conflicting results in terms of DGE and POPF.
In the past the Roux en y with isolated gastric limb (RIGL) was used sporadically in our institution especially in young patients with benign or potentially benign disease while in others, reconstruction was fashioned in a classic single loop. We observed that RIGL had a lower incidence of DGE and better overall surgical outcome. Therefore, at the beginning of 2016 we started to reconstruct all our patients who underwent PD with a RIGL technique. The purpose of the current study is to evaluate the effects of the newly used technique on the incidence and severity of DGE in this unique cohort of patients.
Following the dissection and resection phases of the procedure a Roux en Y reconstruction with an isolated gastric limb is fashioned. The proximal jejunal loop is brought in a retrocolic (transmesocolic) fashion right to the middle colic vessels. Pancreatico-jejunal anastomosis (PJA) is performed followed by end to side hepatico jejunosmy. The bowel is then divided 35-40 cm from the biliary anastomosis by a Gastrointestinal linear cutter.
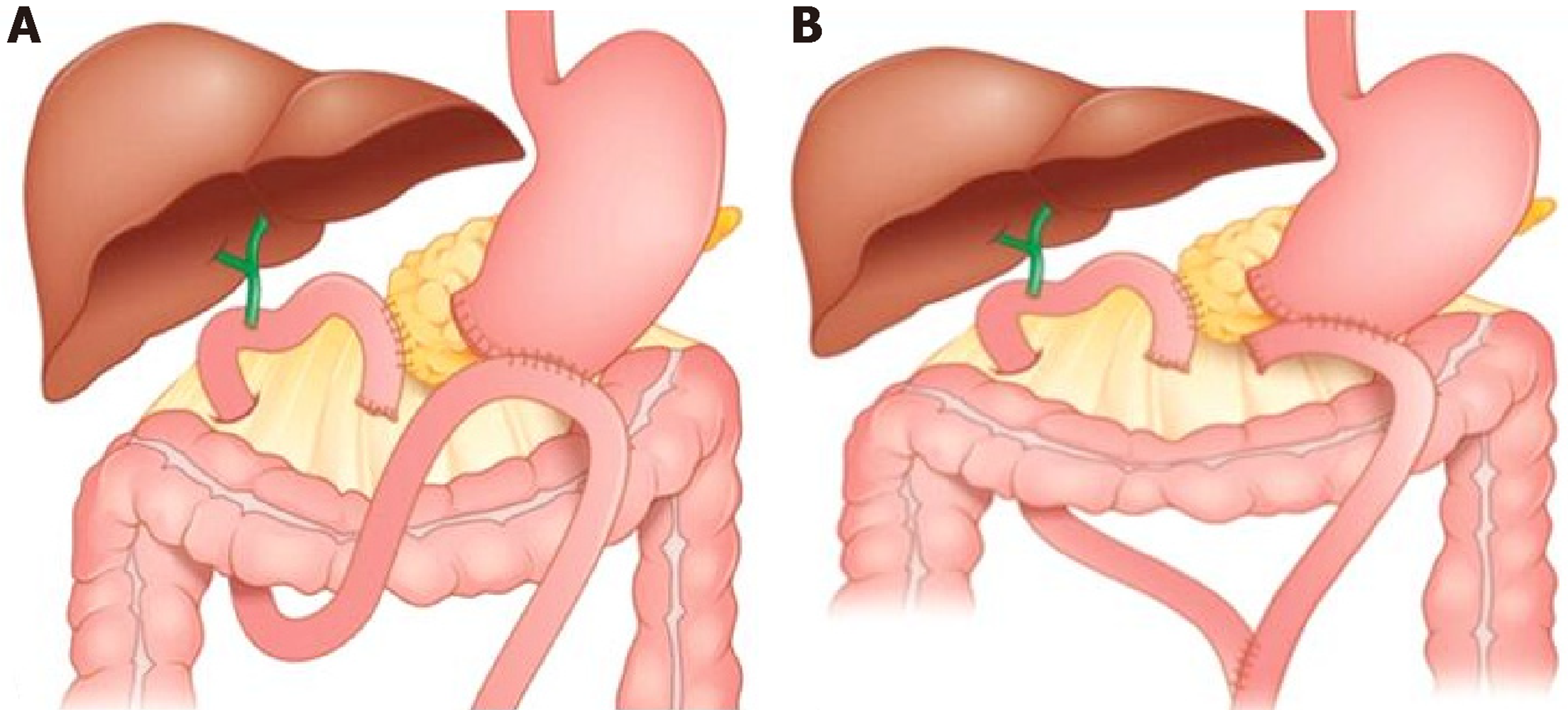
The distal jejunal end is brought in an antecolic fashion towards the stomach and a gastro-jejunal anastomosis is than performed with either side to side hand sawn anastomosis in a two layers fashion to the anterior wall of the stomach or with a circular stapler (Covidien EEATM, 28-3.5 mm circular stapler with DST seriesTM technology) to the posterior wall of the stomach. A Jejuno-Jejunal anastomosis is than performed between the biliopancreatic limb and the alimentary limb. Figure 1 depicts the differences between the traditional SLR (Figure 1A) and the RIGL technique (Figure 1B).
Postoperatively, patients are admitted to a step-down unit or to an ICU, based on their medical comorbidities and clinical condition. Post operative NG tube policy was changed over time and now is typically removed on postoperative day 1 or 2 unless the output is more than 500 mL/d, diet than is slowly advanced. All patients have a drain placed intraoperatively; it is removed when the patient is tolerating a full diet and drain volume is less than 100 mL/d. The decision to start supplemental nutrition is made case per case, depending on patients’ underlying nutritional status and severity of DGE. A CT scan of the abdomen and pelvis is obtained for patients with DGE who demonstrate clinical evidence of Grade B or C POPF or infection, in order to rule out abdominal fluid collections that might be responsible for DGE. Patients are discharged home when tolerating full diet, and are in no need for advanced analgesia.
We retrospectively reviewed the electronic charts of all patients undergoing PD for any pathology in the division of general surgery at the RHCC, Haifa, Israel. All patients undergoing PD from July 2010 through December 2016 were included in the study. Data collected included demographic, clinical, operative and postoperative data. Patients undergoing RIGL reconstruction were compared with those reconstructed in an SLR technique. We have postulated that RIGL reduces the incidence and severity of DGE, and although has one more jejunal anastomosis it is feasible, safe and does not increase the rate of overall complications. Therefor the Primary measure of outcome was incidence and severity of DGE. Secondary measures of outcome included overall complication rate and postoperative mortality. We defined DGE according to the international study group of pancreatic surgery (ISGPS)[10].
Continuous parametric variables were analyzed using the Student’s t-test. The Mann-Whitney U test was used to analyze non-parametric variables. Chi-square test was applied to analyze the association between frequencies in a Univariate fashion. Multivariate analysis was performed using a stepwise logistic regression model and a likelihood ratio test was applied to identify positive associations with the primary and secondary measure of outcome. JMP Pro for Mac (Version 13.0.0) was used to analyze the data. P < 0.05 (2-sided) was considered to indicate statistical significance.
During the time frame of the study 52 patients underwent PD with RIGL reconstruction and 127 patients underwent PD with a SLR. The most common indication for PD was ductal adenocarcinoma (63.7%) followed by intraductal papillary mucinous neoplasms (19.5%), other pancreatic cystic lesions (8.9%) and Neuroendocrine tumors in 4.4%. Both study and control groups were homogeneous in terms of demographic variables and clinical presentation (Table 1). Of the 114 patients with ductal adenocarcinoma, 5.3% (n = 6) were operated following neo-adjuvant chemotherapy. There was no significant difference in operative time between the study and the control group respectively (221.3 ± 39.7 min vs 221.3 ± 40.1 min, P = 0.99) and the need for intraoperative blood transfusion (5.8% vs 10.3%, P = 0.3). In patients undergoing PD for malignancy, RIGL did not cause any oncological compromise with the same rate of positive distal or radial margins (5.7% vs 2.4%, P = 0.58), and no change in average number of lymph nodes procured between the two groups respectively (16.5 ± 6.1 vs 16.1 ± 6.2, P = 0.76). Overall complication rate in the study group was 36.5% vs 41.7% in the control group (P = 0.52) (Table 2). The rate of DGE was significantly lower in the study group (15.4% vs 59.1%, P < 0.001), with no change in rates of POPF formation, intra-abdominal abscesses, and postoperative mortality. These differences remained significant also in subgroup anlaysis of the different grades of DGE (A-C) (Table 2) Furthermore, patients in the study group had significant improvement in all patients related outcome such as earlier extraction of the nasogastric tube, emesis following its extraction, therefor they returned earlier to normal diet and had a shorter stay in the hospital (Table 3). Univariate analysis was used to identify factors associated with development of DGE. SLR, female gender, and postoperative complications were significantly associated with DGE (Table 4). Known factors such as gender, malignancy, POPF, Bilirubin levels, and the Roux en Y reconstruction were inserted into a logistic regression model for multivariate analysis using a likelihood ratio test. SLR and postoperative complications were the only factors independently associated with the development DGE (Table 4).
| RIGL, n = 52 | SLR, n = 127 | P value | |
| Age | 68.2 ± 9.6 | 68 ± 13.7 | 0.93 |
| Gender (male) | 50 (n = 26) | 48.8 (n = 62) | 0.89 |
| Risk factors | |||
| Smoking | 48.7 (n = 19) | 35.8 (n = 44) | 0.15 |
| Diabetes | 32.6 (n = 17) | 39.4 (n = 50) | 0.4 |
| Chronic pancreatitis | 9.6 (n = 5) | 9.5 (n = 12) | 0.3 |
| Alcohol abuse | 8.8 (n = 3) | 5.8 (n = 7) | 0.5 |
| Clinical presentation | |||
| Weight loss | 40.4 (n = 21) | 55.6 (n = 70) | 0.06 |
| Abdominal pain | 61.5 (n = 32) | 66.7 (n = 84) | 0.51 |
| Nausea | 23.1 (n = 12) | 23 (n = 29) | 0.99 |
| Emesis | 15.4 (n = 8) | 13.5 (n = 17) | 0.74 |
| Jaundice | 42.3 (n = 22) | 51.6 (n = 65) | 0.26 |
| RIGL, n = 52 | SLR, n = 127 | P value | |
| Overall complications | 36.5 (n = 19) | 41.7 (n = 53) | 0.52 |
| Superficial SSI | 23.1 (n = 12) | 21.3 (n = 27) | 0.8 |
| Deep SSI | 3.2 (n = 4) | 1.9 (n = 1) | 0.65 |
| Abscess | 15.4 (n = 8) | 11 (n = 14) | 0.42 |
| POPF | 28.9 (n = 15) | 29.1 (n = 37) | 0.96 |
| Intestinal leak | 3.9 (n = 2) | 0 (n = 0) | 0.03 |
| Bile leak | 17.3 (n = 9) | 20.5 (n = 26) | 0.62 |
| Phlebitis | 5.8 (n = 3) | 17.3 (n = 22) | 0.04 |
| Pneumonia | 7.7 (n = 4) | 17.3 (n = 22) | 0.09 |
| Pulmonary embolism | 0 (n = 0) | 1.6 (n = 2) | 0.53 |
| DVT | 0 (n = 0) | 0.8 (n = 1) | 0.52 |
| PVT | 5.8 (n = 3) | 3.2 (n = 4) | 0.41 |
| CV | 9.6 (n = 5) | 12.6 (n = 16) | 0.57 |
| UTI | 7.7 (n = 4) | 15 (n = 19) | 0.18 |
| Delayed gastric emptying | 15.4 (n = 8) | 59.1 (n = 75) | < 0.001 |
| Grade A | 13.5 (n = 7) | 44.9 (n = 57) | < 0.001 |
| Grade B | 1.9 (n = 1) | 11.8 (n = 15) | < 0.001 |
| Grade C | 0 | 2.4 (n = 3) | NR |
| Postoperative Mortality | 3.9 (n = 2) | 5.5 (n = 7) | 0.64 |
| RIGL, n = 52 | SLR, n = 127 | P value | |
| Day of NG tube extraction (d) (median) | 3 (3-4) | 5 (4-6) | < 0.001 |
| Length of hospital stay (d) (median) | 10 (8-14) | 12 (10-18) | 0.005 |
| Emesis After feeding tube extraction | 0 (n = 0) | 19.7 (n = 25) | < 0.001 |
| Need for returning of NG tube | 1.9 (n = 1) | 24.4 (n = 31) | < 0.001 |
| Day of return to normal diet (d) (median) | 8 (6-9) | 9 (8-15) | < 0.001 |
| DGE, n = 83 | No DGE, n = 96 | Univariate P value | Multivariate P value | |
| Age | 67.3 ± 14.5 | 68.8 ± 10.8 | 0.4 | |
| Gender (female) | 59 (n = 49) | 43.8 (n = 42) | 0.04 | 0.03 |
| BMI | 26.8 ± 4.8 | 26.1 ± 5 | 0.39 | |
| RIGL (yes) | 9.6 (n = 8) | 45.8 (n = 44) | 0.001 | < 0.001 |
| Chronic pancreatitis | 8.4 (n = 7) | 10.4 (n = 10) | 0.58 | |
| Alcohol abuse | 3.9 (n = 3) | 9 (n = 7) | 0.19 | |
| Pre-existent DM | 38.5 (n = 32) | 36.5 (n = 35) | 0.77 | |
| Jaundice | 53.7 (n = 44) | 44.8 (n = 43) | 0.24 | |
| Bilirubin total (mg/dL) (median) | 1.1 (0.4-4.5) | 0.8 (0.4-5.5) | 0.84 | |
| Malignancy | 78.3 (n = 65) | 74 (n = 71) | 0.5 | 0.88 |
| Overall complications | 49.4 (n = 41) | 32.3 (n = 31) | 0.019 | 0.04 |
| Pancreatic leak | 26.5 (n = 22) | 31.3 (n = 30) | 0.48 | 0.5 |
| Bile leak | 22.9 (n = 19) | 16.7 (n = 16) | 0.29 | |
| Pneumonia | 20.5 (n = 17) | 9.4 (n = 9) | 0.03 | 0.18 |
| Length of hospital stay (d) (median) | 14 (11-22) | 10 (8-14) | < 0.001 | |
| Postoperative mortality | 4.8 (n = 4) | 5.2 (n = 5) | 0.9 |
DGE is a common hurdle after PD. It’s incidence range between 19%-57%[9]. DGE is defined as the intolerance of standard diet on the 8th post-operative day. Three different grades (A-C) are defined based on the impact on the clinical course and the post-operative management[10].
The type of intestinal reconstruction and its effect on rates of DGE was previously evaluated. Several studies showed that in SLR antecolic reconstruction is preferred over a retrocolic in reducing the rates of DGE[9]. Klaiber et al[11] in a recent meta-analysis compared the classic SLR with a Roux en Y reconstruction using an isolated pancreatic limb. The authors concluded that this reconstruction did not reduce the rates of DGE or the rates of POPF. Deng et al[12] further evaluated these results, in a second meta-analysis replicating the results of their peers.
In our study the overall incidence of DGE was 46.4% (n = 83). The study group showed lower rates of DGE in all the subgroups (A-C) (Table 3) with an overall rate of 15.4% (P < 0.001). The relatively high incidence of DGE in the control group (59.1%) is attributed in our opinion to the strict adherence to the ISGPS definitions and the time frame of study. Patients in the control group were operated in times were the NG tube was left in place for 3-4 d routinely. Subgroup analysis though, shows that the vast majority of these patients presented with grade A DGE, with minimal to no effect on the clinical outcome. The relatively short hospital length of stay of the control group (12 d) further reiterates this assumption. The study group on the other hand shows very low rates of grade B and C DGE (1.9% and 0% vs 11.8% and 2.4% P < 0.001 respectively). We believe that this type of reconstruction reduces the high grade DGE with its associated morbidity.
The type of reconstruction continues to be of great interest to surgeons around the world, Barakat et al[13] described in 2016 an isolated proximal gastro-jejunal anastomosis with pyloric ring resection compared with a traditional SLR. Overall rates of DGE were 10.2% and 57% in the study and the control group respectively, with a significant reduction in the clinically relevant (grade B and C) DGE. These results are similar to the results of our study, with a technique that is quite demanding relatively to the one described in our cohort of patients.
Khan et al[14] described a modification to the traditional SLR technique using a flange gastro-enterostomy. In this technique the gastro-enterostomy is performed in an infra-mesocolic fashion through a hole in the mesocolon left to the middle colic vessels. The authors described an overall DGE incidence of 9% and 23% in the flange and non-flange technique respectively with a prominent reduction in the clinically relevant DGE.
Numerous studies evaluated the risk factors for the development of DGE. Qu et al[9] in a meta-analysis studied factors associated with increased risk for DGE. Gender, malignancy, pre-existent diabetes mellitus, preoperative biliary drainage, pre-operative jaundice, antecolic vs reterocolic reconstruction, pylorus preserving procedure, POPF, postoperative complications and early enteral feeding were studied. The authors concluded that postoperative complications, pre-existent diabetes mellitus and POPF are the only factors significantly and independently associated with DGE.
In our cohort of patients univariate analysis identified female gender, SLR, overall complications and post-operative pneumonia to be associated with DGE. On multivariate analysis the RIGL was independently associated with low rates of DGE, while female gender and overall complications were independently associated with high rates of DGE.
Whereas primary DGE is presumably caused by disruption of the neuro-hormonal pathway, several studies have shown that intra-abdominal complications may cause angulation of the gastrojejunostomy and this is a possible cause of secondary DGE. A lower incidence of DGE was also observed in procedures that allowed for the straight passage of the gastric content under gravity into the jejunum. We believe that RIGL technique may bring both advantages, reduce the chances for torsion or angulation cancelling the omega produced by the SLR on one hand, and allow straight passage of the gastric content due to the antecolic fashion of the anastomosis. Furthermore, in RIGL the stomach is not exposed to the pancreatic-biliary secretions and this may also cause reduction in rates of DGE, but currently there is no evidence to support this assessment. The results of Barakat et al[13] who performed a proximal isolated gastric limb might support this assumption. Apparently the use of proximal or distal loop of jejunum has the same results, although we believe that the RIGL is less demanding technically. In addition the isolated gastric limb permits patients who experience pancreatic or biliary leak to resume normal diet earlier with good results.
The limitation of the current study is its retrospective nature. Some of the patients of the control group were operated at times when NG tube was removed routinely in day 3-4 after surgery. This might compromise our results in part, but the significant differences in high grade DGE (B-C) suggest that the results are valid. There is no doubt that only a prospective randomized control trial is of benefit at this point.
In conclusion, the current study show that dual loop reconstruction with isolate gastric limb cause significant decrease in rates of DGE, particularly in the rates of severe DGE (grade B and C) and other patient's related outcome. Furthermore, we demonstrated that this type of reconstruction does not increase the overall complications rate and has no negative impact on the oncological outcome of this unique cohort of patients.
Single loop reconstruction was routine in our institution for patients undergoing pancreatico-duodenectomy (PD).
Roux-en Y reconstruction with an isolated gastric limb (RIGL) recently became the reconstruction of choice.
The current study evaluates the impact of RIGL on incidence and severity of delayed gastric emptying (DGE).
Retrospective analysis of patients undergoing PD.
On multivariate analysis RIGL was associated independently with reduced rates of DGE.
The current study shows that RIGL reduces the rate of DGE after PD.
Further prospective randomized controlled trials are required to affirm the current data.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Israel
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P- Reviewer: Chiba T, Jin C, Lieto E, Nakano H, Pagano CE, Solaini L S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Wagner M, Redaelli C, Lietz M, Seiler CA, Friess H, Büchler MW. Curative resection is the single most important factor determining outcome in patients with pancreatic adenocarcinoma. Br J Surg. 2004;91:586-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 618] [Cited by in RCA: 716] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 2. | Schnelldorfer T, Ware AL, Sarr MG, Smyrk TC, Zhang L, Qin R, Gullerud RE, Donohue JH, Nagorney DM, Farnell MB. Long-term survival after pancreatoduodenectomy for pancreatic adenocarcinoma: is cure possible? Ann Surg. 2008;247:456-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 377] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 3. | Hartwig W, Werner J, Jäger D, Debus J, Büchler MW. Improvement of surgical results for pancreatic cancer. Lancet Oncol. 2013;14:e476-e485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 277] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 4. | Tanaka A, Ueno T, Oka M, Suzuki T. Effect of denervation of the pylorus and transection of the duodenum on acetaminophen absorption in rats; possible mechanism for early delayed gastric emptying after pylorus preserving pancreatoduodenectomy. Tohoku J Exp Med. 2000;192:239-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Itani KM, Coleman RE, Meyers WC, Akwari OE. Pylorus-preserving pancreatoduodenectomy. A clinical and physiologic appraisal. Ann Surg. 1986;204:655-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 122] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Fox JE, Daniel EE, Jury J, Robotham H. The mechanism of motilin excitation of the canine small intestine. Life Sci. 1984;34:1001-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Naritomi G, Tanaka M, Matsunaga H, Yokohata K, Ogawa Y, Chijiiwa K, Yamaguchi K. Pancreatic head resection with and without preservation of the duodenum: different postoperative gastric motility. Surgery. 1996;120:831-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Tanaka M, Sarr MG. Total duodenectomy: effect on canine gastrointestinal motility. J Surg Res. 1987;42:483-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Qu H, Sun GR, Zhou SQ, He QS. Clinical risk factors of delayed gastric emptying in patients after pancreaticoduodenectomy: a systematic review and meta-analysis. Eur J Surg Oncol. 2013;39:213-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1771] [Cited by in RCA: 2327] [Article Influence: 129.3] [Reference Citation Analysis (0)] |
| 11. | Klaiber U, Probst P, Knebel P, Contin P, Diener MK, Büchler MW, Hackert T. Meta-analysis of complication rates for single-loop versus dual-loop (Roux-en-Y) with isolated pancreaticojejunostomy reconstruction after pancreaticoduodenectomy. Br J Surg. 2015;102:331-340. [PubMed] [DOI] [Full Text] |
| 12. | Deng LH, Xiong JJ, Xia Q. Isolated Roux-en-Y pancreaticojejunostomy versus conventional pancreaticojejunostomy after pancreaticoduodenectomy: a systematic review and meta-analysis. J Evid Based Med. 2017;10:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Barakat O, Cagigas MN, Bozorgui S, Ozaki CF, Wood RP. Proximal Roux-en-y Gastrojejunal Anastomosis with Pyloric Ring Resection Improves Gastric Emptying After Pancreaticoduodenectomy. J Gastrointest Surg. 2016;20:914-923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Khan AS, Williams G, Woolsey C, Liu J, Fields RC, Doyle MMB, Hawkins WG, Strasberg SM. Flange Gastroenterostomy Results in Reduction in Delayed Gastric Emptying after Standard Pancreaticoduodenectomy: A Prospective Cohort Study. J Am Coll Surg. 2017;225:498-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |