Published online Feb 27, 2019. doi: 10.4240/wjgs.v11.i2.41
Peer-review started: February 11, 2019
First decision: February 19, 2019
Revised: February 20, 2019
Accepted: February 21, 2019
Article in press: February 22, 2019
Published online: February 27, 2019
Processing time: 22 Days and 23.5 Hours
Enhanced recovery after surgery (ERAS), a multidisciplinary program designed to minimize stress response to surgery and promote the recovery of organ function, has become a standard of perioperative care for elective colorectal surgery. In an elective setting, ERAS program has consistently been shown to decrease postoperative complication, reduce length of hospital stay, shorten convalescence, and lower healthcare cost. Recently, there is emerging evidence that ERAS program can be safely and effectively applied to patients with emergency colorectal conditions such as acute colonic obstruction and intraabdominal infection. This review comprehensively covers the concept and application of ERAS program for emergency colorectal surgery. The outcomes of ERAS program for this emergency surgery are summarized as follows: (1) The ERAS program was associated with a lower rate of overall complication and shorter length of hospital stay – without increased risks of readmission, reoperation and death after emergency colorectal surgery; and (2) Compliance with an ERAS program in emergency setting appeared to be lower than that in an elective basis. Moreover, scientific evidence of each ERAS item used in emergency colorectal operation is shown. Perspectives of ERAS pathway in emergency colorectal surgery are addressed. Finally, evidence-based ERAS protocol for emergency colorectal surgery is presented.
Core tip: This review comprehensively covers the concept and application of enhanced recovery after surgery (ERAS) program for emergency colorectal surgery. It was evident that ERAS program was associated with a lower rate of overall complication and shorter hospitalization – without increased risks of readmission, reoperation and death after emergency colorectal surgery. However, compliance with an ERAS program in emergency setting appeared to be lower than that in an elective basis. Scientific evidence of each ERAS item and perspectives of ERAS pathway in emergency colorectal surgery are addressed. Evidence-based ERAS protocol in this emergency setting is presented at the end of article.
- Citation: Lohsiriwat V, Jitmungngan R. Enhanced recovery after surgery in emergency colorectal surgery: Review of literature and current practices. World J Gastrointest Surg 2019; 11(2): 41-52
- URL: https://www.wjgnet.com/1948-9366/full/v11/i2/41.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i2.41
The application of an enhanced recovery after surgery (ERAS) program for “elective” colorectal surgery has consistently been shown to decrease postoperative complication, shorten length of hospital stay, facilitate patient recovery, shorten convalescence, and lower healthcare cost[1,2]. High adherence to ERAS program was also associated with better short-term and long-term outcomes including improved disease-free survival and overall survival in patients with resectable colorectal cancer[3]. In an elective setting, ERAS program for colorectal surgery is well established as noted in the recommended guidelines for perioperative care in elective colonic and rectal surgery from the ERAS Society in 2013[4,5], and the American Society of Colon and Rectal Surgeons and the Society of American Gastrointestinal and Endoscopic Surgeons in 2017[6].
However, in daily practice it is estimated that up to 30% of colorectal operations are related to emergency conditions[7] such as acute colonic obstruction, perforated colonic diverticulitis, fulminant colitis, massive lower gastrointestinal hemorrhage, and traumatic injuries to colon and rectum. It appears that patients having emergency colorectal conditions could be high-risk individuals and undergo more complex operations such as multi-visceral resection for obstructed colorectal cancer[8]. As a result, several investigators have shown that patients undergoing emergency colorectal surgery had longer hospitalization and higher rates of morbidity and mortality than those in an elective setting[7,9]. Since there is strong evidence that ERAS program reduced postoperative complication and length of hospital stay in elective colorectal surgery[1], this raises a question whether an ERAS program can be applicable and beneficial to patients having emergency colorectal surgery.
As far as we are aware, there is little information regarding the feasibility and benefit of ERAS program for emergency colorectal surgery[8,10-14]. Part of the problem may be related to the lack of ERAS guideline for emergency colorectal surgery and a difficulty in studying patients with emergency colorectal conditions. Accordingly, this article aimed to review the current evidence about ERAS in emergency colorectal surgery and its outcomes - mainly based on the studies of acutely obstructed colorectal cancer, not perforated hollow viscus and intraabdominal sepsis. Application of each ERAS item in emergency colorectal surgery and its evidence is discussed. Perspectives of ERAS pathway in emergency colorectal surgery are addressed. Finally, evidence-based ERAS protocol for emergency colorectal surgery is presented at the end of article.
Studies were identified by performing a literature search of two online databases (MEDLINE through PubMed and the SCOPUS) with the last search performed in October 2018. The PubMed search strategy was constructed by using the following key words: Enhanced recovery after surgery OR enhanced recovery pathway OR enhanced recovery program OR fast-track surgery, emergency OR emergencies, urgent OR urgency, surgery OR operation, colon, rectum, obstruction, bleeding, perforation, and intraabdominal infection OR intraabdominal sepsis OR peritonitis. Only publications in the English language were included. The search of SCOPUS was conducted using similar search terms. Manual search for other potentially relevant articles that may have been missed on the initial search strategy was performed by reviewing the reference list of all included studies.
After an extensive and systematic review based on the aforementioned searching strategies, we found two settings of ERAS studies on emergency colorectal surgery: A comparison between ERAS program and conventional care in emergency colorectal operations (4 original articles) and a comparison of ERAS outcomes following colorectal surgery between emergency basis and elective setting (2 original articles).
There were four cohort studies comparing ERAS program to conventional care in emergency colorectal surgery[8,10-12]. Three of them[8,11,12] focused on ERAS program in obstructing colorectal cancer, whereas the other[10] covered various emergency abdominal surgeries including colorectal resection for acute colorectal manifestations. All studies used a “modified” ERAS protocol in their institutes (Table 1).
| ERAS elements | Lohsiriwat[8] | Wisely et al[10] | Shida et al[11] | Shang et al[12] |
| Preoperative phase | ||||
| Education and detailed counseling | Y | Y | Y | Y |
| Medical optimization | Y | |||
| No bowel preparation | Y | Y | Y | Y |
| No pre-anesthetic medication | Y | Y | Y | Y |
| Intraoperative phase | ||||
| Use of epidural analgesia | Y | Y | ||
| Active warming | Y | Y | Y | |
| Avoid sodium/fluid overload | Y | Y | Y | Y |
| Prophylaxis of nausea and vomiting | Y | Y | Y | |
| No intraabdominal drainage | Y | Y | ||
| Postoperative phase | ||||
| Opioid-sparing multimodal analgesia | Y | Y | Y | Y |
| Early removal of nasogastric tube | Y | Y | Y | Y |
| Early feeding | Y | Y | Y | Y |
| Early removal of urinary catheter | Y | Y | Y | Y |
| Use of laxatives | Y | Y | Y | |
| Early mobilization | Y | Y | Y | Y |
The first publication, by Lohsiriwat[8] in 2014, was a matched case-control study of patients undergoing colectomy or proctectomy for acutely obstructed colorectal cancer in a university hospital in Thailand. Twenty patients in ERAS group were matched to 40 patients in non-ERAS group for age, co-morbidities, duration of obstruction, tumor location and type of surgical procedure. The author showed that the ERAS group had a significantly 2-d shorter median length of hospital stay (5.5 d vs 7.5 d) and a non-significantly lower rate of postoperative complication (25% vs 48%). Time to gastrointestinal recovery was also significantly shorter in the ERAS group. Regarding the outcomes of post-discharge follow-up, time interval between surgery and the initiation of adjuvant chemotherapy was significantly shorter in the ERAS group (median 37 d vs 49 d).
The next study, by Wisely et al[10] from Australia in 2016, was a retrospective review examining clinical outcomes of patients undergoing emergency laparotomy for various diseases of the lower gastrointestinal tract prior to and after the implementation of ERAS program. From a total number of 370 patients, 177 had colon or rectal resection (pre-ERAS n = 80 vs post-ERAS n = 97). Based on their study of small bowel and colorectal surgery as well as resection and non-resection procedures, they found a significant reduction in the rates of postoperative complication including urinary tract infection and pulmonary infection in the post-ERAS period. There was no difference in inpatient mortality, reoperation, readmission and length of hospital stay between both time frames.
Another study, by Shida et al[11] in 2017, compared clinical outcomes between the first set of 42 non-ERAS patients and the latter 80 ERAS patients undergoing colorectal resection for obstructive cancer in a general hospital in Tokyo. Similar to Lohsiriwat’s study[8], patients with concomitant bowel perforation were excluded in this study. The authors demonstrated a 3-d reduction in the median length of hospital stay in ERAS group, but a comparable rate of postoperative complication and 30-d readmission.
The latest study, published by Shang et al[12] in 2018, was a multicenter study from China. During the study period of 8 years, 839 consecutive patients with acutely obstructed colorectal cancer underwent emergency resection in 4 hospitals. After propensity score matching analysis between ERAS and traditional perioperative care, there were 318 patients in each group. The ERAS group had significantly faster gastrointestinal recovery, fewer complications (34% vs 45%), shorter median length of hospital stay (6 d vs 9 d) and shorter interval from surgery to adjuvant chemotherapy (36 d vs 48 d).
Although the methods of ERAS intervention and the number of ERAS items applied in the aforementioned studies may be various[8,10-12], it appears that an ERAS program can safely be applicable to emergency colorectal surgery with similar beneficial effects of that shown in an elective setting such as a reduction in postoperative complication and length of hospitalization – without a significant difference in 30-d mortality and readmission rate. Study characteristics and clinical outcomes of the four published trials comparing ERAS vs non-ERAS in emergency colorectal surgery are summarized in Table 2.
| Lohsiriwat[8] | Wisely et al[10] | Shida et al[11] | Shang et al[12] | |
| Characteristics | ||||
| Country, year | Thailand, 2014 | Australia, 2016 | Japan, 2017 | China, 2018 |
| Study design | Match case-control | Pre-Post ERAS | Pre-Post ERAS | Match case-control |
| ERAS/non-ERAS | 20/40 | 80/97 | 42/80 | 318/318 |
| Inclusion criteria | Obstructing colorectal cancer | Benign diseases and malignancy | Obstructing colorectal cancer | Obstructing colorectal cancer |
| Exclusion criteria | No bowel resection, concomitant bowel perforation | Laparoscopic surgery | No bowel resection, concomitant bowel perforation | Recurrent tumor, no bowel resection, concomitant bowel perforation |
| Clinical outcomes | ||||
| GI recovery time | Sig. decreased | NA | NA | Sig. decreased |
| Complication | Decreased | Sig. decreased | Decreased | Sig. decreased |
| Hospital stay | Sig. decreased | Same | Sig. decreased | Sig. decreased |
| 30-d mortality | Same | Same | Same | Same |
| 30-d readmission | Same | Same | Same | Same |
| 30-d reoperation | NA | Same | Same | Same |
| Interval between surgery and chemotherapy | sig. decreased | NA | NA | sig. decreased |
There were two studies evaluating clinical outcomes between ERAS in emergency colorectal surgery and that in an elective setting[13,14]. The first study was a retrospective study published in 2012 from the Netherlands examining the feasibility of ERAS program in various patient groups including 41 patients undergoing emergency colorectal resections for benign or malignant colorectal diseases. The authors found that patients undergoing emergency surgery had a significantly longer hospitalization and a considerably higher rate of unplanned reoperation than those undergoing elective surgery. There was no difference in readmission rate and anastomosis leakage rate between elective and emergency colorectal surgery. In their conclusion, they suggested that ERAS protocol for elective surgery needed to be modified before effectively applying in emergency colorectal surgery.
The other publication was a prospective cohort study using the ERAS® Interactive Audit System from a university hospital in Switzerland[14]. The investigators compared clinical outcomes between 28 urgent colectomies and 63 elective colectomies in a well-established ERAS surgical unit. Of note, patients having rectal resection and those requiring ICU admission longer than 2 nights were excluded from this study. The authors found that patients undergoing urgent operations had a significantly lower rate of overall compliance with ERAS protocol (57% vs 77%). It is worth nothing that preoperative and postoperative compliance with ERAS was significantly lower in urgent colectomies – but not intraoperative compliance. Although patients having urgent surgery had more co-morbidities and operative risk, there was no significant difference in the rate of postoperative complication between groups (64% vs 51%). Not surprisingly, emergency operations were associated with a significantly longer length of postoperative stay (8 d vs 5 d). The authors suggested that the application of ERAS for urgent colectomy was feasible and beneficial. Also, many of the ERAS recommended measures can be applied in the emergency situation especially intraoperative measures.
In the ERAS society’s recommended guidelines for perioperative care in an elective setting in 2013, there are 20 and 21 ERAS items for colonic surgery and rectal surgery, respectively[4,5]. Most of the protocol items were used in emergency colorectal surgery with some modification[8,10-12]. Obviously, some preoperative ERAS items such as nutritional support, carbohydrate loading and “full” optimization of medical conditions are impossible to achieve in an emergency basis. However, nearly all ERAS items for elective colorectal surgery appeared to be appropriate and applicable in emergency setting. This session presents some available evidence of individual ERAS item in emergency colorectal surgery (or emergency laparotomy).
In an elective surgery, detailed information and preoperative counseling has been shown to have beneficial effects such as a reduction in postoperative stress, pain and anxiety[15]. However, the supporting evidence for these positive effects in emergency colorectal surgery is lacking. Intuitively, in an emergency setting where postoperative morbidity and mortality could be significantly high, healthcare professionals especially surgeons should provide concise and practical information to patients and their family prior to surgery - including decision-making process, type of surgery, potential intraoperative and postoperative complications, risk of stoma formation and duration of hospitalization.
Regarding stoma education, it is known that stoma formation is sometimes inevitable in many emergency colorectal operations. Presence of a stoma could be a factor associated with prolonged hospitalization - especially when there was no perioperative patient education or counseling. On the other hand, structured patient stoma education by an enterostomal nurse specialist was shown to reduce length of hospital stay and improve patient’s quality of life and psychosocial adjustment[16]. Therefore stoma education should be given preoperatively (if feasible) and stoma teaching should be performed as soon as possible in the early postoperative period.
In an acute surgical emergency, preoperative evaluation and optimization might be limited due to time constraint and patient’s conditions. Risk stratification should be a part of standard preoperative assessment and optimization in emergency colorectal surgery. In addition to the American Society of Anesthesiologists (ASA) classification which is the most common score risk stratification used, the ColoRectal Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (CR-POSSUM) could provide a better predictor of postoperative mortality[17]. All patients requiring an emergency laparotomy with an estimated risk of death of more than 10% should go to critical care unit postoperatively[18], and maybe preoperatively for more optimization of general conditions.
The impact of preoperative optimization on clinical outcome following emergency laparotomy has recently been studied in a prospective randomized trial of 94 patients with generalized peritonitis due to gastrointestinal perforation[19]. This study demonstrated a shorter length of hospital stay and a lower rate of postoperative death in patients receiving standardized, algorithmic management in the preoperative holding room – where central venous cannulation was performed and goal-directed optimization was done. Of note, patients with goal-directed optimization were sent to an operating theater after objectively achieving all three end points (central venous pressure 8-12 cmH2O, mean arterial pressure of 65 mmHg or above, and urine output at least 0.5 mL/kg per hour) while those in the control group (clinical judgment without any fixed algorithm) were taken up for surgery after subjective hemodynamic stabilization. Empirical broad-spectrum antibiotics were given intravenously to patients in both groups. These finding suggested that goal-directed preoperative optimization, including targeted intravenous fluid resuscitation and appropriate antibiotic coverage, is of great importance in emergency major abdominal surgery.
Preoperative high HbA1c and perioperative hyperglycemia were associated with major adverse events after emergency general surgery including colorectal operations[20]. Despite the difficulty in optimizing preoperative HbA1c in emergency patients, perioperative glycemic control is still possible and crucial in both diabetic patients and non-diabetic patients. Distinctive perioperative glucose management should be guided by preoperative glycemic control, type of an operation and patient’s status – with targeted glucose levels between 140 and 180 mg/dL (7.7-10 mmol/L)[21].
Within an ERAS protocol, the use of thoracic epidural analgesia may be associated with superior pain control and quicker return of gut function but this does not translate into improved recovery or reduced morbidity when compared with alternative analgesic techniques such as patient-controlled systemic opiates and continuous wound infiltration[22]. Whether thoracic epidural analgesia will be used in conjunction with general anesthesia in emergency colorectal surgery mainly depends on the policy of hospital and physician’s preference[8,11]. However, the use of epidural analgesia is contraindicated in patients with coagulopathy or having bleeding tendency, and those with hemodynamic instability.
Goal-directed fluid therapy (GDFT) aims to maintain adequate organ perfusion to delivery sufficient oxygen to all organs during and after surgery. In daily practice, several hemodynamic variables such as heart rate, mean arterial pressure, and central venous pressure are measured to adjust the amount of intravenous fluid, blood transfusion, and vasopressor given. In a setting of GDFT, advanced monitoring devices may be required such as esophageal Doppler monitor or non-invasive cardiac output monitor. A recent meta-analysis of 2099 patients undergoing elective major abdominal operations including colorectal surgery indicated that, within an ERAS protocol, GDFT was associated with a significant reduction in the length of intensive care and time to first defecation - but no difference was seen in mortality, time to first passage of flatus, or risk of postoperative ileus[23].
So far, there were few randomized control trials of GDFT in emergency surgery. It appeared that GDFT did not have beneficial effects on renal function, major morbidity and mortality after emergency abdominal operations[24,25]. Nevertheless, in the United Kingdom, the Emergency Laparotomy Pathway Quality Improvement Care (ELPQuiC) Collaborator Group included GDFT as a part of perioperative care bundle to reduce mortality after emergency laparotomy[26]. Lastly, we need more studies to identify emergency surgical patients who will benefit from GDFT - especially in an ERAS setting.
Perioperative hypothermia may contribute to delayed recovery and increased postoperative complications such as surgical site infection, major cardiac events, and blood loss[27]. Prevalence of intraoperative and postoperative hypothermia in emergency surgery could be as high as 60% - especially in patients undergoing major abdominal surgery and those receiving the large amount of intravenous crystalloids. However, there is no significant relationship between perioperative hypothermia and length of hospital stay in critically ill surgical patients[28]. Similar to an elective setting, use of warming techniques such as forced air warming in emergency could reverse or protect against intraoperative hypothermia[27].
When laparoscopy and ERAS protocol are combined in an elective colorectal surgery, postoperative complication and hospital stay are further reduced[29]. Moreover, laparoscopic surgery could offer independent advantages beyond ERAS protocol. According to the American College of Surgeons National Surgical Quality Improvement Program, the use of laparoscopy in emergency colorectal surgery gradually increased from 5.5% in 2005 to 11.5% in 2014[30]. A population-based study in England also reported that laparoscopy use in emergency colorectal resection doubled from 15.1% in 2010 to 30.2% in 2016[31]. However, laparoscopic surgery was less common in patients with poorer physical status, more advanced T-stage and presence of distant metastasis. The reported conversion rate was up to 20% even in the hand of experienced laparoscopic surgeons[32].
Compared with open surgery, the use of laparoscopic approach in emergency resection of colorectal cancer was associated with a shorter length of hospital stay by 3.7 d and a lower rate of 90-d postoperative mortality by 22%. There was no significant difference in rates of readmission or reoperation between the two approaches[31]. The oncological outcomes between laparoscopic approach and open surgery in emergency colectomy for colonic adenocarcinoma seemed to be comparable as shown in a retrospective propensity score-matched study of 108 cases (36 laparoscopies and 72 open operations)[33]. With a median follow-up of 3.6 years, there was no difference in 3-year overall survival and recurrence-free survival by approach although laparoscopic surgery yielded a higher number of lymph nodes harvested.
Based on the recent evidence of laparoscopic approach to emergency colorectal surgery, it was suggested that laparoscopy was linked to a lower rate of postoperative complication and a shorter length of hospital stay when comparing with open surgery. With a sufficient expertise in laparoscopic approach in selective patients, emergency laparoscopy for colon cancer is not inferior to open surgery with regard to short- and long-term oncological outcomes. However, the evidence supporting the feasibility of laparoscopic surgery in emergency setting was mainly based on operations for obstructed colon cancer and perforated sigmoid diverticulitis. Alternatively, open right hemicolectomy through right transverse skin crease incision may be used instead of laparoscopy[8] because it has been shown to have no significant difference in postoperative opioid consumption, gastrointestinal recovery and length of hospital stay between these two approaches[34].
The need of peritoneal drain placement after emergency laparotomy is controversial. So far, there is insufficient evidence supporting the routine use of drain after emergency bowel resection[35]. Many authors have suggested avoidance of intraabdominal or pelvic drainage - except with specific indications such as massive intraoperative bleeding, purulent or fecal peritonitis and tenuous anastomosis[36].
Effective postoperative pain control is crucial but often inadequately seen in an emergency surgical setting because of several reasons such as a lack of priority to treat pain and failure to implement pain management guideline. Many experts have recommended different non-pharmacological and pharmacological modalities (known as multimodal analgesia) for postoperative pain management which should be tailored to the individual and the operation involved[37]. Practically, there should be no argument to imply this concept of opioid-sparing multimodal analgesia in emergency colorectal surgery.
After an emergency colectomy for acute colonic obstruction or perforation, surgeons tend to retain nasogastric tube (NGT) postoperatively to decrease abdominal distension and aim to remove it on postoperative day 1 or 2[14]. However, there is growing evidence supporting the avoidance of NGT insertion in emergency laparotomy. For example, Venara et al[38] examined the results of immediate postoperative removal of NGT after emergency colectomy for malignant large bowel obstruction. Of note, only 10% of 79 studied patients had no postoperative NGT. Interestingly, the immediate removal of NGT and inclusion in ERAS protocol were not associated with the need for NGT reinsertion. Meanwhile, risk factors for NGT reinsertion were left-sided colon cancer, postoperative ileus and severe postoperative complications[38]. A randomized controlled trail examining the effect of prophylactic NGT decompression after emergency laparotomy for generalized peritonitis and intestinal obstruction indicated that routine NGT insertion did not prevent gastrointestinal discomfort or anastomotic leakage[39].
In an elective colorectal surgery, early feeding reduced postoperative complication and length of hospital stay – without significant difference in the rates of anastomotic leakage, pneumonia, vomiting and NGT reinsertion[40]. However, patients undergoing emergency colorectal surgery are more likely to have prolonged postoperative ileus and complications than those in an elective setting[14,41]. Accordingly, conclusions drawn from trials on elective surgery cannot be extrapolated to emergency surgery. Meanwhile, data on early feeding after emergency abdominal surgery are limited - with conflicting results.
Klappenbach et al[42] performed a randomized controlled trial comparing outcomes between early feeding (soft diet within 24 h after surgery) and traditional care (liquid diet commenced upon the passage of flatus or stool) in 295 patients undergoing emergency laparotomy (two-third for perforated appendicitis and few for colorectal diseases)[42]. They found no significant difference in morbidity, postoperative ileus and the length of hospital stay between groups – but a higher rate of vomiting in the early feeding group. In contrast, a retrospective study of 84 patients undergoing emergency bowel resection showed a significantly shorter hospitalization in those with early feeding[43]. Although the concept of early intake after emergency colorectal surgery requires adequately-powered randomized controlled trials, we believe that early feeding after emergency colorectal surgery is possible but should be tailored. Any symptom and sign of postoperative ileus is a caution to slow feeding. Etiologies of feeding intolerance should be carefully investigated and corrected if possible.
In a systematic review and meta-analysis in 2012, postoperative deep breathing exercise was associated with improved pulmonary function and respiratory muscle strength after elective upper abdominal surgery – but it did not reduce the incidence of pulmonary complication[44]. A recent randomized controlled trial of 150 patients undergoing exploratory laparotomy including emergency colorectal surgery (about 45%) showed that adding incentive spirometry to a routine breathing exercise did not improve the recovery of postoperative pulmonary function nor decreased the rate of respiratory complication and length of hospital stay[45]. Although there is no evidence indicating the direct benefits of breathing exercise after emergency colorectal surgery, many surgeons still encourage their patients to have sessions of deep breathing and coughing in the early postoperative period[8].
There is no strong evidence demonstrating clinical benefits of early postoperative mobilization, but prolonged immobilization could increase the risk of pneumonia, thromboembolism, insulin resistance, and muscle weakness[4]. Not surprisingly, the ERAS Society guideline for perioperative care in elective colonic and rectal surgery strongly has recommended early assisted or independent mobilization after surgery[4,5]. However, early mobilization and physiotherapy following emergency colorectal surgery are not well documented. There is an ongoing multicenter randomized controlled trial in Australia studying the effectiveness of enhanced physiotherapy program, including breathing exercises, increased physical activities and rehabilitation, for the prevention of complications and improved physical recovery after emergency abdominal surgery[46].
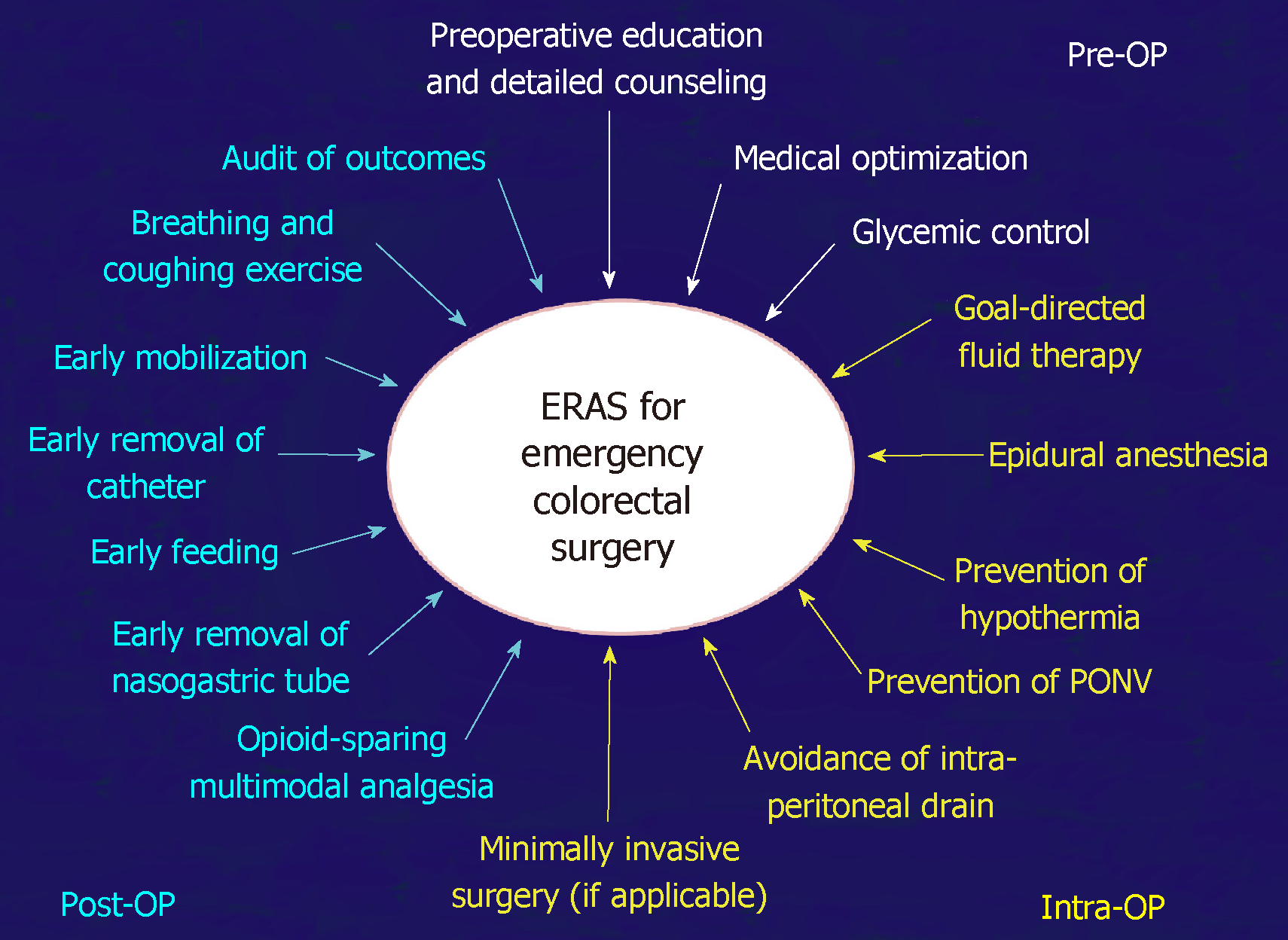
There are many challenges in the implementation of ERAS in emergency colorectal surgery including patient’s acute condition, limited resources and healthcare personals in an emergency setting, and difficulty in optimizing patient’s general condition. Any ERAS items used in emergency colorectal surgery should be guided by the concept of reducing in stress responses to surgery and promoting the function recovery of surgical patients. Evidence-based ERAS protocol for emergency colorectal surgery is shown in Table 3 and Figure 1.
| ERAS item | Recommendation |
| Preoperative phase | |
| Education and detailed counseling | Patients should routinely receive concise and practical preoperative education including stoma counseling |
| Medical optimization | Preoperative risk stratification and “targeted” optimization of general conditions are recommended |
| Glycemic control | Perioperative blood glucose should be maintained between 140 and 180 mg/dL |
| Intraoperative phase | |
| Use of epidural analgesia | Thoracic epidural analgesia may be used in patients with stable hemodynamic and no bleeding tendency |
| GDFT | GDFT may be beneficial in patients with high-predicted postoperative mortality |
| Prevention of hypothermia | All measures should be done to prevent or reverse intraoperative hypothermia |
| PONV | A multimodal prophylaxis of PONV should be used in all patients based on their risk factors for PONV |
| Minimally invasive surgery | Laparoscopy may be performed in selected patients by experienced surgeons |
| Avoidance of intraperitoneal drains | Intraabdominal and pelvic drains should not be used routinely |
| Postoperative phase | |
| Multimodal analgesia | Opioid-sparing multimodal analgesia should be tailored to the individual and the operation involved |
| Early removal of NGT | NGT can be removed safely on postoperative day 1-2 unless paralytic ileus is evident |
| Early feeding | Oral intake can resume in stabilized patients and should progress moderately if patients can tolerate |
| Early removal of urinary catheter | Urinary catheter can be removed safely on postoperative day 1-2 |
| Breathing and coughing exercise | Patients are encouraged to have sessions of deep breathing and coughing exercise postoperatively |
| Early mobilization | Patients are encouraged to have early independent mobilization as a part of physiotherapy and rehabilitation program |
In the future, an ERAS protocol may further be tailored based on the indications of emergency surgery – which could be divided into 2 main categories: presence of intraabdominal infection (e.g., ruptured colonic diverticulitis, perforated colorectal cancer, acute fulminant colitis) and absence of intraabdominal sepsis (e.g., obstructed colorectal cancer and massive lower gastrointestinal bleeding). The former may require damage control surgery rather than definite treatment in the index operation. Preoperative ERAS items might be unable to apply in patients with intraabdominal sepsis, so the intraoperative and postoperative items may be utmost important.
So far, there are a very limited number of studies evaluating the effects of ERAS program in intraabdominal sepsis[10,47,48] - especially with the origin of infection from colon and rectum. A recent small cohort study, by Lohsiriwat from Thailand, evaluating the results of ERAS program in emergency colorectal resection between patients with intraabdominal sepsis (n = 14) and those without (n = 46) found that patients with intraabdominal sepsis had lower adherence to ERAS items (50% vs 78%) and significantly lower compliance with preoperative optimization, scheduled removal of urinary catheter and early mobilization than those without intraabdominal infection[48].
Randomized controlled trials comparing ERAS vs non-ERAS in emergency colorectal surgery are ideal and will give high-quality evidence on the efficacy and safety of ERAS program in this setting. However, it could be unethical or not practical in daily practice because an ERAS protocol has now become a standard of surgical care in worldwide. Therefore, many investigators have compared surgical results before and after implementation of “modified” ERAS protocol in emergency colorectal surgery[10,11]. Matched case-control studies examining clinical outcomes of acute surgical patients with “high” vs “low” compliance with ERAS are possible[8]. Regarding outcomes measured, they should include clinical outcomes (e.g., postoperative morbidity, reoperation, time to gastrointestinal recovery, length of hospital stay, readmission and mortality), patient-reported outcomes (e.g., health-related quality of life and patient’s satisfaction), and economic analysis. Patient engagement as well as barriers and adherence to an ERAS program in emergency colorectal surgery should thoroughly be studied.
There has been growing evidence demonstrating the safety, feasibility and benefit effects of ERAS program on surgical outcomes following emergency colorectal surgery especially an operation for acutely obstructed colorectal cancer. The ERAS program was associated with a lower rate of overall complication and shorter length of hospital stay – without increased risks of readmission, reoperation and death after emergency colorectal surgery. Compliance with an ERAS program in emergency setting appeared to be lower than that in an elective basis. Although there is limited evidence about the benefit of individual ERAS item used in emergency colorectal surgery, many surgeons have adopted and applied several recommended ERAS items form guidelines for elective colon and rectal surgery into the emergency setting.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Thailand
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Koyanagi K, Mikulic D, M'Koma AE S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Greer NL, Gunnar WP, Dahm P, Lee AE, MacDonald R, Shaukat A, Sultan S, Wilt TJ. Enhanced Recovery Protocols for Adults Undergoing Colorectal Surgery: A Systematic Review and Meta-analysis. Dis Colon Rectum. 2018;61:1108-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 2. | Lemanu DP, Singh PP, Stowers MD, Hill AG. A systematic review to assess cost effectiveness of enhanced recovery after surgery programmes in colorectal surgery. Colorectal Dis. 2014;16:338-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 3. | Gustafsson UO, Oppelstrup H, Thorell A, Nygren J, Ljungqvist O. Adherence to the ERAS protocol is Associated with 5-Year Survival After Colorectal Cancer Surgery: A Retrospective Cohort Study. World J Surg. 2016;40:1741-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 260] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 4. | Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N, McNaught CE, Macfie J, Liberman AS, Soop M, Hill A, Kennedy RH, Lobo DN, Fearon K, Ljungqvist O; Enhanced Recovery After Surgery (ERAS) Society for Perioperative Care; European Society for Clinical Nutrition and Metabolism (ESPEN); International Association for Surgical Metabolism and Nutrition (IASMEN). Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg. 2013;37:259-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 849] [Article Influence: 70.8] [Reference Citation Analysis (0)] |
| 5. | Nygren J, Thacker J, Carli F, Fearon KC, Norderval S, Lobo DN, Ljungqvist O, Soop M, Ramirez J; Enhanced Recovery After Surgery (ERAS) Society, for Perioperative Care; European Society for Clinical Nutrition and Metabolism (ESPEN); International Association for Surgical Metabolism and Nutrition (IASMEN). Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. World J Surg. 2013;37:285-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 320] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 6. | Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR. Clinical Practice Guidelines for Enhanced Recovery After Colon and Rectal Surgery From the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum. 2017;60:761-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 289] [Article Influence: 36.1] [Reference Citation Analysis (0)] |
| 7. | Bayar B, Yılmaz KB, Akıncı M, Şahin A, Kulaçoğlu H. An evaluation of treatment results of emergency versus elective surgery in colorectal cancer patients. Ulus Cerrahi Derg. 2015;32:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Lohsiriwat V. Enhanced recovery after surgery vs conventional care in emergency colorectal surgery. World J Gastroenterol. 2014;20:13950-13955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 105] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 9. | Ho KS, Quah HM, Lim JF, Tang CL, Eu KW. Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis. 2012;27:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Wisely JC, Barclay KL. Effects of an Enhanced Recovery After Surgery programme on emergency surgical patients. ANZ J Surg. 2016;86:883-888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 11. | Shida D, Tagawa K, Inada K, Nasu K, Seyama Y, Maeshiro T, Miyamoto S, Inoue S, Umekita N. Modified enhanced recovery after surgery (ERAS) protocols for patients with obstructive colorectal cancer. BMC Surg. 2017;17:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer: A propensity score matching analysis. Medicine (Baltimore). 2018;97:e12348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Verheijen PM, Vd Ven AW, Davids PH, Vd Wall BJ, Pronk A. Feasibility of enhanced recovery programme in various patient groups. Int J Colorectal Dis. 2012;27:507-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Roulin D, Blanc C, Muradbegovic M, Hahnloser D, Demartines N, Hübner M. Enhanced recovery pathway for urgent colectomy. World J Surg. 2014;38:2153-2159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (1)] |
| 15. | Shuldham C. A review of the impact of pre-operative education on recovery from surgery. Int J Nurs Stud. 1999;36:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 86] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Danielsen AK, Burcharth J, Rosenberg J. Patient education has a positive effect in patients with a stoma: a systematic review. Colorectal Dis. 2013;15:e276-e283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 17. | Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, Windsor AC. Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg. 2004;91:1174-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 246] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 18. | Shah N, Hamilton M. Clinical review: Can we predict which patients are at risk of complications following surgery? Crit Care. 2013;17:226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Sethi A, Debbarma M, Narang N, Saxena A, Mahobia M, Tomar GS. Impact of Targeted Preoperative Optimization on Clinical Outcome in Emergency Abdominal Surgeries: A Prospective Randomized Trial. Anesth Essays Res. 2018;12:149-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Jehan F, Khan M, Sakran JV, Khreiss M, O'Keeffe T, Chi A, Kulvatunyou N, Jain A, Zakaria ER, Joseph B. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: What is the role of Plasma Hemoglobin A1c? J Trauma Acute Care Surg. 2018;84:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 21. | Duggan EW, Carlson K, Umpierrez GE. Perioperative Hyperglycemia Management: An Update. Anesthesiology. 2017;126:547-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 241] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 22. | Hughes MJ, Ventham NT, McNally S, Harrison E, Wigmore S. Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis. JAMA Surg. 2014;149:1224-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 142] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 23. | Rollins KE, Lobo DN. Intraoperative Goal-directed Fluid Therapy in Elective Major Abdominal Surgery: A Meta-analysis of Randomized Controlled Trials. Ann Surg. 2016;263:465-476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 162] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 24. | Harten J, Crozier JE, McCreath B, Hay A, McMillan DC, McArdle CS, Kinsella J. Effect of intraoperative fluid optimisation on renal function in patients undergoing emergency abdominal surgery: a randomised controlled pilot study (ISRCTN 11799696). Int J Surg. 2008;6:197-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Pavlovic G, Diaper J, Ellenberger C, Frei A, Bendjelid K, Bonhomme F, Licker M. Impact of early haemodynamic goal-directed therapy in patients undergoing emergency surgery: an open prospective, randomised trial. J Clin Monit Comput. 2016;30:87-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, Quiney N; ELPQuiC Collaborator Group; ELPQuiC Collaborator Group. Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg. 2015;102:57-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 164] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 27. | Bilgin H. Inadverdent Perioperative Hypothermia. Turk J Anaesthesiol Reanim. 2017;45:124-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Abelha FJ, Castro MA, Neves AM, Landeiro NM, Santos CC. Hypothermia in a surgical intensive care unit. BMC Anesthesiol. 2005;5:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Spanjersberg WR, van Sambeeck JD, Bremers A, Rosman C, van Laarhoven CJ. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015;29:3443-3453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 140] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 30. | Davis CH, Shirkey BA, Moore LW, Gaglani T, Du XL, Bailey HR, Cusick MV. Trends in laparoscopic colorectal surgery over time from 2005-2014 using the NSQIP database. J Surg Res. 2018;223:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Vallance AE, Keller DS, Hill J, Braun M, Kuryba A, van der Meulen J, Walker K, Chand M. Role of Emergency Laparoscopic Colectomy for Colorectal Cancer: A Population-Based Study in England. Ann Surg. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 32. | Vennix S, Boersema GS, Buskens CJ, Menon AG, Tanis PJ, Lange JF, Bemelman WA. Emergency Laparoscopic Sigmoidectomy for Perforated Diverticulitis with Generalised Peritonitis: A Systematic Review. Dig Surg. 2016;33:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 33. | Odermatt M, Miskovic D, Siddiqi N, Khan J, Parvaiz A. Short- and long-term outcomes after laparoscopic versus open emergency resection for colon cancer: an observational propensity score-matched study. World J Surg. 2013;37:2458-2467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 34. | Lohsiriwat V, Lohsiriwat D, Chinswangwatanakul V, Akaraviputh T, Lert-Akyamanee N. Comparison of short-term outcomes between laparoscopically-assisted vs. transverse-incision open right hemicolectomy for right-sided colon cancer: a retrospective study. World J Surg Oncol. 2007;5:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Nasir AA, Abdur-Rahman LO, Adeniran JO. Is intraabdominal drainage necessary after laparotomy for typhoid intestinal perforation? J Pediatr Surg. 2012;47:355-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Lohsiriwat V. Pelvic drain after colorectal anastomosis: useful or useless. Transl Cancer Res. 2016;5:S1404-S1407. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, Griffith S, Manworren R, McCarberg B, Montgomery R, Murphy J, Perkal MF, Suresh S, Sluka K, Strassels S, Thirlby R, Viscusi E, Walco GA, Warner L, Weisman SJ, Wu CL. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17:131-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1346] [Cited by in RCA: 1788] [Article Influence: 198.7] [Reference Citation Analysis (0)] |
| 38. | Venara A, Barbieux J, Colas PA, Le Fouler A, Lermite E, Hamy A. Primary Surgery for Malignant Large Bowel Obstruction: Postoperative Nasogastric Tube Reinsertion is Not Mandatory. World J Surg. 2017;41:1903-1909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Sapkota R, Bhandari RS. Prophylactic nasogastric decompression after emergency laparotomy. JNMA J Nepal Med Assoc. 2013;52:437-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Zhuang CL, Ye XZ, Zhang CJ, Dong QT, Chen BC, Yu Z. Early versus traditional postoperative oral feeding in patients undergoing elective colorectal surgery: a meta-analysis of randomized clinical trials. Dig Surg. 2013;30:225-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 41. | Chapuis PH, Bokey L, Keshava A, Rickard MJ, Stewart P, Young CJ, Dent OF. Risk factors for prolonged ileus after resection of colorectal cancer: an observational study of 2400 consecutive patients. Ann Surg. 2013;257:909-915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 157] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 42. | Klappenbach RF, Yazyi FJ, Alonso Quintas F, Horna ME, Alvarez Rodríguez J, Oría A. Early oral feeding versus traditional postoperative care after abdominal emergency surgery: a randomized controlled trial. World J Surg. 2013;37:2293-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 43. | Lee HS, Shim H, Jang JY, Lee H, Lee JG. Early feeding is feasible after emergency gastrointestinal surgery. Yonsei Med J. 2014;55:395-400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 44. | Grams ST, Ono LM, Noronha MA, Schivinski CI, Paulin E. Breathing exercises in upper abdominal surgery: a systematic review and meta-analysis. Rev Bras Fisioter. 2012;16:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 45. | Tyson AF, Kendig CE, Mabedi C, Cairns BA, Charles AG. The effect of incentive spirometry on postoperative pulmonary function following laparotomy: a randomized clinical trial. JAMA Surg. 2015;150:229-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 46. | Boden I, Sullivan K, Hackett C, Winzer B, Lane R, McKinnon M, Robertson I. ICEAGE (Incidence of Complications following Emergency Abdominal surgery: Get Exercising): study protocol of a pragmatic, multicentre, randomised controlled trial testing physiotherapy for the prevention of complications and improved physical recovery after emergency abdominal surgery. World J Emerg Surg. 2018;13:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 47. | Gonenc M, Dural AC, Celik F, Akarsu C, Kocatas A, Kalayci MU, Dogan Y, Alis H. Enhanced postoperative recovery pathways in emergency surgery: a randomised controlled clinical trial. Am J Surg. 2014;207:807-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 48. | Lohsiriwat V. Enhanced recovery after surgery for emergency colorectal surgery: Are there any differences between intraabdominal infection and other indications? J Visc Surg. 2019;In press. |