Published online Nov 27, 2019. doi: 10.4240/wjgs.v11.i11.414
Peer-review started: July 16, 2019
First decision: August 2, 2019
Revised: September 7, 2019
Accepted: September 25, 2019
Article in press: September 25, 2019
Published online: November 27, 2019
Processing time: 145 Days and 19.4 Hours
Intrahepatic bile duct adenoma (BDA) is one of the rarest of the rare benign tumors of the liver in the pediatric age group. It arises from the epithelial lining of intrahepatic bile ducts. The overall incidence of BDA is 1.3% of all primary benign liver tumors. Few case reports of this rare tumor occurring in adult population are present in the literature and to date, only one pediatric case has been reported worldwide.
An 18-month-old male child presented with chief complaints of mass per abdomen for 8 mo. Computerized tomography abdomen revealed a well-defined exophytic solid tumor arising from the posteroinferior margin of the right lobe of the liver with heterogenous enhancement and cystic changes, suggesting a suspicion of hepatoblastoma. Non-anatomical liver resection was done and a tumor of 10 cm × 9.5 cm was excised. Histopathology of the specimen was conclusive with the diagnosis of intrahepatic bile duct adenoma, which was further supported by immunohistochemistry panel testing. The post-operative period was uneventful. On follow-up, the child was doing well and had no post-operative complication.
Intrahepatic bile duct adenoma in children is very rare and to date only one case has been reported. This is the second pediatric case of intrahepatic bile duct adenoma in the world. Additionally this is the first ever case of such a large tumor presenting in a child.
Core tip: Intrahepatic bile duct adenoma is a rare tumor arising from bile ductules in the liver. It is mostly seen as an incidental finding in adults but it is almost unheard of in children. Therefore it is one of the rarest tumors in children. Although it is a benign tumor, it has the potential to be malignant according to one study reported in adults. This case highlights the fact that it is the second case of this rare tumor occurring in the pediatric age group in the world. The progression into a large tumor in our case report necessitates the need for more information on this rare tumor.
- Citation: Roy AK, Das NN. Pediatric intrahepatic bile duct adenoma - rare liver tumor: A case report. World J Gastrointest Surg 2019; 11(11): 414-421
- URL: https://www.wjgnet.com/1948-9366/full/v11/i11/414.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i11.414
Intrahepatic bile duct adenoma is a rare tumor arising from the epithelium of the bile ducts in liver. The incidence of this tumor in adults is 1.3% of all primary liver tumors[1]. Another name of this tumor is peribiliary gland hamartoma as suggested by Bhathal et al[2] due its similarity with peribiliary glands in their secretory gland cell phenotype. It is mostly reported in adults as an incidental finding on surgery or autopsy below the capsule of liver or on its surface[1,3]. Although it is considered benign in nature, it has the potential to turn into adenocarcinoma as reported by Hasebe et al[4] in their study. The first case of this tumor in pediatric age group was reported in 2014[5]. Here we report the second case of this tumor in a child and the first ever case of this tumor of such a large size in the world.
An 18-month-old male child came to the outpatient department of our hospital with complaints of a mass per abdomen for 8 mo.
On elaborating upon the history of presenting illness, the mother noticed the mass 8 mo ago while bathing the child. The mass was insidious in onset and slowly progressive in nature. There were no associated symptoms of fever, vomiting, reduced appetite, failure to thrive, or jaundice.
The child was born full-term and had no previous history of any illness since childhood.
On examination, the child was conscious, playful, and active. His vitals were within normal limits. Per abdomen examination revealed a non-tender mass of approximately 10 cm × 9 cm extending from inferior liver margin in the right hypochondriam to the right iliac fossa and umbilical regions. It was round to oval in shape and firm in consistency with ill-defined margins.
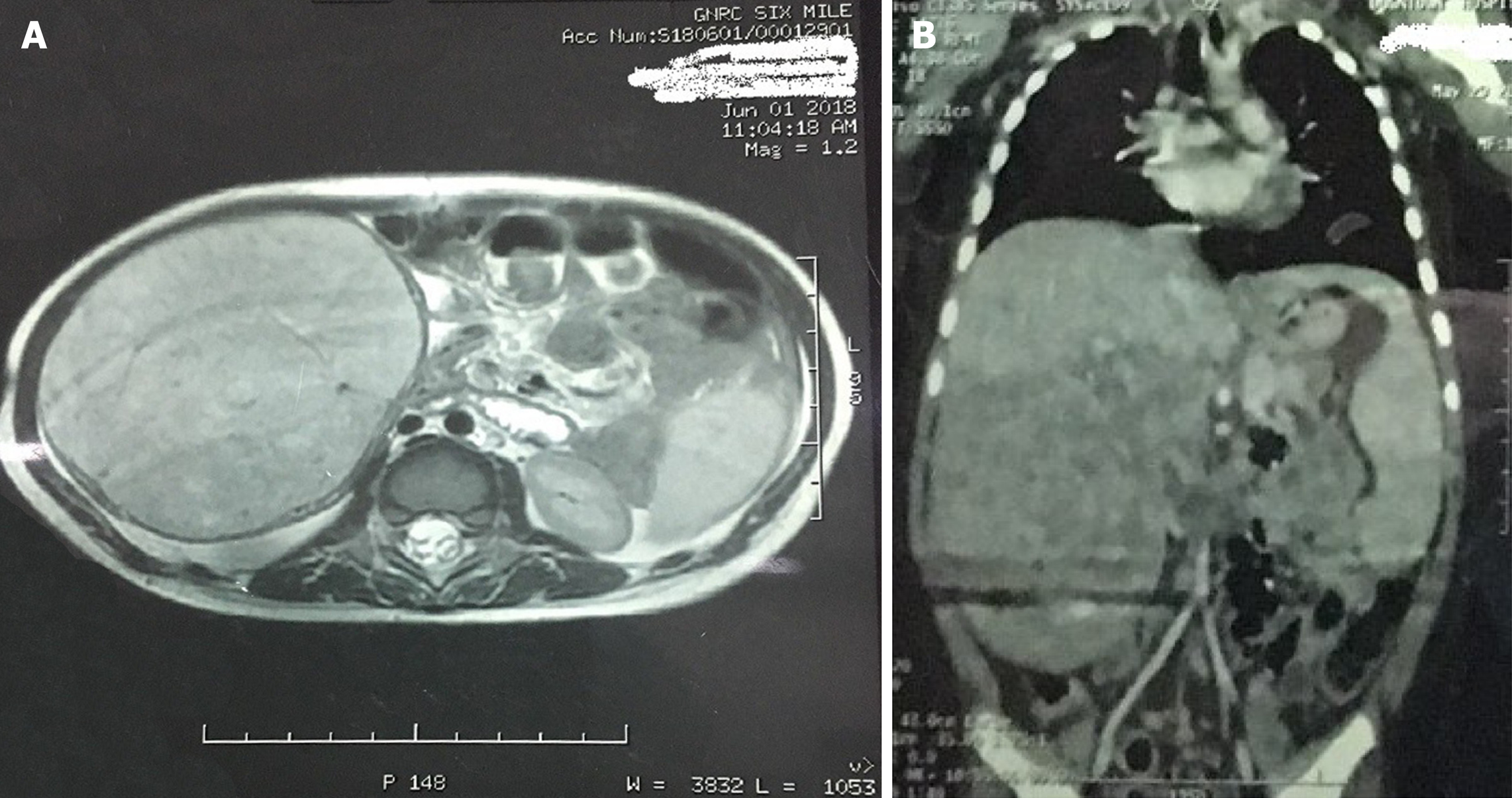
The child was evaluated for the above complaint. Routine blood investigations were normal including the liver function test. Serum alpha-fetoprotein was marginally raised (36.8). Contrast computed tomography (CT) of the abdomen showed a large well defined circumscribed exophytic solid tumor measuring 95 mm × 83 mm × 96 mm arising from the posteroinferior margin of the right lobe of the liver, predominantly from segment V with heterogeneous enhancement and cystic changes. Magnetic resonance imaging abdomen correlated with the CT findings and suggested the possibility of hepatoblastoma (Figure 1). Initial core biopsy showed few groups of atypical cells of epithelial origin infiltrating loose collagenous tissue and was suspicious of hepatoblastoma .
This was a case of intrahepatic bile duct adenoma.
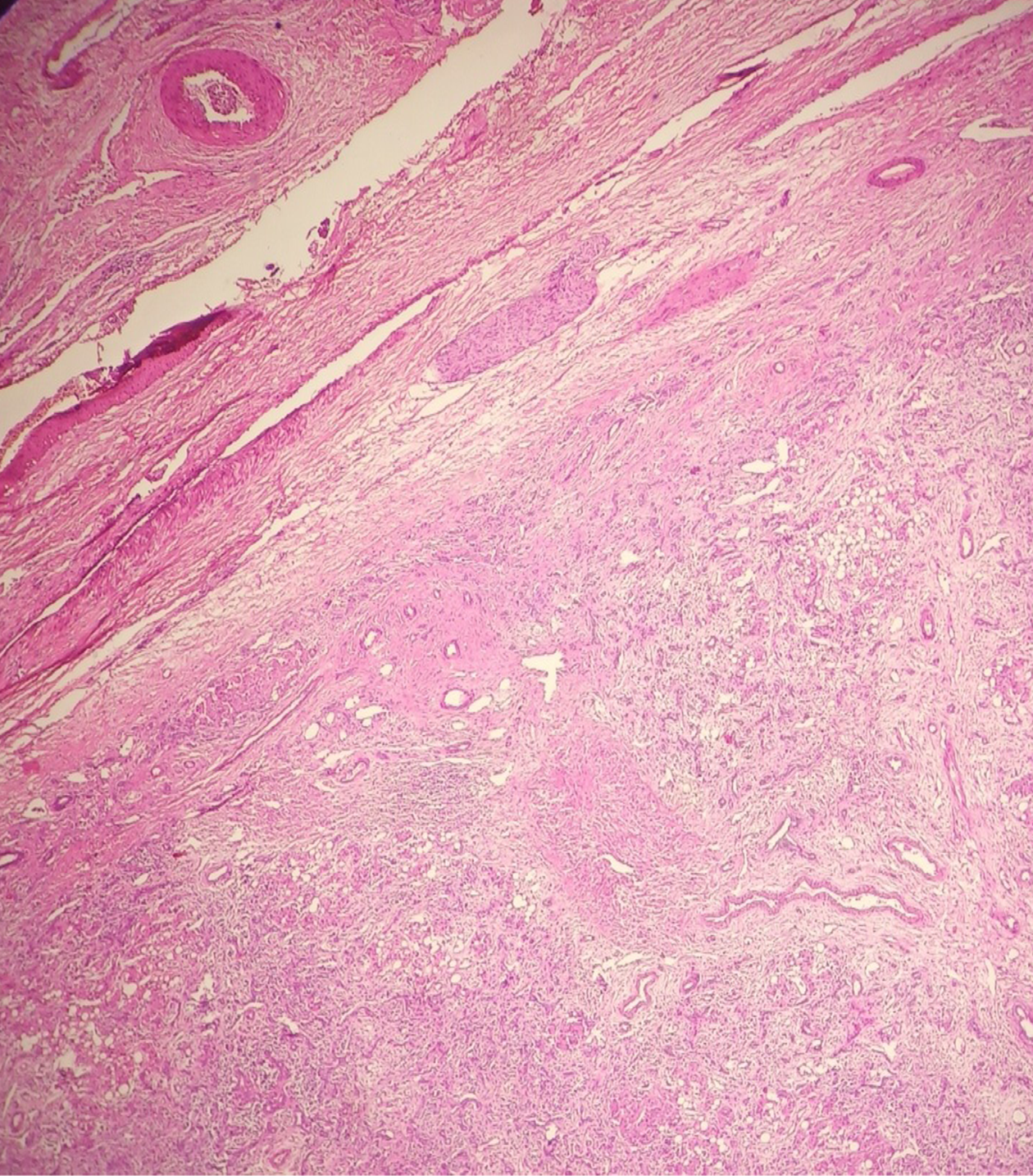
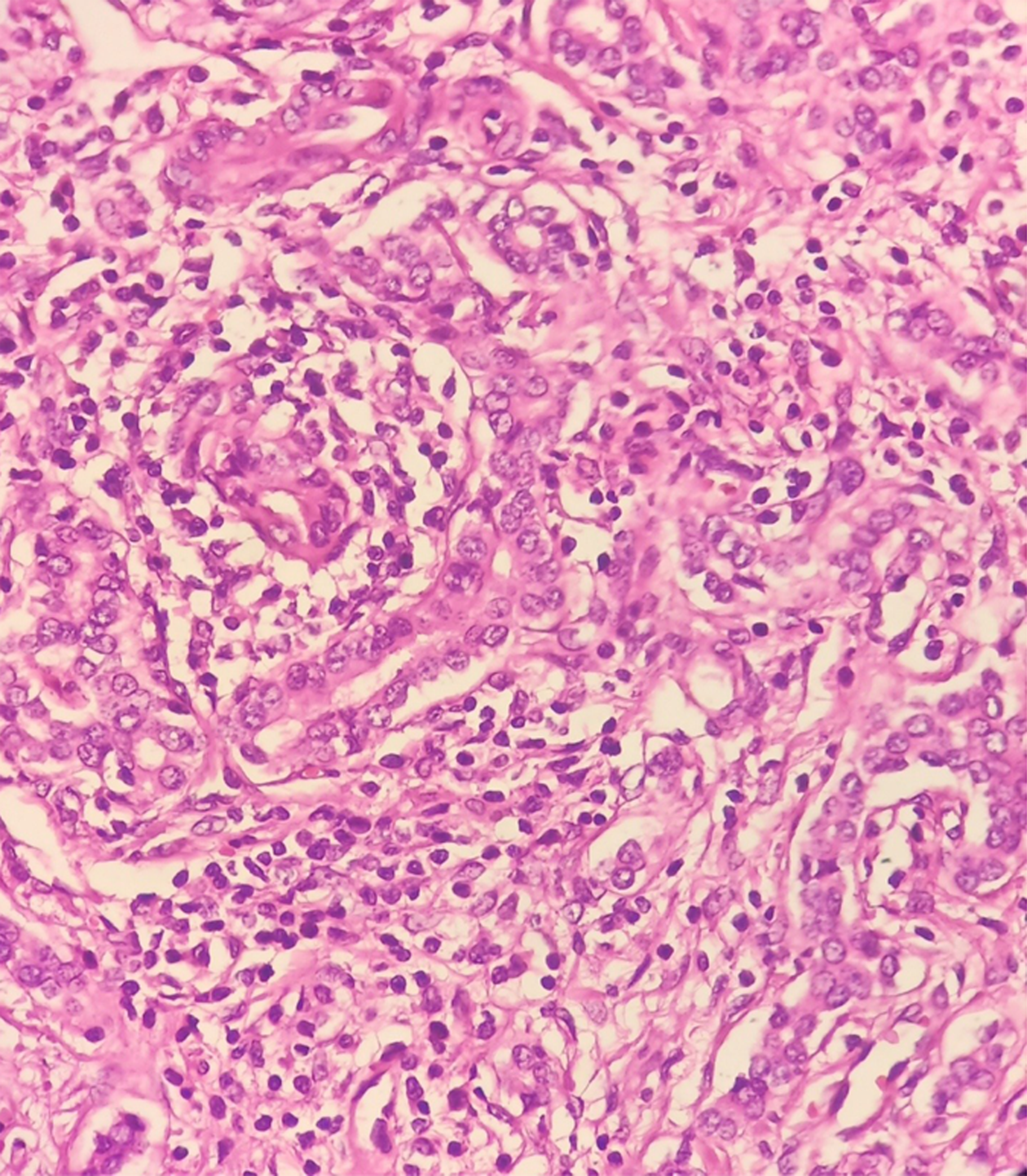
The child was treated with exploratory laparotomy.
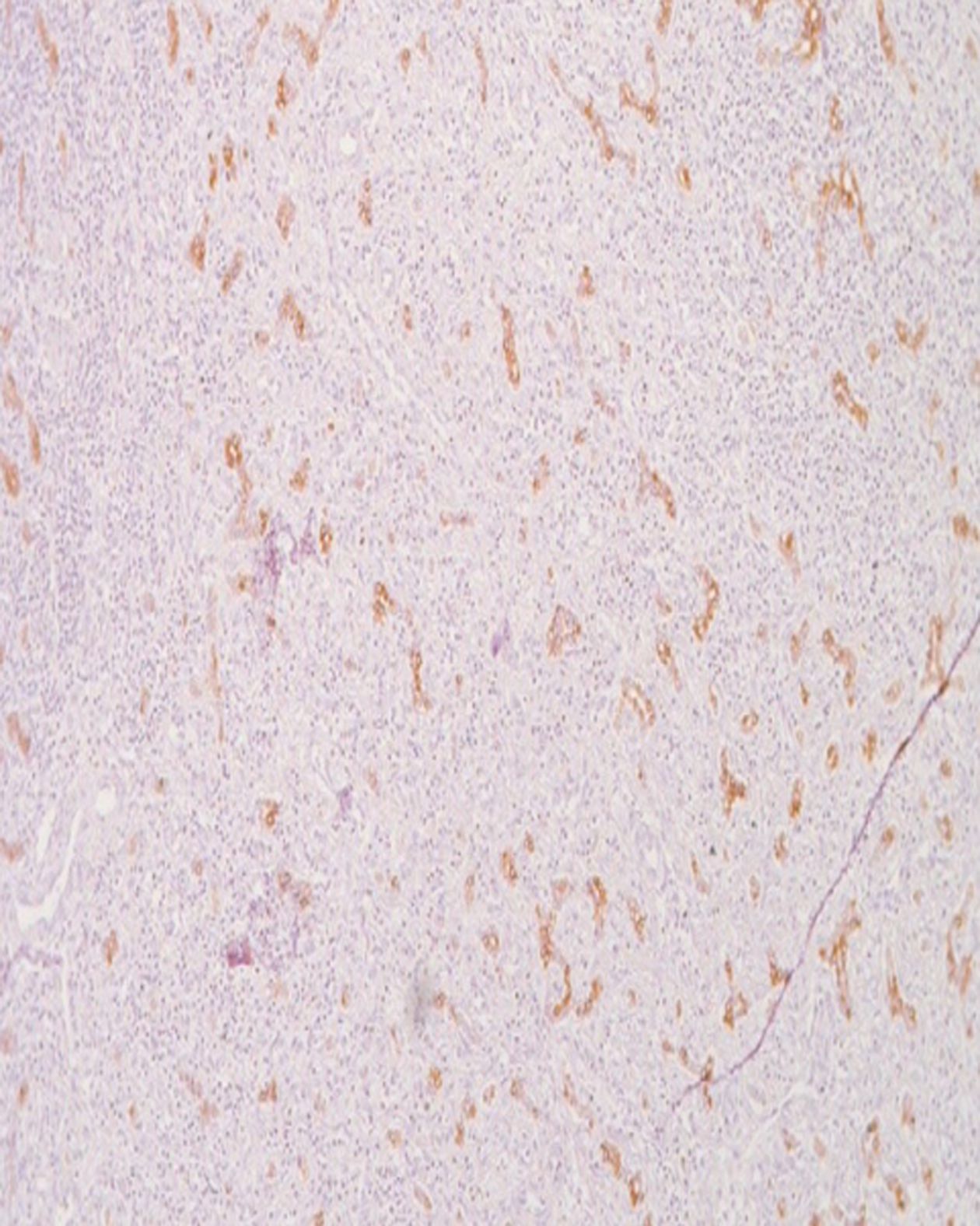
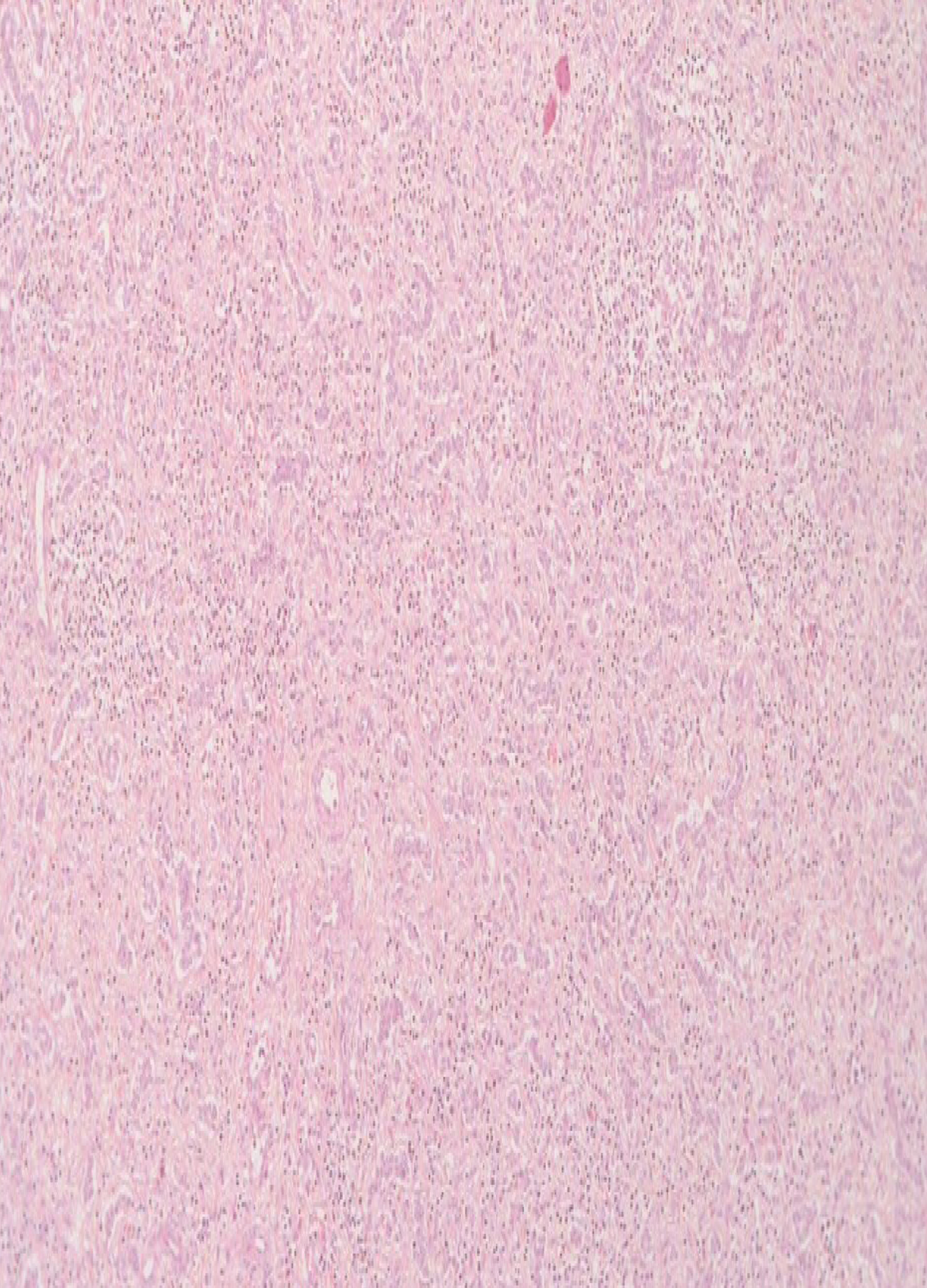
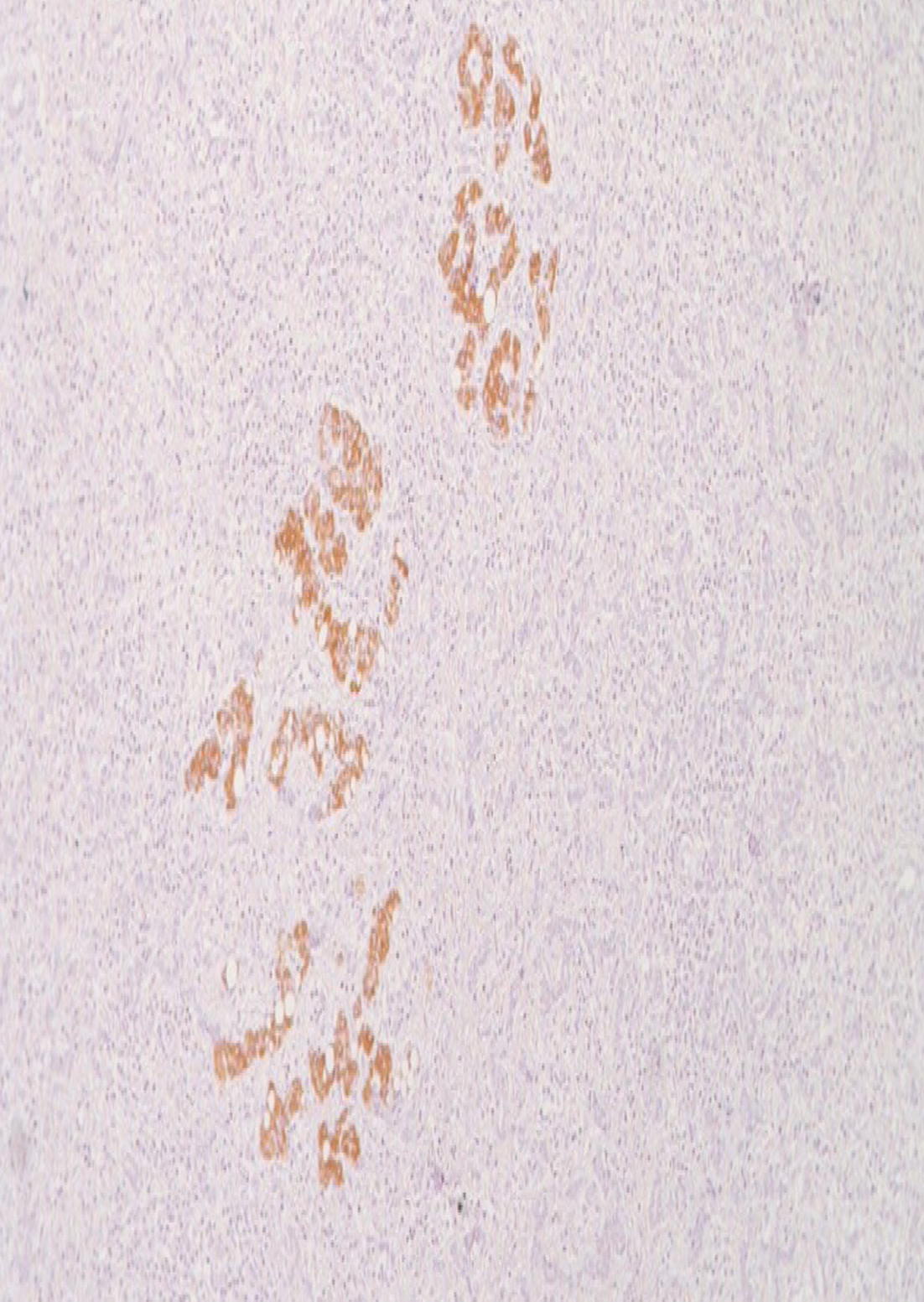
Intra-operatively, a 10 cm × 9.5 cm mass was found to arise from the posteroinferior margins of liver mostly from segment V and was unencapsulated. Non-anatomical wedge resection of liver along with the mass was done under general anesthesia. Histopathology of the specimen showed a lot of proliferative bile ductules in connective tissue stroma containing cells of chronic inflammatory mediators with varying degree of fibrosis, strongly suggesting a diagnosis of intrahepatic bile duct adenoma(Figures 2-4). On further evaluation, the immunohistochemistry panel was positive for cytokeratin 7 (CK7) and was negative for CK20, p53, and anti-human hepatocyte supporting the diagnosis of intrahepatic bile duct adenoma (Figures 5-8). The post-operative period was uneventful and on follow-up, the child was doing well without any complications.
Intra-hepatic bile duct adenoma is one of the rarest liver tumors in children. In the literature, this particular tumor is seen as incidental findings in the adult age group. In their study involving 2125 post-mortem examinations, Cho et al[6] identified only 13 cases of bile duct adenomas. Similarly Craig et al[3] identified only five bile duct adenomas in a study of 50000 autopsies. In the largest series of bile duct adenomas, Allaire et al[1] found 152 cases between 1943 and 1986. Of these 152 bile duct adenomas, nearly 68% (103 cases) were asymptomatic and discovered incidentally during abdominal surgery, while the remaining cases were found at autopsy (49 cases). The incidence in adults is 1.3% of all primary liver tumors[1]. Occurrence of this rare tumor is extremely uncommon in children. To the best of our knowledge, this is the second case of this tumor occurring in a child worldwide.
Peribiliary glands (glands of the biliary tree) are tubular-alveolar glands with serous and mucinous acini. The small glands are deeply embedded in a fibromuscular bed of the duct walls. Peribiliary glands are divided into intramural mucous glands and extramural seromucous glands, and both types are continuous with the lining epithelium of bile ducts[7-10]. Because of its similarity with peribiliary glands in their secretory cell phenotype, this tumor is also called peribiliary gland hamartoma[2]. It mostly affects the age group between 20 and 70 years with no sex differentiation[1], in contrast to our case report where the patient was 18 mo old.
The size of this tumor usually ranges from 1 mm to 20 mm and is usually subcapsular in location. It is typically a solitary lesion but can also present as multiple lesions[6,11]. The size of the tumor in our case report was 10 cm × 9.5 cm, which to the best of our knowledge, is the first ever case of such a large size of this rare tumor being reported in the world.
The pathogenesis of intrahepatic BDA is very unclear. Hughes et al[12] found that BDA is phenotypically similar to the inflamed peribiliary glands suggesting, that it can be formed by reactive processes to focal bile duct injury caused by trauma or inflammation. Grossly the tumor is well-circumscribed but unencapsulated, firm, gray-white, tan or yellow, subcapsular and mostly round to oval in shape. Microscopically BDAs are composed of proliferating bile ductules in a varying degree of fibrous stroma with cells of chronic inflammation[5]. We found similar features in our case. Furthermore, in the bile duct adenomas, the immunohistochemical stains including cytokeratin (CD) 7, CD10, and CD56 were positive. They also stained negative for CD20 and p53[13]. This was again similar to our case in which CD7 was positive and CD20, p53, and anti-human hepatocyte were negative, confirming the diagnosis of intrahepatic bile duct adenoma (peribiliary gland hamartoma). Treatment for symptomatic cases is surgical excision[14] and the overall prognosis is good after surgery.
Intrahepatic bile duct adenoma is an extremely rare benign tumor of liver occurring in children. Although it has a favorable prognosis, it is very difficult to differentiate from other malignancies, especially in the pediatric age group. We describe the first ever case of such a large pediatric BDA to date, which was originally thought to be a hepatoblastoma.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Horesh N, Kato J S-Editor: Ma RY L-Editor: Filipodia E-Editor: Zhang YL
| 1. | Allaire GS, Rabin L, Ishak KG, Sesterhenn IA. Bile duct adenoma. A study of 152 cases. Am J Surg Pathol. 1988;12:708-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 85] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Bhathal PS, Hughes NR, Goodman ZD. The so-called bile duct adenoma is a peribiliary gland hamartoma. Am J Surg Pathol. 1996;20:858-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Craig JR, Peters RL, Edmondson HA. Tumors of the liver and intrahepatic bile ducts. Atlas of tumor pathology; 2nd series, fascicle 26. Washington DC: Armed Forces Institute of Pathology 1989; 56-62. [DOI] [Full Text] |
| 4. | Hasebe T, Sakamoto M, Mukai K, Kawano N, Konishi M, Ryu M, Fukamachi S, Hirohashi S. Cholangiocarcinoma arising in bile duct adenoma with focal area of bile duct hamartoma. Virchows Arch. 1995;426:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Li Z, Sun X, Feng J. The first case of pediatric bile duct adenoma. J Pediatr Surg Case Rep. 2015;3:32-34. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Cho C, Rullis I, Rogers LS. Bile duct adenomas as liver nodules. Arch Surg. 1978;113:272-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Terada T, Nakanuma Y, Ohta G. Glandular elements around the intrahepatic bile ducts in man; their morphology and distribution in normal livers. Liver. 1987;7:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 73] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Terada T, Nakanuma Y. Morphological examination of intrahepatic bile ducts in hepatolithiasis. Virchows Arch A Pathol Anat Histopathol. 1988;413:167-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Nakanuma Y, Katayanagi K, Terada T, Saito K. Intrahepatic peribiliary glands of humans. I. Anatomy, development and presumed functions. J Gastroenterol Hepatol. 1994;9:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Nakanuma Y, Hoso M, Sanzen T, Sasaki M. Microstructure and development of the normal and pathologic biliary tract in humans, including blood supply. Microsc Res Tech. 1997;38:552-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Levin SE, Dail DH, Saik RP. Bile duct adenomatosis of the liver: a misleading finding on surgical exploration of the abdomen. Am Surg. 1975;41:106-108. [PubMed] |
| 12. | Hughes NR, Goodman ZD, Bhathal PS. An immunohistochemical profile of the so-called bile duct adenoma: clues to pathogenesis. Am J Surg Pathol. 2010;34:1312-1318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Albores-Saavedra J, Hoang MP, Murakata LA, Sinkre P, Yaziji H. Atypical bile duct adenoma, clear cell type: a previously undescribed tumor of the liver. Am J Surg Pathol. 2001;25:956-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Rafiq E, Alaradi O, Bawany M, Nawras A. A combination of snare polypectomy and apc therapy for prolapsing common bile duct adenoma. J Interv Gastroenterol. 2012;2:193-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |