Published online Jan 27, 2019. doi: 10.4240/wjgs.v11.i1.27
Peer-review started: November 5, 2018
First decision: November 27, 2018
Revised: December 11, 2018
Accepted: December 29, 2018
Article in press: December 30, 2018
Published online: January 27, 2019
Processing time: 85 Days and 14.1 Hours
Synovial sarcoma (SS) is a rare type of soft tissue sarcoma that is usually developed from areas where synovial tissue exists, especially at the extremities. Nevertheless, several cases of retroperitoneal SS (RSS) have been described. We herein report a case of RSS presented in our institution.
A 69-year-old female patient was admitted with a large, palpable, firm mass in the right abdominal space SS. Computerized tomography scan depicted a concentric, sharply marinated retro-peritoneal lesion which was displacing the right kidney and the lower edge of the liver. Subsequently, the patient underwent surgical excision of the mass with additional right nephrectomy and resection of the right adrenal gland and a part of the diaphragm. The final histological diagnosis of the tumour was grade II monophasic RSS.
RSS is encountered in the biphasic type, the monophasic fibrous, and the monophasic epithelial category as well. Relevant clinical manifestations are not always documented at early stages. Therefore, the final diagnosis is posed after complete histological examination taking into consideration the results of immunochemistry and genetic analysis. Therapeutic approach happens often late when metastases at the lungs and the liver are apparent. Thus, 5-year survival rates remain low.
Core tip: Synovial sarcoma (SS) is a rare type of soft tissue sarcoma that is usually developed from areas where synovial tissue exists, especially at the extremities. Nevertheless, several cases of retroperitoneal SS (RSS) have been described. Diagnosis is accomplished after complete histological examination taking into consideration the results of immunochemistry and genetic analysis. Therapeutic approach happens often late when metastases at the lungs and the liver are apparent. Thus, 5-year survival rates remain low. Despite recent research on the therapeutic strategies against RSS, surgical resection appears the only potentially curative approach.
- Citation: Mastoraki A, Schizas D, Papanikolaou IS, Bagias G, Machairas N, Agrogiannis G, Liakakos T, Arkadopoulos N. Management of primary retroperitoneal synovial sarcoma: A case report and review of literature. World J Gastrointest Surg 2019; 11(1): 27-33
- URL: https://www.wjgnet.com/1948-9366/full/v11/i1/27.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v11.i1.27
Synovial sarcoma (SS) is a rare type of soft tissue neoplastic disorder and accounts for 7%-8% of all relevant reported lesions[1]. It usually arises from areas where synovial tissue exists, especially at the extremities[2]. Nevertheless, several cases of retroperitoneal SS (RSS) have been described in the literature the last decades[3]. Although SS is more frequent in young males, it has been published that RSS affects both men and women aged from 13-52 years[4,5]. In terms of histology, SS has been encountered in the biphasic type, the monophasic fibrous, and the monophasic epithelial category as well. Relevant clinical manifestations are not always present at early stages and usually include non-specific abdominal pain, gastrointestinal (GI) obstruction, swelling of the lower extremities and the presence of a well-defined mass[6,7]. With regard to diagnostic modalities, RSS is usually detected by computerized tomography (CT), magnetic resonance imaging (MRI) and angiography[8]. However, the final diagnosis is established after complete histological examination taking into consideration the results of immunochemistry and genetic analysis[9,10]. As the neoplasm is relatively rare, a limited number of affected patients are available for study. In addition, recent surveys report a difficulty in understanding the molecular mechanism underlying the progression of the lesion. Moreover, RSS consists one of the most biologically virulent cancers and is difficult to cure by conventional procedures. Due to the fact that SS remains asymptomatic in its initial stage, patients may already present with additional pulmonary and hepatic metastatic disease[11-16]. As a result, treatment options are limited and consequently 5-year survival rates remain disappointingly low ranging from 20% to 29%[14]. Despite recent research on the therapeutic strategies against RSS, surgical resection appears the only potentially curative approach. Unfortunately, a mere minority of patients is eligible to undergo surgical intervention[12,14,16]. Furthermore, surgical removal of RSS does not necessarily guarantee patient’s long-term recovery. Alternative therapies, such as radio- and chemotherapy proved inadequate[6]. We herein report a case of RSS presented in our institution. Relevant literature is briefly reviewed. Clinical features, histogenesis, morphological and immunochemical findings are discussed, while the role of current diagnostic and therapeutic management of this uncommon entity is emphasized.
A 69-year-old female patient was presented with increasing right lumbar pain and vomiting for 15 d.
A 69-year-old female patient was admitted to our hospital with a 15-d history of increasing right lumbar pain, symptoms of incomplete bowel obstruction and vomiting. The patient presented with general malaise and loss of weight.
The patient had no previous disease.
Meticulous physical examination revealed a large, palpable, firm mass in the right abdominal space with a recrudescence of symptoms of anemia.
Apart from anaemia, common laboratory blood and urine examinations were within normal limits, whereas subsequent GI endoscopy was not indicative of pathologic findings.
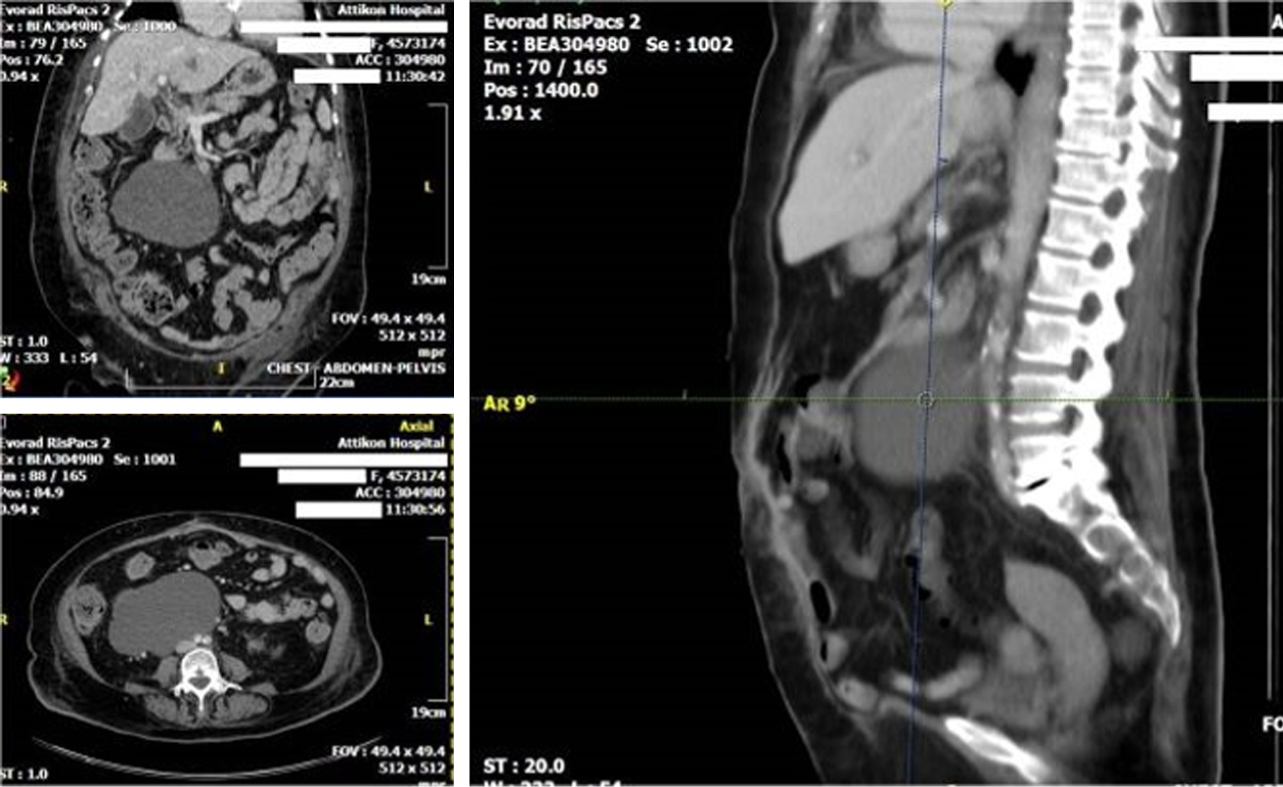
Erect abdominal X-rays depicted limited small bowel fluid levels, indicating intestinal obstruction. Ultrasonography (U/S) elucidated the suspicion of an abdominal cystic mass or haematoma. Subsequent CT scan depicted a concentric, sharply marginated retro-peritoneal lesion which was displacing the right kidney and the lower edge of the liver (Figure 1). Additional infiltration of the major psoas and quadratus lumborum muscles was documented while associated lymphadenopathy was not apparent. Imaging signs of complete intestinal obstruction were absent.
The final histological diagnosis of the tumour was grade II monophasic RSS.
In accordance with multimodality tumor board’s decision surgical treatment was implemented. Pre-operative U/S or CT guided biopsy was avoided as CT depiction was not indicative of lymphoma. In addition, neo-adjuvant administration of radio-therapy was recommended.
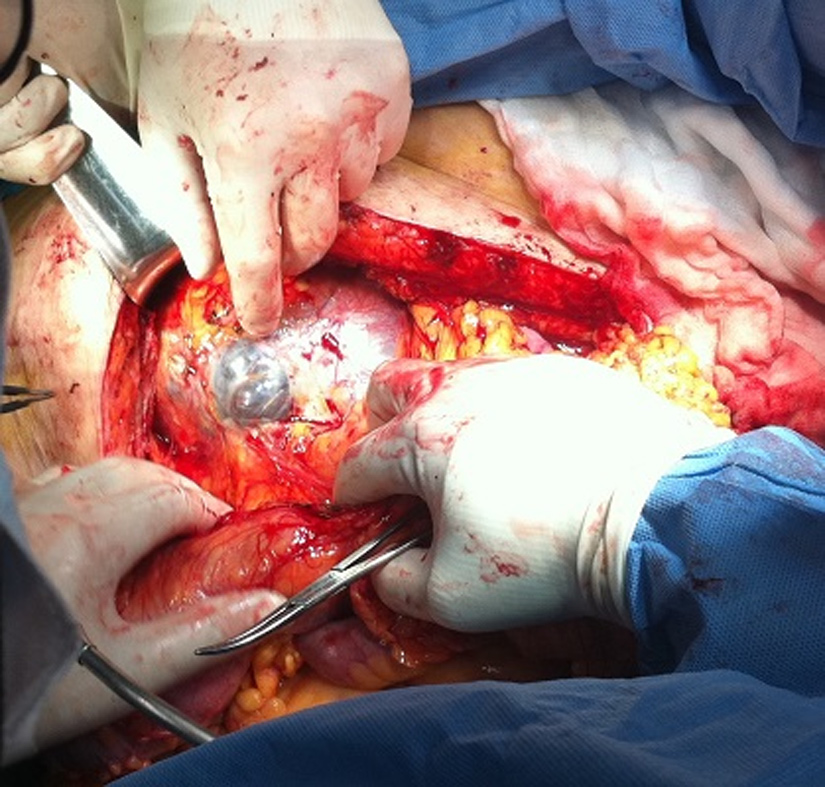
After optimisation of her condition, the patient underwent en bloc surgical excision of the mass with additional right nephrectomy and resection of the right adrenal gland and a part of the diaphragm while infiltration of the major psoas and quadratus lumborum muscles was not verified (Figure 2). Post-operatively, she was admitted to the intensive care unit for close monitoring, where she remained for 48 h. Macroscopically, the tumour measured 16 cm × 12 cm × 10 cm in size but did not appear to invade the kidney, the adrenal gland, the fat and the ureter after complete histological examination. It felt elastic and smooth and the surface was white-brown. Solid and cystic areas with residues of haemorrhage ranging from 1.5-9 cm in size were described. Histologically, the tumour presented a predominantly fascicular pattern of growth and it was consisted of ovoid and spindle cells with nonspecific cellular limits and mild to moderate atypia. An increased rate of mitotic activity was also detected. Moreover, sites of haemorrhage, fibrous tissue, degeneration of small vessels and a hemangiopericytomatous pattern at peripheral regions were documented.
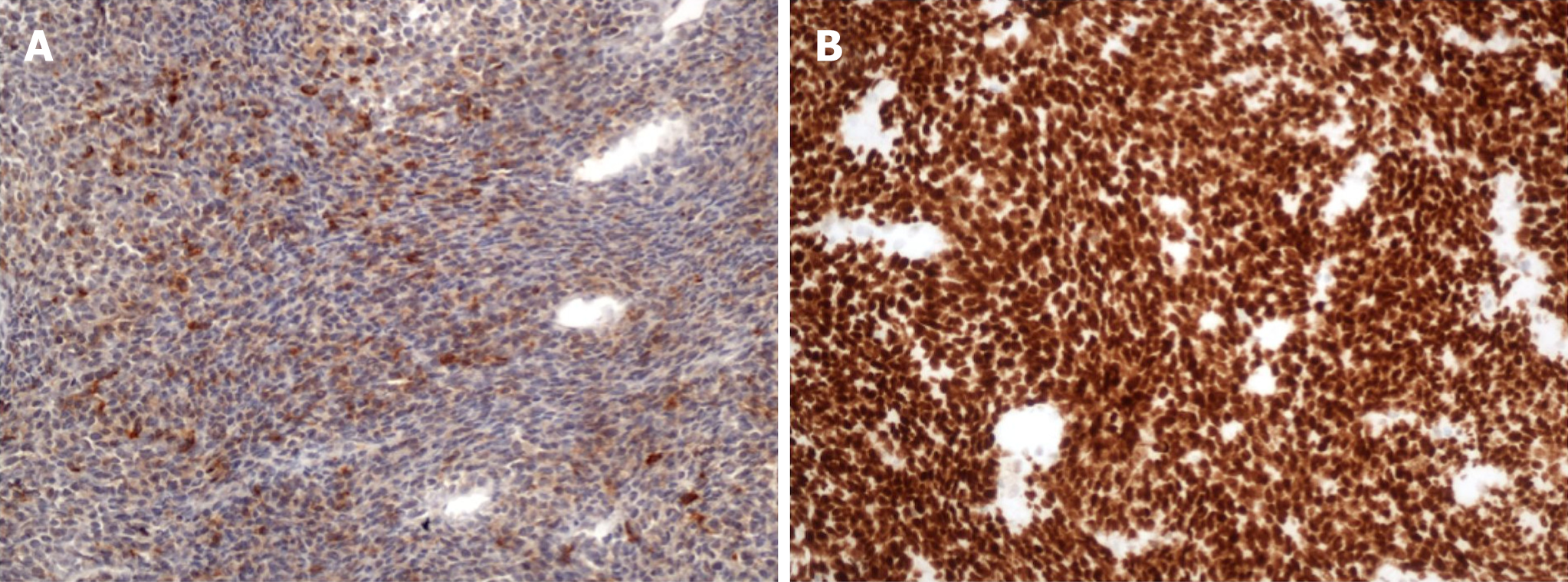
Immunohistochemical staining demonstrated intense positive reaction for vimentin, strong nuclear expression for TLE-1, diffuse expression of bcl-2 protein, and less for CD99, cytokeratins AE1/AE3, epithelial membrane antigen and cytokeratin 19 (Figure 3). Also, a small percentage of the nuclei were weakly positive for p53 protein. Finally, neoplastic cells were completely negative for SMA, HHF-35, h-caldesmon, desmin, myoglobin, CD34, CD68, CD117 and S-100. Additional meticulous genetic analysis detected the presence of the characteristic chromosomal translocation t(X;18)(p11;q11). Therefore, the final histological diagnosis of the tumour was grade II monophasic RSS. Hospital stay was uneventful and she was discharged from the surgical department 8 d postoperatively. Furthermore, according to our institution’s multimodality tumor board, she was administered adjuvant irradiation monotherapy. Finally, the last 60 mo, the patient remains under intense monitoring with CT and MRI of the brain, lungs and the abdomen without signs of relapse.
SS is described as an uncommon type of soft tissue sarcoma and represents approximately up to 10% of associated tumour category[17,18]. It mainly arises from sites with synovial tissue and 95% of the cases have been reported at the extremities, especially in young patients aged between 30 and 40 years old[2,5]. However, many SS cases located at the neck, tongue, abdominal wall, oesophagus and larynx have been described[19-21]. RSS accounts for 0.8%-8.3% of SS affected patients and approximately 21 cases have been detected so far since the first one in 1955, which was reported by Park and Tabah[1,17]. In this case report we refer to a female patient diagnosed with grade II monophasic RSS with sarcomatous spindle cell elements who was admitted at the department of surgery with predominant symptoms of increasing right lumbar pain and incomplete bowel obstruction.
RSs usually appear large in size due to the increased capacity of the retroperitoneal space. The majority of the tumours are asymptomatic at early stages and are incidentally diagnosed during imaging of the abdomen for other medical conditions. Symptomatic retroperitoneal tumours may present similar clinical manifestations with other abdominal neoplasms. Therefore, patients develop signs and symptoms of abdominal or back pain, GI, bowel or ureteral obstruction, anaemia and loss of weight[6,7]. In our case the patient was admitted with the presence of increasing right lumbar pain, vomiting, incomplete bowel obstruction, general malaise and relapse of symptoms of anaemia.
SS is further categorised in the biphasic type (with sarcomatous and epithelial components), the monophasic fibrous (with a predominance of sarcomatous spindle cell elements), the monophasic epithelial category and the poorly differentiated type respectively. Moreover, immunochemical examination is implemented for the differential diagnosis of SS from the other retroperitoneal masses as well as the presence of the characteristic t(X;18)(p11;q11) chromosomal translocation, which exists in more than 90% of the lesions and results in the production of a fusion protein responsible for the procedure of oncogenesis[6,9,10]. In our case, the SS was classified as grade II monophasic RSS with sarcomatous spindle cell elements. Immunohistochemical staining demonstrated intense positive reaction for vimentin, strong nuclear expression for TLE-1, diffuse expression of bcl-2 protein, and less for CD99, cytokeratins AE1/AE3, epithelial membrane antigen and cytokeratin 19, whereas relevant chromosomal translocation was present.
The diagnosis of RS is controversial throughout classic examination. Advanced imaging techniques are always warranted. Spiral CT remains the most valuable diagnostic modality which depicts the tumour as well as the adjacent organs and reveals potential metastatic lesions in the liver, lungs or the peritoneal cavity[22,23]. Moreover, CT distinguishes intra-abdominal and retroperitoneal neoplasms and elucidates the composition of the tumour. CT guided biopsy, alternatively to US, for assessing the therapeutic response has also been reported. MRI with oral or intravenous contrast is another diagnostic tool which displays cystic, necrotic, solid and enhancing areas along with the patency of inferior vena cava[24]. T1 weighted MRI images describe the relationship of the tumour with other adjacent solid organs while T2 weighted images indicate potential muscular invasion or development of the tumour near the spine. Nevertheless, definite diagnosis is accomplished with the histological identification following the biopsy of the tumour[9,10]. Similarly, in our patient, abdominal U/S suggested the presence of a cystic mass or haematoma. CT scan identified a concentric, sharply marginated retro-peritoneal lesion which was displacing the right kidney and the lower edge of the liver with expansion to major psoas and quadratus lumborum.
The treatment of choice for RS is aggressive surgical resection of the tumour along with concomitant regional lymphadenectomy. Additional en bloc resection of the adjacent affected organs including the kidney, colon, bladder, pancreas and the small bowel is often implemented[25-28]. In cases of vascular invasion of the tumour, wide excision accompanied by vascular reconstruction may be performed[27,29-31]. The role of preoperative or postoperative chemotherapy remains uncertain. Potential advantage of neoadjuvant chemotherapy, which reduces the size of the tumour and simplifies subsequent surgical operation, especially in large and high-grade tumours, has recently been reported[32,33]. In addition, patients who underwent adjuvant chemotherapy exhibited improved disease-free survival rates[34]. Radiation therapy alone has been implied as a complementary treatment modality to surgery either before or after the excision with no difference in survival rates[35,36]. Preoperative radiation is usually applied in highly selected cases with large tumours; however, some patients are presented with postoperative complications, such as wound infections. There are reports in the literature which suggest that neoadjuvant administration of chemotherapy combined with radiation may be beneficial, as well. Furthermore, as for SS, the results from chemotherapy remain controversial. Finally, recent publications support that excision of pulmonary and hepatic metastases may improve survival in certain patients[37]. The prognosis is really poor as the 5-year survival rate is only 20-29% and deteriorates when a high mitotic activity is detected. Local recurrence even after complete R0 surgical excision remains the most common cause of death[38].
In our case, we performed surgical resection of the mass with additional right nephrectomy and excision of the right adrenal gland as well as a part of the diaphragm. Post-operative course was uneventful and a month later, PET/CT scan of the whole body did not reveal any residues of the tumour; however, the patient was administered adjuvant irradiation therapy.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Gavriilidis P, Mohamed AA, Dinc B, Demetrashvili Z, Isik A S- Editor: Dou Y L- Editor: A E- Editor: Bian YN
| 1. | Fisher C. Synovial sarcoma. Ann Diagn Pathol. 1998;2:401-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 235] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 2. | Cadman NL, Soule EH, Kelly PJ. Synovial Sarcoma; An Analysis Of 34 Tumors. Cancer. 1965;18:613-627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Girszyn N, Mabro M, Kahn JE, Roullet-Audy JC, Sautet A, Bletry O. [Primary retroperitoneal synovial sarcoma revealed by hemorrhagic shock]. Presse Med. 2006;35:1185-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Shmookler BM. Retroperitoneal synovial sarcoma. A report of four cases. Am J Clin Pathol. 1982;77:686-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Felix EL, Wood DK, Das Gupta TK. Tumors of the retroperitoneum. Curr Probl Cancer. 1981;6:1-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Mullinax JE, Zager JS, Gonzalez RJ. Current diagnosis and management of retroperitoneal sarcoma. Cancer Control. 2011;18:177-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Storm FK, Eilber FR, Mirra J, Morton DL. Retroperitoneal sarcomas: a reappraisal of treatment. J Surg Oncol. 1981;17:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 59] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Davidson AJ, Hartman DS. Imaging strategies for tumors of the kidney, adrenal gland, and retroperitoneum. CA Cancer J Clin. 1987;37:151-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Sreekantaiah C, Ladanyi M, Rodriguez E, Chaganti RS. Chromosomal aberrations in soft tissue tumors. Relevance to diagnosis, classification, and molecular mechanisms. Am J Pathol. 1994;144:1121-1134. [PubMed] |
| 10. | Clark J, Rocques PJ, Crew AJ, Gill S, Shipley J, Chan AM, Gusterson BA, Cooper CS. Identification of novel genes, SYT and SSX, involved in the t(X;18)(p11.2;q11.2) translocation found in human synovial sarcoma. Nat Genet. 1994;7:502-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 576] [Cited by in RCA: 563] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 11. | Braasch JW, Mon AB. Primary retroperitoneal tumors. Surg Clin North Am. 1967;47:663-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 93] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Cody HS, Turnbull AD, Fortner JG, Hajdu SI. The continuing challenge of retroperitoneal sarcomas. Cancer. 1981;47:2147-2152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Karakousis CP, Velez AF, Emrich LJ. Management of retroperitoneal sarcomas and patient survival. Am J Surg. 1985;150:376-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Dalton RR, Donohue JH, Mucha P, van Heerden JA, Reiman HM, Chen SP. Management of retroperitoneal sarcomas. Surgery. 1989;106:725-32; discussion 732-3. [PubMed] |
| 15. | McGrath PC, Neifeld JP, Lawrence W, DeMay RM, Kay S, Horsley JS, Parker GA. Improved survival following complete excision of retroperitoneal sarcomas. Ann Surg. 1984;200:200-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 110] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Glenn J, Sindelar WF, Kinsella T, Glatstein E, Tepper J, Costa J, Baker A, Sugarbaker P, Brennan MF, Seipp C. Results of multimodality therapy of resectable soft-tissue sarcomas of the retroperitoneum. Surgery. 1985;97:316-325. [PubMed] |
| 17. | PACK GT, TABAH EJ. Primary retroperitoneal tumors: a study of 120 cases. Int Abstr Surg. 1954;99:313-341. [PubMed] |
| 18. | Leader M, Patel J, Collins M, Kristin H. Synovial sarcomas. True carcinosarcomas? Cancer. 1987;59:2096-2098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Oppedal BR, Røyne T, Titterud I. Synovial sarcomas of the neck. A report of two cases. J Laryngol Otol. 1985;99:101-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Pruszczynski M, Manni JJ, Smedts F. Endolaryngeal synovial sarcoma: case report with immunohistochemical studies. Head Neck. 1989;11:76-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Bloch MJ, Iozzo RV, Edmunds LH, Brooks JJ. Polypoid synovial sarcoma of the esophagus. Gastroenterology. 1987;92:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Liles JS, Tzeng CW, Short JJ, Kulesza P, Heslin MJ. Retroperitoneal and intra-abdominal sarcoma. Curr Probl Surg. 2009;46:445-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Lahat G, Madewell JE, Anaya DA, Qiao W, Tuvin D, Benjamin RS, Lev DC, Pollock RE. Computed tomography scan-driven selection of treatment for retroperitoneal liposarcoma histologic subtypes. Cancer. 2009;115:1081-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Raut CP, Pisters PW. Retroperitoneal sarcomas: Combined-modality treatment approaches. J Surg Oncol. 2006;94:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Daylami R, Amiri A, Goldsmith B, Troppmann C, Schneider PD, Khatri VP. Inferior vena cava leiomyosarcoma: is reconstruction necessary after resection? J Am Coll Surg. 2010;210:185-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 81] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Pisters PW, Ballo MT, Fenstermacher MJ, Feig BW, Hunt KK, Raymond KA, Burgess MA, Zagars GK, Pollock RE, Benjamin RS, Patel SR. Phase I trial of preoperative concurrent doxorubicin and radiation therapy, surgical resection, and intraoperative electron-beam radiation therapy for patients with localized retroperitoneal sarcoma. J Clin Oncol. 2003;21:3092-3097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 109] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Gieschen HL, Spiro IJ, Suit HD, Ott MJ, Rattner DW, Ancukiewicz M, Willett CG. Long-term results of intraoperative electron beam radiotherapy for primary and recurrent retroperitoneal soft tissue sarcoma. Int J Radiat Oncol Biol Phys. 2001;50:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 157] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 28. | Bonvalot S, Rivoire M, Castaing M, Stoeckle E, Le Cesne A, Blay JY, Laplanche A. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009;27:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 446] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 29. | Gronchi A, Lo Vullo S, Fiore M, Mussi C, Stacchiotti S, Collini P, Lozza L, Pennacchioli E, Mariani L, Casali PG. Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol. 2009;27:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 350] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 30. | Russo P, Kim Y, Ravindran S, Huang W, Brennan MF. Nephrectomy during operative management of retroperitoneal sarcoma. Ann Surg Oncol. 1997;4:421-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Stauffer JA, Fakhre GP, Dougherty MK, Nakhleh RE, Maples WJ, Nguyen JH. Pancreatic and multiorgan resection with inferior vena cava reconstruction for retroperitoneal leiomyosarcoma. World J Surg Oncol. 2009;7:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 32. | Eilber FC, Rosen G, Eckardt J, Forscher C, Nelson SD, Selch M, Dorey F, Eilber FR. Treatment-induced pathologic necrosis: a predictor of local recurrence and survival in patients receiving neoadjuvant therapy for high-grade extremity soft tissue sarcomas. J Clin Oncol. 2001;19:3203-3209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 242] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 33. | Meric F, Hess KR, Varma DG, Hunt KK, Pisters PW, Milas KM, Patel SR, Benjamin RS, Plager C, Papadopoulos NE, Burgess MA, Pollock RE, Feig BW. Radiographic response to neoadjuvant chemotherapy is a predictor of local control and survival in soft tissue sarcomas. Cancer. 2002;95:1120-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 85] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 34. | Eilber FC, Eilber KS, Eilber FR. Retroperitoneal sarcomas. Curr Treat Options Oncol. 2000;1:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 35. | Caudle AS, Tepper JE, Calvo BF, Meyers MO, Goyal LK, Cance WG, Kim HJ. Complications associated with neoadjuvant radiotherapy in the multidisciplinary treatment of retroperitoneal sarcomas. Ann Surg Oncol. 2007;14:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Ballo MT, Zagars GK, Pollock RE, Benjamin RS, Feig BW, Cormier JN, Hunt KK, Patel SR, Trent JC, Beddar S, Pisters PW. Retroperitoneal soft tissue sarcoma: an analysis of radiation and surgical treatment. Int J Radiat Oncol Biol Phys. 2007;67:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 37. | Blackmon SH, Shah N, Roth JA, Correa AM, Vaporciyan AA, Rice DC, Hofstetter W, Walsh GL, Benjamin R, Pollock R, Swisher SG, Mehran R. Resection of pulmonary and extrapulmonary sarcomatous metastases is associated with long-term survival. Ann Thorac Surg. 2009;88:877-84; discussion 884-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 38. | Kim DH, Joo KR, Cha JM, Shin HP, Lee JI, Park JJ, Kim HS, Yang DM. Retroperitoneal synovial sarcoma manifested by obstructive jaundice in an elderly woman: case report. Clin Endosc. 2012;45:428-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |