Published online Jan 27, 2018. doi: 10.4240/wjgs.v10.i1.1
Peer-review started: November 1, 2017
First decision: December 1, 2017
Revised: December 4, 2017
Accepted: December 13, 2017
Article in press: December 13, 2017
Published online: January 27, 2018
Processing time: 86 Days and 2.3 Hours
Alveolar echinococcosis (AE) is a zoonotic disease that is caused by Echinococcus multilocularis that affects liver and a variety of organs and tissues. It differs from other echinococcal disease because it shows tumor like behavior in the affected organ and tissues. The treatment of choice is concomitant medical therapy and resection with negative margins. Nevertheless, resection with the intent of negative margins (R0) may lead to serious complications such as liver failure. In the present case report, we used Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) procedure, which was defined in 2012 by Schnitzbauer et al, in a 28-year-old male patient to avoid complications of major liver resection in order to treat alveolar echinococcosis. Until now, we have not encountered any study using ALPPS procedure for the treatment of alveolar echinococcosis. In the present case report we aimed to show that ALPPS procedure can be safely performed for margin-negative resection of primary or recurrent AE that shows a tumor like behavior. It is our opinion that this procedure should be performed in centers that have expertise and sufficient technical capacity to perform liver transplantation and advanced liver surgery.
Core tip: We have shown the feasibility and efficacy of Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) procedure -initially described for the resection of advanced tumors including colorectal liver metastasis, hilar cholangiocarcinoma and to a lesser extent hepatocellular carcinoma-in resection of recurrent hepatic alveolar echinococcosis in a young patient. In selected patient groups with benign liver disease with extensive hepatic involvement ALPPS can be safely used in centers which have expertise in liver transplantation and major hepatic surgery. According to our knowledge, the present patient is the first extensive hepatic AE case that ALPPS procedure has been applied in the literature.
- Citation: Akbulut S, Cicek E, Kolu M, Sahin TT, Yilmaz S. Associating liver partition and portal vein ligation for staged hepatectomy for extensive alveolar echinococcosis: First case report in the literature. World J Gastrointest Surg 2018; 10(1): 1-5
- URL: https://www.wjgnet.com/1948-9366/full/v10/i1/1.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v10.i1.1
Alveolar echinococcosis (AE) is a zoonotic disease that primarily affects the liver but has the potential for local invasion and metastasis to brain, lung and bones. Therefore; although it seems to be a parasitic disease, it has the clinical behavior of a malignancy[1]. The growth pattern of the parasite determines the biologic behavior of the disease. Usually the disease exceeds the pseudo-membrane formed by the compressed fibrotic liver tissue and compresses the intrahepatic biliary and vascular structures. This causes diverse clinical presentation including adjacent organ compression symptoms, portal hypertension or hepatic outflow obstruction. In addition to all; invasion of the main vascular structures cause metastasis of the parasite[2]. Conservative treatment options include benzimidazole derivatives and percutaneous therapy such as puncture-aspiration-injection-reaspiration, percutaneous evacuation, modified catheterization technique, dilatable multi-function trocar. However, parasite can be dormant for a long time before overt symptoms emerge and most of the patients are diagnosed in the late stages of the disease. Therefore; radical resection and/or liver transplantation seems to be the only sustainable definitive treatment of the disease. However the operation is hard and time consuming requiring multiple organ resection and intraoperative transfusions[3]. Liver resection is often precluded by the fact that disease reaches extensive sizes and reduces the remnant functional liver volume.
Associating liver Partition and Portal vein ligation for Staged hepatectomy (ALPPS) was initially described in 2012 by Schnitzbauer et al[4] for the resection of advanced tumors including colorectal liver metastasis, hilar cholangiocarcinoma and to a lesser extent hepatocellular carcinoma[3]. It provides the means for resection of tumors that is not possible by single stage procedure due to insufficient hepatic reserve postoperatively[5]. Although there are technical variations and controversies the conventional ALPPS procedure includes full mobilization of the liver from its attachments, dissection of the retro-hepatic vena cava, ligation of the right main branch of the portal vein and transection of the liver parenchyma at the Falciform ligament or the Cantlie’s line together with isolation of the right and left livers by polyester or bio-absorbable synthetic material as the initial stage. The second stage that includes the resection of the right lobe is usually performed 7 ± 2 d later after evaluation of the hypertrophy of the remnant liver[6]. The procedure causes enhanced hypertrophy of the remnant liver (60%-90%) in a shorter period when compared to conventional radiologic portal vein occlusion (10 d vs 40 d)[7]. Its use in hepatic EA has not been previously. In the present study, we report a successful ALPPS procedure in 28 years old male patient with hepatic alveolar echinococcosis which is the first report of use of ALPPS in a hepatic hydatic disease.
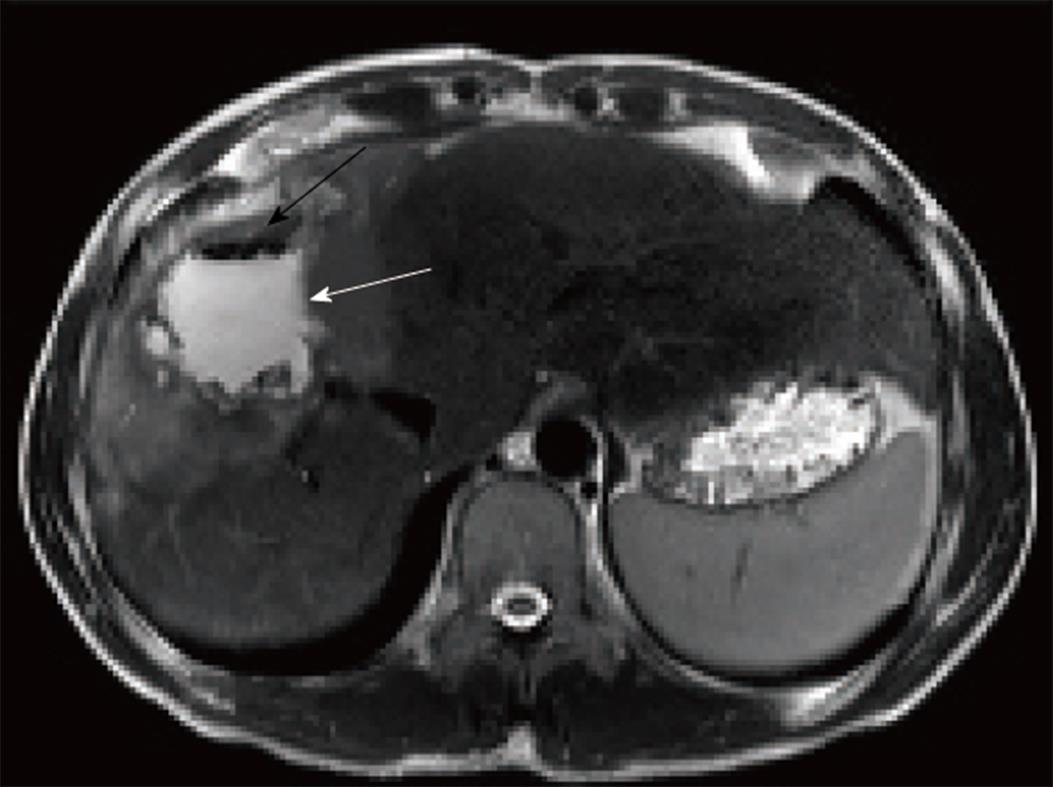
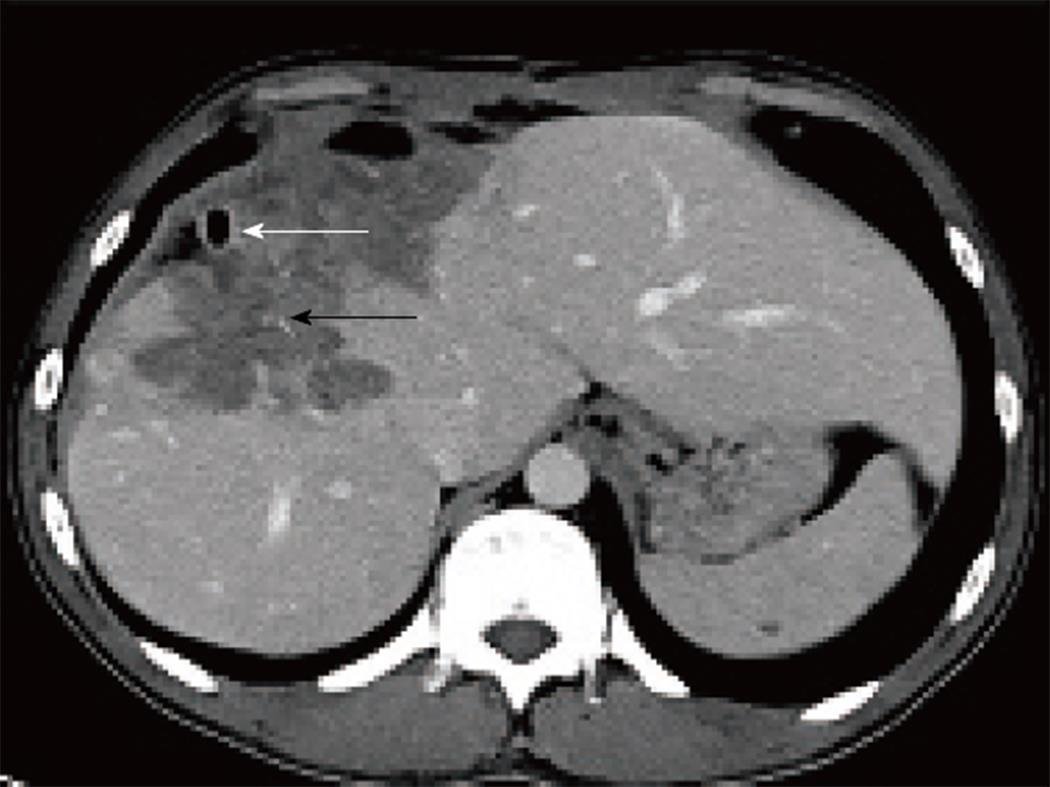
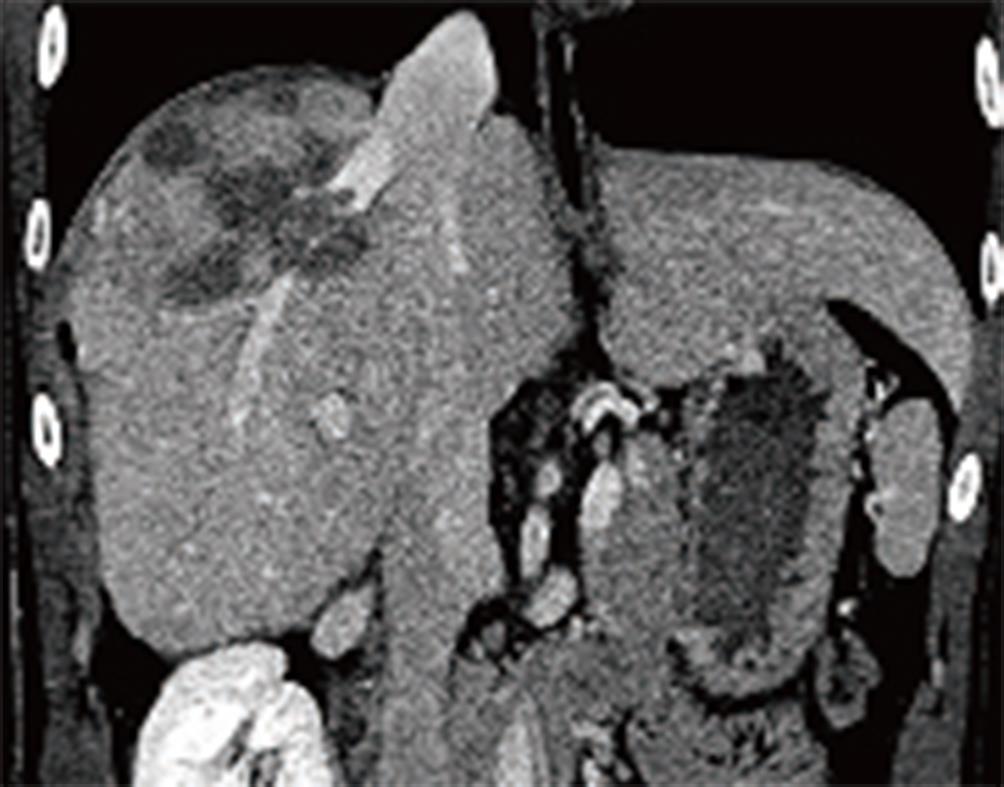
A 28-year-old male patient with recurrent AE was referred to our Liver Transplant Center. Patient history revealed that patient had been on medical therapy for a long time and had been operated twice 1 year prior to admission to our center. In addition, he had received two percutaneous hepatic abscess drainage by interventional radiology. Physical examination of the patient showed that there was subcostal incision and distal to the incision there were two 7 Fr drainage catheters. Laboratory evaluation of the patient was as follows: hemoglobin: 12.6 g/dL; white blood cell count: 27.400; platelet count 480.000, galactosylhydroxylysyl: 113 U/L; ALP: 104 U/L, total bilirubin: 1.13 mg/dL, AST: 373 U/L, ALT: 268 U/L ve INR: 1.3. In order to evaluate the extent of the resectability of the disease both contrast enhanced multidetector computerized tomography (MDCT) and dynamic liver magnetic resonance imaging were obtained (Figures 1-3). In the MDCT, it was seen that there was a hypodense, lobulated masses in segment 4-8 that was 13 cm × 7.5 cm in diameter and had peripheral contrast enhancements in the post-contrast images. Furthermore, the right hepatic vein and the anterior branch of the right portal vein could not be identified. MDCT and the patient’s clinical situation was evaluated all together and decided that an extended right hepatectomy may result in hepatic failure and organ allocation in the emergency setting may be difficult. Therefore, we decided to perform ALPPS procedure in order to provide segment 2-3 hypertrophy in this patient. A laparotomy was performed thorugh the old incision of the patient and dissection and mobilization of the liver took 4 h. The right hepatic lobe was completely dissected away from the inferior vena cava and the right hepatic vein was completely identified to perform ALPPS procedure. This was followed by the hilar dissection and identification of the right hepatic artery originating from the superior mesenteric artery and the bile duct bifurcation was identified and marked by a vascular tape. The right branch of portal vein was identified and transected using a vascular stapler. Hepatic parenchyma transection was performed using cavitron ultrasonic surgical aspirator (CUSA; ValleyLab, Boulder, CO, United States) so that extended right hepatectomy can be performed leaving segment 2 and 3 intact. In order to prevent parenchymal adhesion a drape covered sheet barrier was inserted in to the transection plane. The postoperative course was uneventful and the patient was re-operated for definitive procedure in the postoperative eighth day. The right hepatic artery, right hepatic vein and the bile duct was transected without any problem.
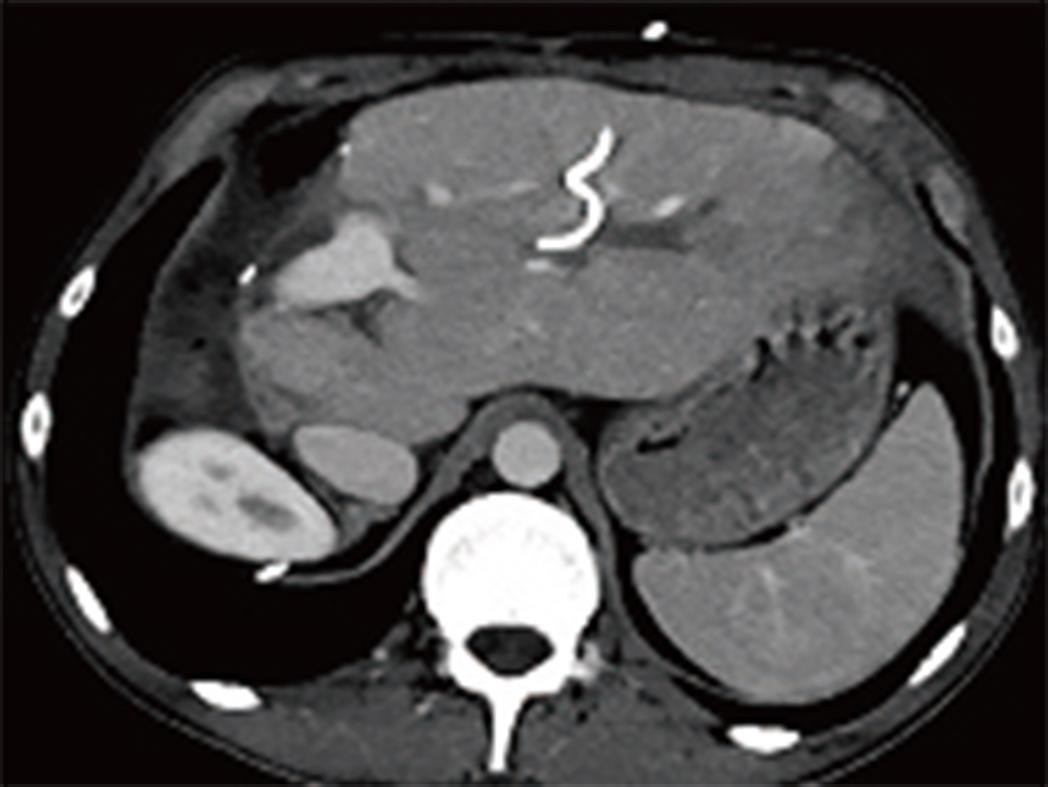
Serum bilirubin and GGT levels of the patient were elevated in the postoperative course. Endoscopic retrograde cholangio-pancreatico-ductography was attempted but failed and a percutaneous trans-hepatic cholangiogram (PTC) guided drainage catheter was inserted. PTC showed severe stenosis of the biliary tract and the guide wire could not be inserted in to the common bile duct. The patient was discharged with an external biliary drainage catheter (Figure 4). PTC guided intervention was repeated after the patient’s general condition improved and again showed severe stenosis preventing any intervention. A surgical exploration was planned. A guide wire was inserted through the drainage catheter and the left branch of the bile duct was identified. Roux-en-Y Hepaticojejunostomy was performed. A control cholangiogram performed on the postoperative 6th week showed that contrast flow through the anastomosis was normal. The drainage catheter was extracted and patient was followed up with a six months course of albendazole therapy (Figure 5).
AE can be located in almost every organ or tissue of the body, although the liver is the most commonly involved organ. It has a multi-vesicular and invasive clinical behavior. Furthermore, it shows hematogenous metastasis to distant organs such as the brain, lung and bone[8]. Mortality rate is high in untreated, extensive or distant organ metastasis cases (90% within 10 years, about 100% within 15 years after the onset of 15 years)[1]. It is an extensive disease of the liver and in 70% of the cases right lobe is affected and 20% of the cases show bilateral involvement. At the time of the diagnosis, in 40% of the cases hepatic hilum is involved[9]. Margin negative resection and medical therapy provides the only chance of cure. Radical resection rates have been reported to be between 15%-85% changing according to the extent of the disease[10]. In Turkey, Aydinli et al[11] have reported the resection rate to be 47% in their series. Otherwise, patients with unresectable lesions, liver failure, recurrent cholangitis are bound for liver transplantation which accounts for 14% of the cases[11,12]. In the majority of patients with unresectable alveolar echinococcosis cases require lifelong medical therapy with antihelminthics and amphotericine B, all of which have only modest efficacy in disease control. Therefore, we thought that ALPPs treatment may be an alternative treatment modality in approach to extensive AE disease in cases where surgical treatment is thought to be impossible.
ALPPS is the procedure of choice in the extensive liver lesions with marginal resectability and borderline future remnant liver volumes. Schadde et al[13] have reported that ALPPS provided margin negative (R0) resection in 91% of the cases with various hepatic malignancies. They reported the morbidity and mortality of ALPPS was 40% and 11%; respectively[13]. Therefore; it should be performed in centers with experience in liver surgery and transplantation such as our liver transplant center. Our Liver Transplant Center is highly experienced in liver surgery and has an average of 400 liver operations per year including 210-220 liver transplantation and 180-200 liver resection. Our experience on ALPPS procedure has begun to increase in the last year and we often apply it to primary and metastatic tumors of the liver. According to our knowledge, the present patient is the first extensive hepatic AE case that ALPPS procedure has been applied in the literature.
Embolization of the portal vein branches have been used for induction of hypertrophy of the future remnant liver. ALPPS seems to be superior in degree of induction of remnant liver hypertrophy and it seems to induce this hypertrophy in shorter period when compared to portal vein embolization[14]. Therefore, in hepatic tumors with borderline resectability ALPPS is a good alternative to portal vein embolization that provide high resectability rates in cases with hepatic tumors who can tolerate major abdominal surgery. Use of ALPPS procedure for benign liver tumors or parasitic infestations have not been reported until now.
In the present case, our patient was a twenty-eight years old male patient with extensive hepatic AE occupying right lobe and segment 4 of the liver. There are several reasons regarding our choice of ALPPS procedure in our patient. First of all, our patient was young and his medical condition tolerated such a major hepatic surgery. Secondly, attempt to perform embolization of the right branch of portal vein could have failed because the MDCT images showed invasion and occlusion of right portal and right hepatic veins. Furthermore, there have been two attempts for surgery in the medical history which did not succeed. Therefore, we believed that ALPPS procedure could provide necessary hypertrophy in the future liver remnant in a considerably shorter period and provide means for radical resection.
In conclusion, in the present study we have shown the feasibility and efficacy of ALPPS procedure in resection of recurrent hepatic alveolar echinococcosis in a young patient. In selected patient groups with benign liver disease with extensive hepatic involvement ALPPS can be safely used in centers which have expertise in liver transplantation and major hepatic surgery.
A 28-years-old male patient was referred to our Liver Transplant Center because of recurrent advanced alveolar echinococcosis.
The patient was diagnose with extensive hepatic alveolar echinococcosis.
The different diagnosis was many malignant liver tumors.
An elevated blood AST and ALT levels suggested parenchymal damage.
Both multidetector computerized tomography and dynamic liver magnetic resonance imaging demonstrated extensive hepatic alveolar echinococcosis.
Alveolar echinococcosis.
Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy.
According to our knowledge, the present patient is the first extensive hepatic AE case that ALPPS procedure has been applied in the literature.
ALPPS: Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy.
In selected patient groups with benign liver disease with extensive hepatic involvement ALPPS can be safely used in centers which have expertise in major hepatic surgery.
Manuscript source: Invited Manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Harizanov RN S- Editor: Cui LJ L- Editor: A E- Editor: Song XX
| 1. | Maddah G, Abdollahi A, Sharifi-Nooghabi R, Tavassoli A, Rajabi-Mashadi MT, Jabbari-Nooghabi A, Jabbari-Nooghabi M. Difficulties in the diagnosis and management of alveolar hydatid disease: A case series. Caspian J Intern Med. 2016;7:52-56. [PubMed] |
| 2. | Poyrazoglu OK, Ataseven H, Bektas S, Aydin A, Yalniz M, Celebi S, Bahcecioglu IH. Portal hypertension due to Echinococcus alveolaris: a case report. Acta Medica (Hradec Kralove). 2007;50:57-59. [PubMed] |
| 3. | Ozdemir F, Ince V, Barut B, Onur A, Kayaalp C, Yilmaz S. Living donor liver transplantation for Echinococcus Alveolaris: single-center experience. Liver Transpl. 2015;21:1091-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Hörbelt R. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 931] [Article Influence: 71.6] [Reference Citation Analysis (0)] |
| 5. | Vivarelli M, Vincenzi P, Montalti R, Fava G, Tavio M, Coletta M, Vecchi A, Nicolini D, Agostini A, Ahmed EA. ALPPS Procedure for Extended Liver Resections: A Single Centre Experience and a Systematic Review. PLoS One. 2015;10:e0144019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Bertens KA, Hawel J, Lung K, Buac S, Pineda-Solis K, Hernandez-Alejandro R. ALPPS: challenging the concept of unresectability--a systematic review. Int J Surg. 2015;13:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Donati M, Basile F, Oldhafer KJ. Present status and future perspectives of ALPPS (associating liver partition and portal vein ligation for staged hepatectomy). Future Oncol. 2015;11:2255-2258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Farrokh D, Zandi B, Pezeshki Rad M, Tavakoli M. Hepatic alveolar echinococcosis. Arch Iran Med. 2015;18:199-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 9. | Kratzer W, Gruener B, Kaltenbach TE, Ansari-Bitzenberger S, Kern P, Fuchs M, Mason RA, Barth TF, Haenle MM, Hillenbrand A. Proposal of an ultrasonographic classification for hepatic alveolar echinococcosis: Echinococcosis multilocularis Ulm classification-ultrasound. World J Gastroenterol. 2015;21:12392-12402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 10. | Joliat GR, Melloul E, Petermann D, Demartines N, Gillet M, Uldry E, Halkic N. Outcomes After Liver Resection for Hepatic Alveolar Echinococcosis: A Single-Center Cohort Study. World J Surg. 2015;39:2529-2534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Aydinli B, Ozturk G, Arslan S, Kantarci M, Tan O, Ahıskalioglu A, Özden K, Colak A. Liver transplantation for alveolar echinococcosis in an endemic region. Liver Transpl. 2015;21:1096-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, Madeddu G, Malaguarnera G, Pavone P, Cappellani A, Cacopardo B. Hepatic echinococcosis: clinical and therapeutic aspects. World J Gastroenterol. 2012;18:1448-1458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 241] [Cited by in RCA: 226] [Article Influence: 17.4] [Reference Citation Analysis (1)] |
| 13. | Schadde E, Schnitzbauer AA, Tschuor C, Raptis DA, Bechstein WO, Clavien PA. Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: associating liver partition and portal vein ligation for staged hepatectomy. Ann Surg Oncol. 2015;22:3109-3120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | Eshmuminov D, Raptis DA, Linecker M, Wirsching A, Lesurtel M, Clavien PA. Meta-analysis of associating liver partition with portal vein ligation and portal vein occlusion for two-stage hepatectomy. Br J Surg. 2016;103:1768-1782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 109] [Article Influence: 12.1] [Reference Citation Analysis (0)] |