Copyright
©2013 Baishideng Publishing Group Co.
World J Gastrointest Surg. Mar 27, 2013; 5(3): 51-61
Published online Mar 27, 2013. doi: 10.4240/wjgs.v5.i3.51
Published online Mar 27, 2013. doi: 10.4240/wjgs.v5.i3.51
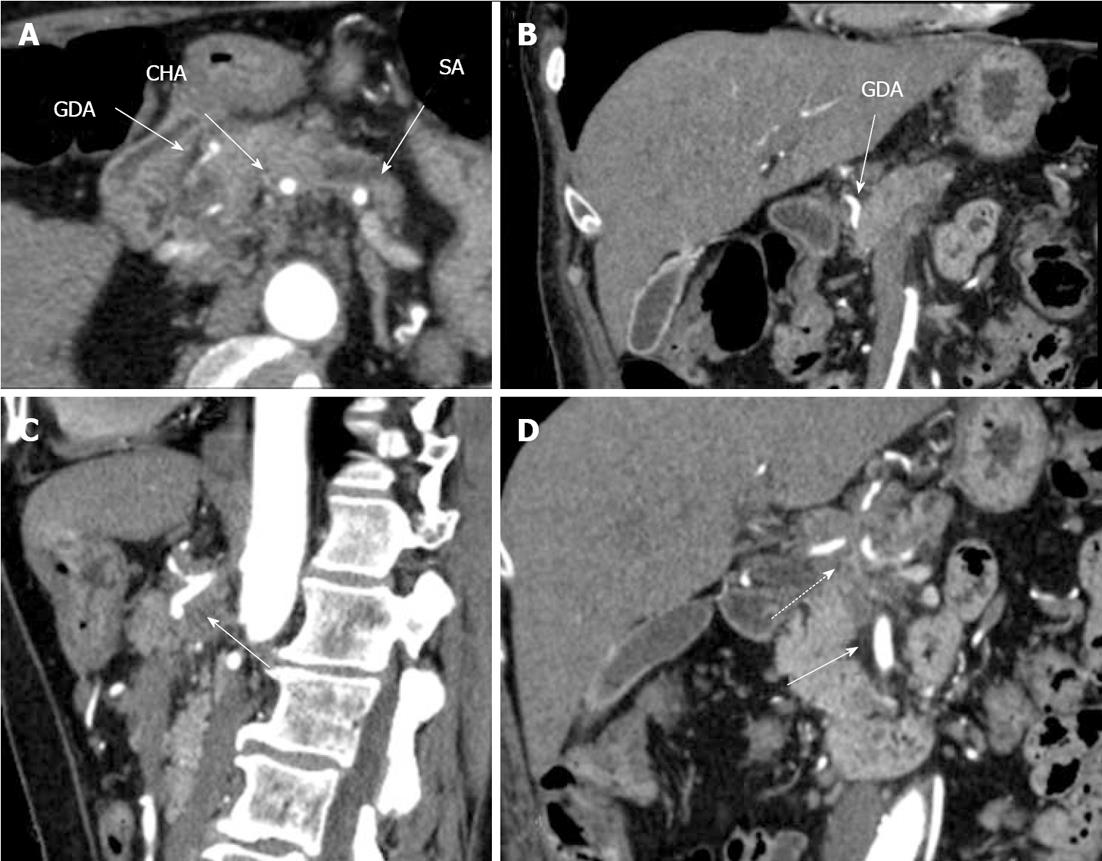
Figure 1 Preoperative computed tomography.
Arterial phase. A: Axial image. The common hepatic (CHA) and splenic (SA) arteries present circumferential adjacency to pancreatic body ductal adenocarcinoma. The gastroduodenal artery (GDA) appears to be completely encircled by tumor; B: Frontal view. Computed tomography (CT) evidences circumferential infiltration of GDA; C: The celiac artery (CA) along with CHA springing from it, are completely circumscribed by tumor (arrow); D. All three CA branches (dashed arrow) show circumferential tumor contact. The superior mesenteric artery is unaffected (arrow).
Figure 2 Three-dimensional computed tomography-angiography before surgery.
Classical arterial architecture (Michels, type I). Tumor-induced common hepatic (CHA) stenosis is noted. Anatomical variation of type I is observed: CHA trifurcation in the absence of proper hepatic artery. RHA: Right hepatic artery; LHA: Left hepatic artery; GDA: Gastroduodenal artery; LGA: Left gastric artery; SMA: Superior mesenteric artery; SA: Splenic artery; aLHA: Accessory left hepatic artery.
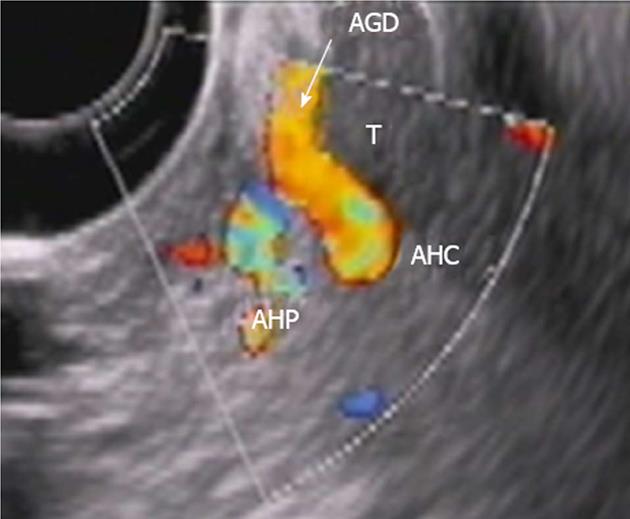
Figure 3 Endoscopic ultrasound.
Tumor (T) abutment to gastroduodenal artery (AGD and arrow) without its encasement. HAC: Common hepatic, HAP: Proper hepatic artery.
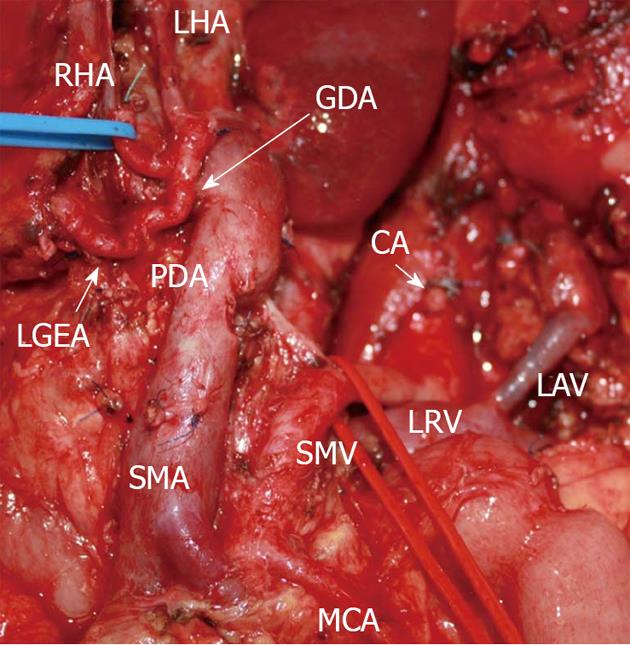
Figure 4 Photograph.
View of operating field after distal pancreatectomy with excision of celiac artery (CA) and its branches. Liver and stomach are fed with blood from the superior mesenteric artery (SMA) via pancreaticoduodenal arcade (PDA) and, thereafter, through the gastroduodenal artery (GDA). Full-blown right gastro-epiploic artery is found. Superior mesenteric vein (SMV) was resected at the site of confluence with splenic vein. LAV: Left adrenal vein; MCA: Medial colic; RHA: Right hepatic; LHA: Left hepatic arteries; LRV: Left renal vein; LGEA: Left gastro-epiploic artery.
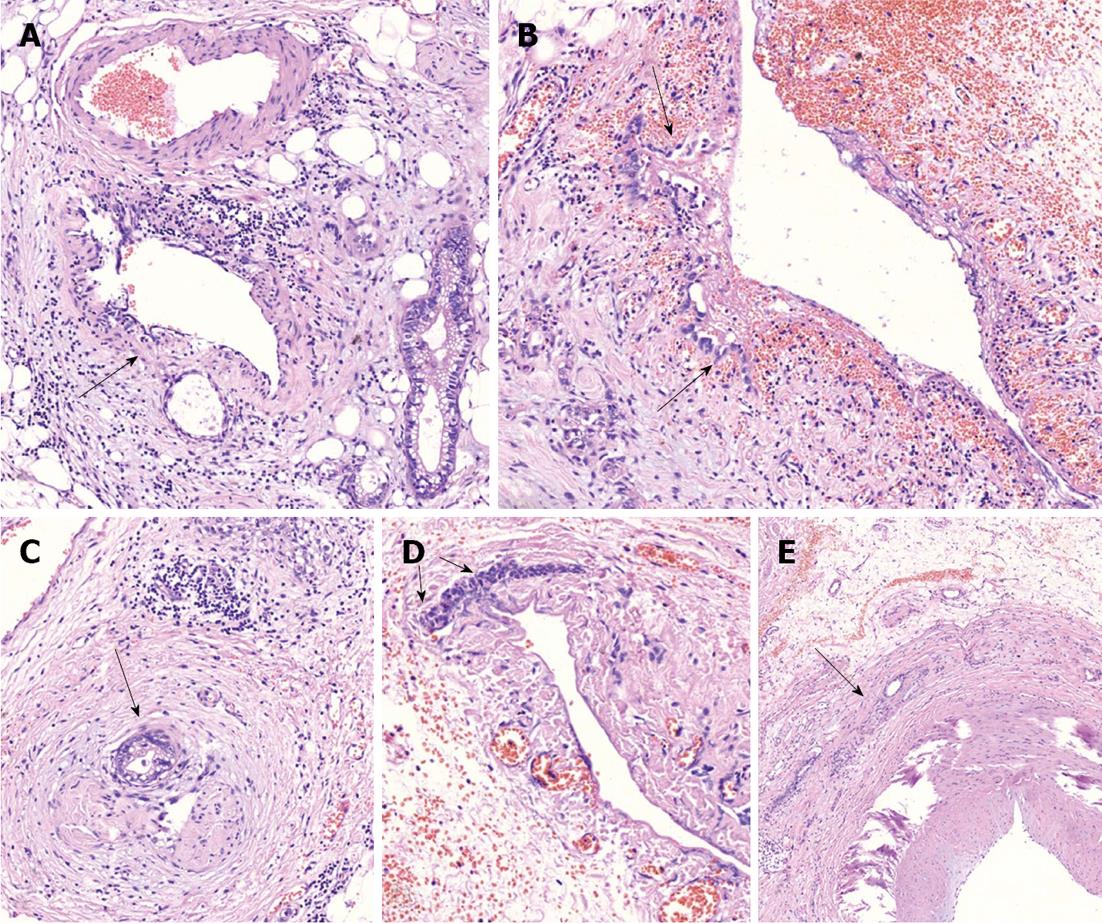
Figure 5 On microscopic examination.
A: Perivascular tumor growth (complexes of malignant cells in adventitia of small artery of peripancreatic fat (arrow), HE, × 200; B: Tumor incursion into vein wall (arrow), HE, x 200; C. invasion of the nerve by the tumor (arrow), HE, x 50; D: Vein wall involvement (complexes of malignant cells in media of 2-mm diameter vein (arrows), HE, × 50; E: Tumor complexes in the common hepatic artery adventitia (arrow), HE, × 50.
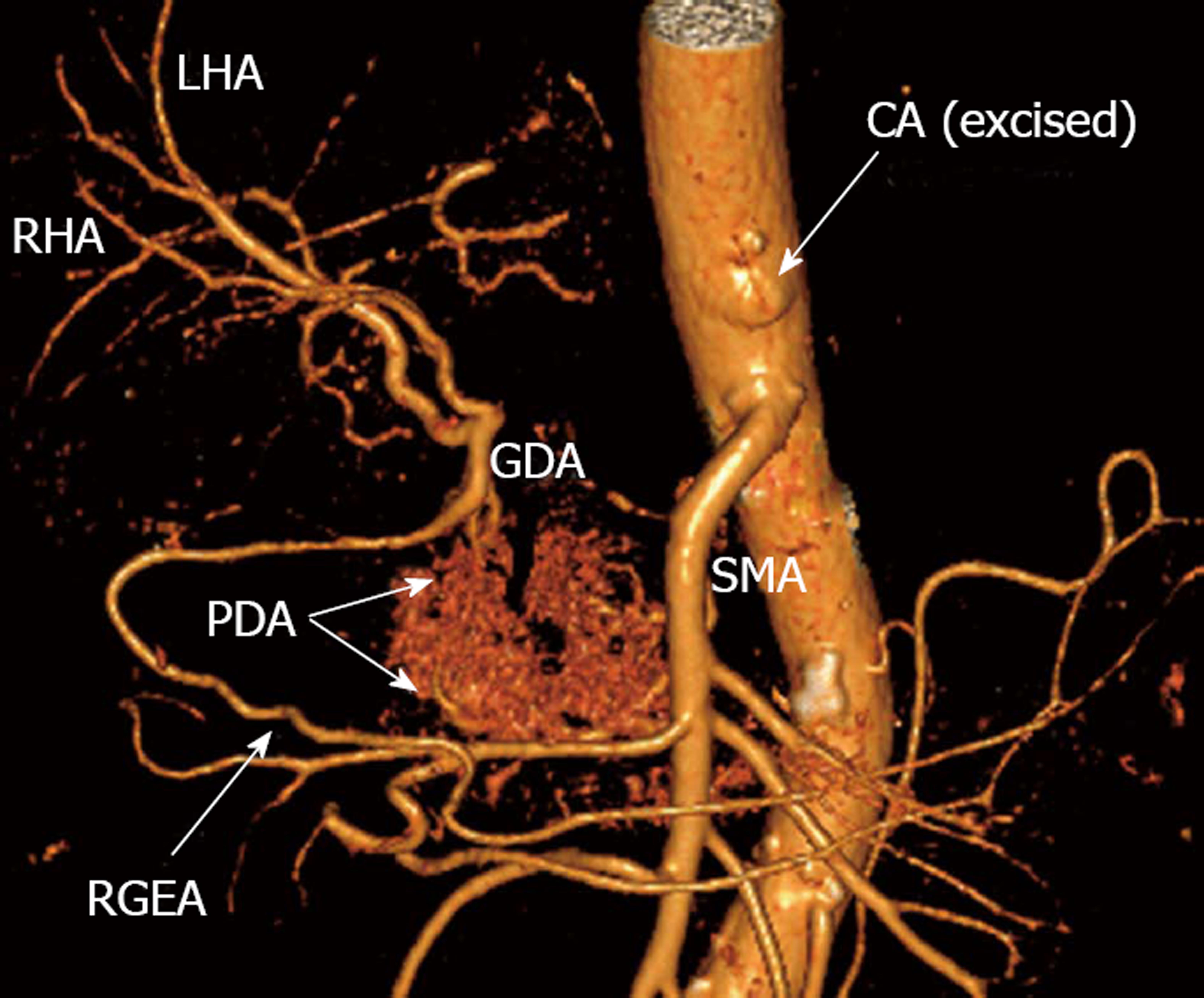
Figure 6 Three-dimensional computed tomography-angiography following distal pancreatectomy with excision of celiac artery and its branches.
Blood supply to liver and stomach is delivered from superior mesenteric artery (SMA) via pancreaticoduodenal arcade (PDA) and then through gastroduodenal artery (GDA). There is robust right gastro-epiploic artery (RGEA) appearing in its entirety. RHA: Right hepatic artery; LHA: Left hepatic artery; CA: Celiac axis; GDA: Gastroduodenal artery.
Figure 7 Computed tomography prior to operation.
A: Axial view. Venous phase. Hypovascular tumor of pancreatic neck (T) is shown to abut portal vein (PV) trunk. Pancreatic head is demonstrated to be intact; B: Sagittal view. Arterial phase. Circumferential encasement of celiac artery (CA) by hypovascular tumor of pancreatic body and the latter’s adherence to anterior aspect of superior mesenteric artery (SMA); C, D: Axial image. Arterial phase. Circumferential contiguity of tumor to CА along with common hepatic (CHA) and splenic (SA), both arising from the former, is visualized. CT: Celiac trunk.
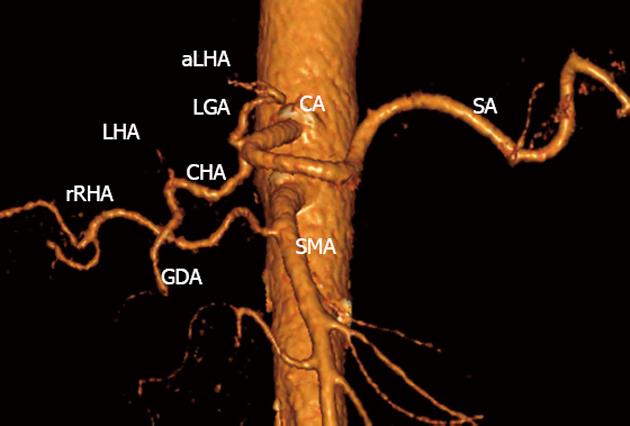
Figure 8 Three-dimensional computed tomography angiography before surgery.
Variant arterial anatomy: replaced right hepatic artery (rRHA) originating from superior mesenteric artery (SMA), accessory left hepatic (aLHA) - from left gastric (LGA) (Michels, type VIIIb). CA: Celiac artery; LHA: Left hepatic artery; SA: Splenic artery; GDA: Gastroduodenal artery; CHA: Common hepatic.
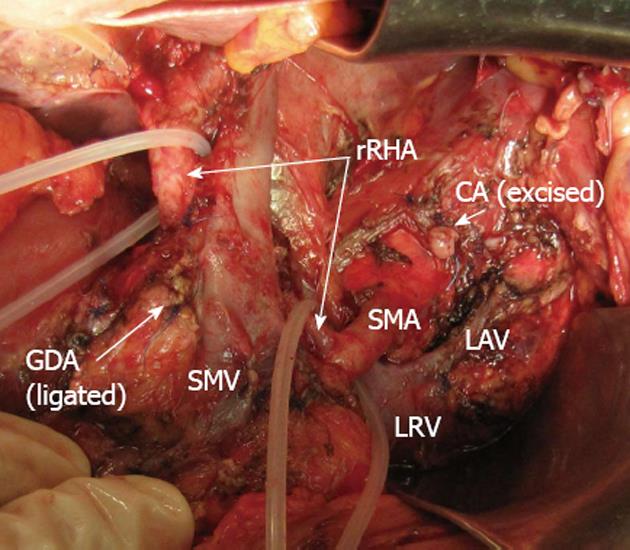
Figure 9 Photograph.
View of operating field after distal pancreatectomy with excision of celiac artery (CA), left gastric, common hepatic and left hepatic arteries. Superior mesenteric artery (SMA)-derived blood feeding of right hepatic lobe carried via the replaced right hepatic artery (rRHA). Blood supply to stomach is routed from SMA via pancreaticoduodenal arcades and then through gastroduodenal artery (GDA) with the latter’s proximal segment being resected and ligated. CA: Celiac artery; LAV: Left adrenal vein; LRV: Left renal vein; SMV: Superior mesenteric vein.
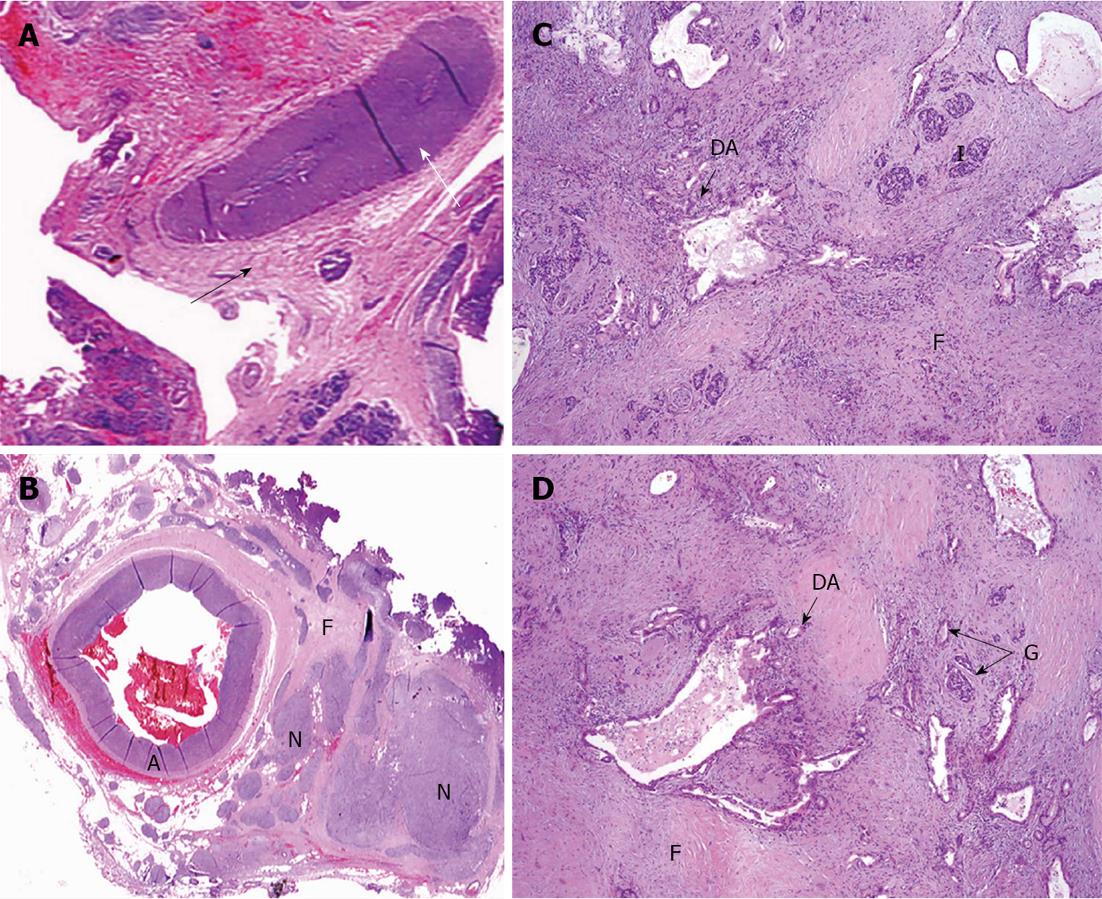
Figure 10 Under microscope.
A: Common hepatic (CHA) section obtained from close to the point of its transection (white arrow) amid fibrotic zone (black arrow) along pancreas margin. No evidence of tumor growth (× 5); B: Celiac plexus and trunk area of diffuse fibrosis (F) (× 5); C: Pancreatic tissue with apparent diffuse fibrosis (F), groups of islets left (I) and that of glandular formations of ductal adenocarcinoma of pancreas (DA) (× 50); D: Structures of DA throughout fibrotic tissue (F) containing remnants of pancreatic tissue (atrophic islets and ductules) (HE, × 5). A: Artery; N: Nerve plexus with large ganglion (G).
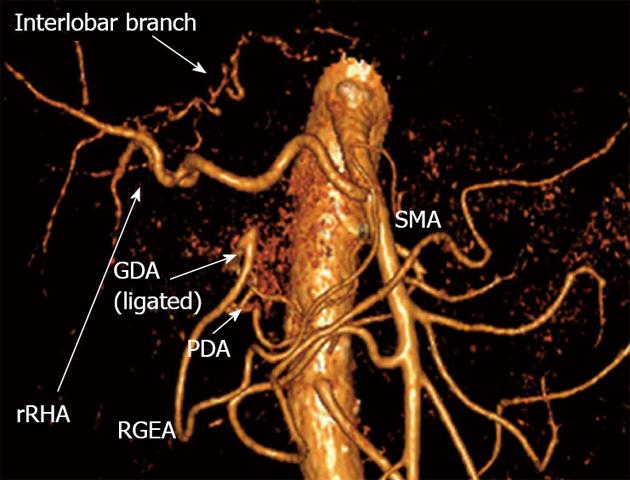
Figure 11 Three-dimensional computed tomography angiography subsequent to distal pancreatectomy with excision of celiac artery, left gastric, common hepatic and left hepatic arteries.
Blood supply to right hepatic lobe is provided by superior mesenteric artery (SMA) through the replaced right hepatic artery (rRHA) and that to left hepatic lobe - via interlobar collateral anastomosing with rRHA. Stomach is supplied from SMA via pancreaticoduodenal artery (PDA) and, thereafter, through gastroduodenal artery (GDA) and right gastro-epiploic artery (RGEA).
Figure 12 Coronal image.
Arterial phase. A: Previous to surgery. Aberrant arterial vasculature (Michels, type VIIIb): replaced right hepatic artery (rRHA) stemming from superior mesenteric artery (SMA), the left gastric artery (LGA) giving rise to accessorial left hepatic artery (aLHA). No interlobar collateral is detectable; B: Distal pancreatectomy with excision of celiac artery (CA), LGA, common hepatic (CHA) and left hepatic (LHA) arteries. Increased blood flow via rRHA is displayed and extraparenchymal hilar interlobar collateral transmitting blood supply to left hepatic lobe became visible.
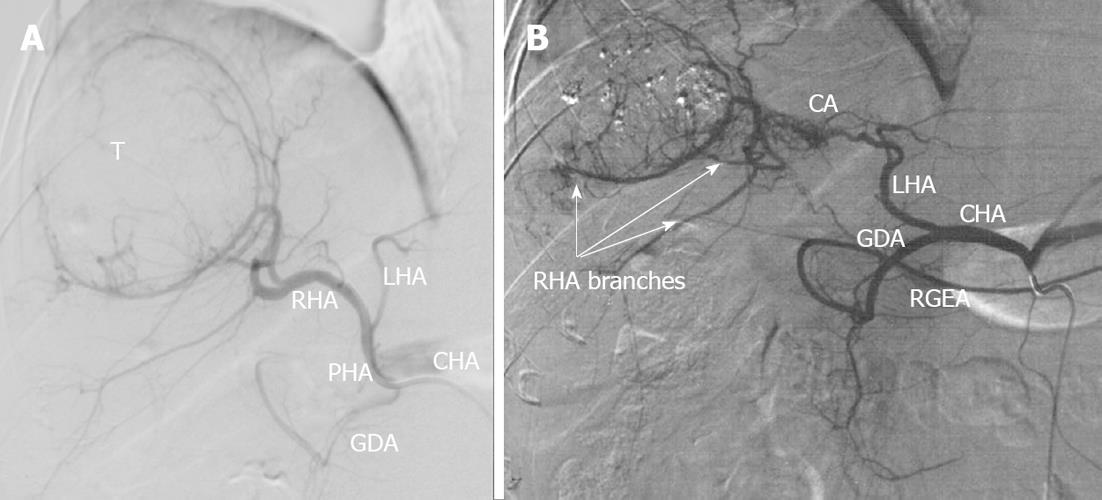
Figure 13 Selective celiacography in a 37-year-old man with firearm (machine gun shots) liver wounds, false aneurysms of left hepatic lobe and hemobilia.
A: Classical arterial architecture (Michels, type 1). There is communicating interlobar artery (CA) connecting right and left hepatic arteries (RHA and LHA). Turbulent blood flow is seen in areas of pulsative hematomas (H); B: Control of hemorrhage was achieved with RHA occlusion but arterial branches of right hepatic lobe keep being filled owing to CA-conveyed blood transit from the left hepatic artery (LHA). GDA: Gastroduodenal artery; PHA: Proper hepatic artery; CHA: Common hepatic artery; RGEA: Right gastroepiploic artery; T: Tumor.
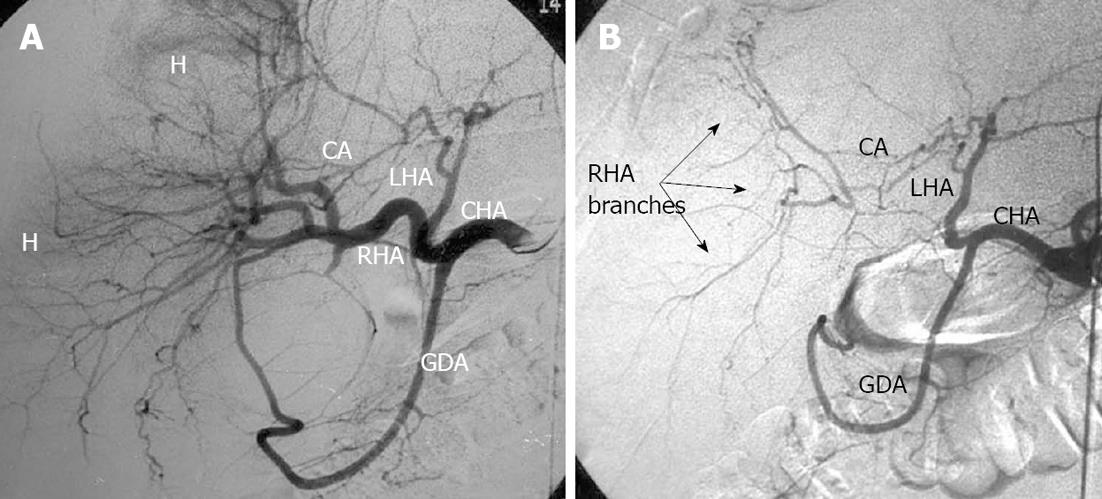
Figure 14 Selective celiacography in a 64-year-old man with hepatocellular cancer.
A: Before and after chemoembolization through the right hepatic artery; B: Arterial branches of right hepatic lobe keep being filled owing to communicating interlobar artery (CA)-conveyed blood transit from the left hepatic artery (LHA). GDA: Gastroduodenal artery; CHA: Common hepatic artery; RHA: Right hepatic artery; H: Hematoma.
- Citation: Egorov VI, Petrov RV, Lozhkin MV, Maynovskaya OA, Starostina NS, Chernaya NR, Filippova EM. Liver blood supply after a modified Appleby procedure in classical and aberrant arterial anatomy. World J Gastrointest Surg 2013; 5(3): 51-61
- URL: https://www.wjgnet.com/1948-9366/full/v5/i3/51.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v5.i3.51