Copyright
©2011 Baishideng Publishing Group Co.
World J Gastrointest Surg. Jul 27, 2011; 3(7): 89-100
Published online Jul 27, 2011. doi: 10.4240/wjgs.v3.i7.89
Published online Jul 27, 2011. doi: 10.4240/wjgs.v3.i7.89
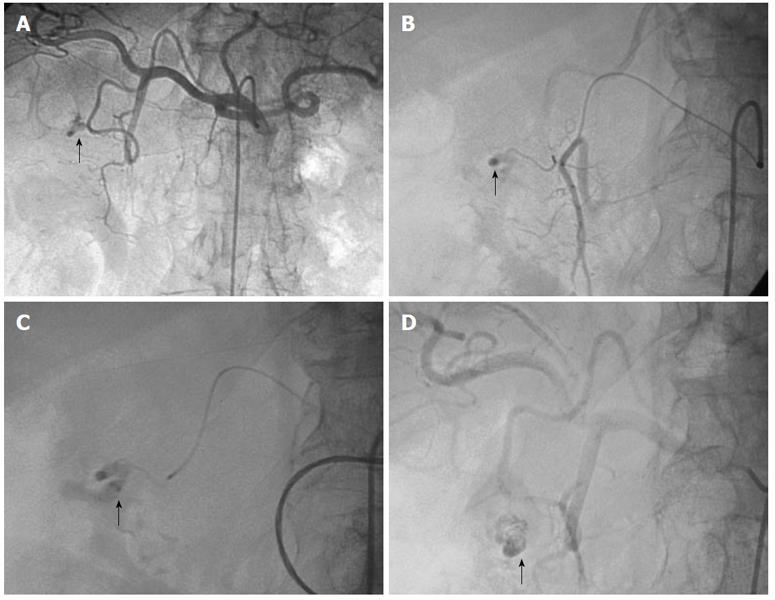
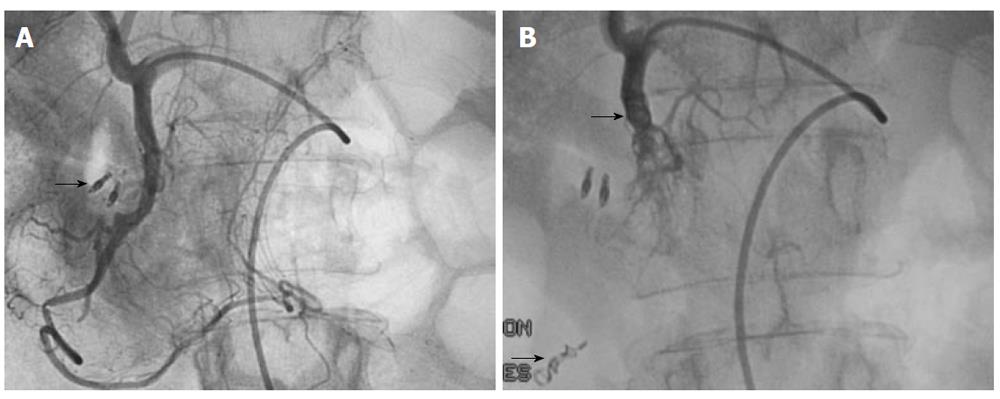
Figure 1 Arteriogram images of bleeding from a bulbar duodenal ulcer in a 76-year-old man.
A, B: Arteriogram showing contrast medium extravasated from a slender branch of the gastroduodenal artery into the duodenum (arrows); C, D: After microcatheterization, selective glue embolization [radiopaque because of associated lipiodol (arrows)] preserving the gastroduodenal artery ensured control of the bleeding, with no early or late recurrences.
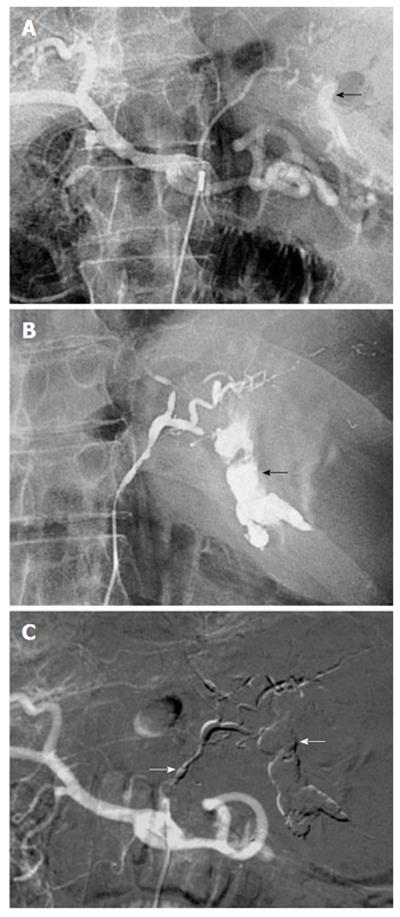
Figure 2 Bleeding dieulafoy lesion in an 87-year-old man.
A, B: Extravasation of contrast medium from the left gastric artery at the celiac trunk and superselective angiography indicates continuing bleeding (arrows); C: After arterial microcatheterization, bleeding was controlled after embolization of the left gastric artery using a Glubran/Lipidol mixture (1:3) (arrows).
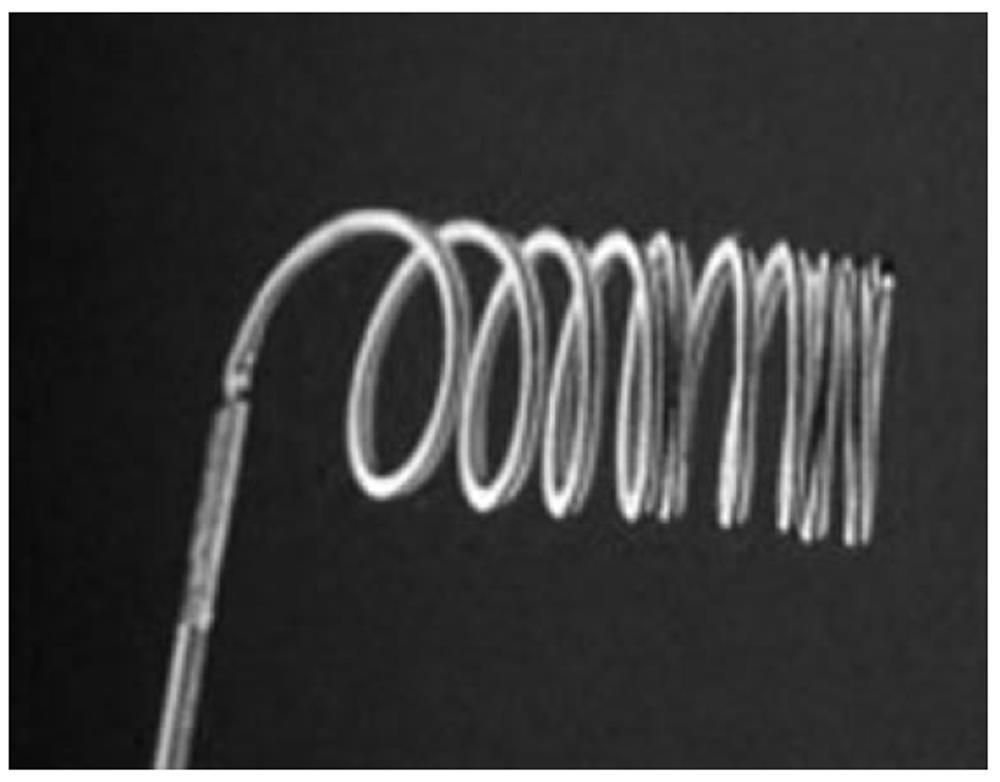
Figure 3 Detachable metallic coil.
This is a vessel-blocking agent which is positioned at the target site, as opposed to released in the bloodstream.
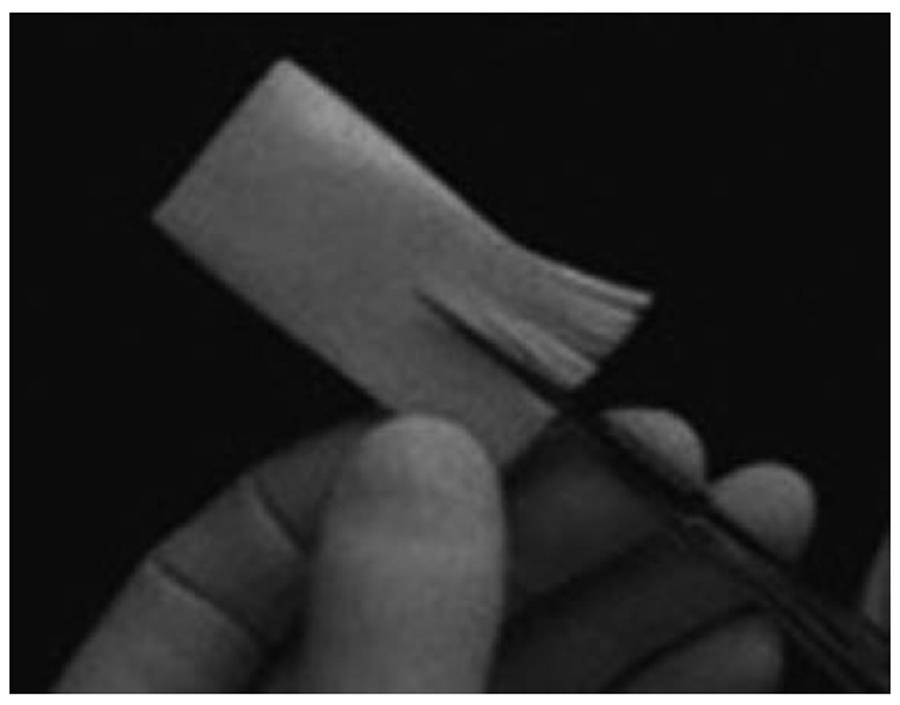
Figure 4 Preparation of gelatine particles of various sizes by manually cutting gelatine sheets.
When the fundamental principles of embolization are scrupulously followed, absorbable agents for temporary embolization are effective, safe and cost-effective.
Figure 5 Tris-acryl gelatine microspheres of 500-700 microns in size.
Microspheres have two major advantages: they can be calibrated to ensure accurate targeting and they do not block the embolization catheter.
Figure 6 Glubran 2®: N-butyl 2-cyanoacrylate + metacrylosulpholane.
The main advantage of cyanoacrylate glue is the lasting nature of the vascular occlusion, compared with particles.
Figure 7 Gelling solution.
The only commercially available gelling solution (Onyx®) is composed of ethylene-vinyl-alcohol copolymer suspended in dimethyl-sulphoxide, with tantalum to ensure visibility by fluoroscopy.
Figure 8 Typical sandwich embolization in a 75-year-old woman with bleeding from a postbulbar duodenal ulcer at endoscopy.
A: Angiography before embolization, guided by clip position (arrow): no evidence of active bleeding; B: Coil embolization of the distal and proximal gastroduodenal artery (with gelatine sponge in the arterial trunk), including the anterior and posterior superior pancreaticoduodenal arteries and the right gastroepiploic artery, to prevent retrograde flow (arrows). Bleeding stopped and no ischemic complications were reported.
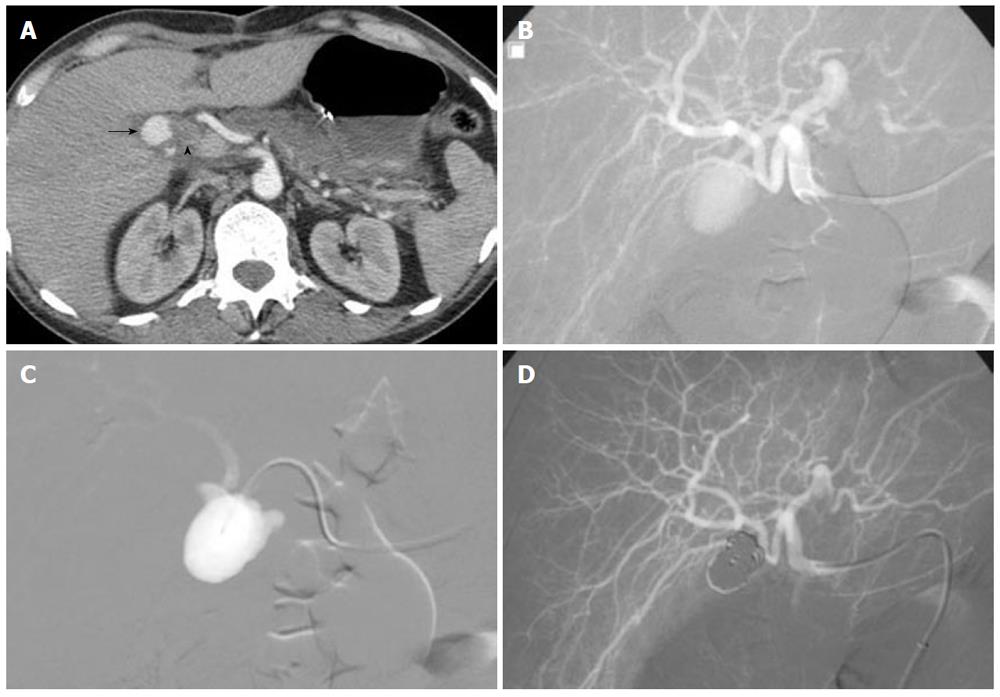
Figure 9 A 41-year-old woman presented 3 wk after laparoscopic cholecystectomy with right upper abdominal pain and hemobilia.
A: Computed axial tomography scan: round mass within the gallbladder fossa that shows contrast filling at the arterial phase (arrow), and dilatation of the bile duct (arrowhead); B: Selective hepatic arteriogram demonstrating pseudoaneurysm of the cystic artery stump; C: Coil embolization of the aneurysmal sac across the neck using the packing technique through a microcatheter; D: Control angiography showing complete occlusion of the false aneurysm and preservation of the main and distal hepatic artery.
- Citation: Loffroy RF, Abualsaud BA, Lin MD, Rao PP. Recent advances in endovascular techniques for management of acute nonvariceal upper gastrointestinal bleeding. World J Gastrointest Surg 2011; 3(7): 89-100
- URL: https://www.wjgnet.com/1948-9366/full/v3/i7/89.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i7.89