Copyright
©2010 Baishideng Publishing Group Co.
World J Gastrointest Surg. Oct 27, 2010; 2(10): 324-330
Published online Oct 27, 2010. doi: 10.4240/wjgs.v2.i10.324
Published online Oct 27, 2010. doi: 10.4240/wjgs.v2.i10.324
Figure 1 Coronal maximum intensity projection from a 3D T2-weighted MRCP acquisition shows a cystic lesion in the uncinate process of the pancreas (asterisk) and a communicating branch duct (arrow) between the cyst and the normal caliber main pancreatic duct.
These findings are characteristic of a branch duct intraductal papillary mucinous neoplasm and this lesion has been stable on follow up MRCP examinations for 3 years.
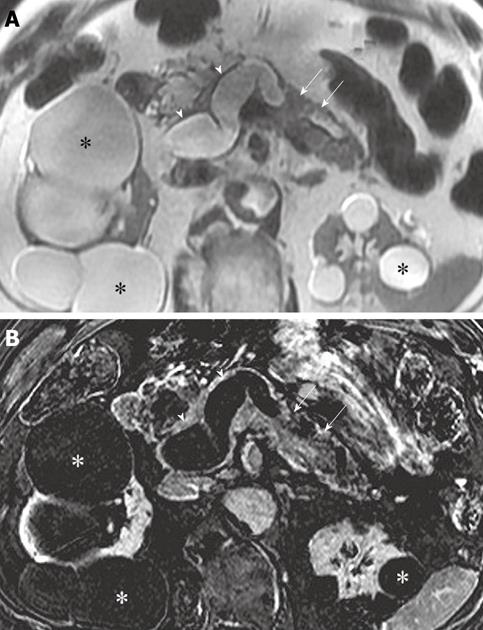
Figure 2 Axial T2-weighted (A) and subtraction (post-contrast minus pre-contrast) (B) images at the level of the pancreas demonstrate marked enlargement of the main pancreatic duct (arrowheads) with intraluminal enhancing papillary projections (arrows).
Main duct intraductal papillary mucinous neoplasm with in situ carcinoma was confirmed at histopathology after total pancreatectomy. Multiple renal cysts (asterisks).
Figure 3 Axial contrast enhanced computed tomography image at the level of the head of the pancreas shows a cystic lesion (asterisk) in the uncinate process of the pancreas with a hypoattenuating area (arrow) in the adjacent pancreatic parenchyma.
Note the intrahepatic biliary dilatation (arrowheads) due to obstruction of the common bile duct (not shown) by the infiltrating mass. Invasive pancreatic adenocarcinoma arising from an intraductal papillary mucinous neoplasm was confirmed at pathology after a Whipple procedure. GB: Gallbladder.
- Citation: Pedrosa I, Boparai D. Imaging considerations in intraductal papillary mucinous neoplasms of the pancreas. World J Gastrointest Surg 2010; 2(10): 324-330
- URL: https://www.wjgnet.com/1948-9366/full/v2/i10/324.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v2.i10.324