Copyright
©The Author(s) 2025.
World J Gastrointest Surg. Aug 27, 2025; 17(8): 108692
Published online Aug 27, 2025. doi: 10.4240/wjgs.v17.i8.108692
Published online Aug 27, 2025. doi: 10.4240/wjgs.v17.i8.108692
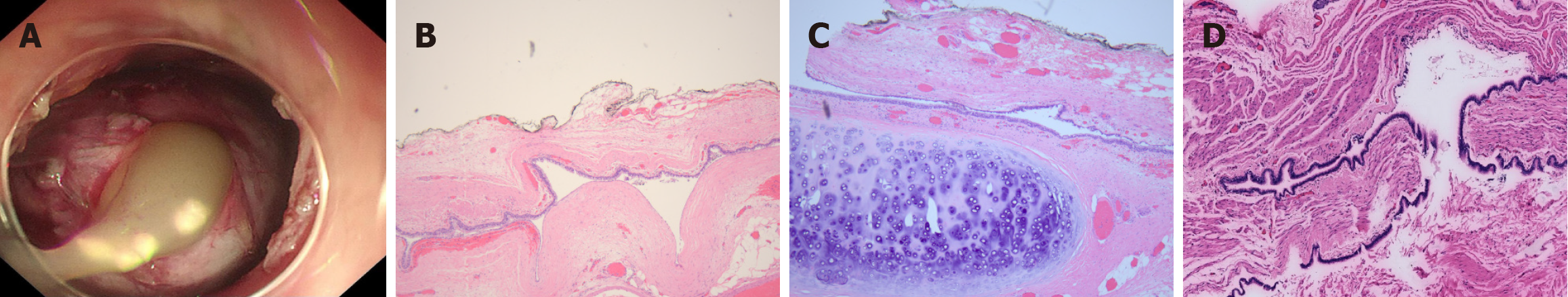
Figure 1 Cystic content and histology.
A: A highly proteinaceous and mucoid content during submucosal tunnel endoscopic resection; B: Histopathologic examination showing the ciliated columnar epithelium lining and smooth muscle layers in the cyst wall (hematoxylin and eosin, 5 ×); C: Histopathologic examination showing the ciliated columnar epithelium lining, smooth muscle layers and cartilage (hematoxylin and eosin, 5 ×); D: A typical pathological image showing that the lesion was originated from muscularis propria.
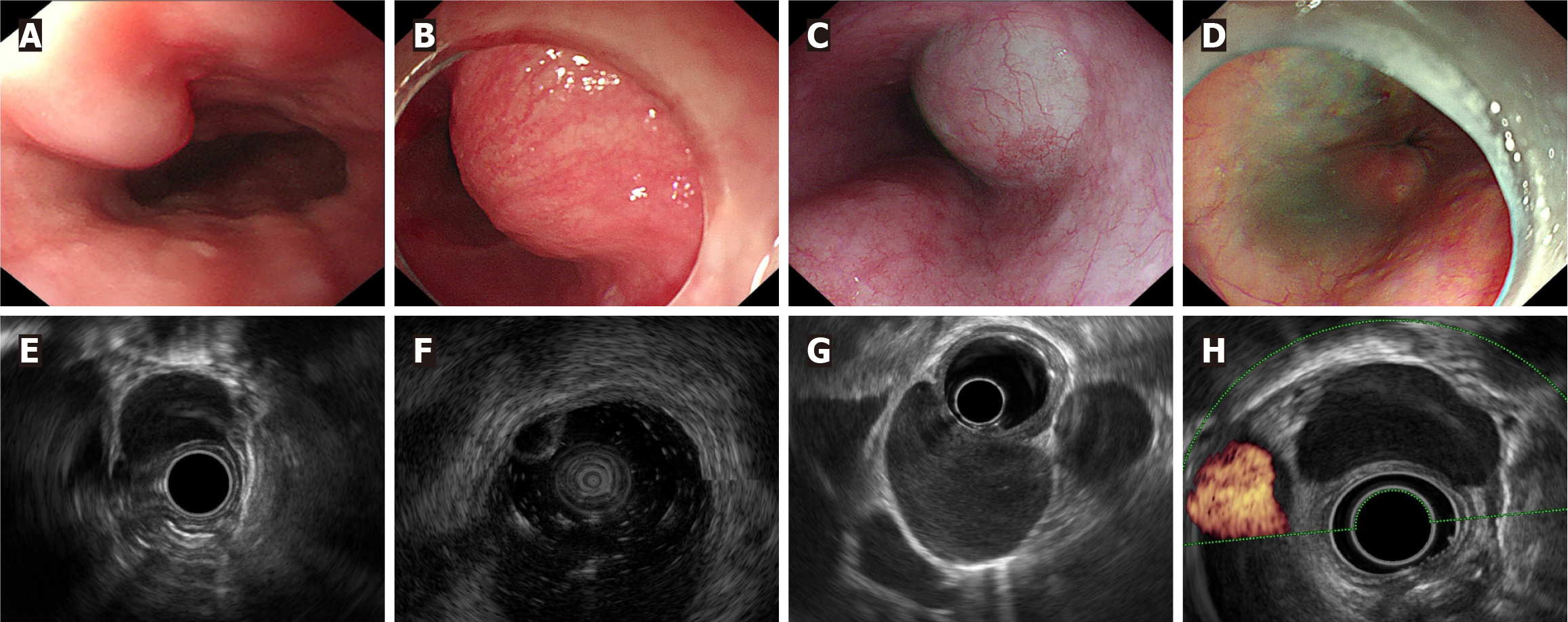
Figure 2 White light endoscopy and endoscopic ultrasonography images of esophageal bronchogenic cysts.
A: An oblong flat bulging lesion in the lower esophagus; B: A light blue hemisphere lesion in the lower esophagus; C: A dumbbell bulging lesion in the lower esophagus; D: No lesions were found in the esophageal cavity; E: A lesion originating from the muscularis propria; F: A lesion originating from the submucosa; G: A lesion with a homogeneous hypoecho; H: No blood flow signal was detected within the lesion.
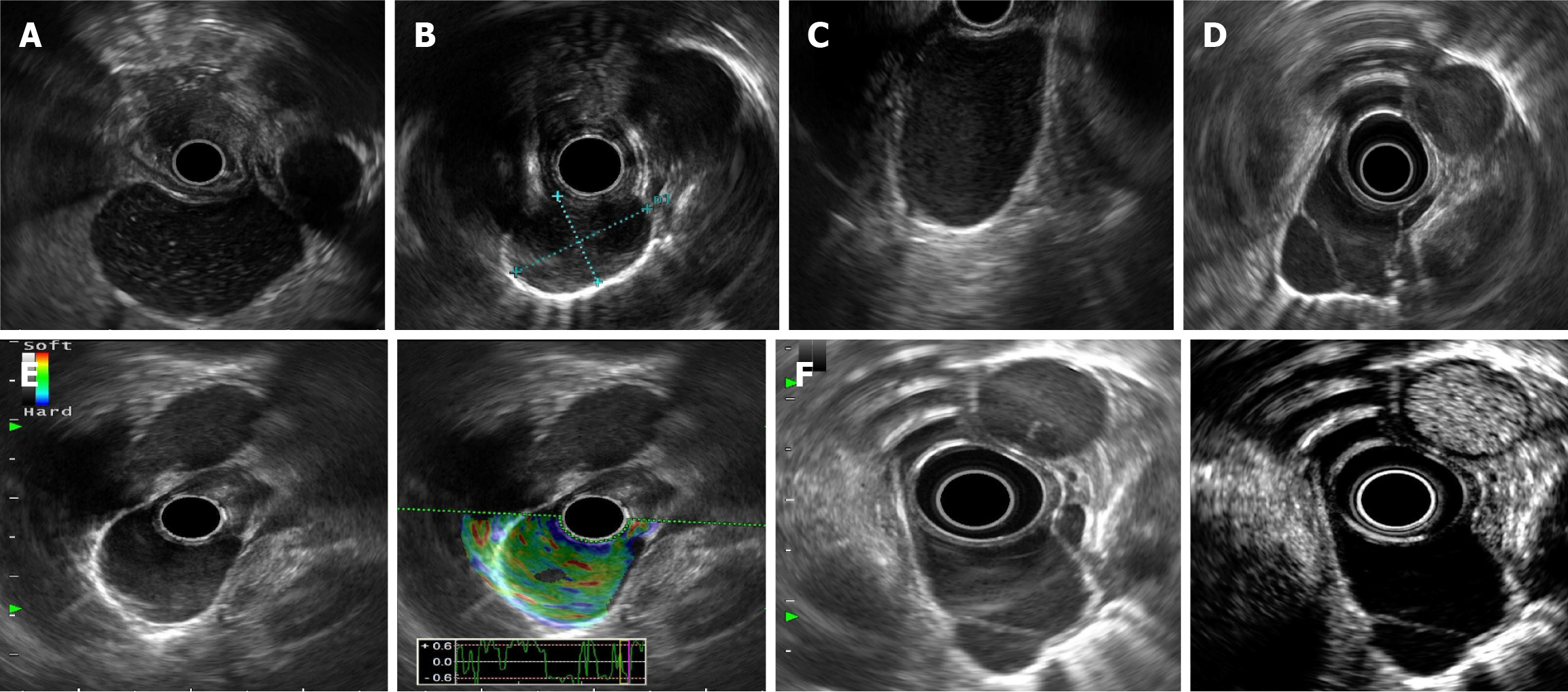
Figure 3 Special endoscopic ultrasonography findings.
A: Punctiform hyperecho inside the lesion; B: Flocculent hypoecho inside the lesion; C: Posterior wall enhancement in the lesion; D: A separable zone was visible in the capsule cavity; E: Endoscopic ultrasonography elastography revealed a green pattern; F: Contrast-enhanced endoscopic ultrasonography revealed no enhancement in the capsule cavity but hypoenhancement in the separable zone and capsule wall.
- Citation: Shan GD, Ning LG, Zhang FM, Du HJ, Chen WG, Wang JJ, Li AQ, Xu GQ, Chen HT. Clinicopathological and endoscopic ultrasonography characteristics of esophageal bronchogenic cysts: A single-center study. World J Gastrointest Surg 2025; 17(8): 108692
- URL: https://www.wjgnet.com/1948-9366/full/v17/i8/108692.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i8.108692