Copyright
©The Author(s) 2024.
World J Gastrointest Surg. Mar 27, 2024; 16(3): 944-954
Published online Mar 27, 2024. doi: 10.4240/wjgs.v16.i3.944
Published online Mar 27, 2024. doi: 10.4240/wjgs.v16.i3.944
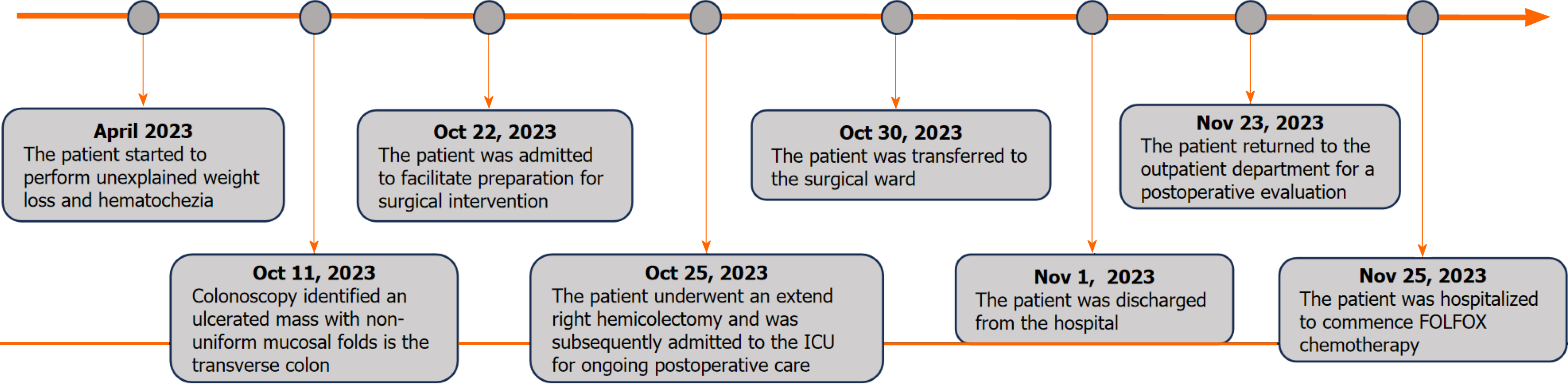
Figure 1 Timeline of the initial diagnosis, surgical intervention, subsequent follow-up period, and adjuvant therapy.
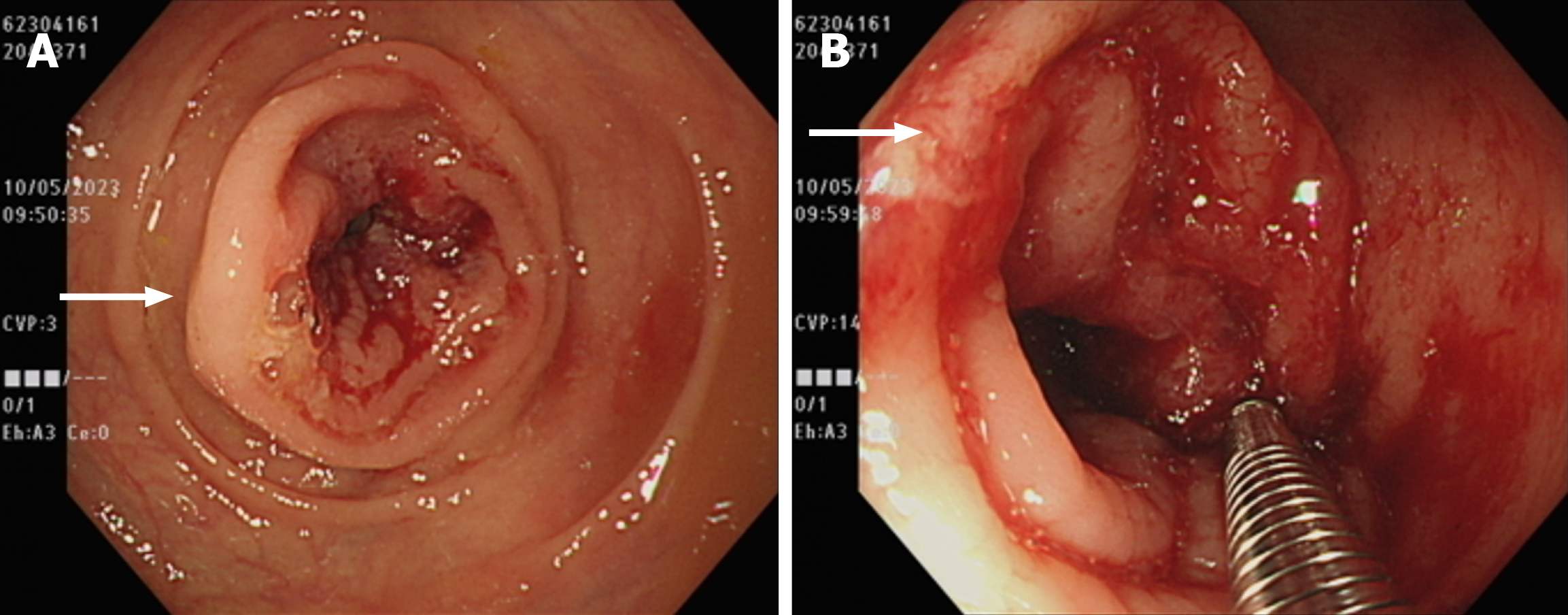
Figure 2 Diagnostic imaging and interventions with the colonoscope.
A: Colonoscopic examination revealed a 3-cm ulcerative lesion within the transverse colon, characterized by irregular luminal stenosis (white arrow); B: An attempt was made to obtain a biopsy through the colonoscope for pathological examination (white arrow).
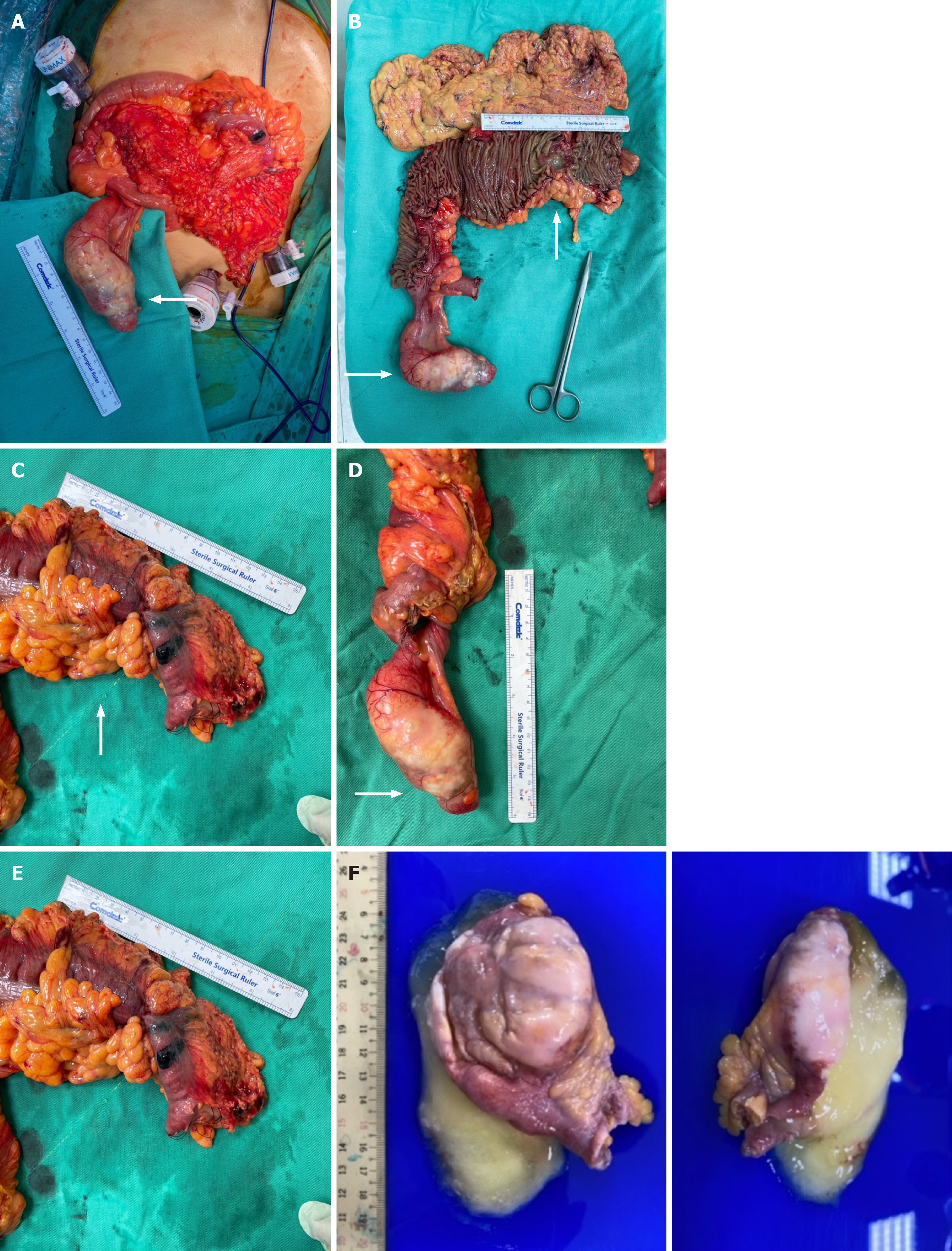
Figure 3 Multistage intraoperative and specimen images of colonic adenocarcinoma and appendiceal mucinous neoplasm.
A: Intraoperative photograph depicting the surgical field (white arrow); B: Comprehensive visualization of the adenocarcinoma and appendiceal mucinous neoplasm following an extended right hemicolectomy (white arrows); C: Image of the 6-cm neoplastic lesion located in the transverse colon (white arrow); D: Image of the 9-cm appendiceal mucinous neoplasm, featuring an intact capsular structure; E: Depiction of a large mucinous cavity within the appendix, which simulates a pseudo-diverticulum formation; F: The specimen submitted consists of one tissue fragment, measuring 10.6 cm × 4.0 cm × 3.3 cm in size, fixed in formalin. Grossly, it is opened and filled with mucoid materials.
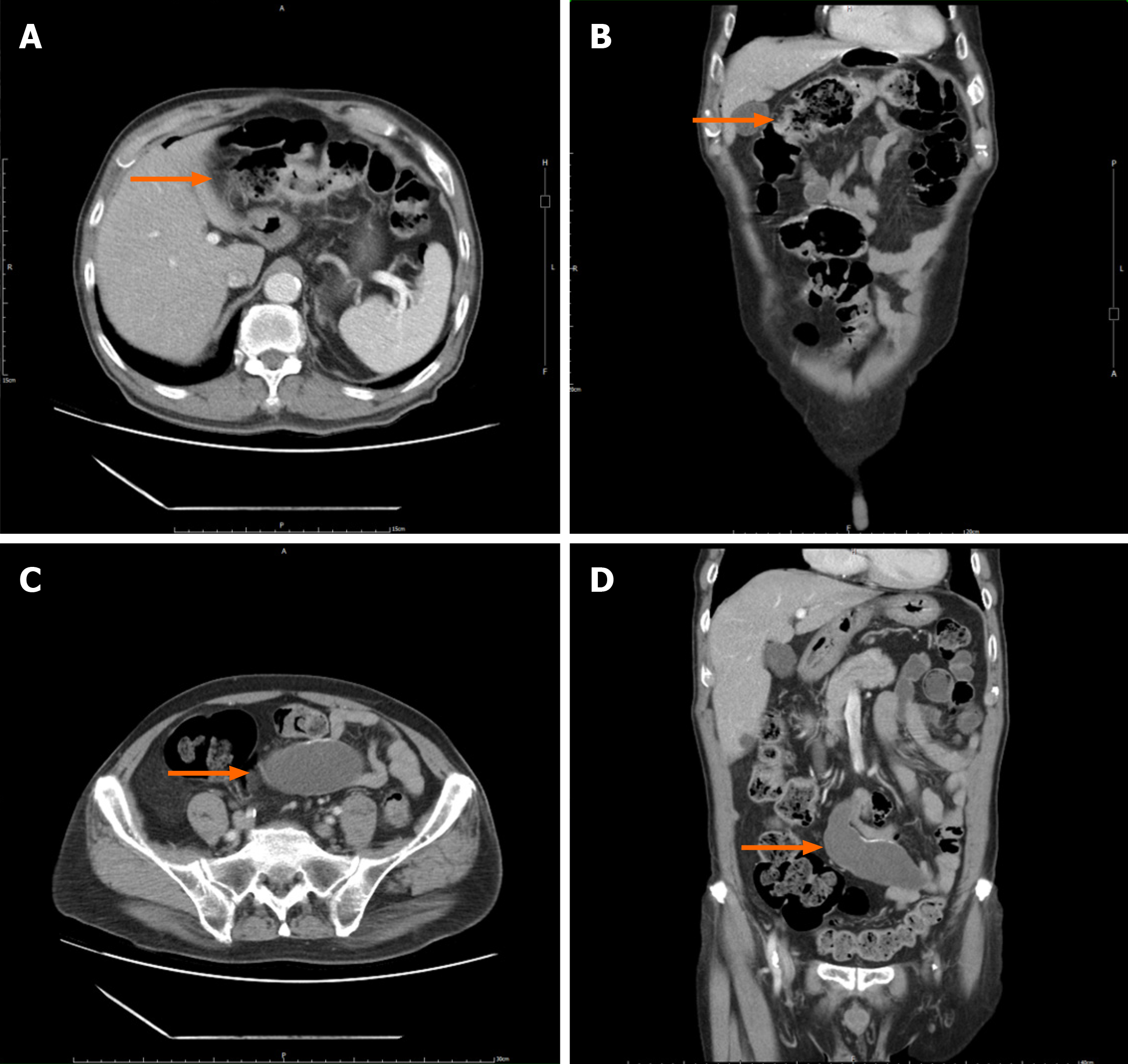
Figure 4 Preoperative abdominal computed tomography image.
A and B: The transverse colon wall and regional lymphadenopathy, correlating to a T3N1Mx stage, according to the 8th edition of the American Joint Committee on Cancer cancer staging guidelines (orange arrow); C and D: A cystic formation approximately 9 cm in size was initially detected and interpreted as a mesenteric cyst; subsequent scrutiny ascertained it as an appendiceal mucinous neoplasm (orange arrow).
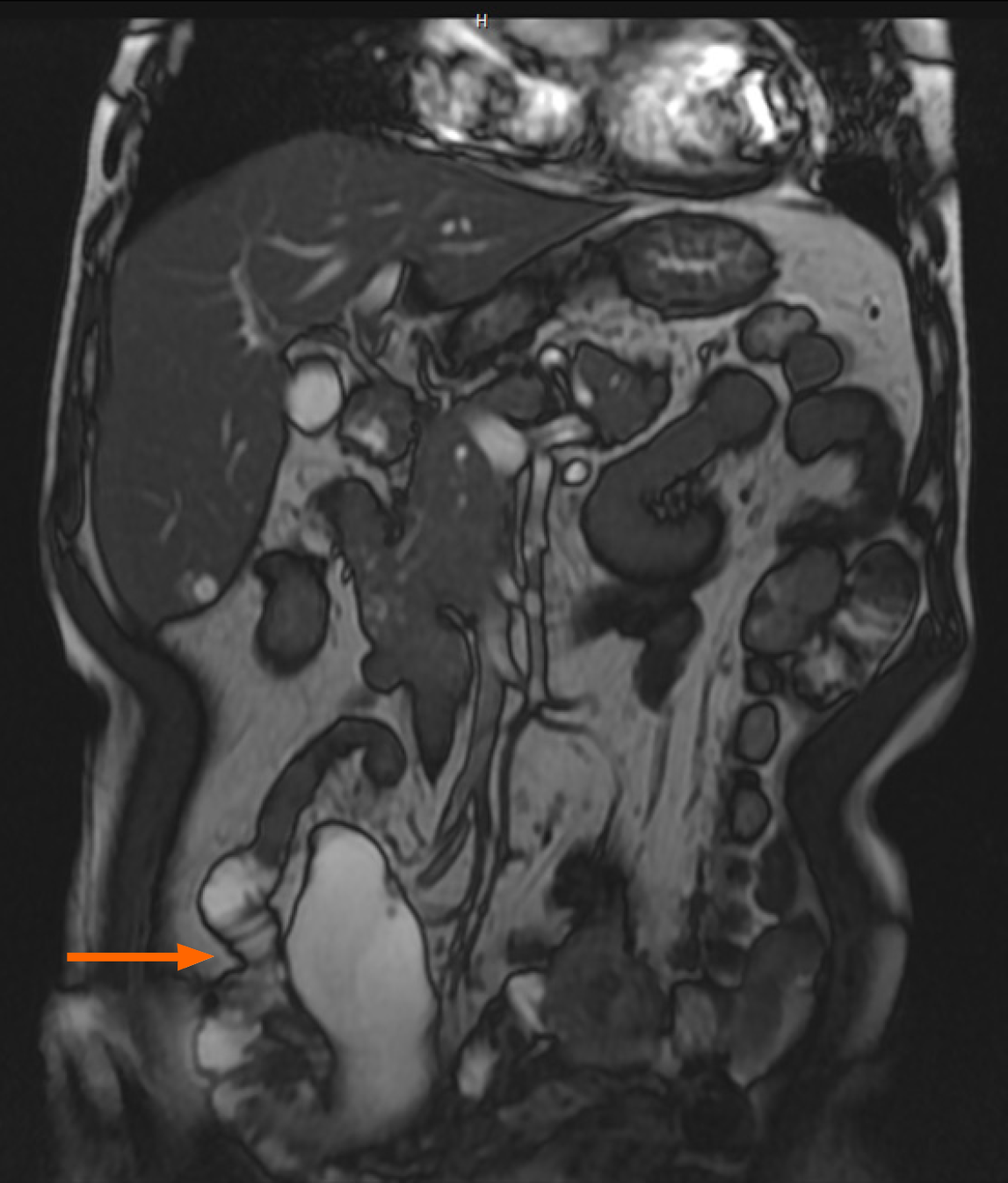
Figure 5 Preoperative coronal 2D Fast Imaging Employing Steady-state Acquisition magnetic resonance imaging of the abdomen revealed a cystic structure measuring approximately 9 cm in the right mesentery.
The imaging was conducted with a 1.5 Tesla superconducting magnet and a phased-array body coil. The patient was positioned supine, with the imaging parameters set to a field of view of 40 cm, a slice thickness of 6 mm, and an interslice gap of 1.5 mm. This lesion was subsequently identified as an appendiceal mucinous neoplasm.
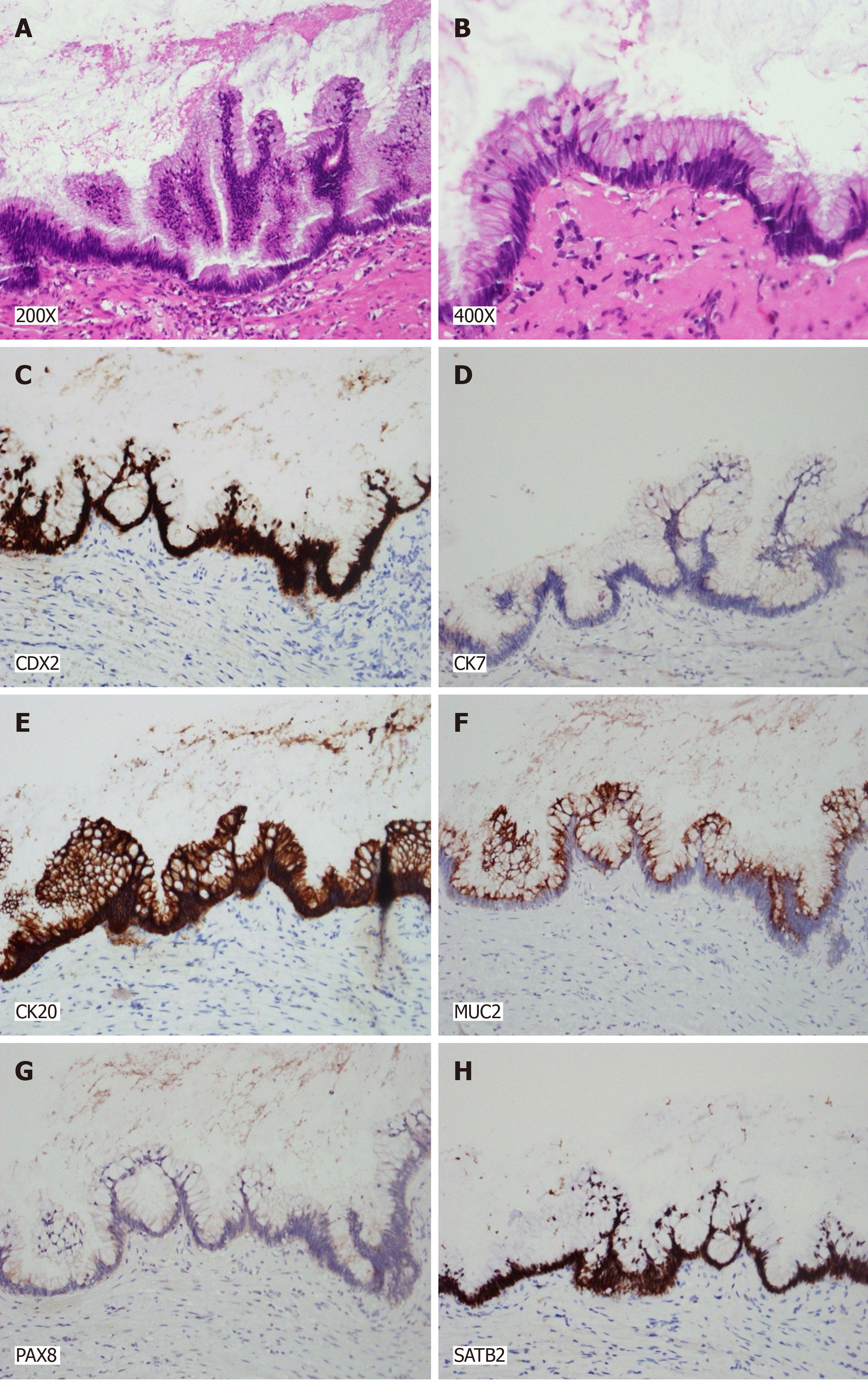
Figure 6 Histological examination of the lesion revealing characteristic patterns.
A: A 200 × magnification image showing slender villi lined by tall mucinous epithelial cells with low-grade dysplasia; B: A 400 × magnification image demonstrating tall mucinous epithelial cells with low-grade dysplasia, set within a fibrous stromal framework; C: Immunohistochemical staining displaying positive CDX2 expression in the villous cells; D: Immunohistochemical staining displaying positive CDX20 expression in the villous cells; E: Immunohistochemical staining displaying positive SATB2 expression in the villous cells; F: Immunohistochemical staining displaying positive MUC2 expression in the villous cells; G: Immunohistochemical staining showing the villous cells negative for CK7; H: Immunohistochemical staining showing the villous cells negative for PAX8.Collective histopathological and immunohistochemical findings indicate the lesion to be a low-grade appendiceal mucinous neoplasm. The evaluation of surgical margins shows no neoplastic presence, indicating a clear disease-free status.
- Citation: Chang HC, Kang JC, Pu TW, Su RY, Chen CY, Hu JM. Mucinous neoplasm of the appendix: A case report and review of literature. World J Gastrointest Surg 2024; 16(3): 944-954
- URL: https://www.wjgnet.com/1948-9366/full/v16/i3/944.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i3.944