Copyright
©The Author(s) 2024.
World J Gastrointest Surg. Oct 27, 2024; 16(10): 3185-3201
Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3185
Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3185
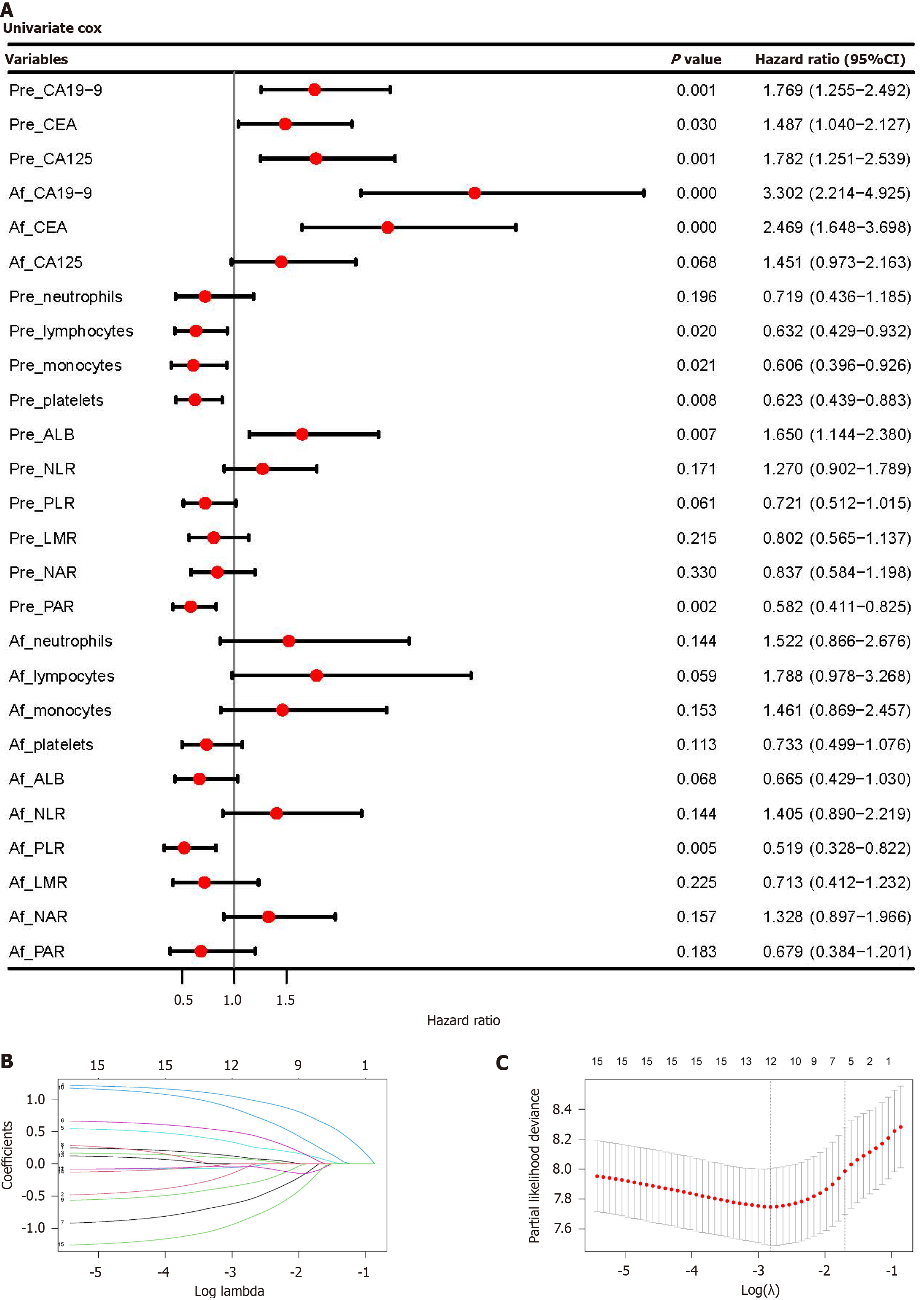
Figure 1 Construction of serum recurrence score based on perioperative serum-derived variables.
A: Univariate Cox regression analysis and Forest plot of perioperative serum-derived variables; B: LASSO regression analysis of 15 serum-derived variables (P value < 0.1) and shrinkage coefficient diagram. Y-axis represents coefficients of variables, and X-axis represents the penalty coefficient (Lambda). As the log Lambda increases, more coefficients of variables will decrease to zero; C: Cross validation (5-fold) of LASSO regression analysis. Dotted vertical line indicates the minimum and one standard error of Lambda values. The one standard error value of Lambda was used as the penalty coefficient. CA: Carbohydrate antigen; CEA: Carcinoembryonic antigen; ALB: Albumin; NLR: Neutrophils, lymphocytes ratio; PLR: Platelets to lymphocytes ratio; LMR: Lymphocytes to monocytes ratio; NAR: Neutrophil to albumin ratio; PAR: Platelet to albumin ratio.
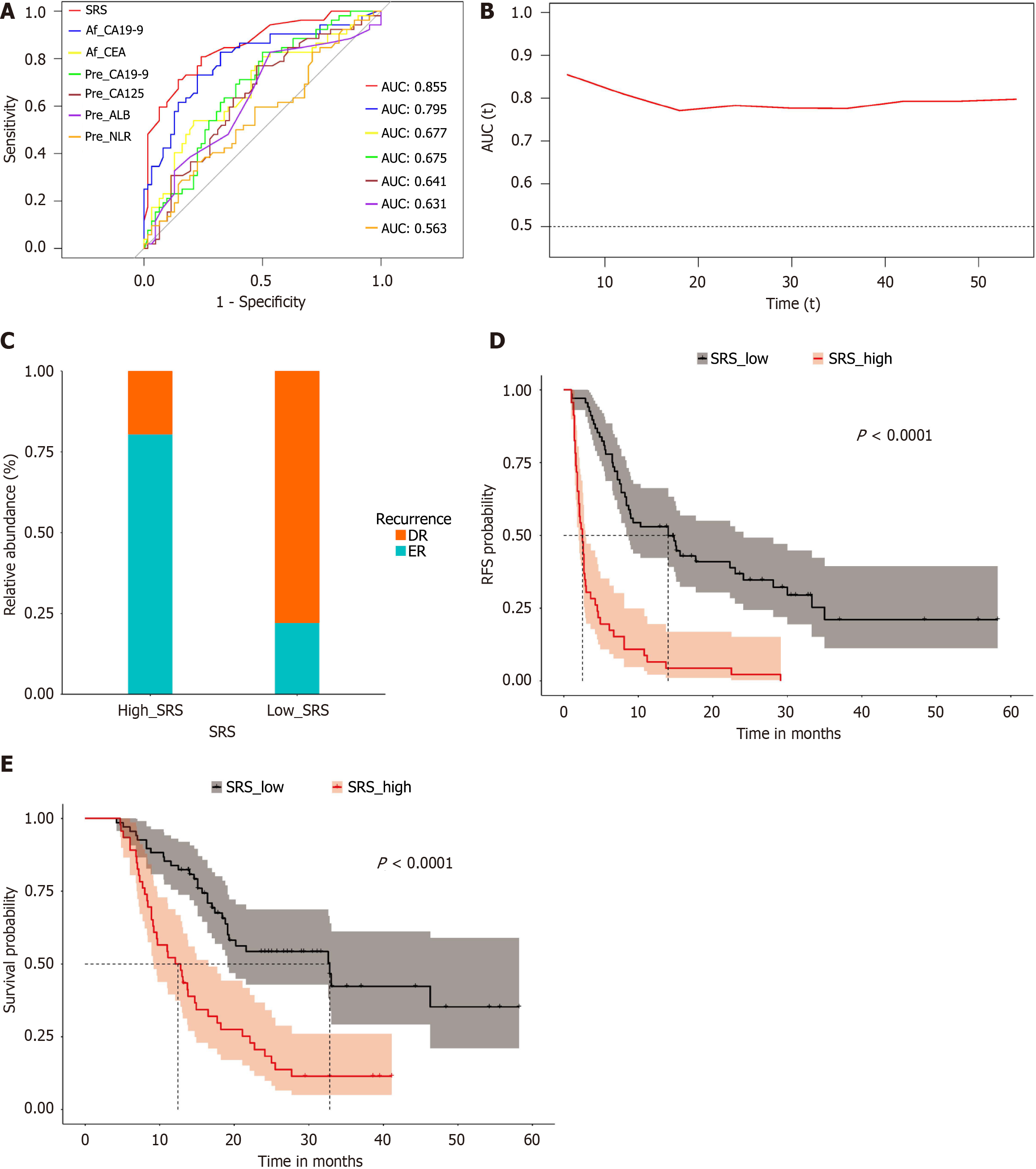
Figure 2 Receiver operating characteristics curve and survival analyses of serum recurrence score in the training cohort.
A: Receiver operating characteristics (ROC) curves of serum recurrence score (SRS) and top six (AUC) serum-derived variables for predicting early recurrence (ER). The AUC of SRS was superior to the AUCs of other serum-derived variables; B: Time-dependent ROC curve of SRS for predicting recurrence, the AUCs of SRS varied over time (months); C: Stacked plot showing significantly different ratios of ER and delayed recurrence, in the high-SRS (SRS > 0.53) and low-SRS (SRS ≤ 0.53) groups, respectively (P value = 2.719e-09); D and E: Kaplan-Meier survival analysis for patients with high SRS and low SRS. The high-SRS group showed significantly poorer recurrence free survival and overall survival compared with the low-SRS group. SRS: Serum recurrence score; ROC: Receiver operating characteristics; AUC: Area under the curve; ER: Early recurrence.
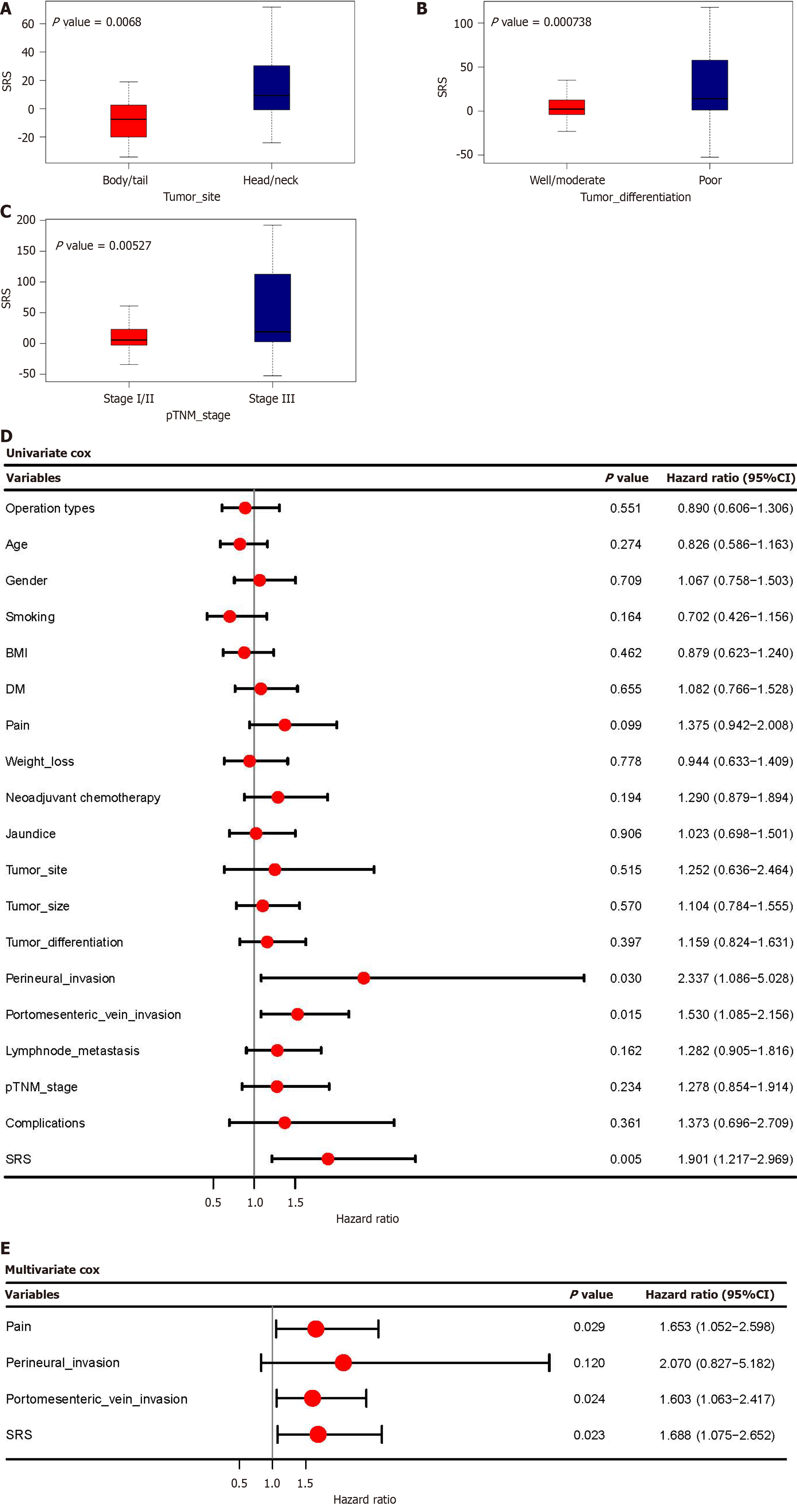
Figure 3 Construction of the recurrence nomogram.
A-C: Correlations between serum recurrence score (SRS) and tumor site, tumor differentiation, and tumor stage. Higher SRS was observed in the head/neck group, the poor differentiation group, and the advanced stage group; D: Univariate Cox regression analysis and Forest plot of SRS and 18 clinicopathological variables; E: Multivariate Cox regression analysis and Forest plot of the independent risk factors of recurrence. SRS: Serum recurrence score.
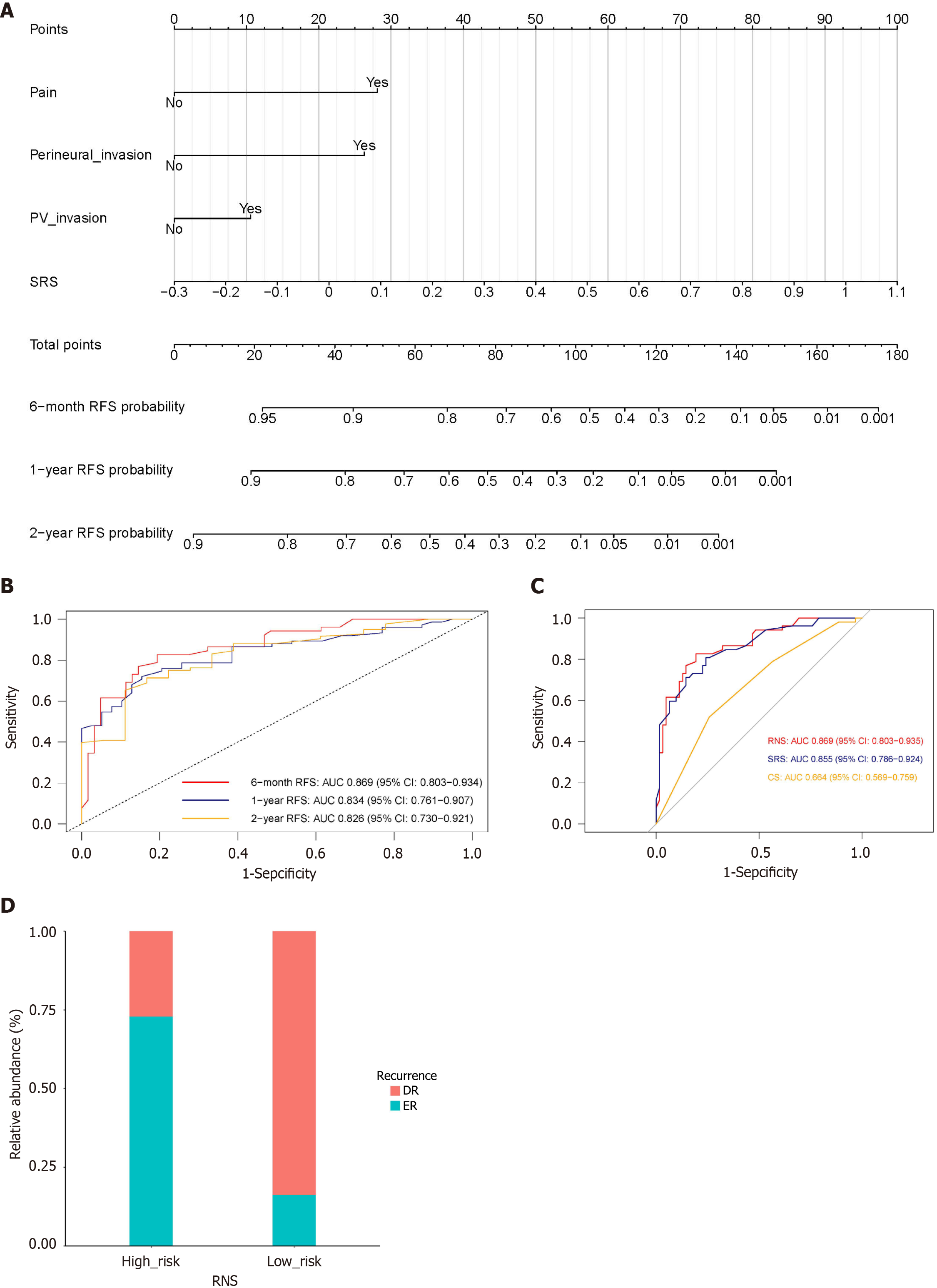
Figure 4 The Recurrence nomogram, and receiver operating characteristics curve analysis of recurrence nomogram score in the training cohort.
A: The Recurrence Nomogram for predicting recurrence; B: Receiver operating characteristics (ROC) curves of recurrence nomogram score (RNS) for predicting recurrence in different time intervals; C: ROC curves of RNS, serum recurrence score, and clinicopathological score for predicting early recurrence (ER); D: Stacked plot showing significantly different ratios of ER and delayed recurrence, in the high-risk (RNS > 4.23) and low-risk groups (RNS ≤ 4.23), respectively (P value = 4.467e-09). ROC: Receiver operating characteristics; RNS: Recurrence nomogram score; SRS: Serum recurrence score; CS: Clinicopathological score; ER: Early recurrence; DR: Delayed recurrence.
Figure 5 Survival analysis of recurrence nomogram score and clinicopathological variables in the training cohort.
A and B: Kaplan-Meier survival plots for patients in the high-risk [recurrence nomogram score (RNS) > 4.23] and low-risk (RNS ≤ 4.23) groups. The high-risk group showed significantly poorer recurrence free survival (RFS) and overall survival (OS) compared with the low-risk group; C-F: Patients with portomesenteric vein invasion showed poorer RFS and OS than those without (C and E), and patients with pain showed poorer RFS and OS than those without (D and F). RNS: Recurrence nomogram score; RFS: Recurrence free survival; OS: Overall survival.
- Citation: He H, Zou CF, Jiang YJ, Yang F, Di Y, Li J, Jin C, Fu DL. Recurrence scoring system predicting early recurrence for patients with pancreatic ductal adenocarcinoma undergoing pancreatectomy and portomesenteric vein resection. World J Gastrointest Surg 2024; 16(10): 3185-3201
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3185.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3185