Copyright
©The Author(s) 2024.
World J Gastrointest Surg. Jan 27, 2024; 16(1): 13-20
Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.13
Published online Jan 27, 2024. doi: 10.4240/wjgs.v16.i1.13
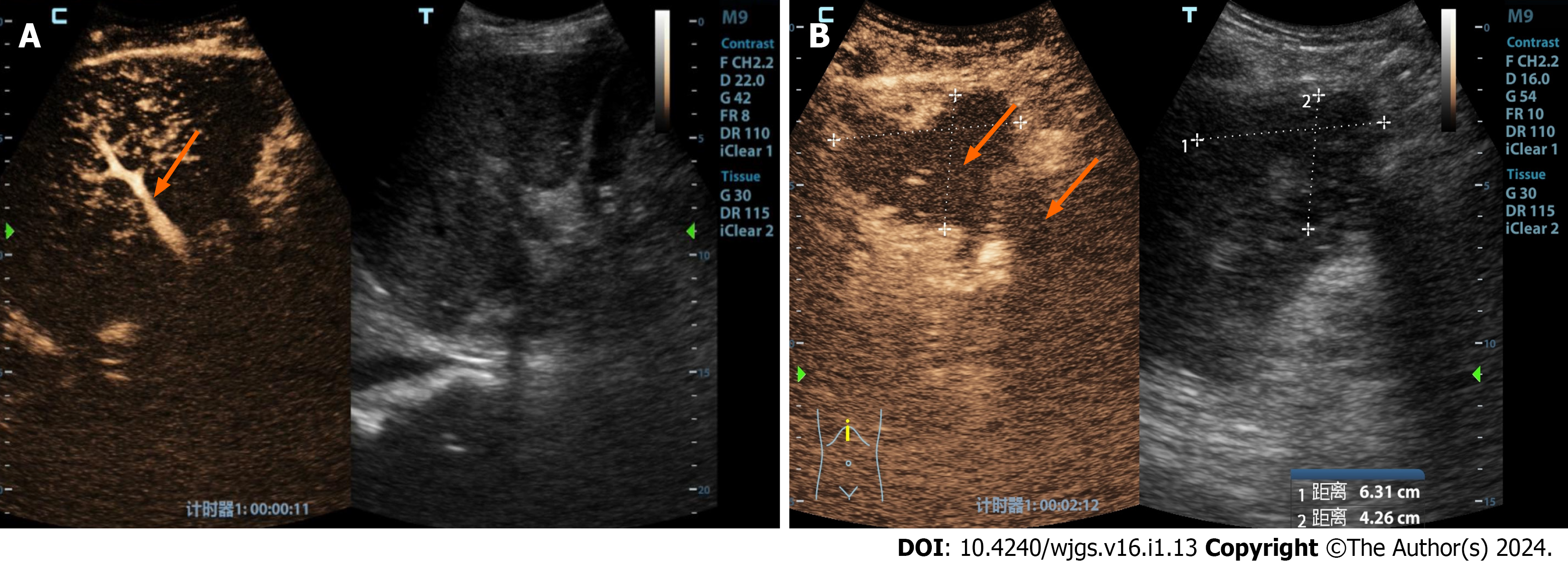
Figure 1 A 32-year-old male patient underwent a piggyback liver transplant for decompensated cirrhosis and acute liver failure.
A: This assessment occurred 15 d postoperatively. Routine ultrasound imaging had failed to reveal hepatic arteries within both the liver and extrahepatic regions. Contrast-enhanced ultrasound showed that the portal vein was prematurely visible (indicated by the orange arrow), while neither intrahepatic nor extrahepatic arteries displayed any enhancement; B: Furthermore, multiple ischemic lesions within the liver were observed in the arterial (phase I), portal (phase II), and late phases (phase III), indicating a lack of enhancement (as indicated by the orange arrow). Surgical confirmation subsequently identified a diffuse formation of arterial thrombosis within the hepatic artery.
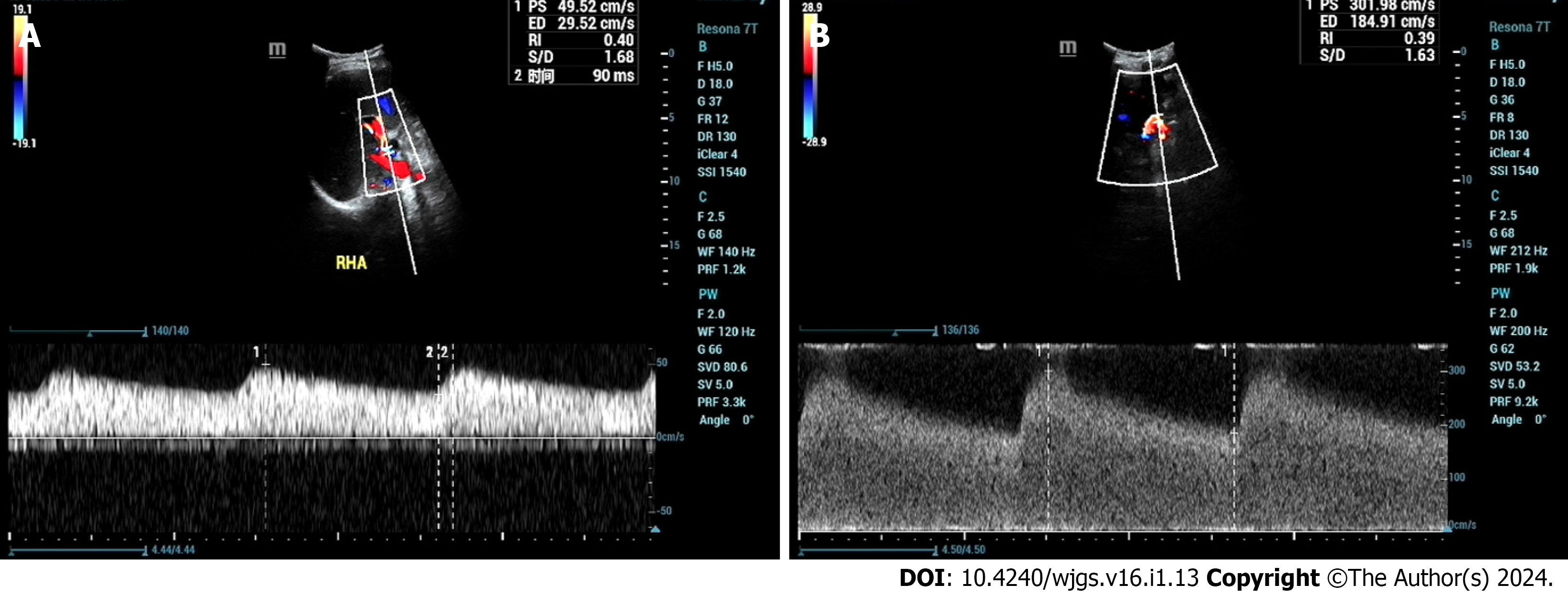
Figure 2 A 46-year-old male patient who underwent liver transplantation for liver cancer received an ultrasound examination at 1 year and 4 mo postoperatively, revealing hepatic artery stenosis.
A: Ultrasound indicated an intrahepatic artery (right hepatic artery) resistive index of 0.40, with a systolic acceleration time of 90 ms; B: Blood flow near the hepatic artery anastomosis reached 302 cm/s.
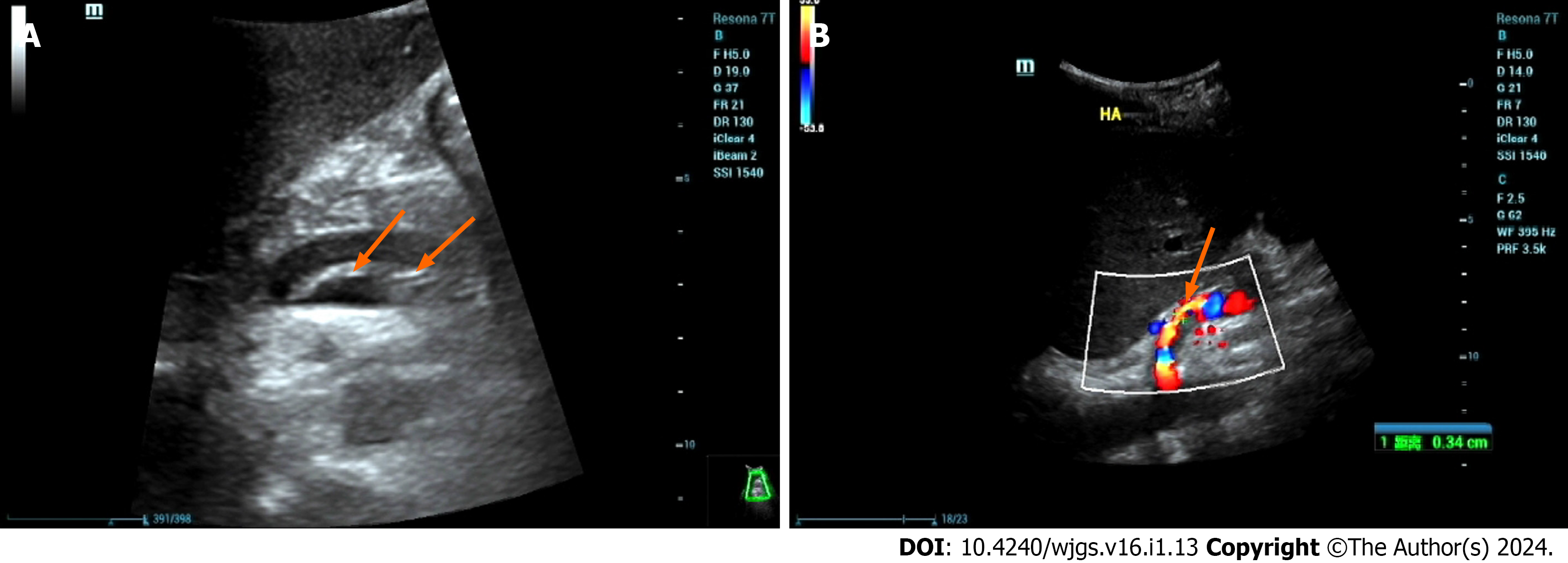
Figure 3 A 46-year-old male patient with decompensated cirrhosis due to hepatitis B underwent liver transplantation.
On postoperative day 1, ultrasound showed no blood flow signals in the hepatic artery, followed by hepatic artery angiography and thrombosis. A: Ultrasound showed intramural-like echoes floating in the proper hepatic artery (arrow); B: Ultrasound showed blood flow in the true lumen of the proper hepatic artery (arrow), with no obvious blood flow signals in the false lumen. Then, the patient underwent hepatic artery stent graft implantation with satisfactory clinical results.
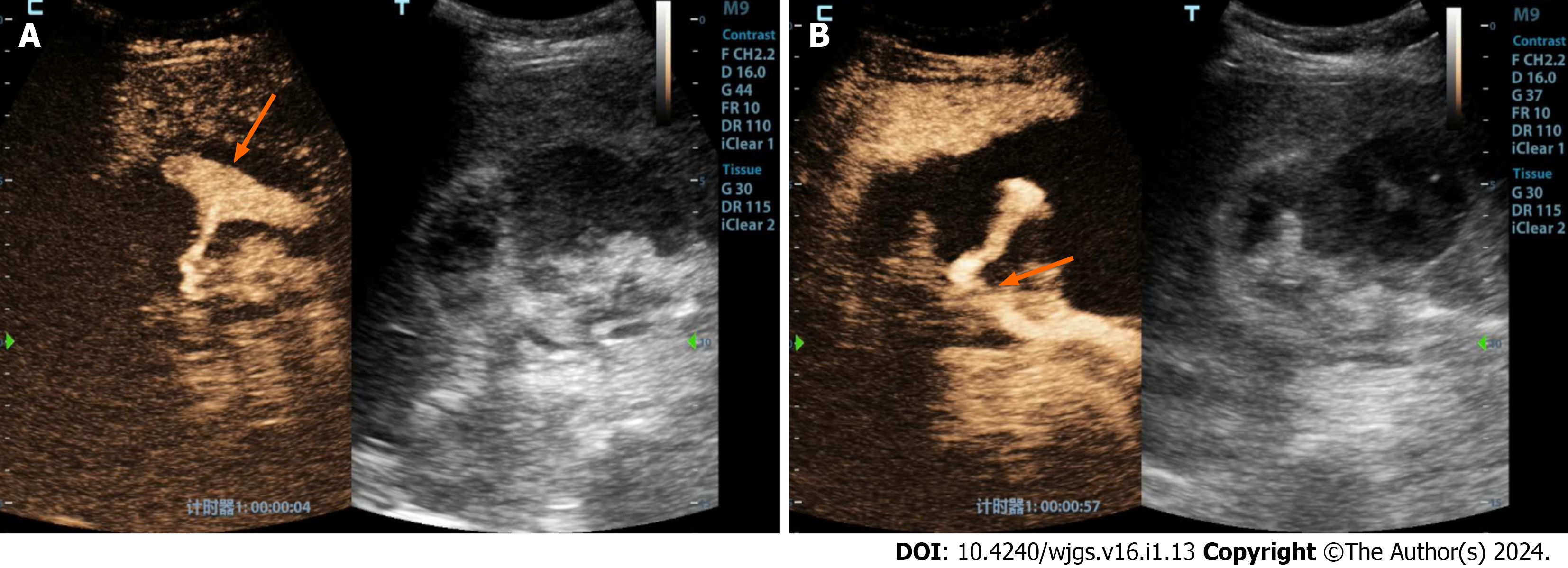
Figure 4 A 48-year-old female patient underwent a piggyback liver transplantation procedure due to decompensated cirrhosis resulting from hepatitis B.
A: Evaluated 13 d postoperatively, the patient’s clinical history revealed a progressive decline in blood pressure and red blood cell count, accompanied by the accumulation of a significant volume of intraperitoneal fluid. Conventional ultrasound examination demonstrated a substantial accumulation of fluid in the porta hepatis region, characterized by hypoechoic features and the presence of numerous fine, low-level echogenic particles suspended within. Contrast-enhanced ultrasound revealed enhanced contrast agent pooling within the intraperitoneal fluid of the porta hepatis, exhibiting a morphology resembling a mushroom cloud (highlighted by the orange arrow); B: Notably, further tracking of the contrast agent leakage within the porta hepatis area (indicated by the orange arrow) indicated that it originated from the hepatic artery anastomosis site.
- Citation: Zhao NB, Chen Y, Xia R, Tang JB, Zhao D. Prognostic value of ultrasound in early arterial complications post liver transplant. World J Gastrointest Surg 2024; 16(1): 13-20
- URL: https://www.wjgnet.com/1948-9366/full/v16/i1/13.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i1.13