Copyright
©The Author(s) 2023.
World J Gastrointest Surg. Aug 27, 2023; 15(8): 1761-1773
Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1761
Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1761
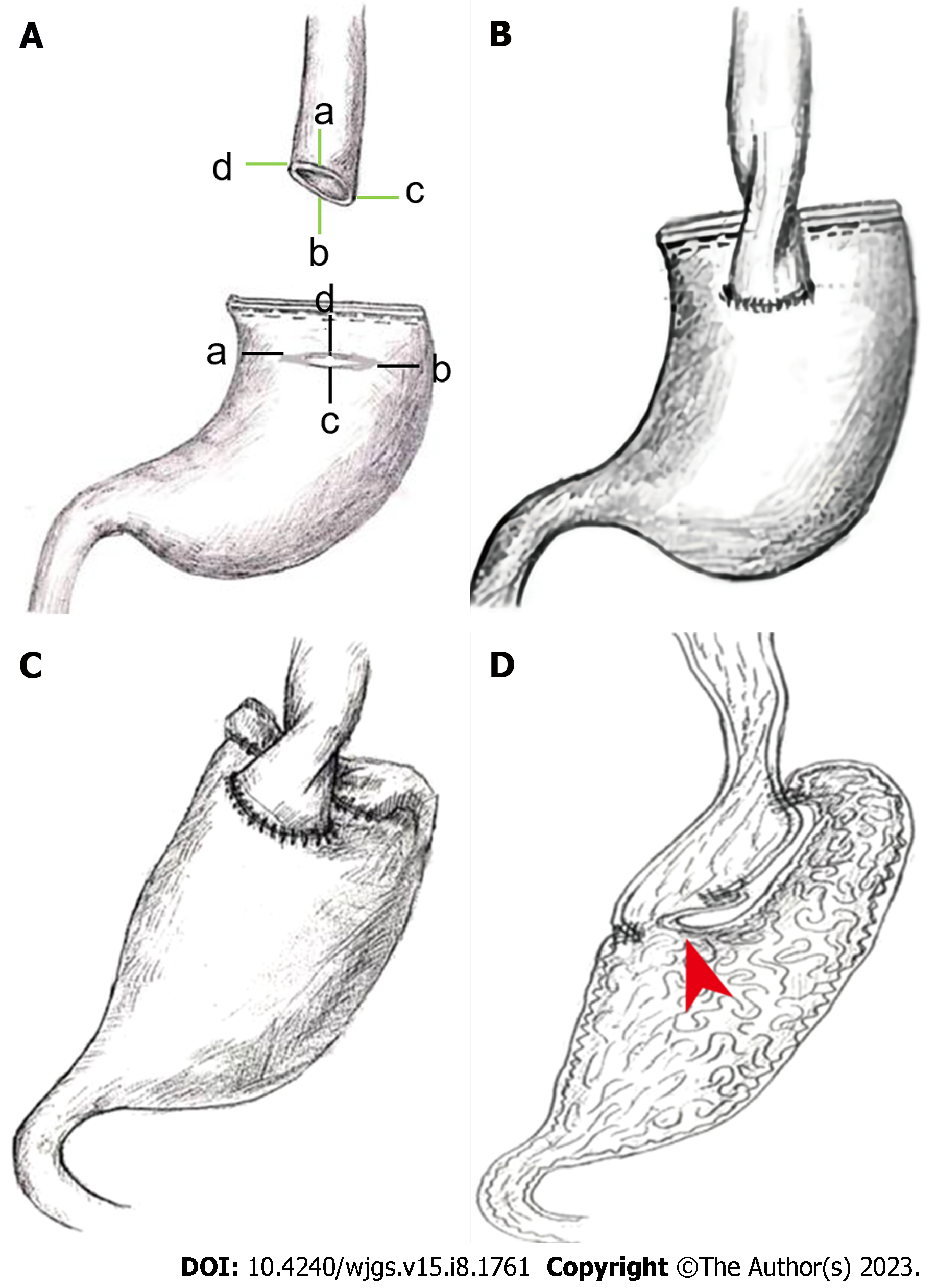
Figure 1 Critical design features of the esophagogastric asymmetric anastomosis technique.
A: (1) The diameter of the esophagus and the incision size of the residual gastric anterior wall are asymmetric; and (2) The length of the two sides of the lower esophagus is asymmetrical; The points a/b/c/d shows the corresponding points of asymmetric anastomosis respectively between esophagus and residual stomach; B: Asymmetry of the longitudinal section (or sagittal surface) of the esophagus and the residual stomach after anastomosis; C: After anastomosis, the seromuscular layer of the residual stomach and esophagus is asymmetrically sutured; D: The sagittal plane of esophagogastric asymmetric anastomosis: Showing the suture point of the asymmetric anastomosis; the red arrow indicates a flap structure formed by the folded gastric wall in the gastric cavity.
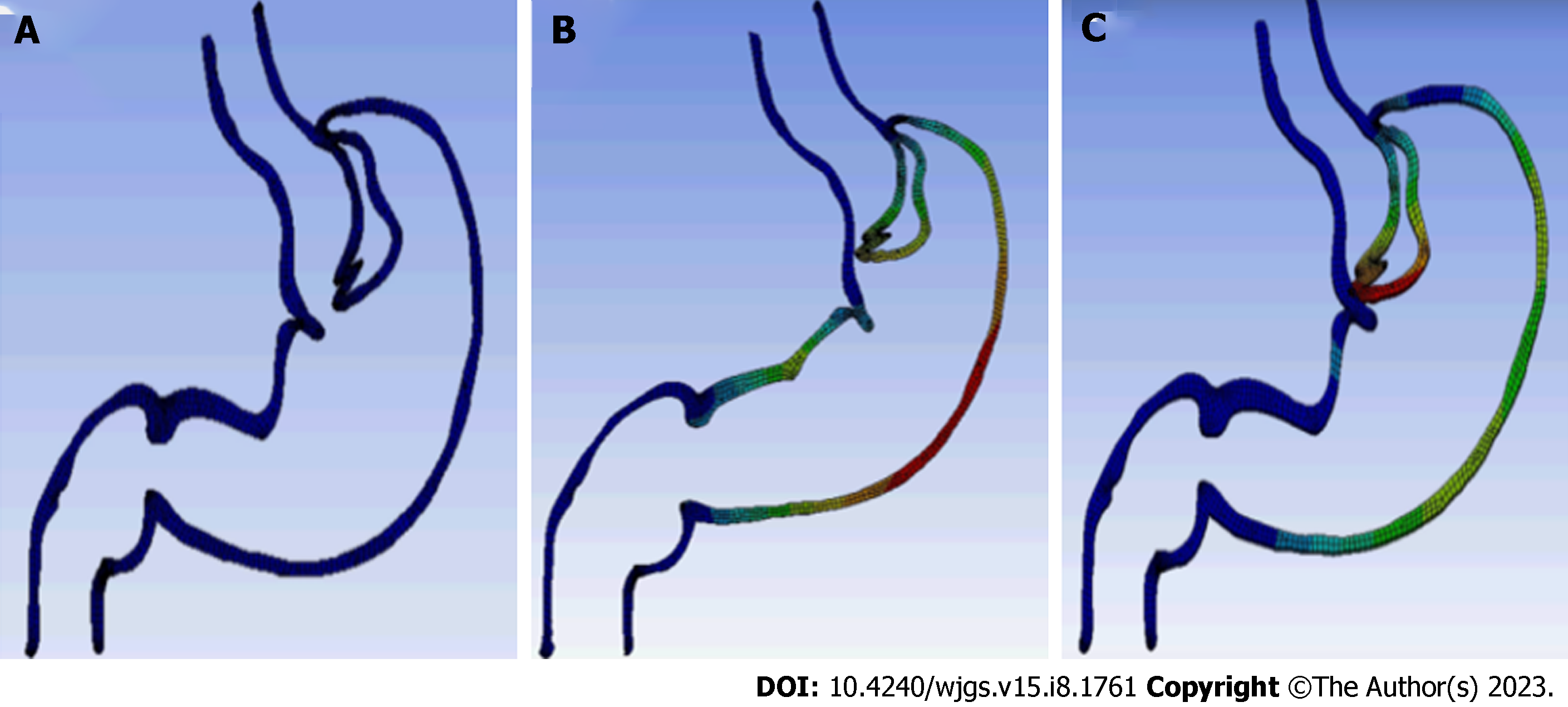
Figure 2 Computer simulations of esophagogastric asymmetric anastomosis mechanisms using the finite element method.
A: Adobe Illustrator was used to draw the curve of the gastric section; B: The valve-like structure of the folded gastric wall and the posterior wall of the lower esophagus move to the upper left side like a lever at the site of anastomotic stoma, causing tightening of the anastomotic stoma; C: Because of the increased pressure in the gastric cavity and the expansion of the gastric fundus, the folded gastric wall and the esophageal wall moved to the left, which effectively tightened the anastomotic stoma.
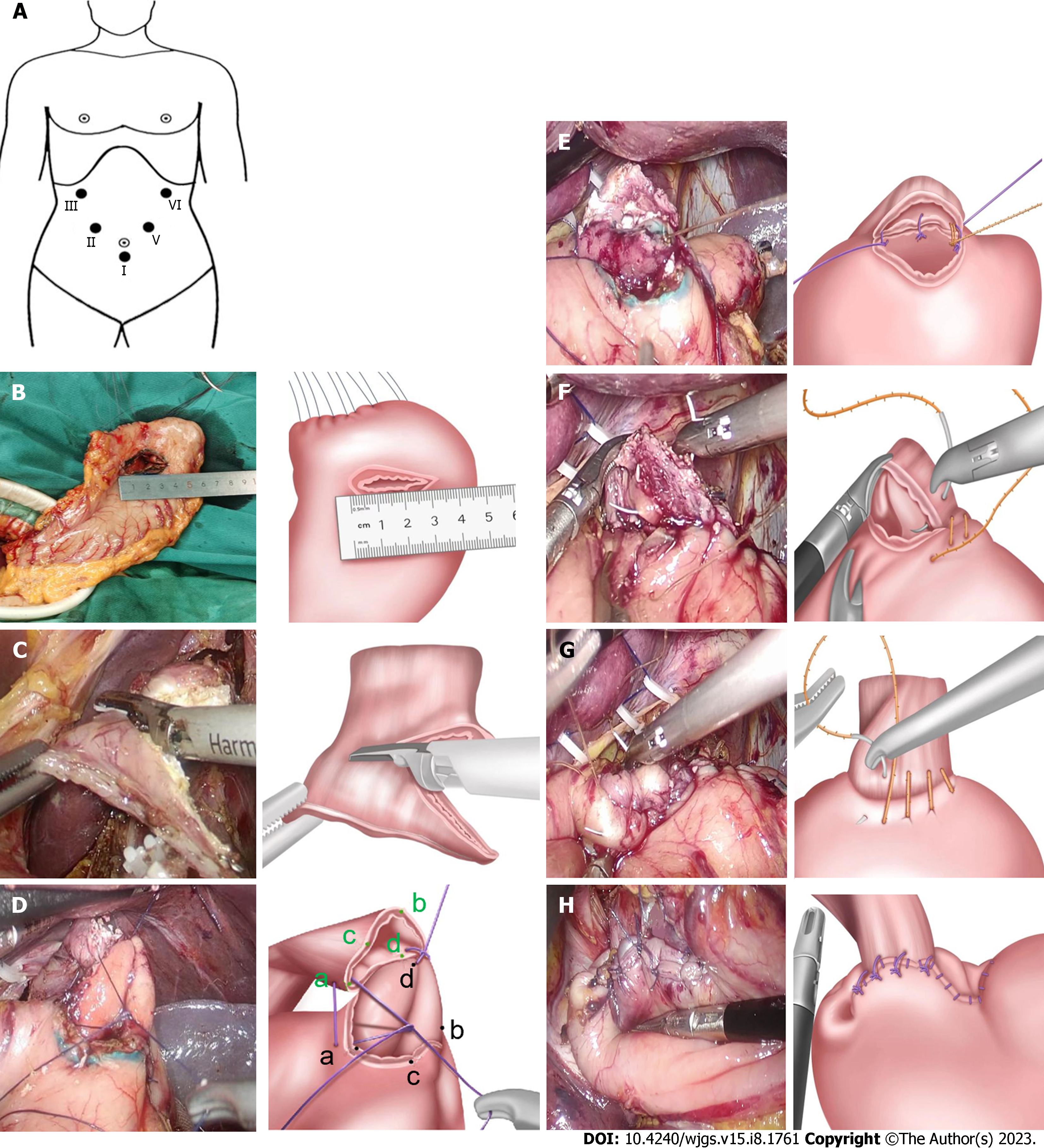
Figure 3 Surgical Procedure of laparoscopic-assisted esophagogastric asymmetric-anastomosis.
A: Reverse Trendlenborg position with both legs separated. Using five-hole method, the points I-V show the location of Trocars and operators respectively; B: The transverse incision of residual stomach wall is about 3.2-3.5 cm away from the proximal end at approximately 3.5 cm; C: The lower end of the esophagus is cut oblique, the length of both sides is asymmetric, the difference is approximately 1.5 cm; D: First, a full-thickness intermittent suture was performed between the right side (point d) of the lower esophagus and the middle point (point d) of the posterior wall in gastric incision. Then, the right point of the gastric wall incision (point a) was sutured to the middle point (point a) of the anterior wall in the lower esophagus, and the left point (point b) of the gastric incision was sutured to the middle point (point b) of the posterior wall in the lower esophagus. After performing a three-needle whole-layer positioning suture of the posterior wall in oesophagogastric anastomosis, oesophageal torsion was completed at a 90° anticlockwise; E: The back wall of the anastomosis was continuously stitched; F: The front wall of the anastomosis was continuously stitched; G: The seromuscular layer of the anterior wall of the anastomosis was further stitched; H: The residual gastric cutting end (approximately 3 cm from the anastomosis) was stitched to the posterior wall of the esophagus, about 0.5-1 cm away from the anastomosis.
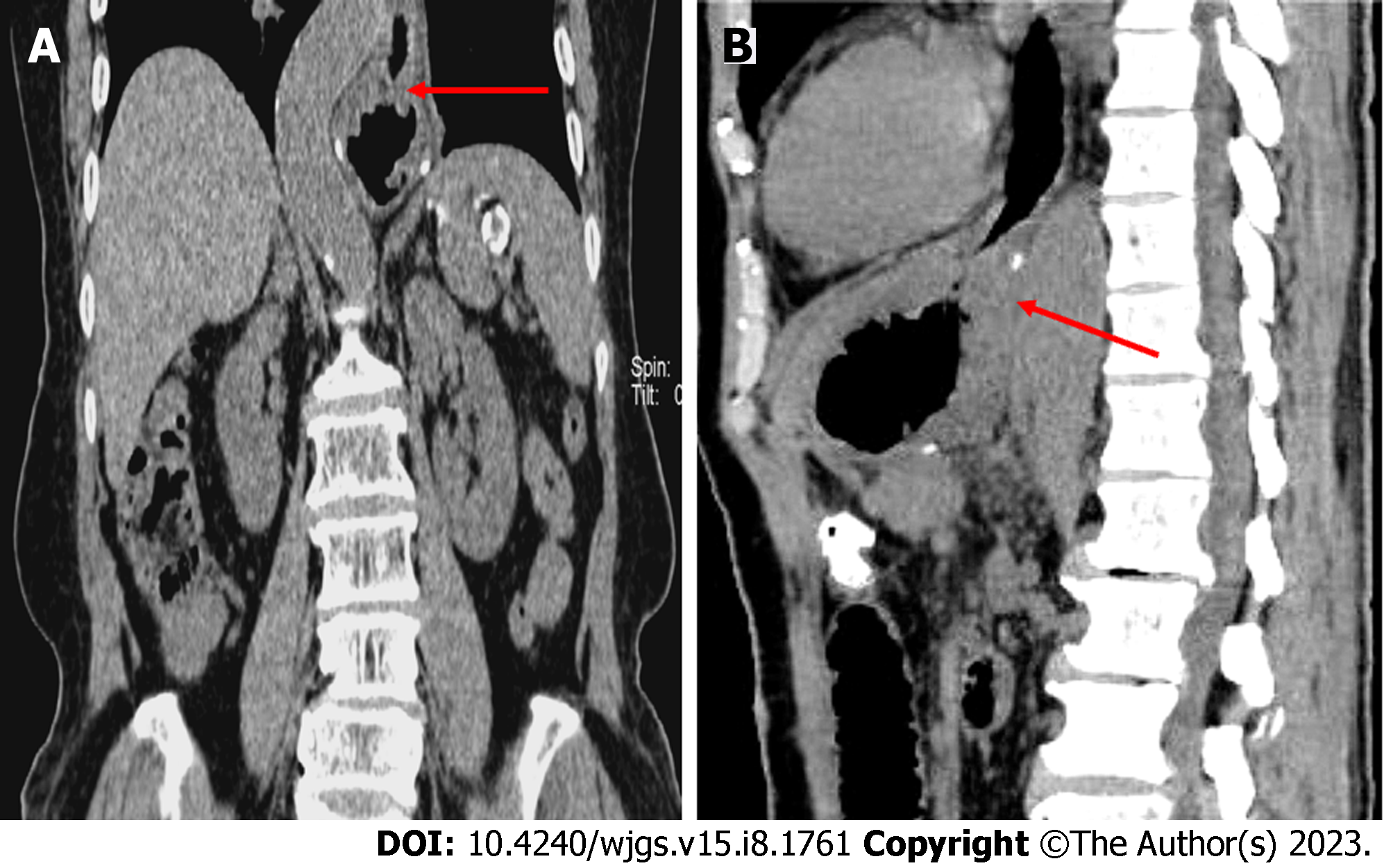
Figure 4 Abdominal computed tomography (oral CO2 powder).
A: coronal surface: The valve-like structure can be seen at the anastomosis, tightly closed; B: Sagittal plane: The gastric cavity is inflated, seeing the anastomotic valve-like structure with gear sample occlusion and a small amount of gas overflow in the esophagus.
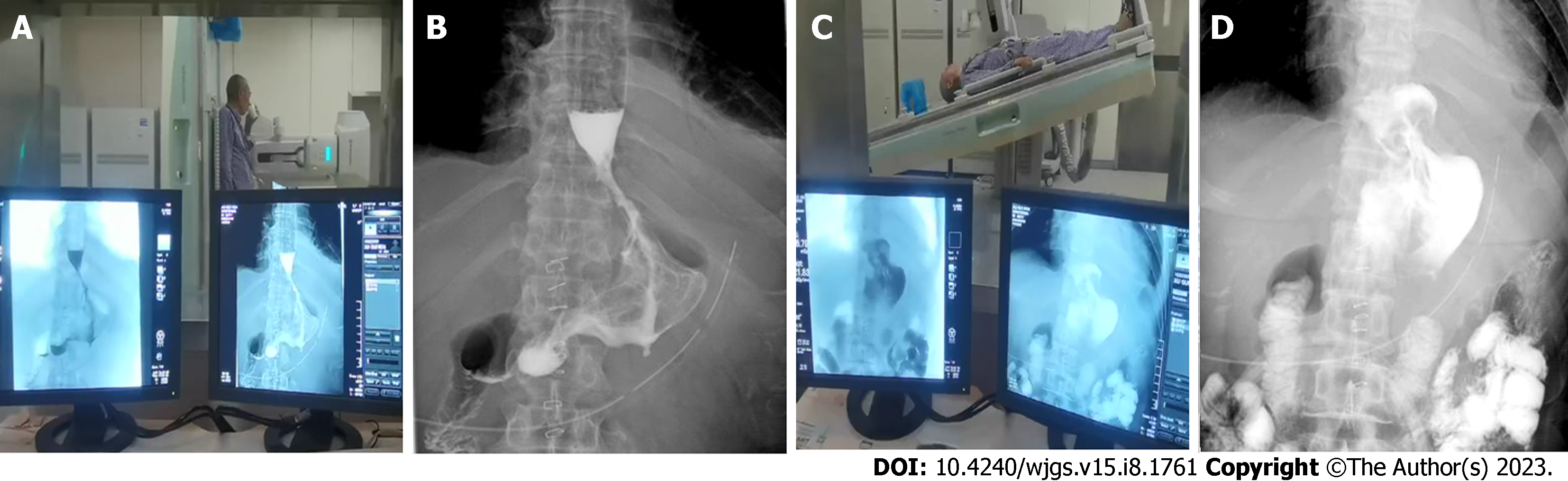
Figure 5 Upper gastrointestinal tract angiography.
A and B: Upright position: Unobstructed anastomosis, such as a normal cardia-like image; C and D: Head low foot high level: See the anastomosis is completely closed, no contrast agent reflux.
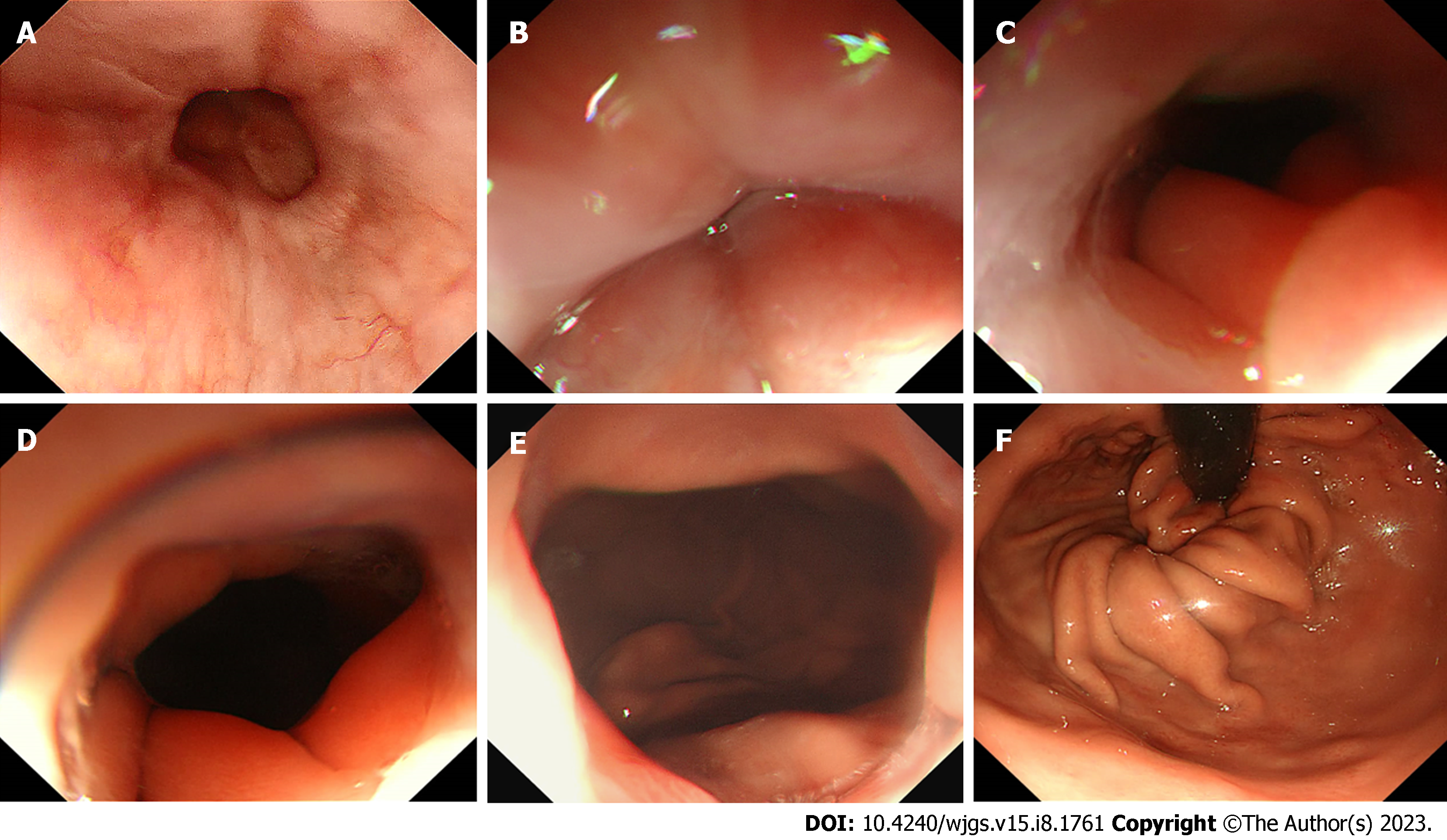
Figure 6 Gastroscope.
A: The esophageal mucosa is smooth, without hyperemia and edema, with a clear capillary network; B: The valve-like structure of the anastomosis is closed in the non-inflated state; C-E: The valve-like structure of the anastomosis opens gradually in the inflated state, with good dilation and extensibility, showing a visible dentate linear-like structure; F: The reconstructed gastric base can be seen under the inverted gastroscope, which was wrapped well by the valve-like structures of the folded gastric wall mucosa at the site of the anastomosis;
- Citation: Pang LQ, Zhang J, Shi F, Pang C, Zhang CW, Liu YL, Zhao Y, Qian Y, Li XW, Kong D, Wu SN, Zhou JF, Xie CX, Chen S. Anti-reflux effects of a novel esophagogastric asymmetric anastomosis technique after laparoscopic proximal gastrectomy. World J Gastrointest Surg 2023; 15(8): 1761-1773
- URL: https://www.wjgnet.com/1948-9366/full/v15/i8/1761.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i8.1761